Background
The difficulty of attracting and keeping allied health personnel in rural Australia has been well established1. Recruitment and retention of these workers is notoriously problematic, particularly in areas removed from metropolitan areas such as the south west of Victoria. Staff turnover rates are high and there is evidence to suggest that this can be attributed to a range of factors, some of which are harder to control than others. The shortage of allied health professionals has been recognised by political leaders as a high priority, requiring effective strategies to improve the stability of this workforce2. In addition, there will be a continued and increasing demand for allied health practitioners due to reasons such as ageing populations3, increased physical inactivity and the associated chronic disease burden4, and effectiveness of allied health interventions within the healthcare system5
Effective allied health recruitment and retention strategies must allow for projected changes in key characteristics of the professions6 and changes in (preventive, curative) healthcare demands in communities5. Health service delivery is likely to be enhanced when skills of allied health professions are used to their full potential. Allied health professionals are well equipped to be involved in cost-effective and evidence-based intervention of a range of chronic diseases and activities such as health promotion5. Despite the higher levels of need for allied health services in rural areas7, Australians in metropolitan areas receive more than double the level of service provision by allied health professionals such as physiotherapists, podiatrists, occupational therapists, and social workers8-10.
Demographic results of a survey in South West Victoria showed that the allied health workforce is an older workforce that values multi-disciplinary teams11. This is in line with other Australian rural and remote allied health surveys12,13. South west Victorian services are predominantly delivered from public agencies that run regional services for more than one location. Professionals are highly qualified. The three most important reasons for remaining in their current position are: lifestyle, career and family ties, whereas the three main reasons for leaving are: lack of career path, personal and social isolation11,14,15. Based on these south west Victorian findings it is important to focus on enhancing allied health workforce retention from the outset in order to ensure that fewer professionals will be lost in future.
Recruitment and retention of allied health professionals is a complex interplay between personal, environmental, and work related factors16. A recent major allied health survey found that many practitioners leave rural practice due to personal factors17. Some of the problems are more difficult to address than others, for instance, it can be hard to find suitable rural work for a spouse or to cater for specific educational needs for some of the children of allied health professionals. Retention problems in allied health have been associated with organisational commitment and management in a number of studies13,18-27. Lack of career structure, input in decision-making, job autonomy, time management, organisational and professional support, and poor job satisfaction can compromise personal needs and intention to stay28. Conversely, allied health professionals and their managers can be trained to enhance team management skills such as respecting and negotiating. Although other retention factors have been identified (eg remuneration, workload, lack of task variety, lack of opportunities for partners, lack of social and cultural infrastructure, communication, distance and transport, educational needs for children)12,16,21,28,29, they can at least in part be addressed by effective management and community support30-32.
The Allied Health Workforce Enhancement Project of the Greater Green Triangle University Department of Rural Health (GGT UDRH) aims to increase the number of practicing allied health professionals in the Barwon South West and Wimmera regions, and their length of stay. The project is funded by the Victorian Department of Human Services and tasks include the design, implementation and testing of an evidence-based recruitment and retention model of allied health professionals. Allied health professionals have been defined as university trained health professionals, other than nurses and medical practitioners, who are involved in direct patient care or services to the community, or both33.
Generational challenges in the recruitment and retention of rural professionals
Many young allied health graduates seek rural positions to start their career, and, as a result, rural regions have been described as 'professional nurseries' 12. Unfortunately, many graduates leave or intend to leave their rural positions11,29.
Workforce trends have been noted in the different age groups of workers. Generation X is the term used to refer to those born between 1961 (or 1965) and 1981 (or 1980)34,35, whereas Generation Y is born after that date. Trends noted with Generation Y include wanting to work in a team environment36, Generation X wants to be mobile and flexible, whereas baby-boomers plan to retire12. Generation X has been described as being empowered, self-directed, techno-competent, flexible, and wanting to change jobs more frequently when dissatisfied with work conditions34. Generation Y are described as team workers36. These findings challenge existing recruitment and retention practices and are likely to have ramifications in relation to management and forward planning of rural workforce requirements37.
For the purpose of allied health rural workforce enhancement, it is useful to focus on factors that attract and keep those who elect to be in the country rather than limiting oneself to putting all the effort in recruiting young graduates from the city. For instance, many physiotherapy students reared and educated in bigger cities are not interested in entering rural practice largely due to social reasons (family, friends and entertainment), long distance travel and perceived cost of living38. Important factors for working in rural areas are rural connectedness, lifestyle, clean environment, adventure, inexpensive accommodation and professional independence38. Surveys among rural dieticians23, new physiotherapy graduates39 and nurses22 confirmed these results, in addition to wanting job opportunity and satisfaction, a desire to be exposed to a variety of work experiences, and to be a valued member of a team. On the downside, factors such as lack of funding for clinical education is inhibiting students to look for rural placements40 due to travel and paying for double accommodation during a period of rural placement. Many rural students have financial problems41. After graduation and spending most of the time in the city, even students who originate from rural areas are not always interested in returning to the country42.
