Introduction
Agrichemicals are commonly used as a defence against plant and insect pests that reduce production in agricultural industries. These pests can have a significant impact on the yield of crops, pasture and animal production. During 2012–2013, approximately $350 billion was spent on insecticides (the group of agrichemicals targeting insects) by Australian agricultural industries1. Pesticide use remains high due to the risks associated with potential loss of production to the cropping industry if farmers did not use insecticides2.
Organophosphates are one of the most common and effective insecticides in the agricultural industry3. Due to the growing resistance of insects and parasites to other forms of pesticide, the use of organophosphate chemicals remains widespread in the agricultural industry due to their broad spectrum efficacy4.
The mode of action of organophosphates is inhibition of the enzyme acetylcholinesterase. Acetylcholinesterase is essential for the regulation of the nervous system within organisms. Organophosphates lead to the eventual death of insects by irreversibly preventing nervous conduction2. The human nervous system is affected by organophosphates in a similar manner.
The acute effects of organophosphates are well researched. High-level acute exposure is known to result in the inactivation of acetylcholinesterase, causing unregulated release of acetylcholine. Acute symptoms include blurred vision, lacrimation, salivation, bronchorrhea, pulmonary oedema, nausea, vomiting, diarrhoea, confusion, convulsions, loss of consciousness and respiratory distress5.
However, less is known about the chronic health effects of organophosphates and whilst there have been a number of studies examining the chronic effects, few have been conducted using longitudinal studies6. The detrimental effect of organophosphates to users was, however, identified as early as 1951. Zuckerman, in a report to the British Minister of Agriculture and Fisheries in that year, recorded that organophosphorus compounds aroused apprehension, and noted that repeated absorption of organophosphate may result in cumulative poisoning7.
Most of the available research on organophosphates is focused on the issues of acute poisoning and exposure. However, it is important to understand the chronic health effects specifically for the farmers who have been using those agrichemicals for years without being aware of the health hazards. Therefore, the objective of this narrative review was to examine the literature focusing on chronic health effects – both neurological and non-neurological – of prolonged exposure of organophosphates.
Methods
For this narrative literature review, three databases were used to search for relevant articles focusing on the chronic health effects of prolonged exposure of organophosphates: Medline, Web of Science and Scopus. The following key words were used: 'organophosph* AND farm* OR agri* AND chronic OR long term AND health'. Inclusion criteria applied for the search were English language and humans, with no limit for dates. The last search was conducted on 6 December 2018. Most of the articles focused on neurological consequences; however, there are some non-neurological studies. Articles were separated into neurological and non-neurological consequences of chronic exposure of organophosphates. Chronic exposure was defined as exposure to organophosphates for 6 months or more in an agricultural setting.
For the neurological effects, the search term 'AND neuro*' was added to existing search terms. It produced 61 articles in Medline, 166 articles in Web of Science and 51 articles in Scopus. Results of each of these searches were then manually sorted with the following exclusion criteria:
- follow-up after an acute poisoning event study
- study where there was a generic exposure to chemicals – not organophosphates specifically
- subjects who weren’t exposed to organophosphate in an agricultural setting
- exposure less than 6 months.
When the duplicates were removed and the grey literature and reference lists of the retrieved articles were reviewed, there were 50 articles in total focusing on neurological effects of organophosphate exposure (Table 1).
Neurological consequences were separated into four categories as identified by common themes in this review:
- neurobehavioural: of or relating to the relationship between the action of the nervous system and behaviour
- neurodegenerative: relating to or marked by degeneration of nervous tissue
- neurodevelopmental: relating to development of the nervous system
- neurological signs and symptoms: signs and symptoms relating to the nervous system8.
For the non-neurological consequences, the previous addition was replaced by 'NOT neuro*' and 89 articles were extracted from Medline, 224 from Web of Science and 51 from Scopus. After de-duplication and careful filtering, there were 17 articles in total focusing on the chronic non-neurological effects of organophosphate exposure (Tables 2–7). The process of article selection for this review is depicted in Figure 1. The non-neurological category was divided into common themes: respiratory symptoms, increased cancer risk, endocrine disruption, cardiac issues, chronic fatigue and infertility.
