Because of the vastness of the Australian continent, people who live in remote areas are quite disadvantaged where medical help is concerned. In the 1999 'Bush Talks' sponsored by the Human Rights & Equal Opportunities Commission, inadequate, inaccessible, and diminishing health services emerged as the principal issues1:
The health of populations living in rural and remote areas of Australia is worse than the health of those living in capital cities and other metropolitan areas... [and] ...mortality and illness levels increase as the distance from such centers increases2.
In rural areas, death rates from most causes are higher, and rural Australians are more likely to suffer from coronary heart disease, asthma, diabetes and many other conditions3.
Relatively poor access to health services, lower socioeconomic status and employment levels, exposure to comparatively harsher environments and occupational hazards contribute to and may explain most of these inequalities4. At the same time, the supply of GPs falls sharply in rural and remote areas, and overall hospitalization rates are highest for those living in remote zones5. Rural dwellers have to travel long distances to see their GP. Patients who aren't well enough to travel simply have to put up with the situation or use expensive ambulance services. Those with chronic conditions may have to leave their homes and live in the city.
An approach to the problem
One of the objectives of the University Departments of Rural Health (UDRH) is to develop innovative service-delivery models to meet the needs of those in rural and remote areas. This involves undertaking research into rural and remote healthcare issues, by collaboration with local healthcare providers.
The disadvantages of ill-health are two-fold: the suffering of the patient and the cost to the community specifically in terms of hospitalization. The former is exacerbated when the patient lives in a remote area. Telemetric assessment and monitoring offers the possibility of impacting on both of these problems.
In rural and remote areas there are generally local residents who are prepared (and indeed keen) to serve the community6. In fact, community involvement enhances the health and wellbeing of volunteers7. A videophone system similar to the one we will describe has already been used for emergencies in the Otway Ranges of Victoria8. Recently the authors have begun training local volunteers to take part in a 'virtual clinic' for simulated non-emergency cases.
Various Remote Patient Monitoring (RPM) strategies have been devised by health authorities to keep people out of hospital 9,10. In Victoria, Australia, the Department of Human Services (Health Department) has developed the Hospital Admissions Risk Program (HARP)11. One aspect of this program is to investigate technologies that might help keep people out of hospital. The system described here was recently discussed at a HARP Technology Workshop11.
Remote monitoring
Due to remarkable advances in technology, telemetric assessment and monitoring of patients has been extensively investigated in recent years. Various sensors combined with either Internet or broadband carrier systems have enabled physiological parameters such as blood pressure and ECG to be monitored and transmitted automatically to hospitals. Such systems are generally expensive. Transmission of clinical data by ordinary phone line has become of interest. For example, it was found that follow-up visits (after surgical procedures) in patients' homes could be satisfactorily accomplished by transmitting low resolution video and high resolution still images over standard telephone lines12. Such transmission is practical and cheap, and people with limited education can facilitate such evaluations13. In another study on the use of low-bandwidth, low-cost telemedicine consultations, all categories of participants noted very high levels of satisfaction14.
The telephone has commonly been used in sparing 'home visits' to people in remote areas. However, doctors are often dissatisfied with the telephone-only consultation, and the lack of visual cues has been offered as a major reason for this unease15. The low bandwidth videophone offsets this lack, and has a place in clinical practice. Tangible benefits expected from such low-end video interaction are two-fold: a contribution to clinical assessment and improved social interaction16.
A virtual clinic - our model
The small pilot study described used an 'off-the-shelf' videophone (MotionMedia 125; Videophone Communications Pty Ltd; Melbourne, Vic, Australia) which has a freeze function, as well as the capability for the operator to control frame rate to adjust balance between smoothness (motion) and clarity (detail). This videophone also has a port to take a second camera. If a digital camera is used, a much better quality video is achieved, which together with the freeze mode gives surprising detail to the remote observer (Figs 1,2).

Figure 1: The degree of detail obtainable via videophone using ordinary phone lines.

Figure 2: View of 'patient' in video, as seen after the signal has traversed ordinary phone lines.