A conceptual model for recruitment and retention
The proposed recruitment and retention model is multidimensional and based on balancing needs and responsibilities of health professionals (including those that pertain to family, profession, peers, career and income), agencies they work for (including the legislative municipal, state and federal entities that affect these organisations), and communities they service (individuals as well as groups in the society that use their services or that support them financially) (Fig 1). Other conceptual models have been described in the health workforce recruitment and retention literature. For example, Crandall and colleagues43 described four types of models, namely: (i) affinity models (recruitment of rural students into training programs and promoting rural practice); (ii) economic incentive models (financial incentives that support rural practice); (iii) practice characteristics models (technical and collegial support); and (iv) indenture models (recruitment of fixed-term providers through scholarships and other incentives). Although the models are simple, describe concrete mechanisms and contain important elements that pertain to some of the needs and responsibilities within each of the three domains (ie, individual, organisational and community needs), they have been designed for one discipline (ie, medical practice) and do not sufficiently recognise needs of other disciplines. It can be argued that for models to be sustainable, needs and responsibilities within each of the three domains (Figs 2-4) need to be recognised and respected.
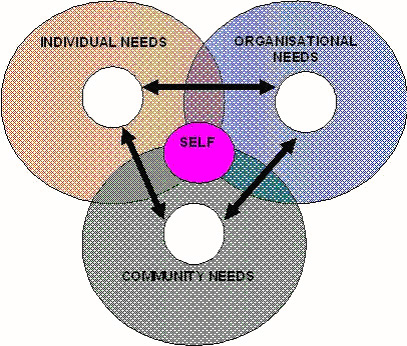
Figure 1: A multidimensional interactive allied health workforce recruitment and retention conceptual model.
The interactive and symbiotic relationships between the needs and responsibilities in these three different domains is dynamic and partially based on Glasser's choice theory and lead management principles44, and Covey's circles of 'concern' and 'influence'45. The model is in line with results from studies by Cheers and Lonne that used narratives46. The many issues that concern each of the groups is represented by the outer circles, whereas what can be influenced by the entities within each of the domains is represented by their respective inner circles. People have the freedom to choose the manner in which they want to respond (response-ability), and Covey45 made a distinction between reactive response patterns (eg 'I can't') and proactive ones (eg 'I choose') whereas Glasser47 made a distinction between deadly habits (eg blaming) and caring habits (eg encouraging). Positive attitudes and responsible actions in each of the domains are likely to enlarge their inner circles of influence. In this sense responsibility is defined by Glasser48 as 'the ability to fulfil one's needs, and to do so in a way that does not deprive others of the ability to fulfil their needs'.
Figs 2-4 show factors within each of the three domains of this conceptual model that can be changed by members of that group with relatively little effort (printed in purple) and those that are more challenging to address (printed in black). It is reasonable to assume that when perceived needs and what is received in reality are comparable, frustration levels are low44 and retention is enhanced. This is confirmed by results of a recent allied health survey that showed that 45% of professionals who felt supported in their job intended to stay for more than 2 years, whereas those who were not supported were less likely to stay and recommend their position to others15,49. This means that retention and recruitment issues are likely to be interrelated and that attention needs to be given to both for a workforce enhancement program to be effective. This may also be applicable to other trades and university student recruitment50. The following is a detailed explanation of the three components of the conceptual model.
Individual needs and responsibilities
The various needs and wants individual practitioners and their families have51 need to be recognised when enhancing rural recruitment and retention46. Needs are similar for everyone48,52,53, although they may differ in intensity. In contrast, 'wants' are personal to the individual54,55. The basic needs are the need for survival, power, fun, belonging and freedom55, and translate to issues such as isolation and peer contact, remuneration, job responsibility, team spirit, autonomy. The higher needs are the need for self-actualisation56, inner-vision and inner-divinity57. It is possible that in fulfilling higher needs people's behaviours are more flexible and effective, and work environments are more pleasant than in situations where people have to struggle to fulfil their external necessities to live.
The hierarchy of needs Maslow postulated in the 1950s and 60s was a break from existing schools at the time, that is psycho-analysis (eg Freud, Jung) and behaviourism (eg Watson, Skinner). In essence, in the humanistic view of Maslow human behaviour is not seen as being solely dependent on the unconscious mind, instincts or a learnt set of actions, but rather on the fulfilment of needs52-54. According to Maslow, needs at the lower end of the scale need to be alleviated first (ie, physiology, safety, love, esteem) before the higher need for self-actualisation can be filled. The need for esteem has two aspects: (i) self-esteem due to the ability of performing certain tasks; and (ii) the positive interest and acknowledgment from peers and others that comes with it. The need for self-actualisation has been defined by Gwynne56 as 'the desire to become more and more what one is, to become everything that one is capable of becoming'. The order of Maslow's needs and the exact definition of them is not necessarily based on precise research data and in this sense these proposed needs are not unlike those suggested by Glasser55.
