full article:
Introduction
A shortage of rural physicians is a major problem for health systems in many countries1. In Japan, this issue has not yet been solved2. The maldistribution of physicians has been associated with many problems, including refusal to accept emergency patients3 and physician overwork4 in rural areas.
To increase the number of physicians in medically underserved areas (MUAs), the Japanese government initiated a special regional quota system, called chiikiwaku. Under this system, applicants to some medical schools are required to have graduated from a high school in the same prefecture. Implementation of the regional quota has been widespread since 2008; in 2016, the quota accounted for 15% of medical student entrants at 67 of 77 Japanese medical schools5. For most regional quota students, medical education is followed by an obligatory medical practice period of approximately 9 years in an MUA5. The practice location is determined by the medical school or the local government of the student’s home prefecture. Most regional quota students are required to take out a student loan but are exempted from repayment after fulfilling their obligation.
In the authors’ previous research, first-year regional quota students were surveyed regarding the motivations and associated factors for staying in MUAs after the obligatory practice period6. In that study, 52% of regional quota students anticipated being willing to remain in MUAs after their obligation was met. The factors associated with this willingness were rural upbringing, a passion to contribute to MUAs, external encouragement during medical school and perceiving the regional quota loan as having a strong influence on their work preferences.
Systems that are similar to the regional quota exist in other countries. For example, the National Health Service Corp (NHSC) in the USA has several types of programs such as scholarships and service-option loans to increase the number of rural physicians. One study reported about NHSC that 67% of those who accepted scholarships fulfilled their obligation to work in rural areas7. Some education programs recruit rural physicians without the use of scholarships, for instance the Physician Shortage Area Program and the Rural Physician Associate Program. Both programs have increased the retention rates of graduates8,9.
Although most regional quota graduates had not yet completed their obligatory practice period at the time of the present study, evaluating regional quota students during their senior year regarding their anticipated willingness to remain in MUAs long-term may be useful for planning ways to support them at an early stage. In addition, factors associated with this willingness could suggest ways of improving the selection criteria of the regional quota system.
This study aimed to clarify sixth-year (final-year) regional quota students’ anticipated willingness to remain in MUAs after their obligatory practice period and the factors associated with this willingness as assessed during the students’ first year.
Methods
Study participants
This was a prospective observational study. All regional quota students at Japanese medical schools whose deans agreed to allow student enrollment in the survey were included. Students who did not answer the question about the primary outcome were excluded. In this study, the regional quota was defined as a special quota system requiring obligatory medical practice in MUAs after graduation, regardless of the length of the obligation or the student loan amount. This definition is the same as that used in the authors’ previous study6. Baseline data were collected during students’ first year, from September 2010 to February 2011. Follow-up data were collected during students’ sixth year, from August 2015 to January 2016.
Data collection
Self-report questionnaires were used in both the baseline and follow-up surveys. The methods of distributing and collecting the questionnaires were the same as in the previous study6. The questionnaire used in baseline survey collected demographic information such as sex and hometown type, the latter defined by scale (metropolis, suburb of metropolis, city, town or village and remote area). Subjects were also asked to rate on a five-point Likert scale the degree to which they experienced external encouragement (whether they felt that admission based on a regional quota was encouraging their studies) and stress (whether they felt that obligatory practice and/or loan repayment was stressful) related to the regional quota status. Regarding factors influencing future work preferences, the questionnaire asked about preferred location type, number of working hours and call frequency, for example. The influence of these factors on work preferences was assessed based on the subjective judgement of respondents using a five-point Likert scale. Most of the questions were the same in the baseline and follow-up surveys. Sixth-year regional quota students’ anticipated willingness to remain in MUAs after their obligatory practice period was the primary outcome, and was assessed using a five-point Likert scale (‘very willing’, ‘somewhat willing’, ‘neither willing nor unwilling’, ‘somewhat unwilling’ and ‘completely unwilling’). Baseline survey questions were described in the previous study6. Student identification numbers were used to link the data in the baseline and follow-up surveys.
