Introduction
The New Zealand (NZ) healthcare system, as in other areas in the world, continues to have an undersupply of doctors in rural areas, especially in general practice1-3. In part, this shortage in NZ may be explained by a lower density of practising physicians overall – 2.2 per 1000 population compared to the OECD average of 3.1 – as well as approximately 80% of registered doctors working in urban areas, compared with 60% of the general population4,5. In 2005, a rural primary healthcare report recommended medical school provide places for those from a rural origin and to organise training in rural settings before the completion of medical school or soon thereafter6. These recommendations were based on evidence that the combination of rural background and curriculum experience improves the likelihood of medical graduates entering rural practice7-10.
From 2004, both NZ medical schools (at the universities of Auckland and Otago) introduced the Rural Origin Medical Preferential Entry initiative, with places allocated at each school to those who met academic as well as rural criteria. Rural criteria included the population size of the student’s home town (less than 20 000) and/or the student’s school years in a rural setting11. While the University of Otago has continued with the size of town being a determinant, criteria at the University of Auckland were altered in 2012 to become a regional–rural admission scheme12. This was in recognition of the higher population density in the northern part of NZ. Students from outside the boundaries of NZ’s largest cities are eligible to apply for this pathway. The rural entry schemes now account for approximately 20% of each year’s entry cohort, being more than 50 students at each school.
All NZ medical students have some rural and regional experience during their programs. A subset of volunteer students undertake longer rural immersion programs, usually in year 53,13. Early results show a high proportion of rural immersion students intend to practise in primary and/or rural health care3,13.
From the mid-2000s, all NZ medical students have been invited to participate in longitudinal career tracking studies. At the University of Auckland, this was initially the Faculty of Medical and Health Sciences Tracking Project but, in 2012, Auckland joined with the University of Otago as part of the Medical Schools Outcomes Database and Longitudinal Tracking (MSOD) project. Students are invited to complete surveys at entry to medical school (year 2) and at exit or completion (year 6), with follow-up in postgraduate years 1, 3, 5 and 814. The database now contains a decade’s worth of career tracking data, allowing for an exploration of how career intentions change during medical school. An earlier study using this dataset found that 21% of Auckland students came from an area of 100 000 or fewer residents15. At the completion of medical school, these students were almost three times more likely than those from an urban background to intend working in an area of fewer than 100 000 (rural area). Yet only about half of rural students intended a rural career. Furthermore, 60% more students who intended a rural career came from an urban background than from a rural area15. This suggests that as well as choosing students from a rural background, preventing loss of interest and fostering increased rural interest in all students are important strategies for growing the rural workforce. There is some evidence that students with a stable intention of general practice between measures late in medical school and in the early postgraduate years are more likely to follow through on that intention16. To date, few studies have looked at stability of career location intention17.
Thus, while there is good evidence for the factors positively influencing rural intentions, there is less evidence for factors influencing a change towards or away from such intentions. Using longitudinally linked national data from the MSOD project, the aims of this study were to:
- determine how career location intention patterns change between entry and exit from medical school
- examine factors that may be associated with these changes to shed light on what may promote or hinder a rural career intention.
There was a specific focus on the characteristics of three groups: the rural ‘persisters’ (those with rural intention at both entry and at exit) and the two groups of ‘changers’ (those who change intentions from rural at entry to urban at exit, or from urban at entry to rural at exit).
Methods
Survey
The entry and exit MSOD surveys result in self-reported student data on factors such as demographics and general career intention (discipline and location), with one question in the exit survey asking about the importance of 24 possible influencing factors on career. The survey also asks about rural club involvement.
Definitions
There is no one agreed definition of ‘rural’ in NZ. In the student surveys there are four options regarding the size of the geographical location of a student’s background or intended career location, accompanied by examples and population sizes. An example is ‘major city (population over 100 000), eg Auckland, Tauranga’. For this study, participants were deemed to have a rural background (R) or location intention if they selected one of the three options of 100 000 or less, and an urban (U) background or location intention if they selected the option of more than 100 000. Once entry and exit intentions were examined, participants were placed into one of four intention groups: rural at entry and rural at exit (R-R), urban at entry and rural at exit (U-R), rural at entry and urban at exit (R-U) or urban at entry and urban at exit (U-U). These groups are represented by the arrows in Figure 1.
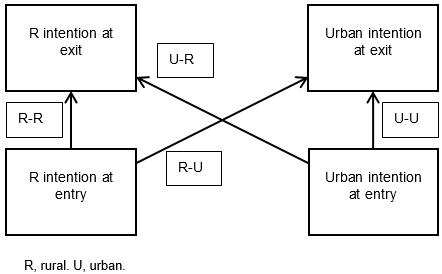 Figure 1: Study groupings based on student entry and exit intentions.
