full article:
Introduction
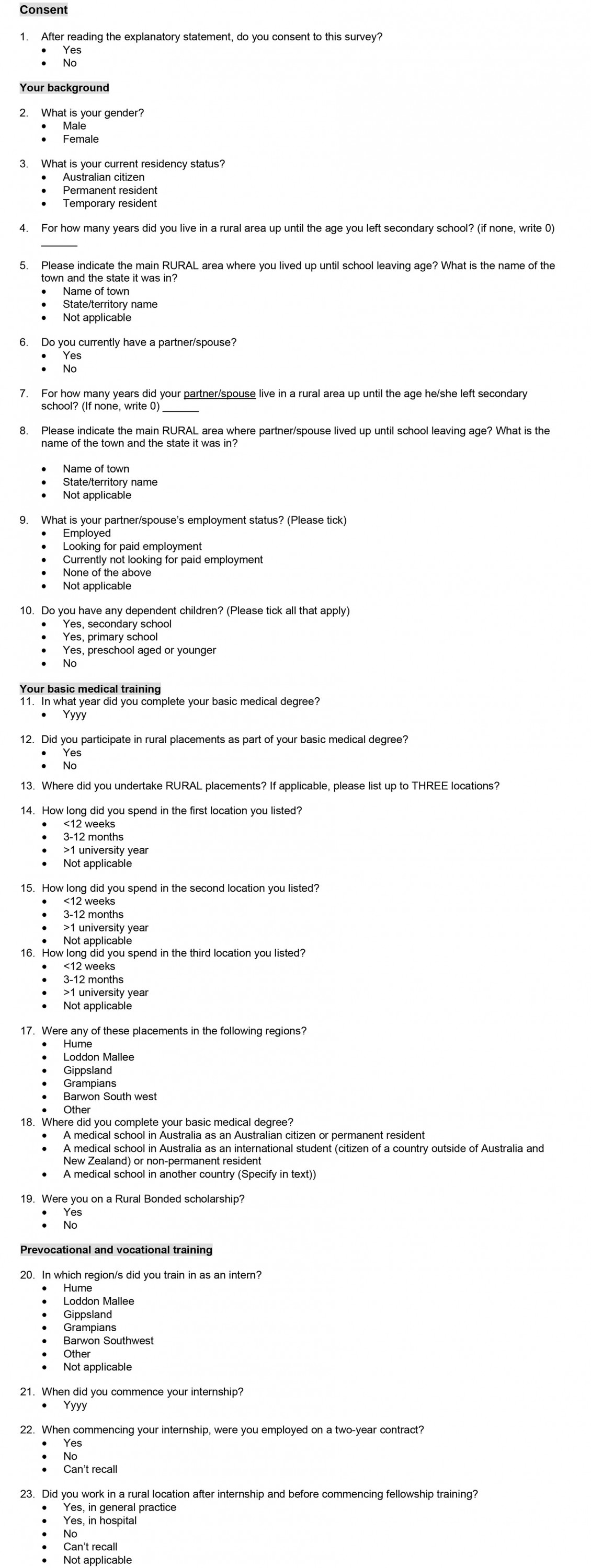
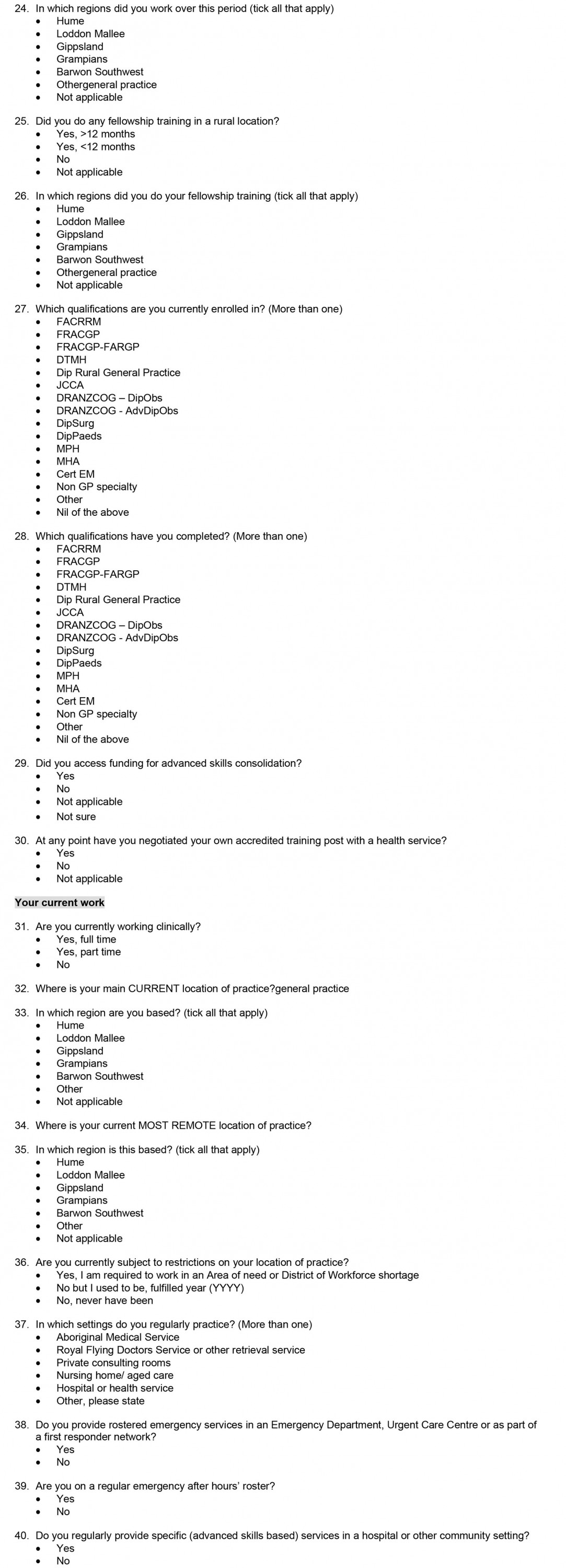
It has been a decade since the Victorian Department of Health invested in its first Rural Community Internship Training (RCIT) Program. The RCIT Program aims to support the development of rural generalist (RG) doctors. Such doctors are GPs who practise in team-based care in rural communities, and who have skills to work at a broad scope to deliver the range of primary care and additional specialist services that the community needs. This provides more comprehensive care in rural communities that have limited access to individual specialists. Internship is the first year after graduating medicine when doctors complete specific terms in order to achieve general registration for independent work. The RCIT involves a year of accredited internship training delivered in smaller rural communities (<50 000 population), where new graduate doctors can undertake up to 20 weeks general practice experience working with qualified RGs and visiting specialists, at broad scope1. In the remaining terms, the doctors complete core internship requirements of 8 weeks of emergency medicine, 10 weeks in general medicine and another 10 weeks in surgery2, by rotating into nearby larger regional health services. This results in at least 47 weeks of full-time equivalent service that interns require for eligibility of general registration. It is a different model from most standard internships, which are wholly hospital-based and delivered mostly in larger metropolitan and regional centres by rotating around hospital departments2. After doctors complete the RCIT Program, they are eligible for the next step in the RG training pathway or to change training directions.
