full article:
Introduction
Skin and soft tissue infections (SSTIs) include cellulitis, wound infections, boils and abscesses. They are common in Aboriginal and Torres Strait Islander Peoples (hereafter respectively referred to as First Nations Australians) living in remote Australian communities1. The burden of SSTIs in First Nations communities is compounded by higher rates of comorbidities, including obesity and type 2 diabetes mellitus. The social determinants of health are critical contributors2,3. In Australia, SSTIs are managed predominantly in outpatient settings. But, for First Nations Australians living in northern Australia, hospitalisation rates for SSTIs are three times that of non-First Nations Australians4. These infections are more likely to be complicated by sepsis and more commonly necessitate intensive care unit admission5,6.
SSTIs present a substantial financial burden on Australia’s health system: a single episode of hospitalisation for SSTIs costs at least $670 per day7. Cellulitis alone accounts for 250 554 hospital bed days and 11% of all potentially preventable hospitalisations. Individuals living in rural and remote Australia often require aeromedical retrieval service to access emergency department and inpatient care; this represents a sizeable financial cost8.
The Torres Strait is a body of water bounded by mainland Papua New Guinea to the north and Cape York, Queensland to the south (Fig1). The 18 inhabited Australian islands9 of the Torres Strait have a population of close to 4500 people, the majority (about 2800) of whom live on Waiben (Thursday Island), the administrative and commercial centre of the Torres Strait region and location of the referral hospital. The Torres and Cape Hospital and Health Service (TCHHS) is the main, publicly funded health service in the Torres Strait. The hospital on Waiben is closely linked to 16 primary healthcare centres on outer islands. TCHHS also services Cape York with an additional three hospitals and 14 primary healthcare centres10. Approximately 64% of the population serviced by the TCHHS identify as Aboriginal and/or Torres Strait Islander, as compared to 3.3% represented in the whole Australian population11. The proximity to Papua New Guinea provides additional challenges for local clinicians and broadens the differential diagnoses for SSTI presentations12.
There are few published studies highlighting the financial expenditure and health economic impact of SSTIs in Australia’s First Nations communities. The aim of this study was to define the health service utilisation and health system costs associated with SSTIs in the Torres Strait in order to identify ways of improving the quality of regional healthcare delivery.
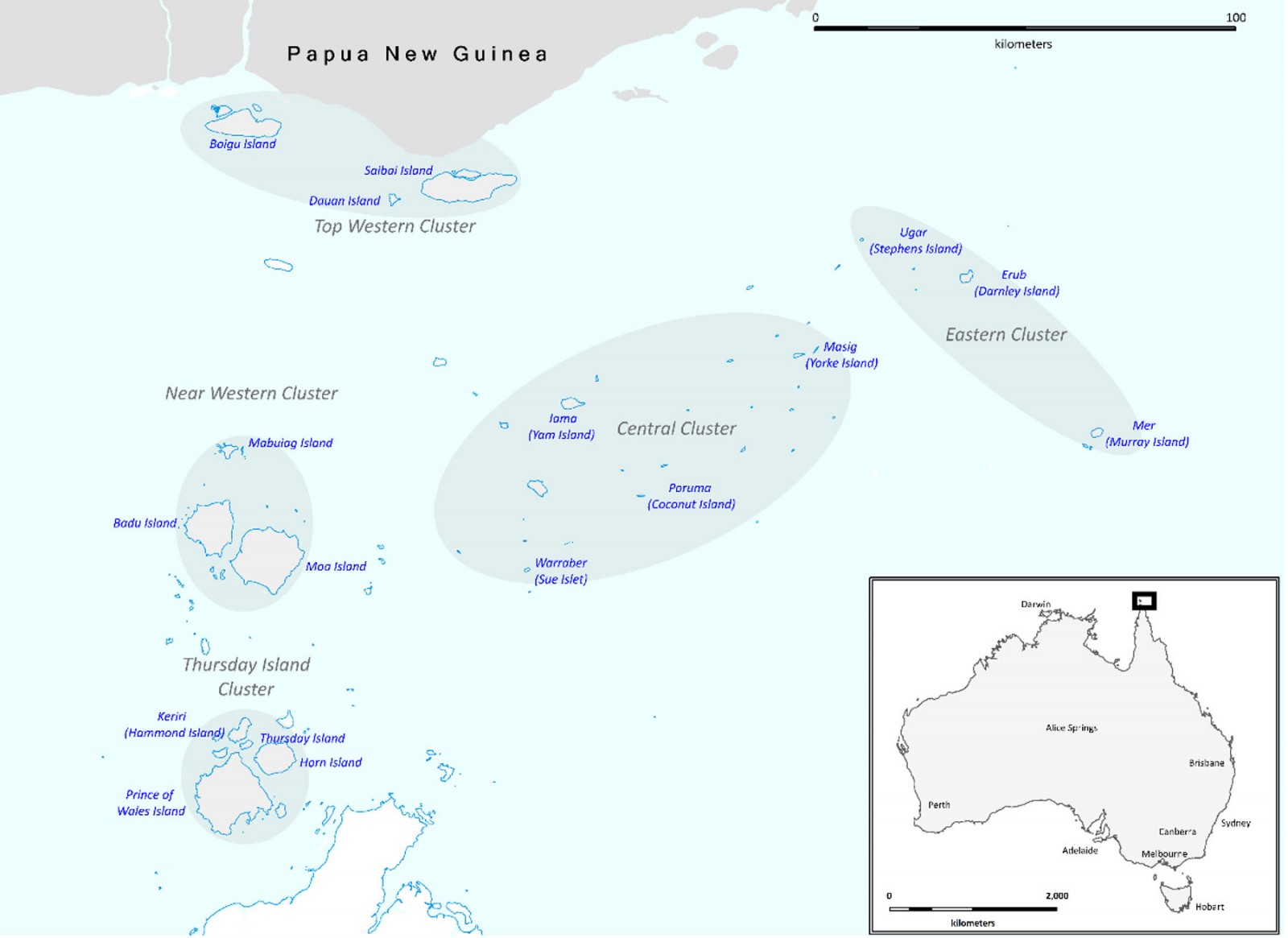 Figure 1: Map of the Torres Strait, Queensland, Australia.
Figure 1: Map of the Torres Strait, Queensland, Australia.
Methods
Data collection