Figure 1: Study groupings based on student entry and exit intentions.
Analysis
Summary statistical analyses were performed. Univariate statistical significance for continuous variables was determined by single factor ANOVA, with Bonferroni corrections for multiple comparisons used in post-hoc testing of differences in the influencing factors. Categorical data were analysed with Χ2 tests.
Further data were not obtained from the medical schools, such as whether or not students underwent a year-long rural immersion program. Nor did the authors compare results between medical schools. Analyses were performed with Microsoft Excel (2010) and SPSS v22 (IBM International; http://www.spss.com).
Ethics approval
Ethics approval for the Faculty of Medical and Health Sciences Tracking Project was granted by the University of Auckland’s Human Participants Ethics Committee (#18456). The MSOD project received ethics approvals from the same committee at University of Auckland (#8539) and the University of Otago ethics committee (07/155).
Results
From 2006 to 2016, 4368 students completed at least part of an entry survey (response rate 85.9%), with 2243 students completing at least part of an exit survey (response rate 66.4%). Not all students answered all questions.
Longitudinally linked entry and exit data were available for 1114 students made up of six paired cohorts from Auckland (2006–2011 entry corresponding to 2011–2016 exit, n=540, 48% of total) and four paired cohorts from Otago (2007–2010 entry corresponding to 2011–2014 exit, n=574, 52% of total).
Patterns
Overall, 628 (33%) of all students who responded to the location intention question in their exit survey were intending to work in a rural area. For the 427 students in the linked data set, the numbers and proportions of students within each intention group are seen in Table 1. There were 239 (21.4%), 188 (16.8%), 135 (12.1%) and 552 (49.5%) students in the R-R, U-R, R-U and U-U groups respectively (p<0.0001). Most students (71%) had a stable geographical career intention at both entry and exit, and more students changed towards a rural career than away from it.
Table 1: Student intention at entry versus intention at exit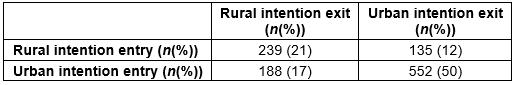
Demographics
Demographic features of students grouped according to intention patterns are shown in Table 2. There were statistically significant differences (p<0.001) among groups for each variable. Of all those with rural intentions at exit, 49% had a rural background, with 51% having an urban background.
Medical students who persisted with a rural career pattern (R-R) had characteristics of coming from a rural background (70%), being female (68%), identifying as NZ European (76%) or having involvement with a rural club for at least 1 year (45%). These students were also more likely to express a GP career intention as their first choice (25%). Post-hoc analysis showed that students who changed away from a rural intention during their time at medical school (R-U) were significantly older than U-U (p<0.001) and U-R students (p=0.002). Apart from a slightly higher age in the R-U group, and 50% of the R-U students having a rural background, no particular demographic factors were associated with students who changed.
Table 2: Student characteristics by intention group 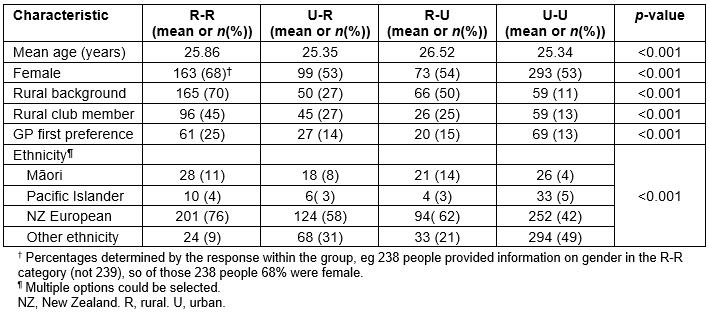
Student responses regarding the influences on most preferred type of future medical practice are shown by intention group in Table 3. The scale ranges from 1 (‘not at all’) to 5 (‘a great deal’). Factors are ranked from the most influential overall to the least.
There was no difference among groups for the top four career influencing factors: atmosphere/work culture typical of the discipline, experience of specialty as medical student, interest in helping people and general medical school experiences (eg mentors, placements).
The rural ‘persisters’ were less influenced by consultants/mentors, the intellectual content of the specialty, job security, perceived career advancement prospects, opportunity for research and/or teaching, perceived financial prospects, perceived prestige of the discipline, financial costs of medical school education and/or debt and the cost of training in the discipline. They were more influenced by geographical location.