Victoria’s RCIT Program commenced in the Hume region in north-eastern Victoria as the ‘Murray to the Mountains’ program in 2012, initiated by Dr Jack Best and funded by the Victorian Department of Health3,4. Based on its success, the department expanded it to Victoria’s four other rural regions in 2015. Hence, by 2015 the RCIT Program was available in not just the Hume, but also the Loddon Mallee, Grampians, Barwon South West and Gippsland5. In 2019, with minimal changes, the program was incorporated as the foundation year of Victoria’s RG training program (VRGP) and retitled the rural generalist year 1 (RG1)6. It has thus become a critical point in Victoria’s longitudinal RG training model, which aims to attract interested doctors to undertake up to 6 years of postgraduate training (RG1–RG6). The VRGP aims for RG-focused doctors to complete a specialist general practice fellowship along with additional advanced skills training, to work as a qualified RG in Victoria’s smaller rural communities, where there are few other specialists7. Despite the significance of the RG1 year (encompassing the former RCIT) for achieving the goals of the VRGP, the characteristics of the newly graduating doctors attracted to this training and the workforce outcomes are yet to be reviewed.
Newly graduating doctors wanting to pursue the RCIT or RG1 internship (hereafter called RG internship) need to apply as part of the state-managed Victorian intern matching system. They do this after completing a direct application to the relevant RG internship program. Places are capped and applications are competitive. Generally, selection is prioritised around the doctor’s rural background, their connection to the region and their demonstrated commitment to practising in rural areas to deliver high quality medical services7.
The rest of the mainstream matching intern process did not specifically allocate doctors with rural interests to rural places. However, the Victorian Rural Preferential Allocation (VRPA) process was introduced for the 2021 internship intake, to increase the capacity for domestic medical students to get preferred rural internships, beyond those with interests in the RCIT8. This is because the VRPA places candidates who have completed high school in Australia, and undertaken undergraduate rural medical training, in a separate first priority round for a rural internship place they want, which occurs before the main intern match. This was introduced following evidence identifying that Victoria’s broader rural internships were being filled by international students (with no prior rural training experience) or many domestic students with low preference of the allocated position rurally9.
Each rural region in Victoria has had full autonomy to design its own locally responsive RG internship program, but there have been points of commonality (Table 1). These have included the option of 10–20 weeks general practice experience, supervised during that term by GPs who work at wider scope with on-call and use advanced skills (except Barwon South West, for which the RG internship was wholly hospital based until 2017). The programs are all based in a setting where there are limited other specialists. Each program has had its own manager and director of clinical training, along with some administrative support. The program staff have played the role of case-managing trainees, facilitating high quality supervised learning across practices and hospitals and overseeing internship training requirements (including providing a program of off-the-job learning opportunities). The Hume is the largest program (growing from five positions in 2012 to 15 per year since 2017, compared with the maintenance of five positions in all other regions). This relates to its RG training capacity and longevity.
When it comes to considering how well this program is delivering on RG workforce goals, it needs to be clear that the Victorian context is unique for attracting and retaining RG doctors. Victoria has a devolved health service governance model and is smaller than other mainland Australian states, with five major regional centres that continue to grow their specialist workforce capacity. Across the state, Victoria has 300 hospitals and health services inclusive of a large number of smaller independent rural hospital services spanning many towns and communities in five rural regions10. These hospitals and health services are governed by independent boards of directors, who may choose to engage in RG workforce development or not11. In doing so, the boards weigh up strategy, risk and compliance issues.
The predominant RG employment model in rural Victoria encompasses doctors employed in a private general practice or Aboriginal Community Controlled Health Organisation (ACCHO), who additionally attend hospitals as a visiting medical officer (VMO) model, and often across more than one health service6. There is currently no state award for RGs in Victoria to provide for RG salaries in hospital or VMO roles, but RGs are free to negotiate their contracts with independent health services. Delivering RG training in the Victorian context depends on extensive coordination of independent entities relative to the interest of RG-focused doctors. This includes managing multiple employment and training needs in the face of changing health service, training and doctors’ priorities. With this context in mind, the longitudinal outcomes of RG internships are likely to rely on whether the program is able to effectively select and harness strong RG career interest in a junior doctor and work to coordinate a pathway for the doctor to continue in RG work and in the region.
