Introduction
Heart failure (HF) is a serious health condition currently affecting 5.8 million Americans1. In addition to causing significant morbidity, high hospitalization rates and decreased quality of life, HF is associated with high mortality with 1-year case fatality as high as 22%2. Among veterans, HF is the most frequent cause for hospital admission and readmission3. Dual use, defined as veterans enrolled in VA care who also received care from non-Veterans Affairs (VA) providers and facilities, has also been associated with increased rates of hospitalization, readmission, and mortality4. Dual use occurs frequently in veterans, carries the potential to be less efficient, less safe, and is likely increasing as a result of the Veterans Choice program5-7. Many veterans live in rural areas where access to care may be limited, and rural veterans may seek non-VA care for reasons different than those of urban veterans8-10. For example, given decreased primary care access, rural veterans may forego treatment in certain situations where their urban counterparts would present for care. Alternatively, during an acute event rural veterans may be more likely than urban veterans to receive care from a non-VA facility. Hence, differences in care patterns between rural and urban veterans may influence the association between dual use and outcomes. Therefore, this study aimed to determine the extent to which rurality modifies the association between dual use and ED visits, hospitalizations, and 30-day hospital readmissions.
Methods
A state-level cohort of veterans with HF receiving primary care from the Veterans Health Administration (VHA) was constructed by linking multiple patient and administrative files from the VHA, Medicare, and the Carolina Office of Revenue and Fiscal Affairs. Details of cohort construction have been previously published4. Subjects were categorized as having HF if they had one or more inpatient or outpatient diagnoses for HF in a given year (International Classification of Disease codes ICD-9 402.01, 402.11, 402.91, 429.3x, 425.xx, 428.xx). Patients with HF who were classified as dual users or VA-only users were included in a final analytic dataset (N=4985) if they had at least one episode of care for an emergency department (ED) visit or hospitalization during the study time period. Subjects were further categorized based on where they received acute ED and/or hospital care as VA-only users or dual users, which served as the primary exposure. Subjects were followed until death, loss to follow-up, or until December 2011.
Primary outcomes for this analysis were counts for ED visits for any primary diagnosis and for HF as a primary diagnosis, hospitalizations for any primary diagnosis and for HF as a primary diagnosis, 30-day all-cause readmission for HF as primary diagnosis, and 30-day hospital readmission for HF as the primary diagnosis at readmission. A main focus of this analysis was to determine whether rural–urban status modified the association between dual use and study outcomes of interest.
Covariates
The primary exposure of interest was dual use. Rural–urban residence acting as a potential modifier of the relationship between dual use and outcomes of interest was the primary covariate of interest. Rural–urban residence, as defined using Rural Urban Commuting Area (RUCA) codes, classified veterans as living in urban, rural and highly rural areas with veterans in rural and highly rural areas being combined into a single group. Additional covariates were age, gender, race/ethnicity, marital status, and service connected disability. Service connected disability is a marker for disease burden, has implications for copayments within VHA, and has been used in prior investigations of veteran patients11,12. Comorbidities were measured using the Elixhauser classification system and classified as present or absent for each patient13.
Statistical analysis
Due to the zero inflation in the study count outcomes leading to overdispersion (ie when the variance is greater than the conditional mean)14, a negative binomial framework was used to study the association between dual use and HF-related ED visits, hospitalization, and hospital readmission15,16. Zero-inflated negative binomial (ZINB) models were used, which are a mixture of a negative binomial model for the count outcome (including some zeros) combined with a logit model to determine the probability for excess zeros. The parameters in the ZINB model have conditional or latent class interpretations, which correspond to a susceptible subpopulation at risk for the condition (in this case ED visit, hospitalization, or readmission) with counts generated from a negative binomial distribution and a non-susceptible subpopulation that provides the extra or excess zeros17. Stepwise variable selection was used based on statistical information criterion18. Model fit was checked using residual diagnostics and plots. All analyses were done in SAS PROC COUNTREG 9.4 (SAS Institute; http://www.sas.com).
Ethics approval
This project was approved by the VA Central Institutional Review Board (Approval 13-22) as well as the local research and development committee.
Results
Of the 4985 veterans with HF with ED visits or hospitalizations during the study time interval who were either dual users or received all of their care at the VA (VA-only), 2923 resided in urban areas while 2062 resided in rural or highly rural areas with dual use being similar across rural and urban veterans (Table 1). Compared to urban veterans, rural and highly rural veterans were of similar age, had a similar racial-ethnic distribution, were more likely to be male (98.6% v 97.2%) and were more likely to be married (58.5% v 54.6%). With respect to comorbidities, compared to urban veterans, rural and highly rural veterans were more likely to have diabetes (65.3% v 62.2%), but less likely to have psychoses (15.0% v 17.8%) or substance abuse (24.0% v 28.8%).
Interaction terms were used to model the association between dual use and all-cause ED visits, hospitalization and 30-day hospital readmission in rural/highly rural and urban veterans (Table 2). The association between dual use compared to VA-only use and ED visits was stronger in rural/highly rural veterans ((rate ratio (RR)=1.28 (95% confidence interval (CI): 1.21,1.35)) than in urban veterans (RR=1.17 (95%CI: 1.11,1.22)) (interaction p-value=0.0109), while the association between dual use and all-cause hospitalizations was similar in rural/highly rural veterans (RR=2.00 (95%CI: 1.87,2.14)] and in urban veterans (RR=1.87 (95%CI: 1.77,1.98)). The association between dual use and all-cause 30-day hospital readmission was also similar in rural/highly rural veterans (RR=1.89 (95%CI: 1.77, 2.02)) and in urban veterans (RR=1.78 (95%CI: 1.68,1.88)). When outcomes were limited to ED visits, hospitalizations and 30-day hospital readmissions where HF was the primary diagnosis the association between dual use as compared to VA-only use was similar in rural/highly rural veterans and urban veterans (Table 2).