While the visual component described is important in clinical assessment over a distance, local volunteer attendants can be trained to acquire considerable medical data for either real-time or store-and-forward transmission to the clinician. There is considerable literature on the value of lay assistants in this context17,18. In the present study, volunteers were recruited by local advertisement, and trained and supervised by staff at The Greater Green Triangle (GGT)Deakin/Flinders UDRH. Lay volunteers can be trained readily to measure blood pressure (using, for example, an Omron T8 [JA Davey Pty Ltd; Melbourne, Vic, Australia] automatic sphygmomanometer), perform basic lung function tests (using a portable automatic spirometer such as the Cosmed 'Pony' T8 [Cosmed; Rome, Italy]), perform an ECG (such as Philips PageWriter 10i [Philips Australasia; Sydney, NSW, Australia]) and even to acquire heart and lung sounds using a digital stethoscope (Stethographics Inc; Boston, MA, USA). All this is performed under the supervision of the doctor who is on-line via the videophone. Other 'peripheral' adjuncts which the authors use include pulse oximeter, tympanic thermometer, glucometer, dipstick urinalysis, scales for weight records, otoscope, laryngoscope or alternatively flavoured spatulas and a digital camera (Fig 3). The authors' attendants have also been trained to use 'BabyCheck'19 when presenting an infant to a doctor. The community volunteer completes a Virtual Clinic Patient Care Record (Fig 4).
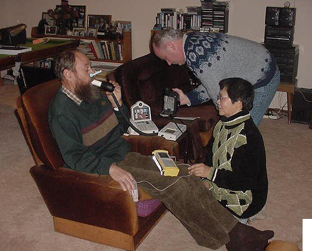
Figure 3: Local volunteer attendants acquire clinical information from a simulated patient. The doctor can be seen supervising via videophone.
Figure 4: Patient care record used by attendants in the 'virtual clinic'.
The pilot (in progress at the time of writing) links three local GPs with four trained lay attendants in a series of simulated common medical cases. The intention is to establish the level of satisfaction which the doctors can reach, not only in terms of 'seeing' the patient, but also in their confidence level in the medical data the attendants acquire. While it was not envisaged that real cases would be undertaken in the current stage, nevertheless a few successful 'virtual clinics' have been conducted in such cases as a psychiatric review, a child with cough (the doctor was able to examine tonsils and posterior pharynx), the monitoring of patient with congestive heart failure, and an elderly woman with a prolapsed uterus. Preliminary results suggest that a doctor can obtain a satisfactory view of a remote 'patient' under the conditions described above, and that lay attendants can acquire and present (under supervision via videophone), reliable and useful medical information.
In a real situation, a patient in a remote area would initially contact his/her GP. If the patient is too unwell to travel in to the clinic, the GP may advise a 'virtual consult'. The patient or carer then contacts local attendants who arrange a time suitable to patient and GP. The attendants visit and assess the patient, then initiate the 'virtual clinic' at the appropriate time. The GP simply sits at the videophone in his/her clinic.
Consultations would normally take place in patients' homes. The potential is there, however, for expansion to a 'call-in centre' which may be in the local community hall or school, or possibly at one of the attendants' homes. The equipment is portable and in the present model consists of two carry-bags containing the videophone and 'peripherals'. While the authors have used equipment donated by medical suppliers for the study, the total cost of two videophones (one for the GP and one for the attendants) and instruments described above is currently approximately AU$15 000.
Evaluation
Staff at the GGT UDRH have provided videophones at two other sites for the purposes of generating data for statistical evaluation. One site is in far eastern Victoria, the other in outback New South Wales, Australia.
Literature on the cost-benefit evaluation of telemedicine is limited and conflicting. For example, one study compared hospital and home-based treatment models for acute exacerbations of chronic obstructive pulmonary disease, and found that home-based costs were significantly less than hospital-based costs20. Another study found that 'virtual outreach' was more costly to the National Health Service, although less costly to patients21. That particular outreach, however, involved GP and specialist and was, therefore, different from the system described in the present article.
Should the responses from GPs be positive in this small pilot, the next step will be to set up a larger, controlled trial. The aim would be to compare outcomes between cohorts using the 'virtual clinic' system described for real medical cases, and cohorts not using the system. Ethics approval would be sought. GPs would be sought who practise in remote areas. Attendants would be recruited by local advertisement, and appropriate patients monitored as they presented.
In summary
While the pilot 'virtual clinic' is still in the evaluation stage, the authors believe that in most isolated communities it should be possible to train a few volunteers along the lines described. With low-cost equipment volunteers may be able to save their neighbours long trips into town to see the GP. With such remote monitoring, patients may be able to avoid going to hospital or to come home sooner than would otherwise be possible. This should save on ambulance and hospital costs, quite apart from patient satisfaction.