This study aimed to explore the characteristics and satisfaction of newly graduating doctors who participate in RG internship training in Victoria and the workforce outcomes of this training in terms of rural work, in the same or another region, in general practice and/or at broad scope.
Table 1: Design of the rural generalist internship program in each rural region3,4,12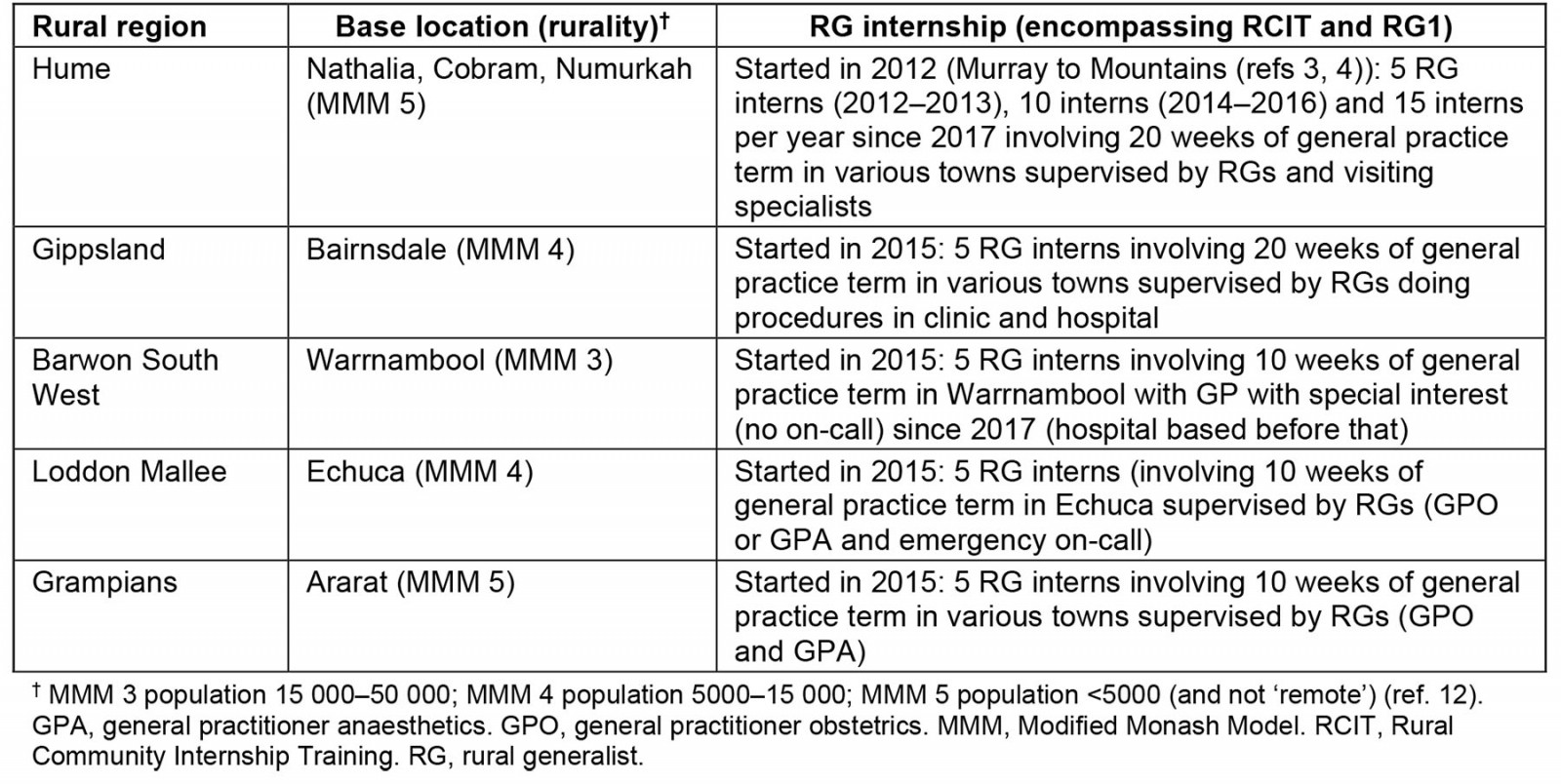
Methods
This study was developed in consultation with the Victorian Department of Health, a statewide evaluation advisory group, the VRGP regional networks and coordinating unit and clinical leads, the Postgraduate Medical Council of Victoria, VRGP Program staff, a health service executive team of participating organisations along with RG supervisors and trainees.
It was nested within a broader VRGP Program evaluation and a program logic that was agreed by a statewide Evaluation Advisory Group, chaired by the Victorian Department of Health. A simplified evaluation theory was applied based on the work of Funnell and Rogers13. It followed that if the RG internship program is known and considered to be attractive to soon-to-graduate doctors, and medical students apply for the program and find it meets their expectations and they complete the program, then they will show skills and capabilities to work at RG scope and to maintain rural work interests specific to the area where they trained. Based on this logic, a survey was designed to assess the characteristics of doctors attracted to RG internship training, their satisfaction with the training quality and development of skills aligned with the work of an RG, pursuit of general practice careers and whether they proceeded to stay and work in smaller rural areas and/or the same rural regions, at broader scope.
