full article:
Introduction
In many developing countries, strategies focusing on an increased number of births assisted by skilled birth attendants (SBAs) are commonly adopted to reduce maternal mortality1. Some countries showed considerable reduction in maternal mortality after employing such strategies. In Malaysia and Sri Lanka, a scaled-up SBA program was established and sustained, resulting in notable improvement in maternal health2. Afghanistan Ministry of Public Health provided training for about 805 midwives between 2002 and 2007, and successfully expanded its midwifery program3. An international systematic review of maternal and child health interventions found no rigorous evidence that an increase in the proportion of SBAs had a definitive effect on decreased maternal mortality4; however, this may not apply in contexts such as Sudan and many other parts of Africa where there is a shortage in SBAs and insufficient infrastructure, emphasising the important role rural health workers may play. Walraven and Weeks5 expressed concern over the shift towards SBAs in international safe motherhood initiatives and policy without adequate assessments of the effectiveness of the training for traditional birth attendants (TBAs) and the services they provide. Prata et al1 stated that although there is a global trend of strengthening health systems, this strategy is not sufficient alone but should be considered on a country or regional basis.
Many sub-Saharan countries are still experiencing an overall SBA shortage. The Republic of Sudan (hereinafter referred to as Sudan) has been in a reconstruction stage since the 2005 Comprehensive Peace Agreement was signed after prolonged civil war. Maternal and child health indicators, such as the maternal mortality ratio and infant mortality rate, remain high, and are among the most urgent health issues for the country. Sudan’s shortage of qualified human resources for health hampers provision of optimal maternal and child health care, especially in rural areas. To provide supervision for all levels of midwives working at health facilities and in local communities, a national strategy of supportive supervision was institutionalised by Sudan’s Federal Ministry of Health. Under this system, health visitors/assistant health visitors are assigned to supervise village midwives (VMWs). One health visitor/assistant health visitor is assigned as the locality supervisor for all health visitors/assistant health visitors in that locality. At the next level, the State Ministry of Health is responsible for supervising locality supervisors. As part of supportive supervision, health visitors/assistant health visitors are recommended to regularly visit clients’ houses with the VMWs for supervision. However, some health visitors/assistant health visitors face considerable operational constraints in geographically widespread communities with inadequate infrastructure and transportation6 This means that minimally trained VMWs are left in the community without opportunity to receive training or supervision.
In reality, VMWs provide many basic maternal services in rural Sudan6. Nearly half of community women chose to deliver at home with traditional birth assistants or no assistance, and many do not receive antenatal care (ANC)6. Mwangome et al (2012) identified a number of perceived barriers to seeking care of an SBA at birth-in facilities such as lack of resources, customer care, and knowledge and beliefs in rural Kenya7. A previous study in Sudan reported that lack of ANC was associated with a higher risk of neonatal and maternal mortality, and indicated that most deliveries start at home and are referred to health facilities if there are maternal complications8. This highlights the need for community-based birth assistants with proper knowledge and skills to recognize abnormalities in a timely manner. This is especially the case in rural Sudan, which has a serious shortage of human resources as well as cultural barriers that inhibit access to health facilities. Arabi et al9 indicated that Sudan’s system of VMW training, which was started in 1921 by the government, was based on selection of community women by local municipalities to attend one of the nation’s 40 midwifery schools, become VMWs and work in their village of origin. There are around 17 000 VMWs handling 76.6% of the total births at home in Sudan6,9. To address pregnancy-childbirth complications and reduce maternal and newborn deaths, incorporating the existing health workers (VMWs) into the national health system/plan became urgent policy in Sudan because health workers who come from these localities are likely to return there for work; many people cannot access formal health facilities due to transport and cost issues, therefore preferring to be attended at home; and there are local realities and issues that are better addressed by the people who live in the area6.
This article examined a realistic strategy adopted in Sudan that aimed to improve home-based maternal and newborn services provided by VMWs, assessed whether VMW training and other interventions had an effect on improving service delivery and identified factors linked with the improved performance of VMWs in their communities from their own and their communities’ perspectives.