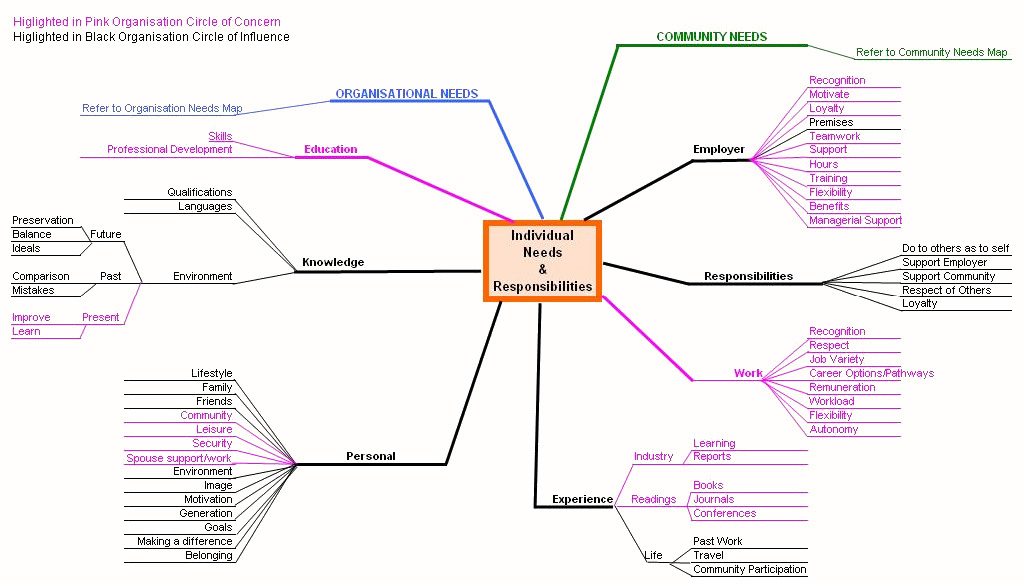
Figure 2: Needs and responsibilities of the individual
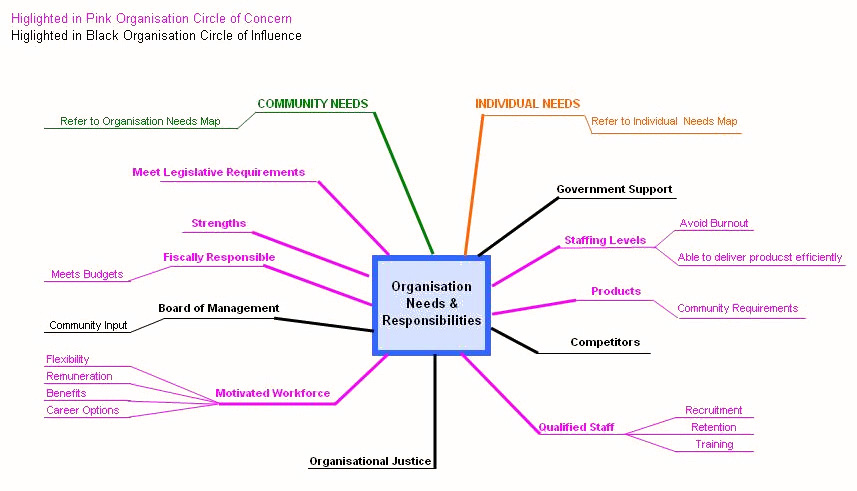
Figure 3: Needs and responsibilities of the organisation
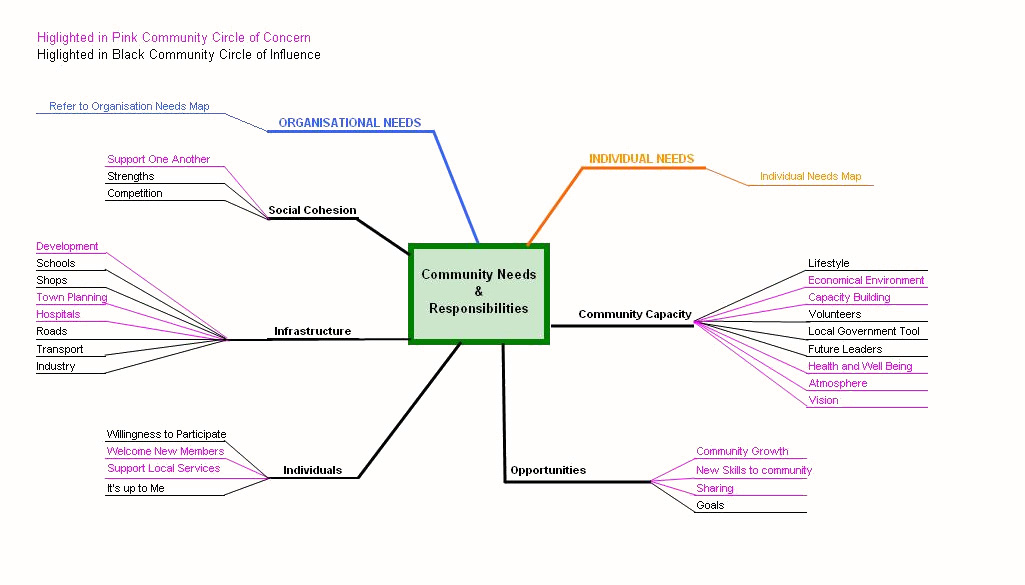
Figure 4: Needs and responsibilities of the community
A recent survey among allied health practitioners in south west Victoria showed that they preferred teamwork15. Teamwork was associated with the intention to stay in their positions. In choice theory, lead managers assist their team members in helping themselves to fulfil their present needs by making responsible choices44. The desire to minimise the difference between what people want to have (based on what their perceived quality world) and what they perceive to have in reality drives them to action. The person who uses internal control methods58 is likely to apply the following behavioural patterns:
- has a win-win method of dealing with problems
- will investigate to appreciate a particular problem
- recognises the needs of others
- fosters confidence in others
- recognises the input of others
- accept others for who and what they are
- looks at the present situation as well as ahead
- will ask rather than demand
- will communicate and depends on cooperation
- is concerned with others and does not use them
- gets on with the job without blaming others.
Although well meant, existing and newly proposed models of healthcare management such as that for the enhancement of recruitment and retention of medical practitioners31 do not necessarily cater for the individual needs of other health professionals. Current evidence-based practices in health care require input from more than one discipline, particularly in the prevention and treatment of chronic diseases5,59. This has ramifications for rural health care where clients are generally older, have more chronic diseases than their metropolitan counterparts, and are less likely to be eligible for rebates of the private sector60. Teams operating from rural health agencies may therefore include expert professionals and assistants from a range of disciplines that have common purpose and goal performance, possess complimentary skills and keep themselves mutually accountable61.