Episodes of outpatient care, emergency department visits, inpatient care and aeromedical retrieval services for patients with SSTIs were collected from TCHHS health service electronic medical records for the 2-year period between 1 January 2018 and 31 December 2019. This period coincided with a year-long observational study evaluating the safety, effectiveness and community acceptance of outpatient treatment of SSTIs across the Torres Strait region in 20191. Demographic data included gender, age, ethnicity and residential address. Costs for inpatient and emergency department use were derived from the Australian Refined Diagnosis Related Groups (AR-DRG) and Urgency Related Group (URG) codes for each inpatient and emergency department occasion of service respectively. This information was combined with the mean costs reported by the National hospital cost data collection public sector report 2018–201913. Each outpatient service was assigned a cost based upon Tier-2 number 40.13 (Wound Management). Patients with SSTIs who resided outside of Waiben and who required inpatient or emergency department care were transferred by the aeromedical retrieval services. The cost of an aeromedical retrieval in the Torres Strait was sourced from Queensland Health. Outer islands were defined as any inhabited island other than Waiben.
Individual data were de-identified, aggregated and entered into an electronic spreadsheet (Microsoft Excel). The demographic characteristics of people accessing health services for SSTIs in the Torres Strait were reported by health service type including outpatient clinic, emergency department and inpatient. The individuals accessing health services were disaggregated by outpatient clinic, emergency department, inpatient and retrieval services. Of those who accessed health services, we recorded the mean number of episodes for each type of health service accessed. The mean costs per healthcare episode for individuals with SSTIs were reported and the total number of health service episodes were reported. Total costs associated with SSTIs were disaggregated by health service type (outpatient clinic, emergency department, inpatient and retrieval services); these were calculated by multiplying the number of episodes per year by the mean cost per episode in that year. All health service utilisation and cost results were reported for the years 2018 and 2019.
Ethics approval
The Far North Queensland Human Research and Ethics Committee provided ethics approval for the study (HREC/2018/QCH/44535). As data was retrospective, aggregated, and de-identified in nature, the committee waived the requirement for informed consent.
Results
Between 2018 and 2019 there were 3509 episodes of SSTI care in outpatient clinics, 507 episodes of SSTI care in the emergency department and 100 inpatient admissions (Table 1). Most outpatient presentations were from outer island residents (2313/3509 (65%)), whereas most presentations to the emergency department were from Waiben residents (331/507 (66%)). Of those admitted to hospital on Waiben, 55/100 (55%) were from outer islands.