Intervention
The intervention discussed here was part of a larger project to provide comprehensive assistance to improve maternal and child service delivery based on the continuum of care: integrated efforts during the entire lifespan, in which services are provided in households, communities and health facilities10-12. In this project, a number of activities were conducted in Sinnar state, including VMW capacity building, placing medical professionals at local hospitals, strengthening linkages between health facility/staff and VMWs, strengthening the supervision system and linkages between health visitors/assistant health visitors and VMWs, providing medical equipment, repairing and maintaining facilities, and strengthening the governance capacity of Sinnar’s State Ministry of Health. In addition, community activities were conducted to establish a community volunteer system to ensure the health of pregnant mothers and neonates, and a system of pregnancy registration and emergency referral was introduced by raising and pooling funds from community members as preparation for emergency referrals. To measure the effectiveness of the intervention, a baseline survey was conducted in October 2011 and an endline survey in October 2013.
Methods
Study setting and population
The baseline and endline survey were conducted in one locality hospital, two rural hospitals, five health centers and two basic health units. In total, 57 VMWs who worked at health facilities and received interventions in the eight communities (Gladeema, Fagad, Al Sahaba, Al Rigeeba, Fanguga, Om Rihaba, Al-Giwazat and Alazaz Damous) in Sinnar state were surveyed. Community women who had given birth within the previous year in the same eight communities were also targeted; 160 community women were surveyed at baseline and 156 were surveyed at endline. After data cleaning, data for all 57 VMWs were analysed. Five of the targeted 156 community women were excluded from the analysis because the validity of their responses was questioned.
Although the participants in the baseline and endline surveys were not the same, the authors compared characteristics such as demographics, residence and number of previous pregnancies to ensure that they were relatively similar (Table 1).
Table 1: Characteristics of targeted community women in the baseline and endline surveys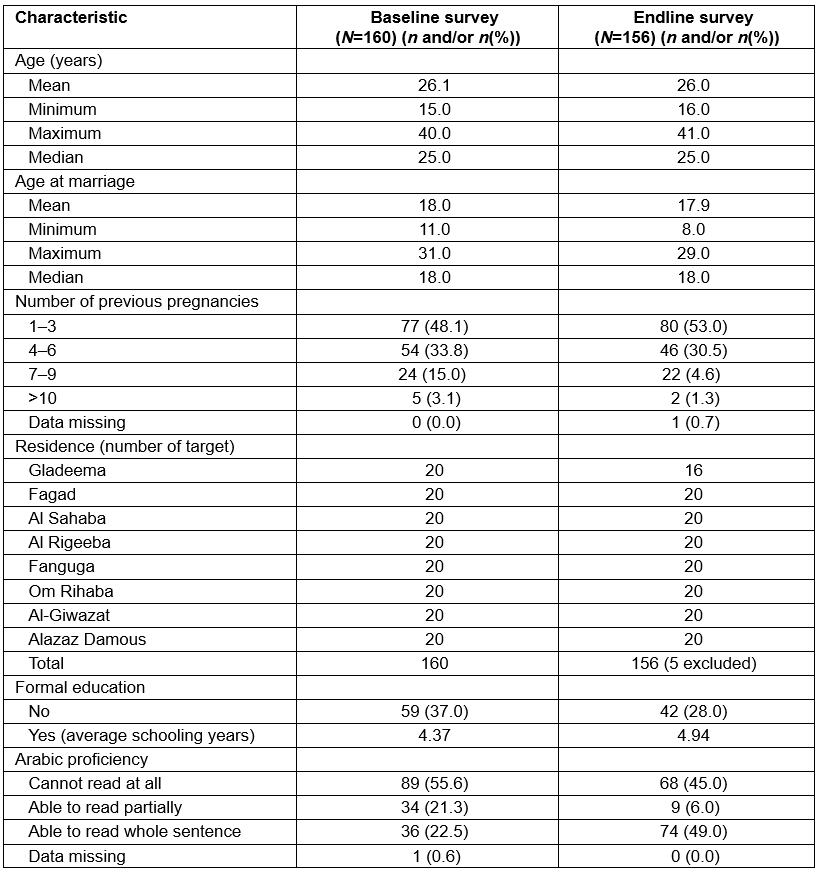
Data collection
Semi-structured questionnaires were developed to collect data on several domains and the same questionnaire was used for both surveys. For VMWs specifically, data collected related to:
- general background information
- their experience of in-service training
- ANC
- births
- postnatal care
- their experiences of referral
- supervision and their relationships with supervisors
- recording and reporting
- VMW kits and materials
- their experience of working with the community.