For a team to function effectively there must be a motive for operating together, an awareness that joint input is more effective than working alone, a dependence for members on each other to attain the agreed goal, joint accountability within an organisation or community, and leadership62-64. Functioning in a team requires professionals to trust and respect each other, to remain flexible, to accept program protocols, to understand the procedures, to take part in team development, and to be able to let go or accept particular roles64,65. This is particularly relevant when client-focused teamwork progresses from multidisciplinary (separate disciplinary treatment plans) to interdisciplinary (shared plan and monitoring of progress) or even transdisciplinary (crossing professional boundaries) modes of service delivery, particularly in small rural organisations that have limited resources. The latter mode requires integration, collective thinking and the highest degree of trust, and even blurring of professional boundaries66.
Allied health professionals need a range of competencies to manage their clinical work, to be a team player or to give direction to a team, to function as a member of a multidisciplinary organisation, and to represent clients, the profession or organisation. Lincoln, Adamson and Cant67 grouped managerial competencies in seven different domains, namely: organisational practices, legislative knowledge, staff relations management, management of future planning, negotiating skills, managing funding, and team leadership skills.
New graduates may feel that they lack competence in different areas through lack of experience, contacts and/or knowledge68-70. Consequently, they may feel less secure in their positions, particularly when they are required to work as a sole practitioner. The shock after starting a career in rural practice can have a profound impact on the individual professional68,71,72 and their intention to stay. Providing the required information and support (eg education, professional network, and management) is likely to assist retention of allied health practitioners in rural settings28. Unfortunately, allied health professionals are not always well supported and included in the communication networks. For example, there is evidence that professionals from diverse backgrounds are less likely to be included in formal and informal information networks and decision-making processes within organisations73. A supportive and anti-discriminative work environment can assist in filling personal needs people have and could enhance retention of the younger recruits in rural allied health professions.
Organisational needs and responsibilities
Health organisations and their workers are generally expected to respond to health needs in their communities in an effective and efficient manner. The availability of human resources (ie, younger workers), competence and a healthy work environment are important factors that assist optimal long-term outcomes for all stakeholders74. Organisations need to deal with workforce changes and have the responsibility to create a stimulating and supportive environment in which employees can be innovative, productive and learn2. A recent Mercer's workforce survey in Australia found that employees who are in open communication with management are more likely to be committed to the organisation, whereas those who do not receive sufficient support (ie, training) are more likely to leave75.
Costs associated with the recruitment of staff for rural health agencies services can be high76. There can be a potential conflict between managers who are under increasing pressure to control costs and professionals who are expected to deliver up-to-date evidence-based practice, and who may have a need to advance in their profession77. Collins et al.20 found that career progression in allied health professionals and nurses was associated with enhanced job satisfaction, whereas low job satisfaction was associated with intention to leave the profession. Recognition for performance and creativity of counsellors has been related with organisational commitment and intention to stay, and job autonomy was found to be directly related to intention to stay24. Keeping valuable employees of any discipline by facilitating career paths is an important issue78, although may require creative management.
A holistic workforce recruitment and retention model should balance the needs of all parties involved and deliver services in an effective, efficient and fair manner (ie, organisational justice). This includes utilising allied health assistants79 and disciplines such as exercise scientists to improve health services in an ageing society and enhance allied health workforce retention through interdisciplinary teamwork, improving career options and preventing professional burnout80-84. Although it can be useful to highlight individual and group interests, satisfactory workforce planning is unlikely to be served by preferential treatment of professions over the interests of health agencies, communities, or of one profession over the other. Challenges for organisations include the development of alternative management models77, teaching professionals specific managerial competencies67, and inviting their workers and other members of the community to take more responsibility for their own needs and that of new staff/community members30,31,85.
Community needs and responsibilities
Communities can be defined as groups of people with diverse characteristics who are linked by social ties, share common perspectives, and engage in joint action in geographical locations or setting86. The needs of communities can change over time and depend on factors such as population growth, movement and age. For example, the population age-mix of communities in south west Victoria is predicted to change dramatically over the next 25 years in favour of those who are 60 years of age or older87 (Fig 5). In addition, coastal towns, particularly Warrnambool, are predicted to expand in comparison with towns in other parts of the region87 (Fig 6). These factors together will have ramifications for the number of allied health professionals needed to improve and maintain services to larger and ageing communities of south west Victoria, for example, podiatrists.
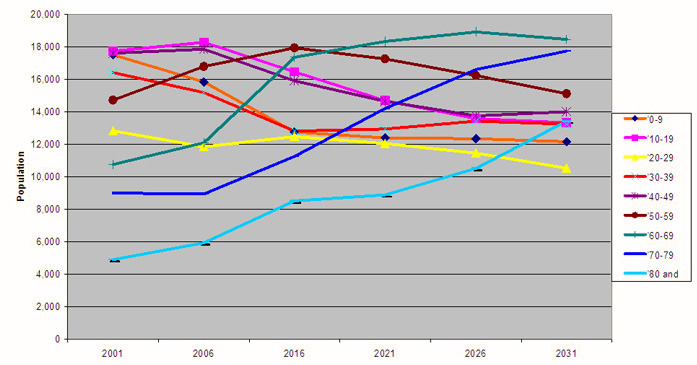
Figure 5: Projected population age-mix for South West Victoria, based on data from the Victorian Department of Sustainability and Environment87.