A total of 2529 individuals accessed health care for SSTIs, 2307/2529 (91%) presented to an outpatient clinic, 396/2529 (16%) to an emergency department, 92/2529 (4%) were admitted as an inpatient and 163/2529 (6%) were retrieved by air (Table 2). A mean outpatient clinic episode cost $240.00, an emergency department episode cost $400.85 and an inpatient episode cost $8403.05. A retrieval service cost $18,670.00 for individuals with an SSTI (Table 3).
The largest contributor to total cost was retrieval services, a mean of $4,303,435 per year. The total cost to the health system for SSTI management was $6,169,881 (Table 3). The mean annual amount of funding for TCHHS between 2018 and 2019 was $216,482,295. These amounts cover the Torres Strait (population close to 4500) and all the towns and communities of Cape York (approximate population 7500). This SSTI management in the Torres Strait accounts for 3% of the total annual TCHHS health service budget.
Table 1: Demographic characteristics of people assessing health care for skin and soft tissue infections across the Torres Strait, 2018–2019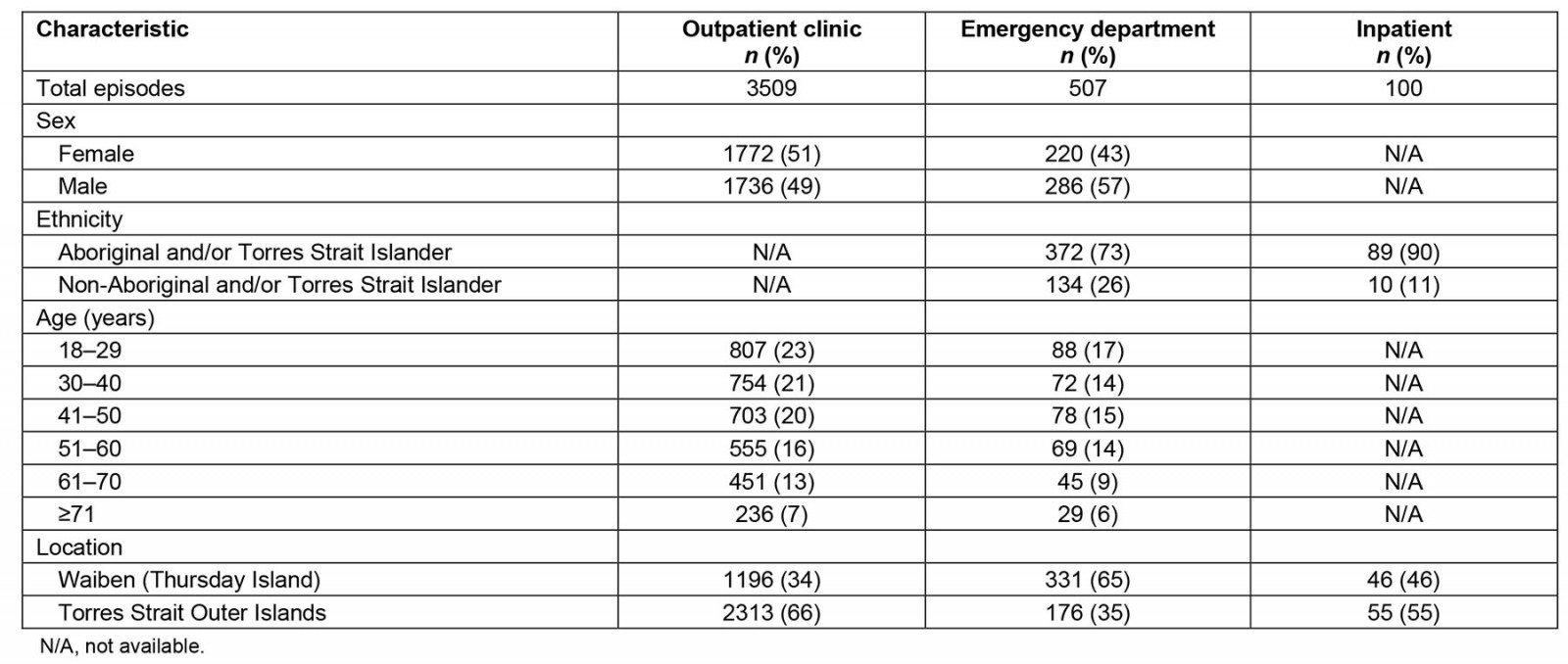
Table 2: Number of individuals accessing different types of health care for skin and soft tissue infections across the Torres Strait and mean number of episodes for individuals who did access care, 2018–2019>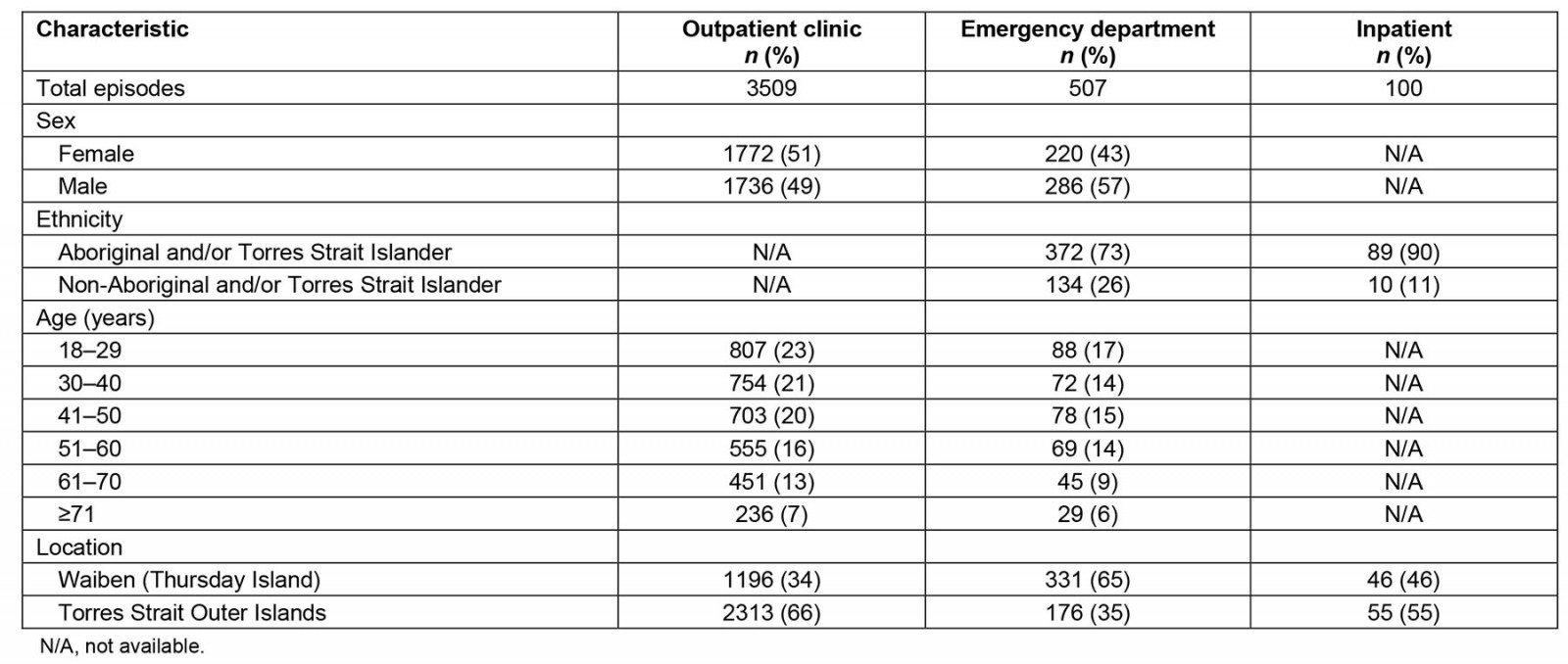
Table 3: Estimated mean health systems costs per episode and total costs for individuals with skin and soft tissue infections across the Torres Strait, 2018–2019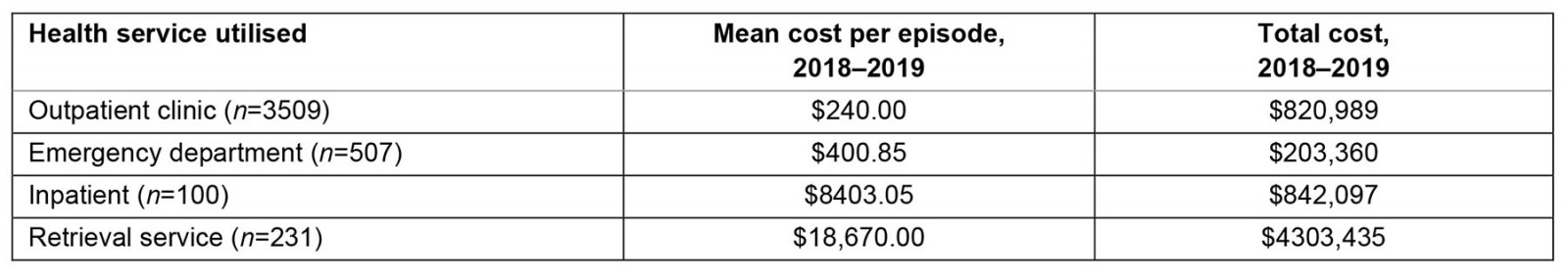
Discussion
SSTIs in the Torres Strait are a substantial financial burden for the health system. The yearly number of individuals accessing the health service for SSTI management was 2529, a staggering 56% of the total local population. SSTI management in the Torres Strait alone accounts for 3% of the total health service budget for the Torres Strait and Cape York. This burden of SSTIs highlights