For the targeted community women specifically, data collected related to:
- child mortality
- background
- ANC
- delivery plan and emergency preparedness
- delivery
- postnatal care
- knowledge of key danger signs, and information gaps
- comments on health services.
The survey team comprised five data collectors. A field coordinator visited the target communities and the surveys were usually conducted at health centers in a central location in each community. Before conducting the survey, the data collectors received 2 days of training to enable them to understand the purpose of the survey, familiarise themselves with the content of the questionnaires and develop their interview techniques. Data were collected through face-to-face interviews conducted by the data collectors. The interviews lasted approximately 30 minutes. Interviews were conducted and transcribed in Arabic, and later translated into English.
In-depth interviews were conducted to gain more detailed or background information about the data obtained from interviews based on the semi-structured questionnaires. In-depth interviews were also conducted when data from the semi-structured questionnaire-based interviews seemed contradictory or invalid, and necessitated further clarification and information. The duration of each in-depth interview was 15–45 minutes and followed guidelines that had been developed to standardise the interviews as much as possible.
Data entry and cleaning
The survey supervisor checked completed questionnaires at the end of each field day to ensure optimal data quality. Data collected from the semi-structured questionnaires were first translated into English and then entered into Excel 2010 or SPSS v22 (IBM Corporation; https://www.ibm.com/analytics/data-science/predictive-analytics/spss-statistical-software). Some data were converted into numerical data to calculate basic statistics. The data were cleaned to ensure quality and guarantee validity. In this analysis, all of the interviewed VMWs were included as valid respondents. After careful examination of the data, invalid data were identified and excluded from the analysis. When the data contained contradictory or valuable information, the information was checked directly with the respondents over the telephone.
Data analysis
The data were analysed quantitatively and qualitatively. Data in the Excel spreadsheets were merged with that from SPSS and analysed using both Excel and SPSS. Quantitative data were summarized using percentages or ratios. Some continuous data were analysed by categorization into equal-sized groups. Some quantitative data are presented as median, mean, minimum and maximum values to allow comparisons with baseline data. Qualitative data were collected from open-ended questions in the questionnaires and from in-depth interviews. Free comments elicited by some questions in the semi-structured questionnaires were coded and categorized into themes, whereas free comments elicited from other questions were simply presented as transcripts without coding.
Ethics approval
Ethics approval for the survey was obtained from the Federal Ministry of Health Ethical Committee, Khartoum, Sudan. Participants were first informed about the purpose of the survey and their right to decline an interview. Consent to participate was obtained before participants were interviewed and participation was voluntary. Participants were assured that all information collected would remain confidential and their names and affiliations would be anonymized when the data were documented and disclosed for the program purpose.
Results
Endline interviews with VMWs revealed the average number of years of schooling was 3.4 years, and 30% had never received any formal education. More than half of the VMWs had less than 10 years of work experience, whereas others had worked as a VMW for more than 20 years. As shown in Figure 1, 33.3% of VMWs were allocated to hospitals and 35.1% were based at health centers; of these, one-third received a formal salary. The number of VMWs working regularly at a health facility decreased from 83% (baseline) to 60% (endline). More VMWs were working in the community rather than in health facilities at endline compared with baseline.
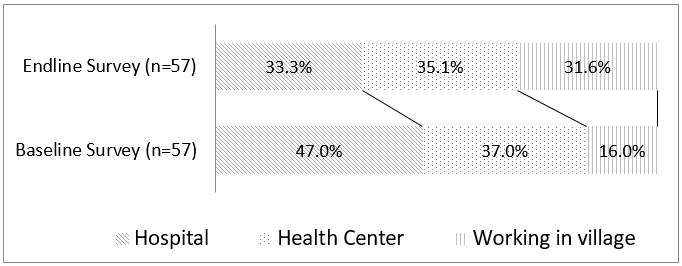 Figure 1: Distribution of village midwives at baseline and endline surveys.