Table 1: Literature review of neurological studies9-58
Table 2: Literature review of respiratory studies59-67
Table 3: Literature review of cancer studies68-70
Table 4: Endocrine study in the literature review71
Table 5: Cardiac study in the literature review72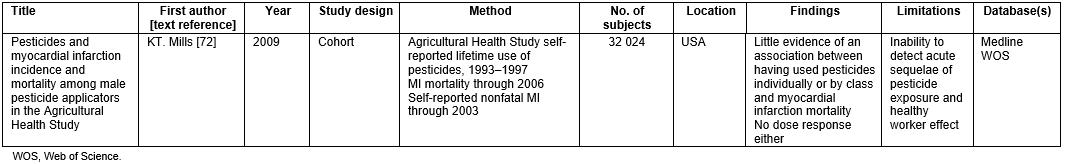
Table 6: Chronic fatigue study in the literature review73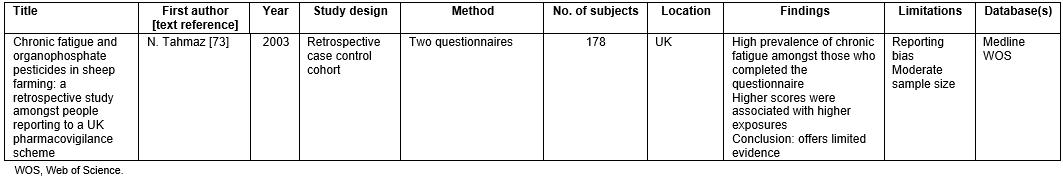
Table 7: Literature review of fertility studies74,75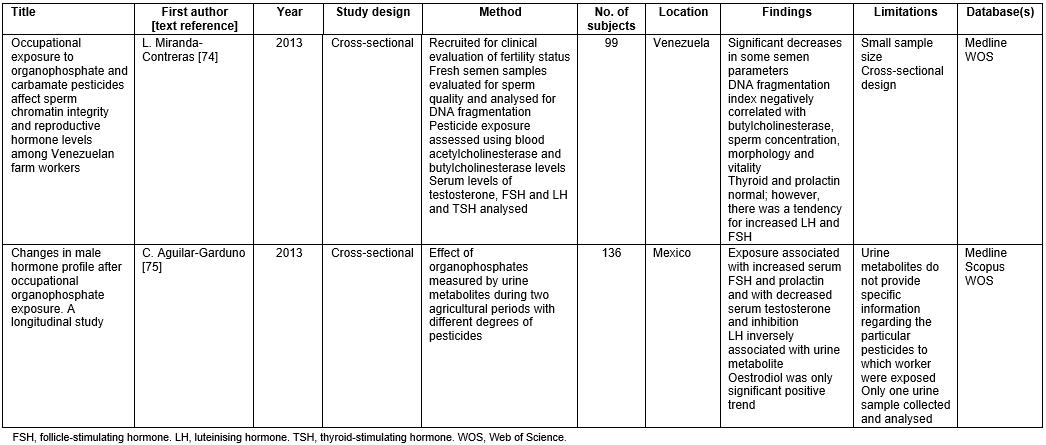
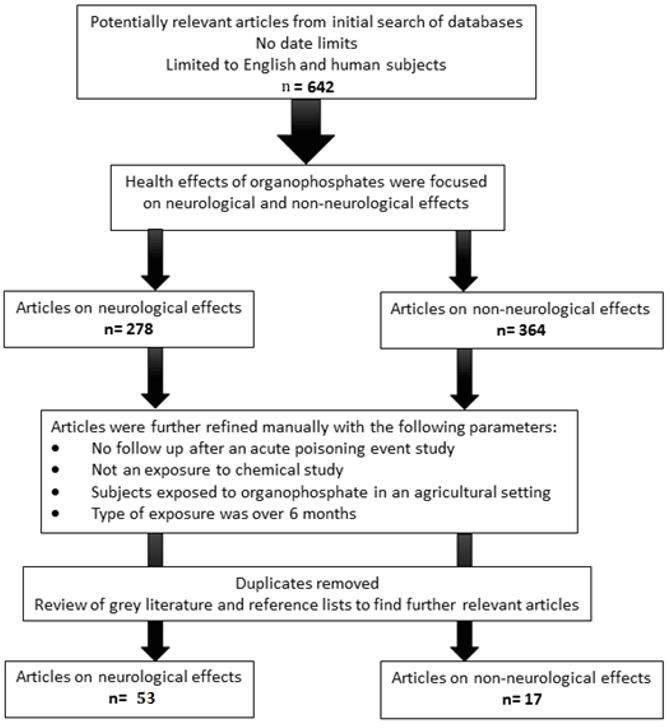 Figure 1: Flow diagram of the selection process of the articles for the narrative literature review.
Figure 1: Flow diagram of the selection process of the articles for the narrative literature review.
Results
Neurological changes were the most studied chronic health effects of prolonged exposure to organophosphates. The research was focused on neurobehavioural, neurodegenerative, neurodevelopment and neurological signs and symptoms. The majority of these studies were conducted in the USA and UK, with contributions from South Africa, Mexico, Spain, Thailand, Taiwan and Ecuador.
Neurobehavioural effects
The associations between chronic organophosphate use and neurobehavioural symptoms have been researched in 31 studies9-29. Eight of these articles reported a deficit on neurobehavioural batteries (a group of tests performed together for assessment purposes) when there was previous exposure to pesticides 9,10,12-15,17,18,20,21,24-29. Deficits were found in short-term memory components, with partcipants scoring significntly lower on the Digit Span (forward and reverse recall of digit sequences) and Match-to-Sample tests (matching to previously demonstrated stimuli)9,10,12-15,17,18,20-22,24-29. Attention span was also found to be affected in two studies9,18.
Three studies did not find a significant effect on neurobehaviour with prolonged organophosphate exposure. One study from South Africa showed a slight effect but was explained to most likely be the result of misclassification of exposure11. Another study from Iran found no neurobehavioural deficits19. The third study, with children from agricultural backgrounds in Thailand, showed no neurobehavioural deficits. However, a negative effect on work performance, although not significant, was demonstrated at times16.