Participants and data collection
Between October and November 2021, a retrospective 10-minute anonymous survey invitation was sent to all contactable interns (n=222) who had completed/were completing the RG internship training between 2012 and 2021, from up-to-date email contact lists held by RG internship managers. The survey was co-designed with RG internship program managers and the statewide evaluation advisory group, and informed by the latest evidence regarding RG medicine and rural training predictors and outcomes of interest3,4,9,14-18. The survey was also designed to test the key research questions. It was circulated, with study information, directly to doctors who had completed the RG internship or indirectly via the RG internship manager in one region (at their request). Invitations were sent by blind copy email with three reminders. Participants completed the survey using Microsoft Forms, which was deemed the most accessible format relative to the email networks used by the trainee group (many gmail-based personal email addresses) (Appendix I). Informed consent was recorded. A control group was not available for this study as the statewide evaluation advisory group had determined that contact details for non-RCIT/RG1 rural interns backdated for this study period were inaccurate. As such, comparative benchmarks were drawn from best-practice state or national data or data from other RG training programs.
Analyses
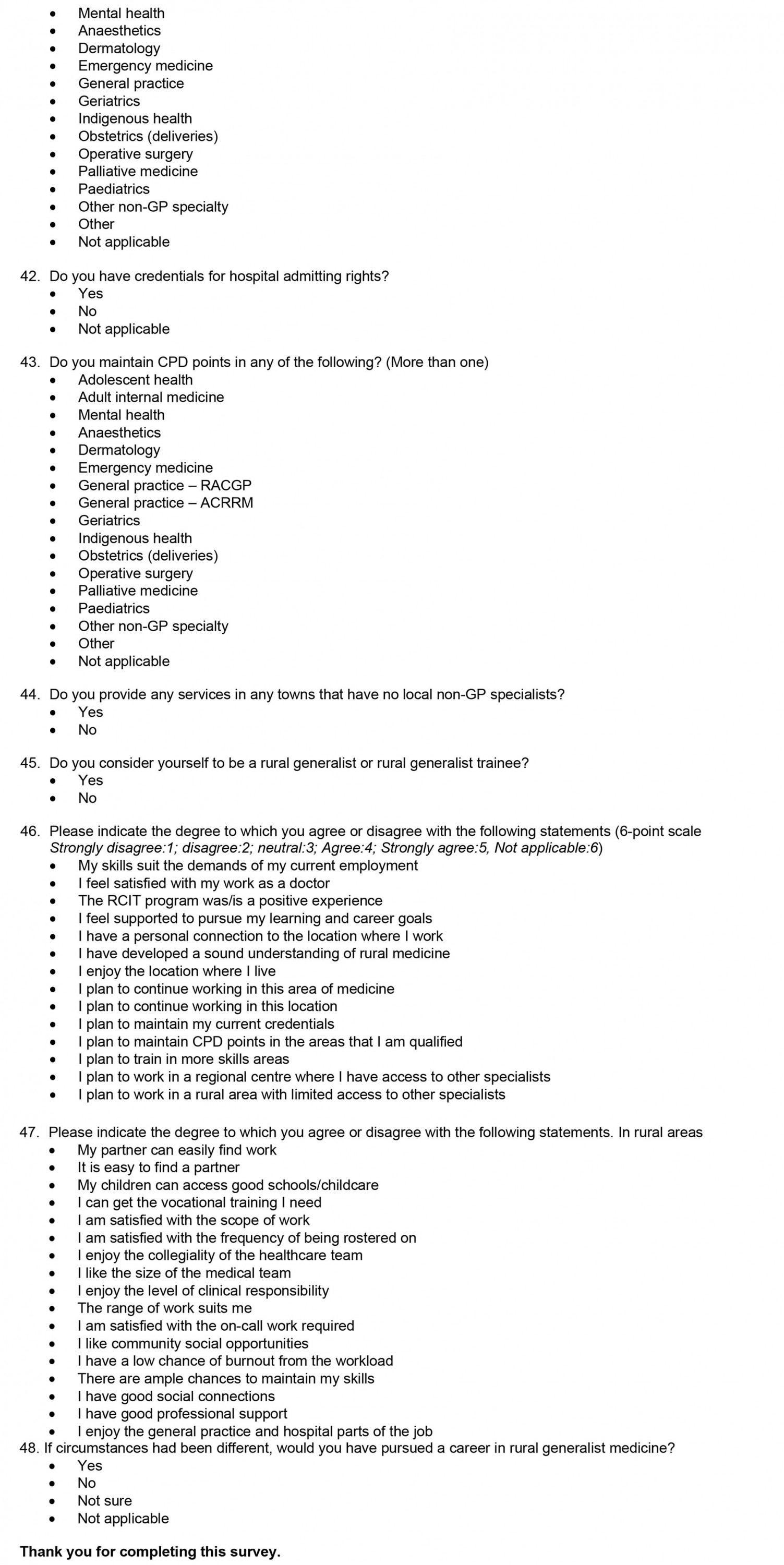
The data were analysed descriptively, by subgroup, to explore pathway outcomes by region, training stage and specialty choice. Depending on the indicators, some analyses were limited to doctors at particular training stages and those who reported their region of RG internship (n=6 reported missing). The RG scope was defined in line with the recommendations of a national evaluation working group, which was chaired by the lead evaluator in 2018–19. This working group reported to the Taskforce for the National Rural Generalist Training Pathway, which informed national policy advice to the Commonwealth Minister for Health. This group had determined that measuring RGs was best achieved by using a range of indicators of RG scope, including rural distribution, servicing more rural areas as a prevocational doctor or GP, being rostered onto an emergency department (ED) roster, engaging in on-call and after-hours components to work, having hospital admitting rights, working in towns with few other specialists, practising or training in additional skills/maintain continuous professional development (CPD), working in multiple settings across the community or self-identifying as an RG12. A core set of more specific criteria were further applied to explore RG scope. Self-identity as an RG was used given that the RG workforce is becoming more well known and embedded in training curriculums19. Rural areas were defined as Modified Monash Model (MMM) 2–7 in line with Australian policy, with further stratification to explore distribution to smaller communities (<15 000 population delineated as MMM 4–7)12. Quantitative analyses used Stata SE v15.1 for Windows (StataCorp, https://www.stata.com), with descriptive statistics of counts and proportions used to present patterns among respondents.