Statistical analysis
Participants were categorized into two groups (willing and unwilling) for the primary outcome. The willing group consisted of participants who reported that they were ‘very willing’ or ‘somewhat willing’ to remain in MUAs after the obligation period. The unwilling group consisted of participants who answered ‘neither willing nor unwilling’, ‘somewhat unwilling’, or ‘completely unwilling’. To identify factors associated with the anticipated willingness to remain in MUAs, a univariate analysis was performed using the Χ2 test. Independent variables included demographic characteristics, stress and external encouragement related to the regional quota status, the primary reason for applying for the regional quota, factors influencing work preferences, and first-year students’ anticipated willingness to remain in MUAs. These variables were collected during the baseline survey. Independent variables were all categorical and were dichotomized using the same cutoffs as used in the previous study6. Regarding the influence of factors on work preferences, the cutoff for each factor was between ‘large influence’ and ‘small influence’ of a 5-point Likert scale. The Likert scale consisted of ‘very large influence’, ‘large influence’, ‘small influence’, ‘tiny influence’ and ‘no influence’.
Variables in the multivariate logistic regression analysis included sex and the variables from the univariate analysis that had a significance level of p<0.1. The collinearity between independent variables was examined using Spearman’s coefficient of correlation. If the coefficient was over 0.6, the variable with a higher p value in univariate analysis was removed from the multivariate analysis. The significance level in multivariate analysis was set at p<0.05. Statistical analysis was performed using the Statistical Package for the Social Sciences v23 (IBM; http://www.spss.com).
Ethics approval
The cover page of the questionnaire stated that the information gathered in the survey did not affect the student’s academic record. Students were asked to submit completed questionnaires in a sealed envelope provided by the researcher. This study was approved by the Ethics Committee of the Faculty of Medicine of the University of Tsukuba. The approval numbers were 21-413 and 21-413-2.
Results
Of 63 medical schools that had a regional quota at the time of baseline survey, 42 schools agreed to participate in this study. A total of 405 first-year students (74.7%) at 38 medical schools answered the questionnaire. Of these, 208 students (51.4%) were followed up 5 years later (Fig1). There were 121 (58.2%) male students and 87 (43.8%) female students. Sixty-seven students (32.2%) came from rural areas (‘town or village’ or ‘remote area’).
The baseline survey results showed that 95 (23.4%) first-year students anticipated being very willing to remain in MUAs, 117 (28.9%) were somewhat willing, 157 (38.8%) were neither willing nor unwilling, 31 (7.7%) were somewhat unwilling and 5 (1.2%) were completely unwilling. In the follow-up survey, 8 (3.8%) sixth-year students were very willing, 32 (15.4%) were somewhat willing, 119 (57.2%) were neither willing nor unwilling, 42 (20.2%) were somewhat unwilling and 7 (3.4%) were completely unwilling. The proportion of respondents who as first-year students stated an anticipated willingness to remain in MUAs (‘very’ or ‘somewhat’ willing) was 53.8% in the follow-up group and 50.8% in the group that was lost to follow-up.
Tables 1 and 2 categorize subject characteristics by sixth-year students’ anticipated willingness to remain in MUAs. Due to their large number, factors influencing work preferences are shown separately in Table 2. In the univariate analysis, rural upbringing, external encouragement to participate in the regional quota, first-year students’ anticipated willingness to remain in MUAs and influence of income on work preference were significantly associated with sixth-year students’ anticipated willingness to remain in MUAs. All of these variables were included in multivariate analysis because Spearman’s coefficient of correlation was less than 0.6.
Multivariate analysis showed that rural upbringing (odds ratio (OR) 2.1; 95% confidence interval (CI) 1.0–4.4), influence of income on work preference (OR 0.3; 95%CI 0.1–0.9) and first-year students’ anticipated willingness to remain in MUAs (OR 3.3; 95%CI 1.4–7.8) were significantly associated with sixth-year students’ anticipated willingness to remain in MUAs (Table 3).