Table 1: Characteristics of rural/highly rural versus urban subjects with heart failure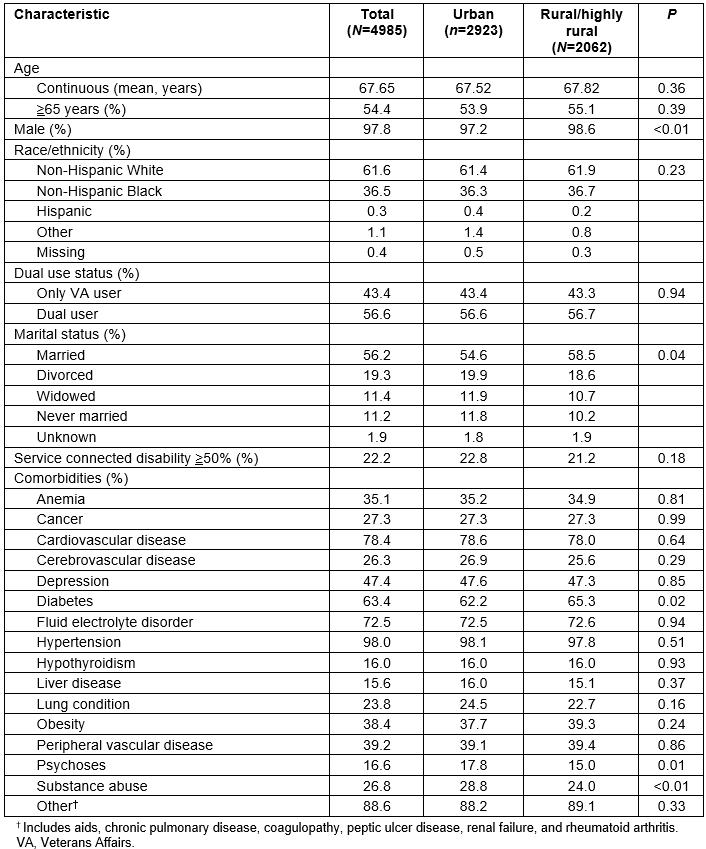
Table 2: Effect of dual use versus Veterans Affairs-only use† on emergency department visits, hospitalizations, and 30-day hospital readmissions in veterans living in rural/highly rural areas and in veterans living in urban areas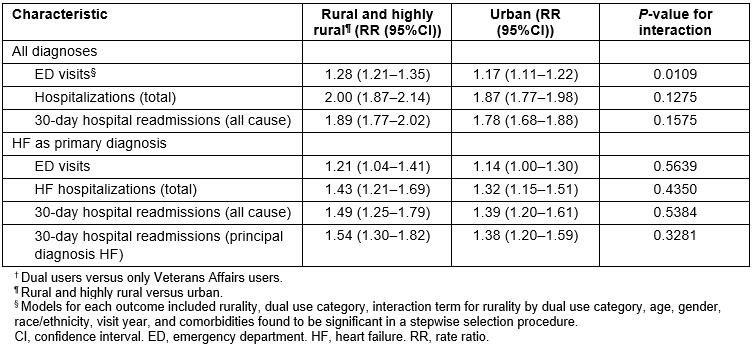
Discussion
Poorer access to care may affect both VA and non-VA facilities for rural veterans with HF. With the exception for the case of all-cause ED visits, when analyzing a cohort with information on both VA and non-VA acute healthcare utilization, rural residence was not observed to significantly modify likelihood of acute healthcare utilization when comparing dual users to VA-only users. Moreover, the prevalence of dual use as defined in this study, focused on hospitalizations and ED visits, was similar in rural and urban veterans. In contrast, with respect to outpatient care, rural veterans have been observed to rely on Medicare more for primary care and on VA services for specialty and mental health care8.
Over one-third (ie 36%, 3.1 million) of veterans receiving care from the VHA live in rural or highly rural areas and often face barriers to access related to travel distance. Since 2014, the Veterans Choice Program has expanded eligibility for community care to veterans, especially for outpatient primary care and specialty care in veterans facing long wait times greater than 30 days or long travel distances greater than 64 km (40 miles). However, the Veterans Choice Program has also led to estimated increases in non-VA hospital use. West and colleagues analyzed all-payer claims data from eight states and estimated an average 8.2% increase in non-VA hospitalizations associated with Veterans Choice, with increases as high as 17–18% in states with higher proportions of rural-dwelling veterans19.
Limitations of the study include potential unmeasured differences between patient populations as well as the potential for reverse causality if veterans who utilize more health care are also more likely to be dual users. Comorbidity profiles between rural/highly rural and urban veterans were somewhat different, although these differences were accounted for in regression models. Finally, this analysis might have been strengthened through inclusion of information on the severity of HF such as New York Heart Associate class or ejection fraction, but such information was not available in the datasets examined.
Conclusion
Dual use appears to be a marker for higher healthcare utilization and worse outcomes for both urban and rural veterans, but rurality appears to modify the effect of dual use on rates of ED visits for HF. These findings have clinical and healthcare policy implications as VA develops interventions to address this higher risk. For example, while a wide variety of disease management programs have been developed for HF and other chronic diseases prone to acute exacerbation, few if any address receipt of cross-system care20,21. Additional attention to care coordination across healthcare systems, especially in rural patients, is warranted.
Acknowledgements
This work was supported by the Department of Veterans Affairs, Veterans Health Administration, Health Services Research and Development, Office of Research and Development (IIR 12-331, Axon-PI). The contents of this article do not represent the views of the Department of Veterans Affairs or the United States Government.