Figure 1: Distribution of village midwives at baseline and endline surveys.
Endline interviews with community women revealed that a large proportion of mothers chose to give birth at home (78.1%; Table 2). The main birth attendants at the respondents’ most recent births were VMWs (58.9%). The number of home births attended by VMWs increased substantially at endline compared with baseline; baseline data showed the mean number of home births assisted by a VMW was 1.4, which increased to 3.3 at endline. In total, 47.0% of mothers had received ANC from VMWs. Health centers were the most common place to receive ANC (59.6%), followed by hospitals (27.2%) and the women’s own homes or a VMW’s house (25.2%). The main postnatal providers were family members (53.0%) and VMWs (47.7%).
The improvement needed for provision of ANC services most commonly mentioned by VMWs was increased knowledge and confidence in providing advice for community people or making referral decisions. VMWs also noted a need for increased awareness among the community.
My supervisor always tells us to increase the awareness of community women and advises us to take any opportunity to raise awareness during social activities where community women gather, such as wedding ceremonies and baby-naming ceremonies. (VMW in Fanguga village)
I offer ANC even without being paid because I now understand how important ANC is. (VMW in Tererat Madani village)
Mothers understand the importance of ANC now: that’s why they keep showing up to receive ANC. (VMW in Wadanile village)
Table 2: Places and providers of maternal health care at endline survey (N=160).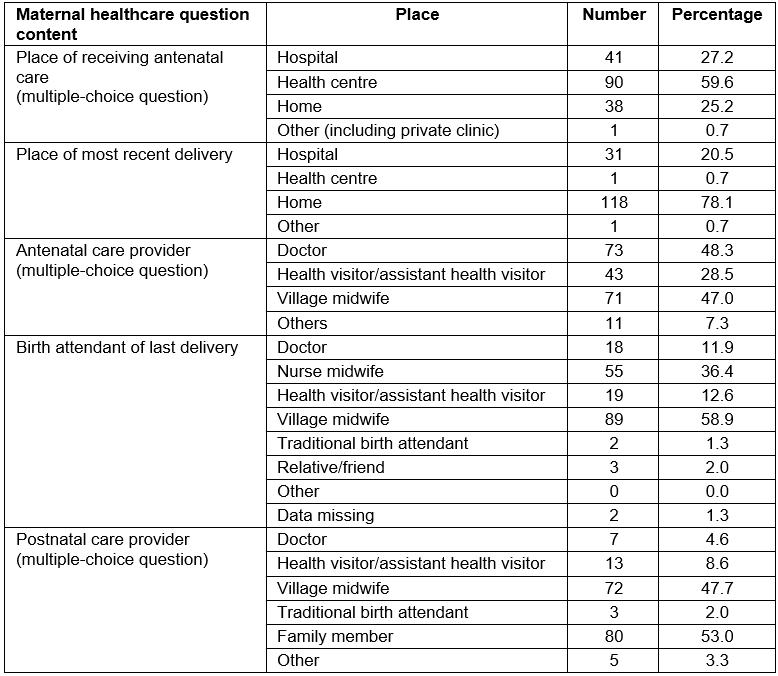
Of the 57 VMWs interviewed, 52 had made emergency referrals in the past year; 34 referrals (60%) were made during a woman’s pregnancy, 36 (63%) during labour and 13 (23%) during the postpartum period. The average number of emergency referrals increased from 1.55 to 3.54. VMWs were asked whether they felt it was easier to refer emergency cases of mothers and neonates to the hospital than it had been before. Ten VMWs (18%) answered ‘yes’, whereas 46 (81%) disagreed. The main reasons why many VMWs did not feel emergency referrals were easier concerned community members’ lack of transportation (too expensive, unavailable and/or inaccessible during the rainy season) and/or lack of available money to pay for transportation. In addition, some women believed that a referral would automatically lead to a caesarean section, in which case they refused to be referred to hospital. Despite these obstacles and misunderstandings, some VMWs played a major role in referring mothers to hospitals.