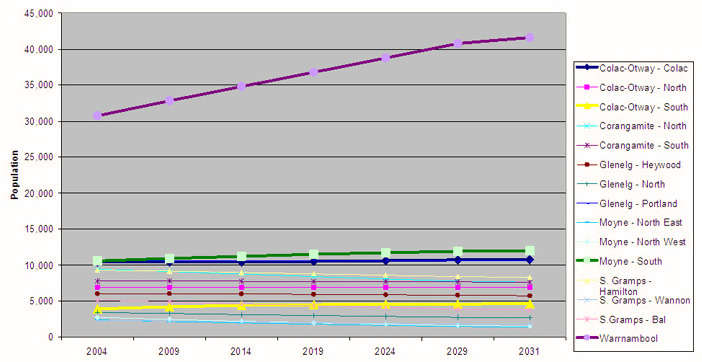
Figure 6: Projected population growth of communities in South West Victoria, based on data from the Victorian Department of Sustainability and Environment87.
Given the predicted population changes and current shortage of allied health professionals in the south west of Victoria, particularly in areas of physiotherapy, occupational therapy and podiatry, communities require organisations that: (i) address the changing needs in the community effectively and efficiently; and (ii) provide employment for its members. One of the challenges for communities, organisations and employees is to adjust to increasing change. This requires flexibility and particularly 'quality input' on behalf of the community members88. Teamwork through constructive partnerships between members of communities, organisations and various levels of government can be very effective in achieving a satisfying balance between the immediate and future needs of communities, and their organisations and workers.
Evidence shows that active and dynamic communities reach better outcomes in areas such as health, education and economic development2 by 'doing it for themselves'74(p.16). In addition, active and supportive communities keep their allied health professionals for longer periods of time than less supportive communities. An Alaskan study found that allied health workers in places with low attrition rates were more likely to feel respected and supported by the community28.
Implementation and evaluation of the recruitment and retention concept
Successful performance of the allied health recruitment and retention concept requires the design, implementation, evaluation and adjustment of sets of actions that lead to optimising workforce outcomes for each of the communities or health agencies in the south west of Victoria as a part of an ongoing process (Fig 7). Factors that may affect recruitment and retention outcomes and health service delivery could include marketing strategies, size and location of the community, type of health agency, demand for particular disciplines, interdisciplinary teams that utilise trained allied health assistants to enhance quality and quantity of service delivery and that reduce workload, and availability of recruits from particular generations.
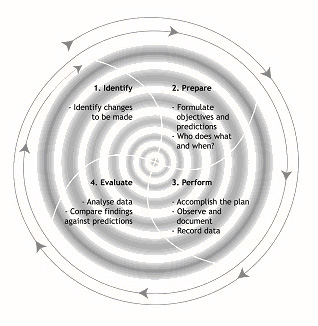
Figure 7: A model for the enhancement of health recruitment and retention, based on Langley, Nolan and Nolan89
Recruitment is enhanced by effective and efficient marketing strategies, and there is a need for human resource administrators to constantly evaluate and improve the outcomes of these90. An Alaskan study found that the three most effective methods across the different health agencies were websites (28%), word of mouth (26%) and newspapers (16%)76. Given the cost of recruiting staff and advertising in newspapers, it can be attractive for organisations to optimise staff retention by assisting in satisfying basic needs of individuals and their communities since Alaskan workers were found to be very effective in bringing in new recruits. The three least effective recruitment strategies were newspaper advertisements (32%), websites (15%) and journals (13%). Reasons given for the ineffectiveness of newspapers included 'dismal return on investment', 'indiscriminate ads are not useful' and 'not appropriate enquiries'76. Likewise, websites were found to be ineffective when they were not well targeted. Also, websites (including Government sites) can be extremely user-unfriendly.
Program initiatives so far address issues in all three domains of the conceptual model for workforce recruitment and retention in south west Victoria. They include:
- exit interviews to find out why professionals left
- working together with organisations on evidence-based recruitment
- cost-benefit analysis of promoting a professional to a Grade 2 position versus recruiting and training a person for a Grade 1 position
- promoting new models of care (eg interprofessional, teamwork, assistants, teleconsultation) and locum services to prevent professional burnout
- providing continuous professional development (CPD) based on professional group needs and adult learning principles91 and flexible delivery92
- preceptorship training to boost the quantity and quality of student placement (eg through problem-based learning93), and to improve work enjoyment of the preceptors94
- delivering population health seminars and cultural awareness training for professionals and students to increase awareness of rural health issues, and to promote interdisciplinary practice95,96
- orientation program for students and linking them with local groups in the community
- involving the community in projects and providing information on workforce and health service developments.
Preliminary findings suggest reduced staff turnover, reduced number of vacancies, high levels of satisfaction with CPD, and a positive effect of CPD on clinical skills and the number of patients seeking treatment.
Conclusion
It is essential to target the younger professionals and those with young families to become part of the rural workforce in south west Victoria. The projected growth of coastal towns, the ageing populations, and an ageing allied health workforce require strategic action and evaluation of evidence-based practices that include alternative ways of service delivery to provide for future needs. At the same time, one needs to take into account preferences of the younger workers. The provision of a supportive work environment, flexible working hours, and opportunities for work exchange to gain experience or to move into private practice should be catered for. Recruitment and retention of the allied health workforce is likely to improve with a set of actions that include: the provision of CPD and work exchange opportunities, teaching managerial competencies, utilising the various disciplines and allied health assistants, enhancing student placement, creating a supportive and creative work environment, and having an active and supportive community. Recruitment is likely to be enhanced when retention is optimal, because workers are willing to recommend their workplace. Last, in marketing vacancies, it is essential to use evidence-based strategies in line with the preferred forms of communication by the different generations (Baby Boomers, X and Y).