Acknowledgements
The authors wish to acknowledge the technical assistance of Elizabeth Meade throughout the program; also acknowledged is the time and advice of Dr Peter Barnett, Royal Children's Hospital, Melbourne, and Drs Steve and Veronica Fitzgerald and Warwick Rouse, general practitioners.
References
1. Anon. Bush talks. Human Rights & Equal Opportunities Commission Report, ISBN 0 642 26961 0; 1999; 3.
2. Australian Institute of Health and Welfare. Health in rural and remote Australia. Canberra: AIHW, 1998; 14.
3. Australian Institute of Health and Welfare. Health in rural and remote Australia. Proceedings, National Rural Public Health Forum, National Rural Health Alliance. 1997; 1.
4. Australian Institute of Health and Welfare. Australia's Health 2000. Canberra: AIHW, 2000; 223.
5. Australian Institute of Health and Welfare. Health in rural & remote Australia. Cat. No. PHE 6. Canberra: AIHW, 1998.
6. O'Meara P. The prehospital community-volunteer model has a place in rural Australia. Journal of Emergency Primary Health Care 1: 43. (Online) 2003. Available: http://www.jephc.com/ (Accessed 1 July 2004).
7. Savage SA, Bailey SR, O'Connell B. Health status and participation in a range of activities in an Australian community. Rural and Remote Health 3: 154. (Online) 2003. Available: http://rrh.org.au (Accessed 24 June 2004).
8. Meade B, Barnett P, Walker T. Right technology, right situation - a case report in prehospital telemedicine. Journal of Emergency Primary Health Care 1: 56. (Online) 2003. Available: http://www.jephc.com/ (Accessed 1 July 2004).
9. Kornowski R, Zeeli D, Averbuch M et al. Intensive home-care surveillance prevents hospitalization and improves morbidity rates among elderly patients with severe congestive heart failure. American Heart Journal 1995; 129: 762-766.
10. de Toledo P, Jimenez S, Del Pozo F. A telemedicine system to support a new model for care of chronically ill patients. Journal of Telemedicine and Telecare 2002; 8 Suppl 2: 17-19.
11. Department of Human Services (Vic). Hospital admissions risk program (HARP) Technology working party report. (Online) 2003. Available: www.medgraphics.cam.ac.uk/downloads/TECHRPT.pdf (Accessed 5 July 2004).
12. Rosser J, Prosset R, Edga B, Rosser L, Murayama M, Brem H. Evaluation of the effectiveness of portable low-bandwidth telemedical applications for postoperative follow up: initial results. Journal of the American College of Surgeons 2000; 191: 196-203.
13. Field M, Grigsby J. Telemedicine and remote patient monitoring. JAMA 2002; 288: 423-427.
14. Norris TE, Hart GL, Larson EH et al. Low-bandwidth, low-cost telemedicine consultations in rural family practice. Journal of American Board of Family Practice 2002; 15: 1233-1237.
15. Foster J, Jessop L, Dale J. Concerns and confidence of general practitioners in providing telephone consultations. British Journal of General Practice 1999; 49: 111-113.
16. Howard A. Clinical call centers: does low-bandwidth have a place? Journal of Telemedicine and Telecare 2001; 7: 14-16.
17. Thomas AD, Maclean JR. Design of a clinical data-collection form for remote health care. Journal of Telemedicine and Telecare 1995; 1: 209-216.
18. Jerant AF, Azari R, Nesbitt TS et al. Reducing the cost of hospital admissions for congestive heart failure. A randomized trial of a home telecare intervention. Medical Care 2001; 39: 1234-1245.
19. Morley CJ, Thornton AJ, Cole TC, Hewson PH, Fowler MA. Baby Check: a scoring system to grade the severity of acute systemic illness in babies under six months. Archives of Disease in Childhood 1999; 66: 100-105.
20. Nicholson C, Bowler S, Jackson C, Schollay D, Tweedale M, O'Rourke P. Cost comparison of hospital and home-based treatment models for acute chronic obstructive pulmonary disease. Australian Health Review 2001; 24: 181-187.
21. Jacklin PB, Roberts JA, Wallace P et al. Virtual outreach: economic evaluation of joint teleconsultations for patients referred by their general practitioner for a specialist opinion. BMJ 2003; 327: 84.