Table 1: Participant characteristics by anticipated willingness to remain in medically underserved areas 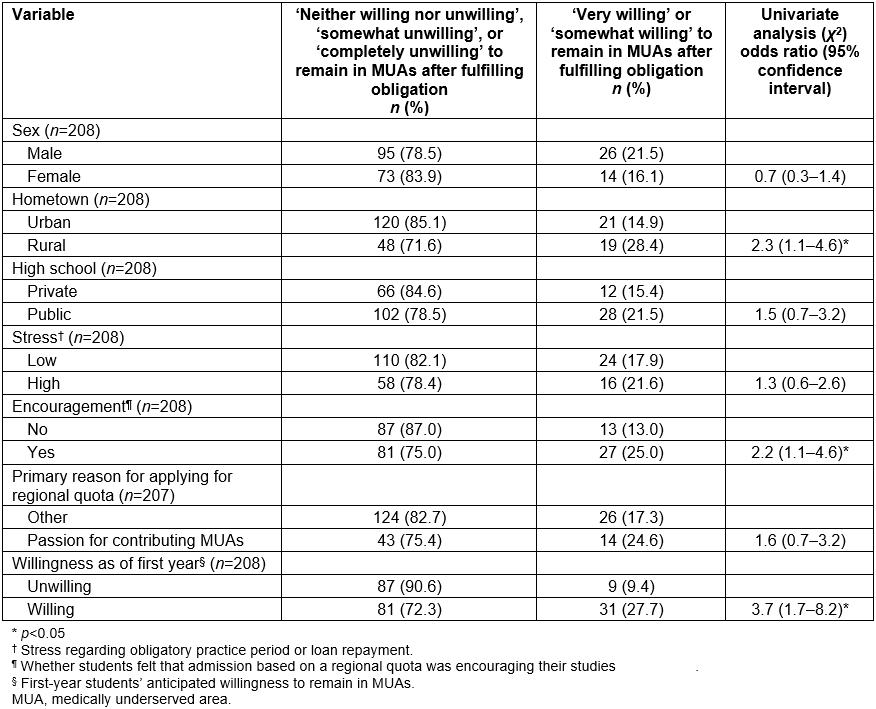
Table 2: Factors influencing work preferences by anticipated willingness to remain in medically underserved areas 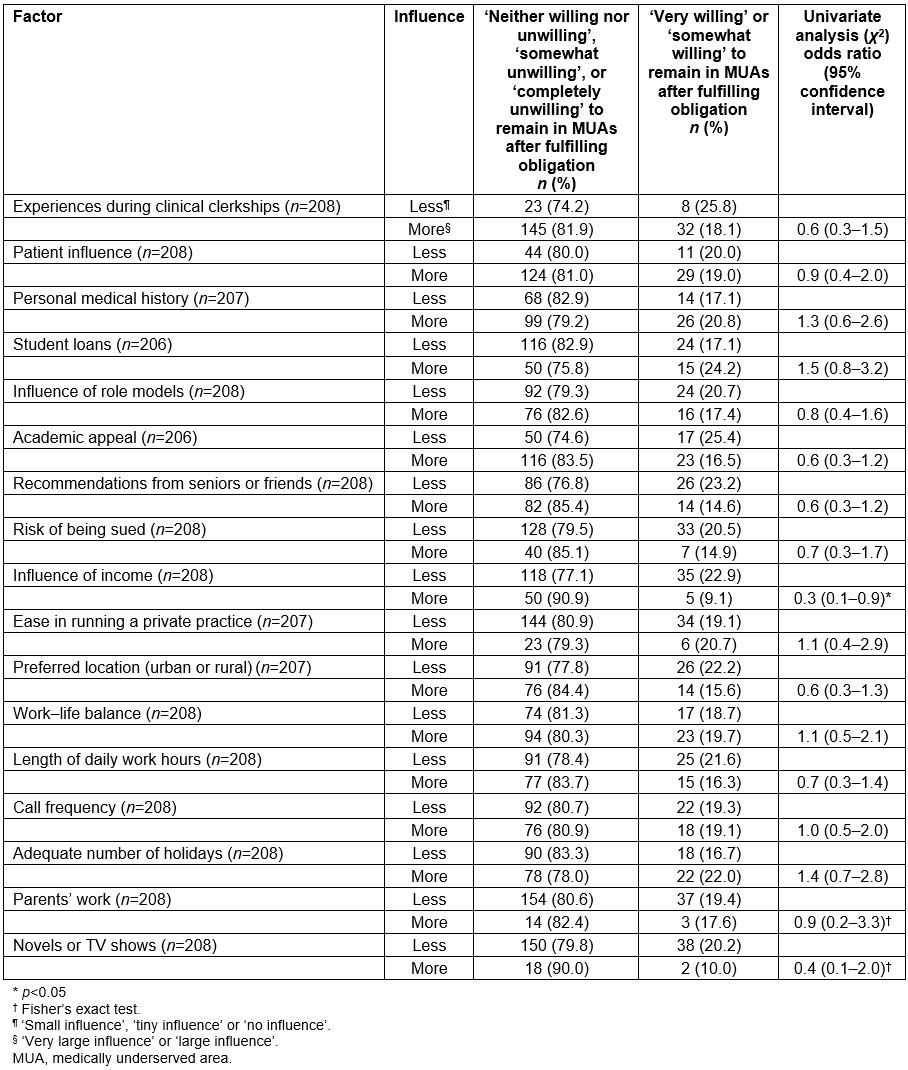
Table 3: Multivariate analysis† of factors associated with anticipated willingness to remain in medically underserved areas (n=208)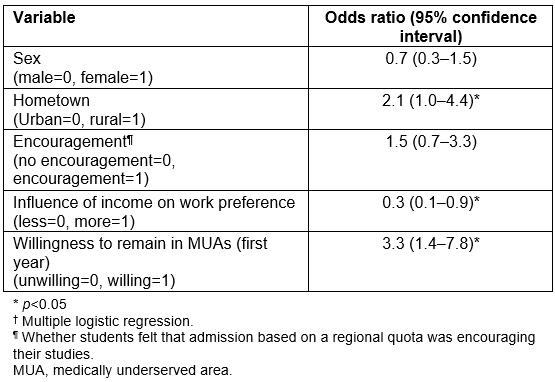
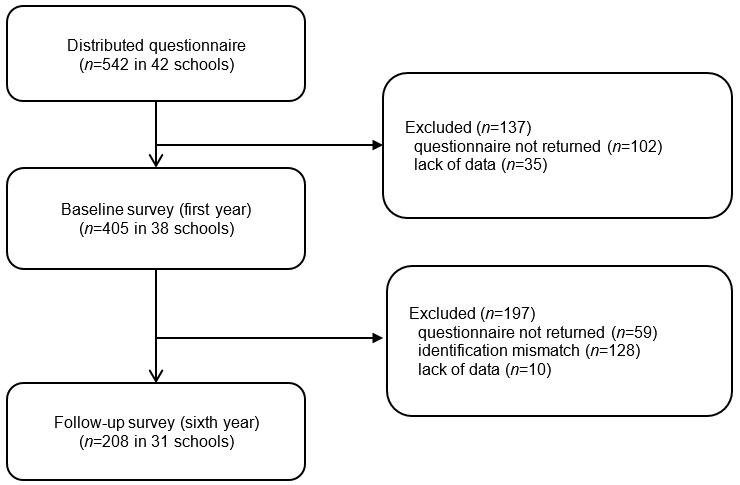 Figure 1: Study flow chart.
Figure 1: Study flow chart.
Discussion
During their first year, 52% of regional quota students were ‘very’ or ‘somewhat’ willing to remain in MUAs after their obligatory practice period, but this proportion declined to 20% by the time students reached their sixth year. Factors associated with sixth-year students’ anticipated willingness to remain in MUAs were rural upbringing, influence of income on work preference and anticipated willingness to remain in MUAs during their first year. These factors were reported by previous studies to be related to working in rural areas or MUAs.