Ethics approval
Ethics approval for this study was obtained from Monash University’s Human Research Ethics Committee (Project ID # 2021_30309).
Results
The survey achieved a 27% response rate; 59 doctors from different regions responded (Table 2). Most (81%) participants were between postgraduate years 3–7 and only three were completing the RCIT year at the time of the survey. There was a slight male bias in respondents, which was less than found in other literature about practising RGs in Australia20. A higher proportion (85%) of respondents were Australian-citizen locally trained doctors, compared with Victorian intern data suggesting that 24% of rural interns were international medical students9. Slightly fewer were rurally bonded compared with studies of early career doctors working rurally in Victoria21. A higher proportion had previous undergraduate rural training of longer duration than comparator cohorts15,21. A higher proportion (39%) were from a rural background compared with other benchmarks (30–34%)15,21 (Table 2). Most respondents were from the Hume region (42%).
Table 2: Respondent characteristics of participants in the rural generalist internship (n=59)9,15,20-22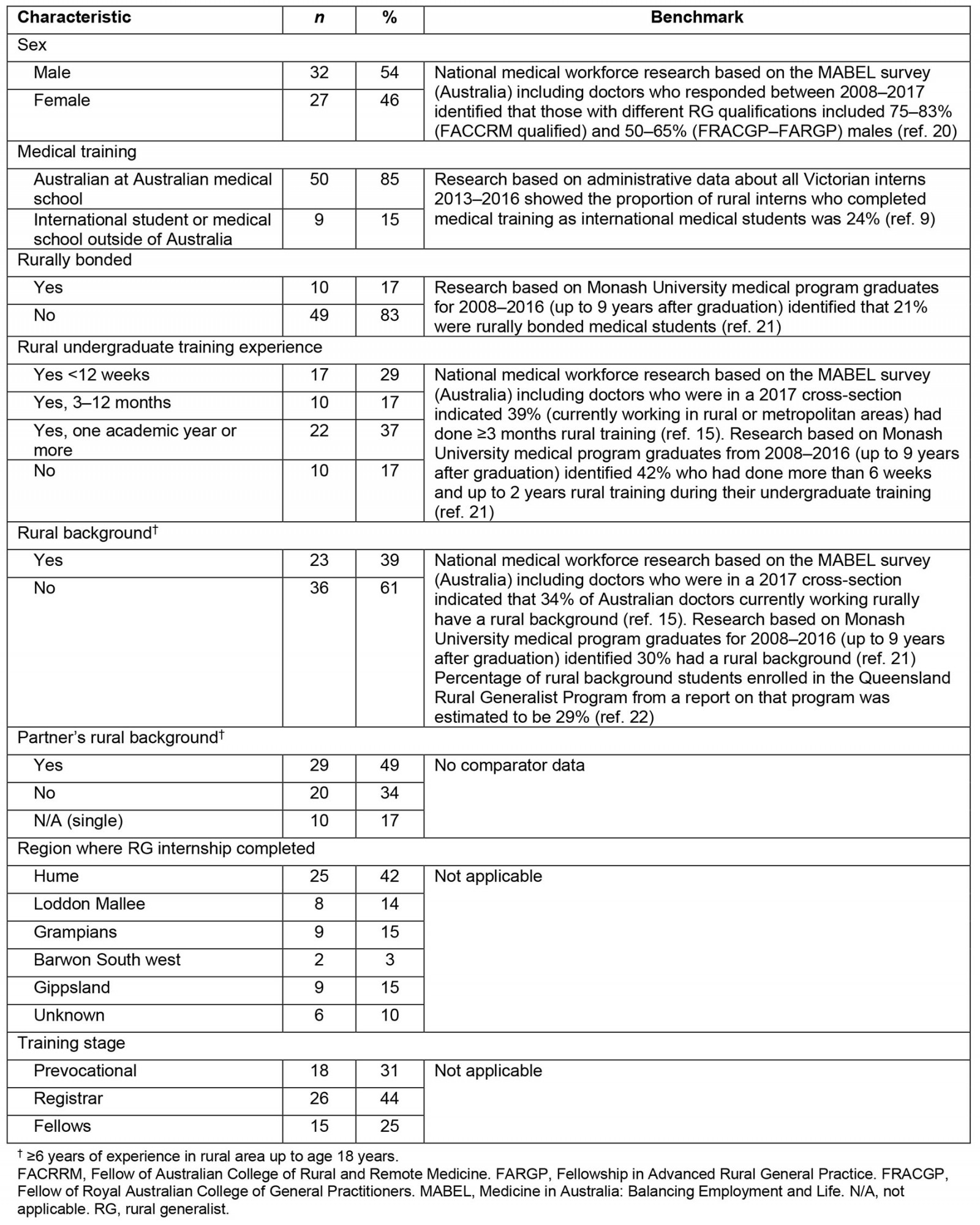
Table 3 indicates the results relating to satisfaction and retention. On most benchmarks of rural workforce development in Australia, the RG internship achieved better outcomes. Overall 48% returned to the region where they had done undergraduate training compared with 25%, as indicated from national studies23. Although there was no comparator data, a high proportion (56%) remained in their RG internship region for further prevocational training, and 40% (excluding three current interns) were currently working in the same region where they did their RG internship. Excluding current interns, the cohort also showed signs of being distributed to smaller towns, although there was no comparator data. The uptake of general practice training/fellowship was high at 61% (25/41, after excluding prevocational doctors not yet enrolled in specialty training) compared with comparator data suggesting uptake of general practice of up to 36% and only 9% uptake of rural general practice24.