I convinced a mother to be referred because of a previous caesarean section scar. Since the mother’s family could not afford to pay for the cost of referral, I asked for financial support from community members. Thus, the mother was able to borrow 350 SDGs [Sudanese pounds] from the community fund [which was initiated as part of the project’s community activities] and she successfully gave birth at a hospital. (VMW in Fanguga village)
There was an unmarried woman who suffered from placenta previa. I lent money to her and took her to Sinnar hospital. She couldn’t ask for [support] from community members because the pregnancy of unmarried women is not socially acceptable.
I am faced with a problem when I advise mothers to be referred. In about half of the cases in which I recommend referral, relatives of the mothers reject my advice and delay their referral which means that I need to convince them repeatedly. Some people do not understand the necessity of referral. There are misunderstandings about referrals among community members. They think that when a mother is referred, she will have to have a C-section and that this will be very costly. (VMW in Abu Hujar locality)
Most reasons cited by VMWs who felt referral was now easier were to do with increased awareness among the community and improved infrastructure, namely improvement in the availability of transportation, ambulances and staff at health posts or health centers.
As shown in Figure 2, more VMWs were involved in decision-making about where the birth would take place than husbands or other medical professionals. The endline survey showed 25.8% of community women said that their community VMW was the main decision-maker about the place of birth, which was notably higher than at baseline (3.1%).
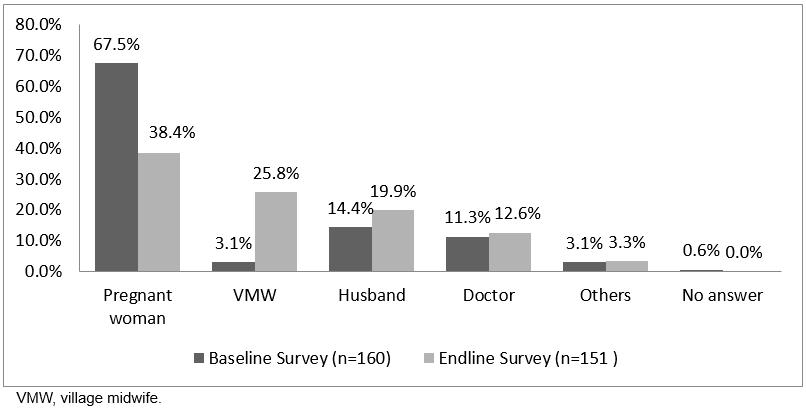 Figure 2: Decision-makers regarding place of birth.
Figure 2: Decision-makers regarding place of birth.
Improvement of supportive supervision and reporting
The findings indicated that the frequency of supervision provided by the Sinnar State Ministry of Health had increased over the study period. Occasionally, VMWs received supervision such as follow-up training (67%), periodic meetings at health facilities (40%) or when they were visited by their supervisors (29%). The main reasons VMWs gave for calling their supervisors were to seek advice regarding difficult/emergency cases (45%) and discuss or ask for assistance with monthly reports (35%). Supervision mainly took place at health facilities such as health centers (51%) or hospitals (49%). More than 80% of VMWs knew their supervisor’s contact number at endline, compared with 60% at baseline.
The presence of supervisors helps me a lot when I deal with emergency cases and decisions about referral. (VMW in Al-Abassiah village)
At endline, many more VMWs (81%) were recording information about deliveries using the national monthly reporting format provided by the Sinnar State Ministry of Health compared with at baseline (33%), which was mainly in notebooks or on pieces of paper. The report submission rate increased by 7% over the study period. Some VMWs reported that repeated instructions from their supervisors about how to compile the reports made it easier for them to follow the report format. The Sinnar State Ministry of Health follow-up training and more frequent periodic meetings at health facilities for VMWs was promoted as a part of the interventions.