the need for greater upstream preventative intervention measures. This should reduce the burden on the healthcare system and help to prevent other complications, including sepsis, long-term disability, recurrent cellulitis and possible acute rheumatic fever and acute post-streptococcal glomerulonephritis14-17.
Most outpatient presentations for SSTIs were in the outer islands, compared with emergency department presentations, which were mostly by Waiben residents. This reinforces the value of the primary healthcare centres in remote communities, which are typically staffed by remote area nurses and Aboriginal and Torres Strait Islander Health Workers. Ensuring adequate primary care resources on Waiben would also reduce the burden of unnecessary SSTI presentations to the emergency department.
Over a third of emergency department episodes and over half of inpatient episodes were from outer island residents. For both emergency department and inpatient episodes, patients required aeromedical retrieval or commercial flight transfer from their outer island home to hospital on Waiben. This is a huge additional financial impost on an already-stretched healthcare system. A hospital-in-the-home (HITH) or telehealth service may represent a more cost-effective healthcare model. In other Australian metropolitan and regional settings, home-based care has proven to be safe and highly cost-effective18-20.
Previous community-driven skin health promotional activities have improved skin health knowledge; however, greater investment of resources is required21,22 Strengthening of primary care services might expedite the earlier treatment of SSTIs while also potentially reducing the burden of comorbidities that drive the high incidence of SSTIs in the region. The savings from reduced retrieval, emergency and inpatient costs could be used to support other health priorities in the region including metabolic syndrome, macrovascular disease, dementia and chronic kidney disease3,23,24. Improving housing and addressing overcrowding remain priorities in this region and across northern Australia and are critical in preventing SSTIs and other infectious diseases25,26.