Although preliminary findings suggest reduced staff turnover, reduced number of vacancies, high levels of satisfaction with CPD, and a positive effect of CPD on clinical skills and the number of patients seeking treatment, more research is needed to test the utility of the conceptual model. The long-term approach to evaluating the utility of the model will be focussed on the three domains. For the individual domain, methods will include focus groups and semi-structured interviews including: continual data collection on exit interviews and the impact of CPD training; and a survey of allied health workforce needs in 2008. The latter will be a follow-up survey and compare results of the 2008 survey with the 2003 survey. For the organisation domain, methods will include a survey of organisations with regards to management style, staff management, and remuneration packages within the organisation. For the community domain, analysis will be made of health and professional organisations, number of support groups, and community initiatives. Data will be wide ranging and include newspaper articles, to demographic profiles of a community, to mapping of infrastructure within a community.
Acknowledgement
The project was funded by the Department of Human Services, Victoria.
References
1. Best J. Rural Health Stocktake Advisory Paper. Canberra: Commonwealth Department of Health and Aged Care, 2000.
2. Thwaites J. Victorian community building initiative. Victorian Goverment. (Online) 2004. Available:
www.communitybuilding.vic.gov.au (Accessed 9 December 2004).
3. Coory MD. Ageing and healthcare costs in Australia: A case of policy-based evidence. Medical Journal of Australia 2004; 180: 581-583.
4. Bauman A. Health benefits of physical activity for older adults - epidemiological approaches to the evidence. In: ME Morris, AMM Schoo (Eds). Optimizing exercise and physical activity in older people. Edinburgh: Butterworth Heinemann, 2004.
5. Segal L, Robertson I. Allied health services planning framework for chronic diseases. Melbourne: Monash University, 2003.
6. Selby-Smith C, Crowley S. Labor force planning for allied health in Australia. Journal of Allied Health 1995; 24: 249-265.
7. Strong K, Trickett P, Titulaer I, Bhatia K. Health in rural and remote Australia. Canberra: Australian Institute of Health and Welfare, 1998.
8. O'Kane A, Curry B. Unveiling the secrets of the rural and remote allied health workforce. In: Proceedings, 7th National Rural Health Conference, Hobart, Australia, 1-4 March 2003.
9. Causby RS. Facilitating recruitment of podiatrists to rural health in South Australia through a joint academic-clinical appointment. Rural & Remote Health 3: 165. (Online) 2003. Available: http://rrh.org.au (Accessed 20 December 2003).
10. Lannin N, Longland S. Critical shortage of occupational therapists in rural Australia: Changing our long-held beliefs provides a solution. Australian Occupational Therapy Journal 2003; 50: 184-187.
11. Stagnitti K, Reid C. Allied health workforce survey of the Barwon South West region of Victoria. Warrnambool: Greater Green Triangle University Department of Rural Health, 2004.
12. Miles RL, Marshall C, Rolfe J, Noonan S. The attraction and retention of professionals to regional areas. Queensland Health Report. Brisbane: Queensland Government, 2004.
13. SARRAH. A study of allied health professionals in rural and remote Australia. Canberra: Services for Australian Rural & Remote Allied Health, 2000.
14. Stagnitti K, Schoo A, Reid C, Dunbar J. Access and attitude of rural allied health professionals to CPD and training. International Journal of Therapy and Rehabilitation 2005; 12: 355-361.
15. Stagnitti K, Schoo A, Reid C, Dunbar J. Retention of allied health professionals in the south west of Victoria. Australian Journal of Rural Health 2005; 13: 364-365.
16. Mills A, Millsteed J. Retention: an unresolved workforce issue affecting rural occupational therapy services. Australian Occupational Therapy Journal 2002; 49: 170-181.
17. Belcher S, Kealey J, Jones J, Humphreys J. The VURHC Rural Allied Health Professionals Recruitment and Retention Study. Melbourne: VURHC, 2005.
18. Akroyd D, Mulkey W, Utley-Smith Q. The impact of work rewards on radiographers' organizational commitment. Radiology Management 1995; 17: 51-56.
19. Broom JP, Williams J. Occupational stress and neurological rehabilitation physiotherapists. Physiotherapy 1996; 82: 606-614.
20. Collins K, Jones ML, McDonnell A, Read S, Jones R, Cameron A. Do new roles contribute to job satisfaction and retention of staff in nursing and professions allied to medicine? Journal of Nursing Management 2000; 8: 3-12.
21. Denham LA, Shaddock AJ. Recruitment and retention of rural allied health professionals in developmental disability services in New South Wales. Australian Journal of Rural Health 2004; 12: 28-29.
22. Hegney D, McCarthy A, Rogers-Clark C, Gorman D. Why nurses are attracted to rural and remote practice. Australian Journal of Rural Health 2002; 10: 178-186.
23. Hughes R. An omnibus survey of the Australian rural health dietetic workforce. Australian Journal of Nutrition & Dietetics 1998; 55: 163-169.
24. Knudsen HK, Johnson JA, Roman PM. Retaining counseling staff at substance abuse treatment centers: effects of management practices. Journal of Substance Abuse Treatment 2003; 24: 129-135.
25. Kraeger MM, Walker KF. Attrition, burnout, job dissatisfaction and occupational therapy managers. Occupational Therapy in Health Care 1993; 8: 47-62.
26. Rachman R. Hospital social work and community care: the practitioner's view. Social Work in Health Care 1997; 25: 211-222.