The report format is easy to understand. Now I can even calculate percentages. (VMW in Wadanile village)
Enhanced mother–VMW relationships and community participation
At the time of the endline survey, VMWs reported that they felt it was easier to work in the community than it had been before because of increased awareness and respect towards VMWs among community members. Some VMWs mentioned that increased awareness and support from the community had contributed to improvement of their working situation. Improvement in their skills and knowledge may also have led to enhanced trust of VMWs by community members.
Mothers began to respect me and are satisfied with my performance now. That is why they follow my diagnosis. All of this is due to the increased awareness of healthcare among mothers. (VMW in Al Rigeeba village)
They [community members] trust our work and men ask us [VMWs] to give advice to their wives. (VMW in Wadanile village)
Now they [community members] support us [VMWs] more financially and have started paying for our work and appreciating our important role. (VMW in Wadanile village)
At endline, a higher proportion of VMWs were conducting activities to increase community awareness. Eleven VMWs ran community awareness activities in schools, 10 in public spaces and eight in health facilities. A greater proportion of VMWs were using health facilities for such activities at endline than at baseline, which might have contributed to strengthening linkages between facilities and VMWs. The main topics covered by VMWs in such activities were awareness of maternal health, followed by nutrition, health education and community emergency funds.
The majority of VMWs felt that their clinical skills (eg sterilisation techniques, blood pressure measurement and physical examination techniques) had improved after they received training. Increased knowledge, such as a better understanding of the referral system and improved self-efficacy, was also reported.
In-service training was a turning point in my life. I gained self-confidence. (VMW in Fagad village)
I gained knowledge and also a sense of responsibility from the training. (VMW in Al-Abassiah village)
Findings suggest that in-service training enhanced self-confidence and fostered a greater sense of responsibility in some VMWs, and produced changes in their work ethics and attitudes.
Discussion
There was a period when the WHO and many safe motherhood advocates encouraged TBA training, and so the number of TBA training programs increased in most developing countries in the 1970s13,14. However, in 1997 the WHO shifted its policy to promote training for SBAs, and TBAs were excluded from the definition of ‘skilled birth attendant’14,15. The effectiveness of TBA training remains controversial. Some authors have argued that the number of robust studies with adequate assessments to reveal true outcomes is limited15-17, whereas others18 argued that the emphasis on training SBAs is supported by theory, without non-causal data. Other studies claimed TBAs play an important role in the health of many mothers in countries where there is scarcity of SBAs and/or geographical and financial barriers14,15,19,20.
In Sinnar state, VMWs, sometimes considered to be trained TBAs, are the most important workforce for maternal care in rural communities, despite that fact that they do not meet the WHO criteria for SBAs. The results of the present survey indicate that the number of emergency referrals for mothers by VMWs increased at the endline because VMWs had more opportunity to gain knowledge and maintain their skills. More VMWs appear to have made proper judgements about when to refer emergency cases. VMWs were encouraged to hold community activities to raise awareness about health care to complement other social activities held in the community. Intervention efforts resulted in VMWs’ increased knowledge and enhanced self-efficacy to provide proper maternal healthcare services in their communities. The national policy of strengthening VMWs’ capacity to assist births at home, along with recommendations for primigravidas, multigravidas and pregnancies with complications to give birth at health facilities, may be a sustainable and realistic measure in the context of rural Sudan, where more than half of women choose to give birth at home. Throughout the intervention period, the local government promoted capacity building of VMWs and supervisors and with follow-up training through a strengthened supportive supervision system, which are considered to result in increased knowledge and self-efficacy.
A number of previous studies argued that trained TBAs without the support of skilled back-up services or networks outside the formal structure of the health system may not have significant effects on improved maternal care in the community21,22. Dietsch pointed out the importance of relationships between TBAs and SBAs that are based on mutual respect and collaborative practice to improve maternal service delivery in rural areas, yet many examples of abusive, disrespectful behaviour of SBAs towards TBAs are observed around the world23. A number of authors asserted that teams or continuous supervision have advantages over performance of community health workers for joint problem-solving, improved delivery of preventive health services and provision of consistent health education messages24-26. Benefits of teamwork have been discussed in many studies, including reinforcing individual capabilities, creating the feeling of participation and involvement, better decision-making and generating a diversity of ideas for a common purpose27,28.