The ‘changers’ towards a rural intention were less influenced by the appraisal of their own skills/aptitudes, perceived career advancement prospects, perceived financial prospects, perceived prestige of the discipline and possibly by their own domestic circumstances.
The changers away from a rural intention were more influenced by the intellectual content of specialty and perceived financial prospects.
Table 3: Mean scores on factors influencing most preferred career, by intention group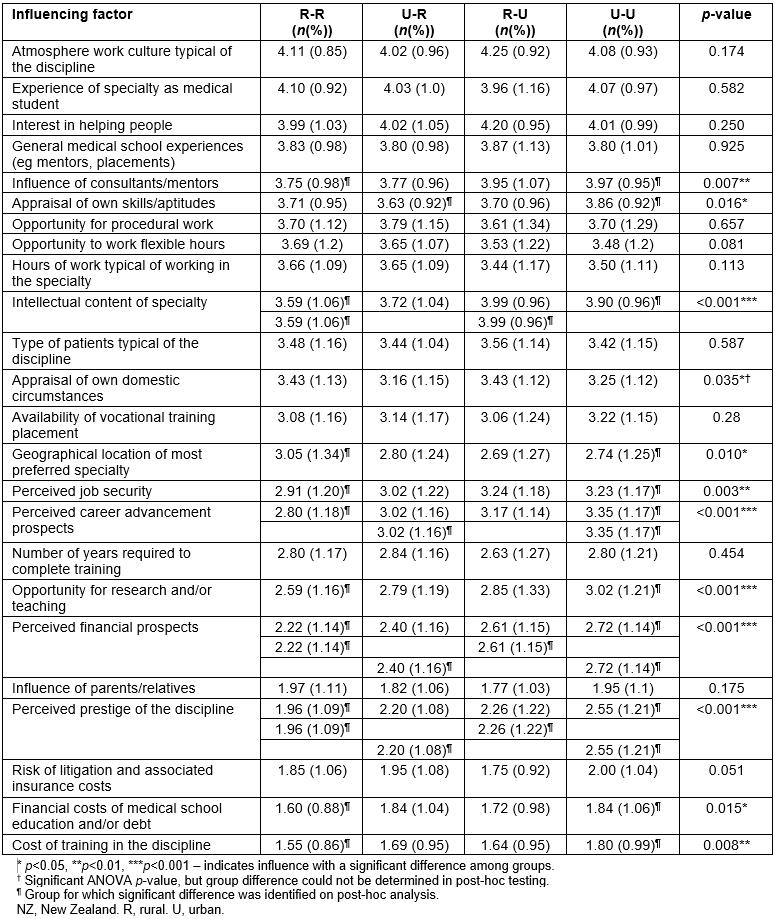
The study was based on linked survey data collected at entry and exit from medical school from more than 1000 NZ medical students. The majority of medical students had stable career location intentions, with a fifth of all students showing persisting rural intentions (R-R) and half showing persisting urban (U-U) intentions. Encouragingly, of the changers, nearly 40% more moved from U to R than from R to U; however, half of those who changed from R to U were from a rural background.
At graduation, over a third of NZ medical students are considering working in an area of 100 000 or fewer which was defined as ‘rural’ for the purposes of this study. Although encouraging, this is a lower proportion than seen in the NZ 2013 census, which reported that around 1.75 million, or 40% of the total NZ population, live outside urban areas5. Nearly two-thirds of rural-intending students at graduation had a rural background, which is consistent with other studies7,15.
From the present study’s results, the broad themes are that rural ‘persisters’ seem to be ‘selected, not made’; that is, they have attributes that are apparent at entry (eg from a rural background, being NZ European or female). The latter is in contrast to findings in a recent Australian study that suggested a lower rate of women heading rurally18.
The ‘changers’ seemed more influenced by financial and career prestige factors, which are largely outside the purview of medical schools. However, the overall influence of these factors was moderate at best. The top four influences on medical student career choice included medical school experiences and did not differ among categories. The duration of NZ medical programs is 6 years, and students have a similar range of placements, both in terms of specialty and in having one or more clinical placements in areas with populations of 100 000 or less. A small number of students undertake rural immersion programs, but as these placements may be allocated to those with a rural background or stated rural career intention, the curriculum effect may be difficult to determine. Nonetheless, incorporating details on placements students undertook during medical school, particularly rural immersion or other prolonged attachments outside urban areas, would add to future studies.