Satisfaction with RG1 training was complete (100%). Satisfaction with specific training quality indicators was also positive (Table 3) except for a few results suggesting that around one in five needed to negotiate their own training post (22%), and only 1 in 10 (11%) agreeing that it was easy to find a partner in rural areas. One in four (25%) agreed that in rural areas there is a low chance of burnout (suggesting 75% viewed the chance of burnout was probable).
Table 3: Satisfaction with rural generalist internships and workforce outcomes22-27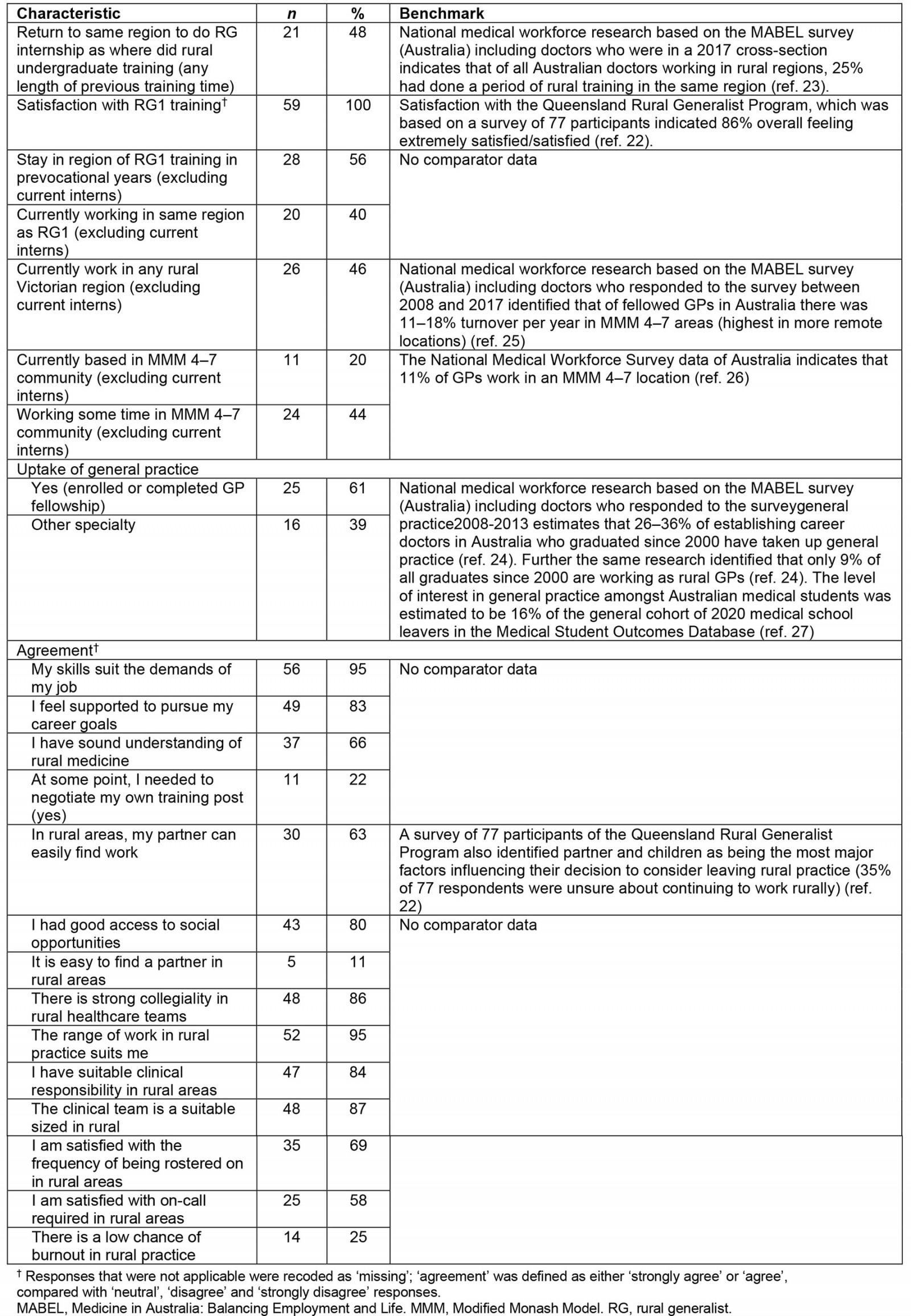
Table 4 indicates the scope of work and RG identity of RG internship participants. Overall, 42% self-identified as an RG. A higher proportion indicated current or plans to maintain CPD at additional specialist scope (92%), and 68% planned to work rurally in a setting where there are limited other specialists. Around one in four (26%) had hospital admitting rights and 8% worked in aged care, and 90% worked at least partially in hospital or health services other than private consulting rooms. Nearly all (97%) met at least one of the key indicators of extended (RG) scope and 80% met more specific criteria including working in ED and on after-hours rosters, with hospital admitting rights, servicing towns with few other specialists and self-identifying as an RG.