The results revealed that the interventions, which included regular supervision and training for VMWs by health visitors/assistant health visitors, had a positive knock-on effect of cultivating mutual relationships between health visitors/assistant health visitors and VMWs, and community promotion activities provided by VMWs. Sinnar health facilities became a hub for health workers (including VMWs) to exchange and gain information on various occasions. VMWs are considered an integral part of the formal obstetric healthcare system in Sudan and receive regular supervision from healthcare professionals such as health visitors/assistant health visitors who work as their superiors and as a team in their assigned areas. Health facility staff had become a part of the team within each community, bridging VMWs, health visitors/assistant health visitors and community members, and conveying vital messages to the communities.
This study indicated that, through interventions, VMWs had been encouraged by their supervisors to hold (and they actually did hold) more community activities to encourage women to receive ANC at health centers or recommend facility births. This led to enhanced linkages between VMWs, the community and health facilities. VMWs provided knowledge and maternal care services close to mothers and communities, and almost all the interviewed women reported an increased level of respect towards VMWs. This enhanced trust might be attributable to the improvement in VMWs’ skills and knowledge but also to these community activities. Training for VMWs also appears to have contributed to increased respect for and recognition of the improved work of VMWs, enabling them to convince women to attend health facilities in a timely manner at a times of emergency, and to ultimately save lives of mothers and newborns in communities.
Walraven and Weeks5 stated that maternal healthcare providers need to have the trust and respect of the community to provide services. A previous study reported that some healthcare providers from outside community occasionally felt fear during home visits29. Kok et al30 argued that trust and respect from the community can be major factors contributing to the success of training of community health workers and enhancing their motivation. The UN Population Fund31 stated that mutual trust between midwives and the community is important for the provision of midwifery services in the community, and that midwives who do not belong to the community sometimes do not gain trust from clients. In some low-income countries, retention in rural or remote areas is challenging because SBAs often move to urban areas seeking higher payment, better living conditions and cultural familiarity32. Afghanistan’s midwifery model recruited candidates from communities where they would eventually be deployed, which may be a central to ensuring a high retention rate2. In Sudan, midwifery school candidates are usually recruited from their hometown, and eventually return to their community and are more easily accepted by that community, which results in retention of VMWs in communities and aids mutual trust between VMWs and community members.
This study had some limitations. First, the community women selected as participants for the baseline and endline surveys were not identical, which raises questions of reliability. Although the two groups of community women in the baseline and endline surveys are similar, it is possible that the changes may be partially due to the interventions as well as minor differences between the two groups. In addition, the sampled VMWs were not fully representative of all VMWs in Sinnar; therefore, the findings cannot be generalized to all VMWs in Sinnar or Sudan as a whole. It is also uncertain if the observed improvement will be translated into a lower maternal mortality ratio. Future studies and quantitative analyses are required to confirm whether improved skills and work conditions of VMWs positively affect maternal mortality.
Conclusions
Issues of shortage and retention of healthcare providers are continuous challenges in many rural areas in developing countries. Maternal care provided by SBAs at health facilities is recommended by international donor communities. Important implications from the authors’ experience in a resource-scarce area of Sudan are that some positive effects and changes have been observed in the quality of maternal care being provided by trained VMWs as frontline healthcare providers. Regular and adequate supervision and follow-up within a supervision system embodied by local government improved community participation and communication among VMWs and mothers, improved VMWs’ skills and knowledge and resulted in enhanced trust in communities. This has enabled and ensured more sustainable maternal and newborn health services. The findings of this study may inform other countries around the world facing similar challenging situations regarding the promotion of maternal and newborn health.
Acknowledgements
The project received funding from the Japan International Cooperation Agency under the Technical Assistance Scheme.The authors thank the Sinnar State Ministry of Health and participants who kindly provided their time and insights for their involvement in this survey. They gratefully acknowledge the Japan International Cooperation Agency who supported the Frontline Maternal and Child Health Empowerment Project.