27. Thornton M, Melis EH, Pham B. Development, implementation and results of a survey to identify factors affecting motivation in an acute care
physiotherapy setting. Physiotherapy Canada 1999; 51: 251-258.
28. US Department of Health and Human Services. Factors influencing retention and attrition of Alaska community health aides/practitioners: A qualitative study. Washington: US Department of Health and Human Services, February 2004.
29. Millsteed J. Factors affecting the retention of occupational therapists in rural services. Occupational Therapy in Health Care 2001; 14: 55-72.
30. Veitch C, Grant M. Community involvement in medical practitioner recruitment and retention: Reflections on experience. Rural & Remote Health 4: 261. (Online) 2004. Available: http://rrh.org.au (Accessed 20 December 2005).
31. Worley PS. Good health to rural communities? Rural & Remote Health 4: 292. (Online) 2004. Available: http://rrh.org.au (Accessed 20 December 2005).
32. Battye KM, McTaggart K. Development of a model for sustainable delivery of outreach allied health services to remote north-west Queensland, Australia. Rural & Remote Health 3: 194. (Online) 2003. Available: http://rrh.org.au (Accessed 20 December 2005).
33. Hodgson L, Berry A. Rural practice and allied health: The establishment of an identity. Brisbane: Queensland Health, 1993.
34. Kupperschmidt BR. Kupperschmidt BR. Understanding generation X employees. Journal of Nursing Administration 1998; 28: 36-42.
35. Hill KS. Defy the decades with mulitgenerational teams. Nursing Management 2002; 35: 32-35.
36. McKenna TC. The New Management Challenge. Proceedings, American Organisation of Nurse Executives. 29 March-2 April 2003; New Orleans, USA.
37. Spin Communications and Sweeney Research. The definitve lifestyle guide to 16-28 year olds in Australia. Melbourne: Spin Sweeney Report, 2004.
38. Mitchell R. Perceived inhibitors to rural practice among physiotherapy students. Australian Journal of Physiotherapy 1996; 42: 47-52.
39. Hoekstra B. Rural employment: attitudes and perceptions of allied health students and graduates. Melbourne: School of Physiotherapy, University of Melbourne, 2002.
40. Health Professions Council of Australia. Solving the crisis in clinical education for Australia's health professions. Melbourne: Health Professions Council of Australia, July 2004.
41. Durkin SR, Bascomb A, Turnbull D, Marley J. Rural origin medical students: how do they cope with the medical school environment? Australian Journal of Rural Health 2003; 11: 89-95.
42. Stewart SR, Pool JB, Winn J. Factors in recruitment and employment of allied health students: preliminary findings. Journal of Allied Health 2002; 31: 111-116.
43. Crandall LA, Dwyer JW, Duncan RP. Recruitment and retention of rural physicians: Issues for the 1990s. Journal of Rural Health 1990; 6: 19-38.
44. Glasser W. The control theory manager. New York: HarperCollins, 1994.
45. Covey S. The 7 habits of highly effective people. Melbourne: The Business Library, 1998.
46. Cheers B. The place of care - Rural human services on the fringe. Available: http://www.stthomasu.ca/academic/scwk/rural/cheers.htm (Accessed 15 November 2005).
47. Glasser W. Reality therapy II. New york: Harper Collins, 2000.
48. Glasser W. Reality therapy. A new approach to psychiatry. New York: Harper Colophon, 1975.
49. Schoo A, Stagnitti K, Reid C, Dunbar J. Allied health professionals in South West Victoria: An exploration of issues of management and intention to stay. Journal of Allied Health 2006; (in press).
50. Seidman A. Recruitment begins with retention: Retention begins with recruitment. Colleage: State University of New York, 1989.
51. Veitch C, Crossland LJ. Medical family support needs and experiences in rural Queensland. Rural & Remote Health 5: 467. 2005 (Online). Available: http://rrh.org.au (Accessed 20 December 2005).
52. Maslow AH. Toward a psychology of being. New York: Van Nostrand, 1968.
53. Maslow AH. The farther reaches of human nature. New York: Viking, 1971.
54. Maslow AH. Motivation and personality. 2nd edn. New York: Harper & Row, 1970.
55. Glasser W. Warning: psychiatry can be hazardous to your mental health. New York: HarperCollins, 2003.
56. Vanier College. Abraham Maslow. Available: http://ddmt.vaniercollege.qc.ca/~s0330431/ece/abraham_m.htm (Accessed 22 December 2005).
57. Schoo AMM. Reality therapy and the human energy field: working with needs that influence mind and body. International Journal of Reality Therapy 2005; 24: 15-22.
58. Devine D. Intensive training week [basic] in choice theory, reality therapy, lead management. December edn. Sydney: The William Glasser Institute, Australia; 2001.
59. Commonwealth Department of Health and Ageing. The Australian coordinated care trials: Final technical national evaluation report on the first round of trials. Canberra: AusInfo; 2001.
60. Grimmer K, Bowman P. Differences between metropolitan and country public hospital allied health services. Australian Journal of Rural Health 1998; 6: 181-188.
61. Katzenbach JR, Smith DK. The wisdom of teams. New York: Harper Business, 1993.
62. Reilly AJ, Jones JE. Team-building. The 1974 handbook for group facilitators. San Diego: University Associates, 1974.
63. Spencer PA, Coye RW. Project BRIDGE: A team approach to decision-making for early services. Infants and Young Children 1988; 1: 82-92.