Previous cross-sectional studies10,11 showed that medical students in their junior (first or second) year had great interest in rural medicine. Some cohort studies reported the proportions of medical school graduates who remained in rural areas after a special program8 or medical school12 to increase the number of rural physicians, but few cohort studies have assessed undergraduate students across multiple schools in terms of their intention to remain in MUAs or rural areas. The cause of the decrease in anticipated willingness to remain in MUAs from the first to the sixth years was not clear in this study, but medical students have been shown to change their views of their occupations as physicians after their clinical clerkships13,14. Colwill indicated that the curriculum in medical schools focused on biomedical sciences and hospital-based specialties15. This perspective has not yet changed16. This academic milieu may decrease interest in rural medicine or ‘primary care’-based specialties during undergraduate education. Students may be more influenced by urban doctors than rural doctors since most clerkships in Japanese medical schools take place at tertiary care facilities in urban areas17. Career choice can also be influenced by debt load17,18, concern about lifestyle19 and burnout20. Rural physicians, especially primary care physicians, have lower incomes than other specialists21, which may make rural work unattractive to medical students who place significant importance on salary and control over work schedule22. In addition, empathy for patients is essential to physicians including rural doctors, but empathy declines among medical students over the course of medical school23.
Rural upbringing was associated with rural recruitment24,25 and retention12 in several studies. The present study also showed an association between rural upbringing and anticipated willingness to remain in MUAs. Selecting rural students for regional quotas might help increase the number of well-motivated students who remain in MUAs after their obligatory practice period. Kawamoto et al11 showed that medical students who placed importance on their expected income were less motivated to practice in rural areas. Such students may prefer urban life and the greater variety of ways to spend their incomes. Regional quota students’ anticipated willingness to remain in MUAs was much lower in their sixth year than their first year, but there was a significant association between the two time points. This finding is consistent with the concept of the rural pipeline26; to increase the rural medical workforce, it is important to select rural students and support them in maintaining their motivation to work in rural areas. Undergraduate medical education tends to emphasize tertiary care27, but it should focus more on primary care or community medicine to foster community doctors.
In the authors’ previous study, rural upbringing was associated with first-year students’ anticipated willingness to remain in MUAs6; this factor seems important regardless of when students are assessed. On the other hand, a passion to contribute to MUAs as the primary reason for selecting the regional quota, external encouragement during medical school and perceiving the regional quota loan as having a strong influence on work preferences were not significantly associated with the anticipated willingness to remain in MUAs during sixth year. This may be because regional quota students’ viewpoints regarding student loans or obligatory practice change during medical school.
There are several limitations to this study. First, the follow-up rate (51.4%) was not high because of non-cooperation and identification mismatch. However, the proportion of first-year students who anticipated being willing to remain in MUAs was similar in the follow-up group (53.8%) and the loss to follow-up group (50.8%), suggesting that the former was representative of the overall population. Second, the primary outcome of this study, namely the anticipated willingness to remain in MUAs, was a surrogate outcome. Whether regional quota students actually observe the obligatory practice and remain in MUAs after their obligatory practice periods should be surveyed in the future. Third, there was no control group such as non-quota students to compare the willingness of study participants. A cross-sectional survey of first-year medical students28 showed that regional quota students were more willing to remain in MUAs after their obligatory practice period than were non-quota students. Regional quota students may have higher willingness than non-quota students in their final year if the willingnesses of regional quota students and non-quota students decrease by the same proportion. In addition, specifics regarding educational or regional quota systems (for instance, the length of the obligatory practice period or the amount of loans) were not considered in this study. These factors may be confounders of other variables.
Conclusions
Regional quota students’ motivation to remain in MUAs decreased as they progressed through medical school. The present results suggest that to increase the number of physicians in MUAs, it may be important to recruit regional quota students who grew up in rural areas, who are not interested in expected income and who anticipate a willingness to remain in MUAs at the time of admission.