The influence of consultants/mentors was less for the R-R group than for the U-U group, but whether this relates to lack of exposure to senior rural doctors, or less need for this in the R-R group, is uncertain. It was striking how many job-related influences -– financial aspects, intellectual content of specialty, job security, career advancement prospects, opportunity for teaching/research, and prestige – were reported as less influential to students in the R-R group than in the U-U group. This may reflect the nature of the work itself, as well as how the students see their careers developing.
Strengths of this study include the large sample size, prospective data collection and high response rates. The student backgrounds and proportions with rural intentions are comparable with previous research7,10,15,19. These strengths add to the robustness of the findings. Generalisability is increased by this being a national study involving two medical schools, one in a large city. The use of a population of 100 000 as the cut-off between urban and rural areas was pragmatic, as there is no single agreed definition of ‘rural’ in NZ. Findings would be relevant to countries with similar health and medical education systems, and population spread.
The study has several limitations. These include self-reported data and the possibility of social desirability bias, where respondents might answer questions in a manner that would be viewed favourably by others, especially in the entry responses of those who entered medical school through a rural entry pathway. The questionnaire is a relatively blunt instrument for determining factors in career location. Students are asked to assess the level of influence on ‘their most preferred area of medicine’, not specifically where they will practise. Within each influencing factor it is possible that the factor is more important to some within a group than others; this would be concealed in a mean score. However, the standard deviations of both the highest influences and the least are relatively small and consistent, around 1, giving more confidence to the findings. Future studies might verify if the observed patterns are predictive of actual practice, and explore influential factors not captured by the questionnaire.
As yet in NZ there is no systemic linkage of MSOD data with workforce outcomes. The first set of MSOD postgraduate year 8 data will be collected in 2019 and should be informative as graduates will be confirming practice intentions. A recent Australian article has established that rural career intention at entry to medical school is predictive of rural practice, particularly when supplemented by an undergraduate rural immersion experience19. In that study, 17% of students had a rural intention at entry compared with 21% of NZ students in the present study with a rural intention at both entry and at exit. Thus, it seems plausible to assume that the latter students are more likely to enter rural practice.
Notwithstanding the weaknesses and lack of pointers to medical school experiences fostering rural careers, there are implications for medical schools and the wider health sector. Career choice involves aspects of both nature and nurture20. Students with a persistent rural intention are more likely to be born in a rural area, to be female and not as concerned about career prestige, career advancement or financial factors as their urban-intending colleagues. Therefore, schools should continue to recruit large numbers of students from rural backgrounds. Over half of medical students are women, and they outnumber men among new doctors21. Women have long been overrepresented in general practice in NZ and elsewhere, but now the proportion of women working in rural hospital medicine is increasing22. It was encouraging that women formed more than two-thirds of the R-R group, but whether this represents greater exposure to female role models is uncertain. The findings suggest the need for strategies to ensure that women who have indicated an interest in rural medicine progress smoothly through the early years of postgraduate training, noting that this is a time when part-time or interrupted training is more likely for women than for men23. It also underscores the importance of family-friendly features in medical practice, especially in rural areas.
Collectively, students report the atmosphere/work culture typical of the discipline as the most influential on their career decision, with medical school experiences not far behind. Thus, quality experiences in rural areas during and in post-medical school training seem important. The flip side of increased exposure is that students may be deterred if there are relative differences between rural and urban practice in work conditions, remuneration and how doctors are valued. It was notable that nearly half of students who changed from R to U had a rural background. Yet these students were numerically offset by urban background students who change their minds to R. Many work-related influences are more important to urban-intending students than to rural ones. While health and education systems can promote rural practice as attractive compared with other specialties, in the end rural practice must be perceived by students as a job that is ‘good to do’ compared with other specialties24-26.
Conclusion
For nearly a third of students, career location intentions change during medical school, with more changing towards a rural career than away from it. Rural background is a key determinant of a persistent rural career intention. Being female emerged as another important factor, as did being NZ European. While some experiences during medical school will be important, overall the atmosphere/work culture typical of a discipline is the most influential. Medical schools should continue to select rural students and give all students positive rural experiences. Attention to the financial and prestige aspects of rural practice could be a focus during medical school to increase interest in rural practice overall. All stakeholders should advocate for excellent work conditions and opportunities in rural settings.
Acknowledgements
The authors gratefully acknowledge the medical students/graduates who completed questionnaires, and the use of this data collected by the NZ MSOD project, funded by the University of Auckland, the University of Otago and Health Workforce New Zealand. Ying Huang and Chris Frampton provided statistical assistance.
Matthew Kent was funded by a University of Auckland Summer Scholarship in 2016–2017.