64. Rush D, Shelden M. On becoming a team: A view from the field. Seminars in Speech and Language 1996; 17: 131-142.
65. Antoniadis A, Videlock JL. In search of teamwork: A transactional approach to team functioning. Infant-Todler Intervention: The Transdisciplinary Journal 1991; 1: 157-167.
66. Sands R, Angell B. Social workers as collaborators on interagency and interdisciplinary teams. In: K Bentley (Ed.). Social work practice in mental health: contemporary roles, tasks and techniques. Pacific Grove: Books/Cole/Thomson Learning, 2002.
67. Lincoln MA, Adamson BJ, Cant RV. The importance of managerial competencies for new graduates in speech pathology. Advances in Speech-Language Pathology 2001; 3: 25-36.
68. Tryssenaar J, Perkins J. From student to therapist: exploring the first year of practice. The American Journal of Occupational Therapy 2001; 55: 19-27.
69. Lee S, Mackenzie L. Starting out in rural New South Wales: the experiences of new graduate occupational therapists. Australian Journal of Rural Health 2003; 11: 36-43.
70. Steenbergen K, Mackenzie L. Professional support in rural New South Wales: perceptions of new graduate occupational therapists. Australian Journal of Rural Health 2004; 12: 160-165.
71. Zapf MK. Remote practice and culture shock: Social workers moving to isolated Northern regions. Social Work 1993; 38: 694-704.
72. Lonne R. Beginning country practice. Australian Social Work 1990; 43: 31-39.
73. Barak MEM. Beyond affirmative action: toward a model of diversity and organizational inclusion. Administration in Social Work 2000; 23: 47-68.
74. Bryden JM. Why do some rural economies 'do' better than others? Some results of the European research project on the Dynamics Of Rural Areas (Dora). Warrnambool, VIC: Deakin University, 2003; 1-32.
75. Mercer Human Resource Consulting. What's working: Mercer's survey of Australia at work. New York: Mercer Human Resource Consulting, 2004.
76. Department of Health and Social Services. Status of recruitment resources and strategies. Juneau, Alaska: Department of Health and Social Services, 2004.
77. Southon G. Health service structures, management and professional practice: Beyond clinical management. Australian Health Review 1996; 19: 2-16.
78. Dibble S. Keeping your valuable employees. New York: John Wiley, 1999.
79. Duckett SJ. Health workforce design for the 21st century. Australian Health Review 2005; 29: 201-210.
80. Balogun JA, Titiloye V, Balogun A, Oyeyemi A, Katz J. Prevalence and determinants of burnout among physical and occupational therapists. Journal of Allied Health 2002; 31: 131-139.
81. Mandy A, Rouse S. Burnout and work stress in junior physiotherapists. British Journal of Therapy & Rehabilitation 1997; 4: 597-598.
82. Ogiwara S, Hayashi H. Burnout amongst physiotherapists in Ishikawa Prefecture. Journal of Physical Therapy Science 2002; 14: 7-13.
83. Painter J, Akroyd D, Elliot S, Adams RD. Burnout among occupational therapists. Occupational Therapy in Health Care 2003; 17: 63-78.
84. Wandling BJ, Smith BS. Burnout in orthopaedic physical therapists. Journal of Orthopaedic & Sports Physical Therapy 1997; 26: 124-130.
85. Wallis S. Recruiting and retaining general practitioners in rural areas: A community resource manual for community capacity building. Ballarat, VIC: University of Ballarat, 2002.
86. MacQueen KM, McLellan E, Metzger DS et al. What is community? An evidence-based definition for participatory public health. American Journal of Public Health 2001; 91: 1929-1938.
87. O'Leary J. Victoria in future (VIF): 2004 projections, estimated resident population by 5 year age group and sex, statistical local areas. Melbourne: Department of Sustainability and Environment, July 2004.
88. Oscarsson B, Hammarström O, Karlsson G, Lindholm R. A new world of work; experiences from the Swedish development program on new technology, work organisation and management. No. 64-10-60. Stockholm: Swedish Work Environment Fund, January 1988.
89. Langley GJ, Nolan KM, Nolan TM. The foundation of improvement. Silver Spring, MD: API, 1992.
90. American Society for Healthcare Human Resources Administration, Society for Healthcare Strategy and Market Development. Building a framework for workforce solutions. Chicago, IL: American Hospital Association, 2001.
91. Spencer JA, Jordan RK. Learner centred approaches in medical education. BMJ 1999; 318: 1280-1283.
92. Hays R, Veitch J, Lam A. Teaching clinical pathology by flexible delivery in rural sites. Australian Journal of Rural Health 2005; 13: 232-235.
93. VanLeit B, Cubra J. Student-developed problem-based learning cases: Preparing for rural healthcare practice. Rural & Remote Health 5: 399. (Online) 2005. Available: http://rrh.org.au (Accessed 20 December 2005).
94. Walters LS, Worley PS, Prideaux D, Rolfe H, Keaney C. The impact of medical students on rural general practitioner preceptors. Rural & Remote Health 5: 403. (Online) 2005. Available: http://rrh.org.au (Accessed 20 December 2005).
95. Shannon CK, Baker H, Jackson J, Roy A, Heady H. Evaluation of a required statewide interdisciplinary rural health education program: student attitudes, career intends and perceived quality. Rural & Remote Health 5: 405. (Online) 2005. Available: http://rrh.org.au (Accessed 20 December 2005).
96. Liaw S-T, McGrath B, Jones G, Russell U, Bourke L, Hsu-Hage B. A compulsory experiential and interprofessional rural health subject for undergraduate students. Rural & Remote Health 5: 460. (Online) 2005. Available: http://rrh.org.au (Accessed 20 December 2005).