Table 4: Scope of work, rural generalist identity among participants in the rural generalist internship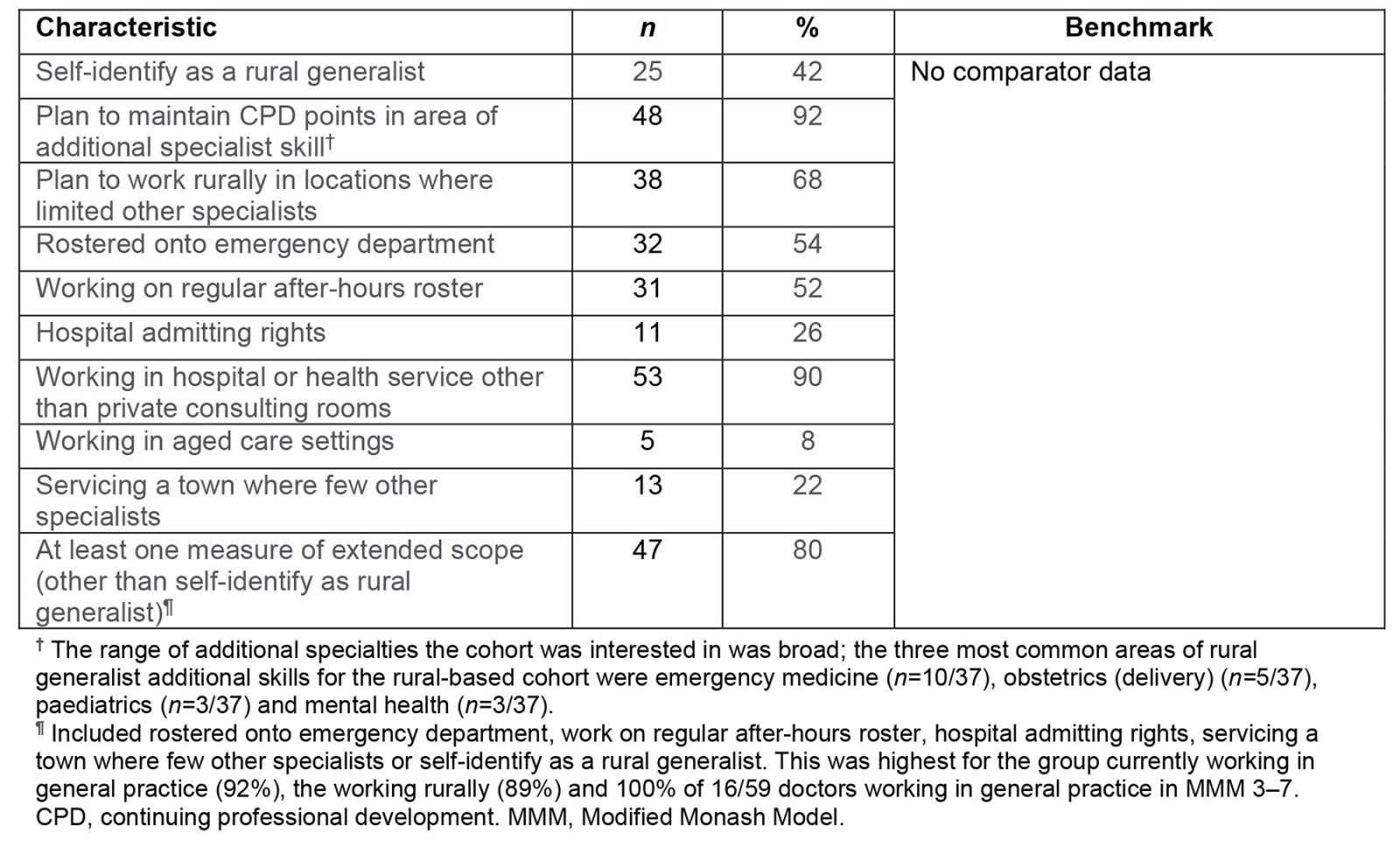
Discussion
This research fulfils its purpose of exploring the characteristics and outcomes of doctors who participated in RG internships in Victoria. Although a small cohort, they are a critical one to understand with respect to shaping RG training and workforce policies. The research indicates the outcomes of RG-focused internship training, up to 9 years (with around 69% of the cohort having commenced or completed specialty training at the point of data collection). It informs the ongoing development of the VRGP longitudinal training pathway7. It also supports the evidence base for developing the national RG pathway28. The primary finding is that the program’s attractiveness and its training outcomes are better than national benchmarks for attracting and retaining a workforce in rural communities, and for retaining doctors longitudinally through training in the same region. This suggests that RG-focused internship training where doctors have access to program coordination staff and enable general practice RG supervision and RG scope of work in general practice is helpful for growing the rural workforce.
The RG internship tended to attract relatively equal proportions of male and female RGs compared with other research, noting that females are likely to be less attracted to rural work, even though they more likely take up rural training opportunities during medical school15. It suggests that RG internships may suit the needs and interests of female doctors, including considering children and partner needs29. A framework to help rural pathways to be more responsive to the needs of female doctors was recently published30. The RG internship also attracted a higher proportion of Australian-citizen doctors who trained at Australian medical schools, of rural background and rural undergraduate training experience in the same region. This suggests that RG internships may play a role in strengthening the capacity to attract rural-background, rural-intentioned doctors to continue to work rurally in the early postgraduate years – what is called end-to-end rural training models. The updated WHO recommendations in 2021 reiterated the 2010 global evidence supporting that training health workforce using a ‘grow your own’ approach is critical to drive better retention rates31.