This study has several limitations. First, we were unable to obtain complete demographic details from some of the healthcare settings. Second, this study did not examine indirect costs of SSTIs such as work and school absenteeism, relocation away from home and family for SSTI treatment and mental health. It is time for a multicentred prospective study exploring these indirect costs – and how we might avoid them – while providing highest quality care. Finally, mean hospital costs were based on national data and we acknowledge that there is large variability in these costs between national and state-based estimates.
Conclusion
The management of SSTIs in the Torres Strait places a substantial resource and financial burden on local health services and the regional health system. Preventative and primary care measures such as skin health promotion programs, expanded telehealth, a HITH service and the addressing of comorbidities that drive the incidence of SSTIs have the potential to reduce their impact in this region. This may also enable the reallocation of necessarily finite resources to other local health priorities.
Acknowledgements
We acknowledge all the Torres and Cape Hospital and Health Service staff who assisted in patient enrolment and project support. We thank Peter Horne for assistance with the production of Figure 1.
Funding
This research was funded by the Emergency Medicine Foundation (grant number EMJS-300R30-2018-HEMPENSTALL), the Australian National Health and Medical Research Council (grant numbers 1046812, 1098337 and 1131932; the HOT NORTH initiative), One Disease and James Cook University. All researchers were independent from the funding bodies and had full access to all the data in this study.
Conflicts of interest
The authors declare no conflicts of interest.