There may be some variability between the attractiveness of different RG Internship programs that were studied, but this was not possible to tease out from the available data. The findings are weighted to the longest standing and largest RG internship program, called Murray to Mountains, in the Hume rural region, which had already shown positive early results of retaining doctors into their second postgraduate year3,4. However, the combined results hint that the selection criteria used to recruit doctors into the RG internship programs overall are achieving the program’s purpose (based on the characteristics of this sample, of whom a large proportion have a rural background). It may be a model that other postgraduate specialist training could adopt given non-general practice colleges show limited consistency in their rural-focused selection policies32.
Other findings suggest that the RG internship program has some capacity to attract and retain doctors in the same region beyond the RG internship period. This is a period when rural retention is typically challenged due to the difficulties in accessing relevant specialist training pathways. The results of this study suggest that RG internship participants commonly stay in the same region for further prevocational work and ongoing specialist training, well above national benchmarks. For example, the best quality national research about this, which was unbiased to institution or funding body, showed that of Australian doctors currently working rurally, 25% had done a period of rural training in the same region23. However, the rates in this study were approximately double: 48% of RG internship doctors remained in the same region for further prevocational work and 40% currently worked in the same region. There are also very high levels of satisfaction with the RG internship training provided, which may relate to the positive results on doctors remaining in the same region. This suggests that RG internship training that has administration and case management support for the doctors, along with RG-focused supervised learning opportunities, may give good connections to a networked regional training system. The results are more remarkable in the Victorian context where training and employment need to be negotiated with independent health services whose board and executive teams may or may not choose to support RG models.
The results hint that the RG scope of work relative to training needs may be difficult to negotiate: around one in five of the RG internship participants indicated that they needed to negotiate their own training posts. There is no comparable data against which to assess this, but while training posts are not systematised in Victoria between general practices and the hospitals, there is going to be a need for more expenditure on coordination of staff, and dependence on individual doctors and their willingness to negotiate the RG training system. The nationally funded coordination units that have been implemented in each state and territory to support RG training are hence important6.
The final point of discussion is that the RG internship training shows better outcomes than industry benchmarks with regard to developing a GP workforce that works rurally at broad scope. Overall, nearly two in three participants enrolled in or had completed their fellowship were on the general practice pathway and 42% of the total cohort identifies as an RG. The intention of the doctors to maintain a wide scope, connection to rural areas and work in distributed sites where there are few specialists suggests the RG internship may assist to build the type of workforce that Australia is trying to promote under its new National Medical Workforce Strategy (2021–2023)33. Many of the doctors responding to the survey identified that they feel that they have the skills for the job and good variability of work, and they enjoy the collegiality of rural practice. However, potential retention pressures noted were non-professional issues, related to partners, and professional issues like the perceived risk of professional burnout. If these two issues were specifically addressed, then the sense is that RG workforce retention may be further enhanced in the Victorian context. This may rely on attention to selecting people who have partners, whose partners can find work in rural areas34. Fostering sustainable models of rural health care is also likely to substantially address concerns of burnout, and these form a major thrust of current Australian government policy and research, however they rely on co-planning with state governments given that RGs also support hospital (state-government) caseload35-37. In Victoria, the procedural caseload of rural hospitals and visiting medical officer (VMO) services are considered to be reducing over time, which threatens the potential to retain RGs who go through the VRGP1,38.
The study has some major limitations. It was done in the Victorian context, which is unique in that the rural health services are all independent and there is no RG award, with RGs mostly working on fee-for-service contracts as VMOs, which they have to negotiate at each health service. The survey only had 59 respondents, which limited the capacity for multivariate analysis or any comparisons between regions. However, the response rate was reasonable, particularly given that the survey was done during the COVID-19 pandemic. There was no comparison group for the study, due to the lack of up-to-date administrative data to contact other rural interns who weren’t part of the RG internship training, but this research used a range of published sources to provide a sense of how the RG internship program’s outcomes are tracking. Further, this is the first research to build in measures of RG scope of work, to provide a starting point for other studies to explore how to measure the RG workforce. More research is warranted about this and the outcomes of RG training programs to objectively inform RG training design, but this will require specific investment in postgraduate workforce tracking methods.
Conclusion
This research is the first to explore the outcomes of an RG internship program in the Victorian context. The findings positively suggest that the RG internships attract rurally intentioned and rurally experienced doctors. The doctors have a satisfying training experience, many remain in the same rural region as their rural undergraduate and rural internship training, and they complete postgraduate training in the same region. They also often follow a general practice career and work at broad scope, including hospital roles and intending to stay in that region, which are better outcomes than demonstrated in the wider literature about rural workforce development. This suggests RG internship programs are likely to be a positive intervention for promoting an RG workforce and their design might contribute to informing the ongoing development of RG training programs.
Acknowledgements
We gratefully acknowledge the Victorian Department of Health, which funded this evaluation and funds the Rural Community Internship Training Program in Victoria, part of the Commonwealth and Victorian co-funded VRGP. This project was possible due to the support of rural community internship training staff and the participation of the doctors who responded to the survey.
Funding
We gratefully acknowledge the Victorian Department of Health, which funded this evaluation and funds the Rural Community Internship Training Program in Victoria, part of the Commonwealth and Victorian co-funded VRGP.
Conflicts of interest
BOS was funded for this research by the VRGP; SB and AS were directly employed by the VRGP. SB and JP were involved in the internship training model in the Hume region. BOS, SB, AS and JP live and work in the regions under study.
references:
You might also be interested in:
2012 - Extending the paramedic role in rural Australia: a story of flexibility and innovation
2009 - Survey of a videoconference community of professional development for rural and urban nurses