Ten articles analysed the vulnerability to psychological conditions with chronic exposure to organophosphates, particularly referring to the general health questionnaire19,25,30,32-38. Two of the 10 studies noted an association with organophosphate exposure in farmers 25,36. The remainder did not find a significant relationship19,30,32-35,37,38. One study demonstrated a lower percentage of depressive symptoms amongst farm residents (20.6%) in Colorado, USA, compared to the general population (34%)33. This was more likely to be related to the healthy worker effect, as the farm population might be healthier due to their nature of work compared to the general population in that study33. The relationship of organophosphate pesticide chronic exposure with suicide was also examined30. This study reported no significant association between organophosphate exposure and suicide30.
Vulnerability to specific psychological conditions as a result of chronic exposure is not supported. Further, a 1996 Spanish study on agricultural workers reported that suicides in the farming populations were not caused by chronic exposure to organophosphate, rather it was the result of accessibility to this substance and decreased knowledge of the lethality30. This result is consistent within the Australian population, with MacFarlane et al demonstrating in their study a non-significant relationship between exposure and suicide39. Nine out of 10 articles reviewed were cross-sectional designs, thus stronger studies need to be conducted to support this theory.
Overall, short-term memory and attention were noted to have a significant difference for those who were chronically exposed to organophosphate. The levels of evidence according to the National Health and Medical Research Council (NHMRC) of the 21 articles reviewed in terms of short-term memory and attention were NHMRC III-2 and IV76. This was because they had a cohort or cross-sectional structure (Table 1). The number of subjects ranged from 48 to 917, which reduces the power of some of the individual studies. Compared to the other sections in this review, the section on neurobehavioural effects of organophosphates has the strongest evidentiary support. However, bias does come into effect as these do not account for educational and cultural backgrounds.
Neurodegenerative diseases
In relation to neurodegenerative diseases, three articles were identified40-42. The two disorders described were Alzheimer’s disease and Parkinson’s disease. Two of the articles related to Alzheimer’s disease and both of them showed a positive association between chronic exposure to organophosphates and Alzheimer’s disease40,41. Zaganas et al described a possible theory for the causal relationship: that excess synaptic acetylcholine leads to chronic excitation of the post-synaptic neurons, which causes excitotoxic damage and degeneration of the cholinergic system77.
Chronic exposure of organophosphate has been linked to Parkinson’s disease. One study investigated the relationship between Parkinson’s disease and chronic exposure and found a positive relationship that was not significant (odds ratio (OR) 1.56, 95% confidence interval (CI) 0.95–2.58)42. The same article concluded that being acutely poisoned was a more significant indicator for likely development of Parkinson’s disease42.
Short-term memory problems have previously been shown to be associated with chronic exposure to organophosphates77. This may explain the increased incidence of Alzheimer’s disease in the population, as this disease initially affects short-term memory. The level of evidence of the two articles reviewed was NHMRC IV, which does not provide strength to the theory.
Overall, compared to the Alzheimer’s disease articles, the Parkinson’s disease article had a clearer design structure and higher number of subjects, making it a powerful study.
Neurodevelopmental diseases
Neurodevelopmental effects from chronic exposure to organophosphate were found in three of four articles29,43-45. Three articles described an effect on neurodevelopment when exposed to organophosphates in the prenatal period29,43. The effects were on both neurobehaviour and IQ, with one study showing a seven-point decrease in IQ at the age of 7 years when there was a prenatal chronic organophosphate exposure43. Another study looked at effects of exposure in the post-natal stage and found neurodevelopment of boys in the group was significantly reduced, by two standard deviations44. An article by Fortenberry et al described a relationship between prenatal exposure to organophosphates and the development of attention deficit hyperactivity disorder. The authors found no association but concluded that more research was needed in that area because the study had limited power45.
Overall, chronically inhibiting the acetylcholinesterase during the prenatal period has been shown to affect nervous system development. The strength of this conclusion was mostly supported by cohort designs, with three of the four studies being of NHMRC level III-2 (Table 1).
Neurological effects
Fourteen articles described neurological symptoms related to chronic exposure of organophosphate pesticides36,46-58. Seven studies looked into neurological findings from physical examinations47-49,52,54,55,57. A study with a focus on sheep farmers exposed to organophosphates in the UK reported a significant difference (p=0.011) between the most symptomatic farmers, least symptomatic (asymptomatic) farmers and quarry workers (non-farmers) with two-point discrimination (the distance required to determine that two points are separate when pressed on the skin) highest in the symptomatic farmers47. Another UK study found the intensity of the concentrate of organophosphate as the significant factor (p=0.005) involved in the development of neurological symptoms, which was independent of the duration of exposure49. A study in the USA found toe proprioception (detection of toe movement with eyes closed) to be significantly different between controls and farmers exposed to organophosphate52. A South African study found no association between organophosphate pesticide use and neurological deficit in relation to vibration sense or tremor48.
Some articles reported results of nerve conduction studies performed to assess chronic effects of exposure. Five studies examined this in different areas of the body46,53,54,56,58. Four of these studies showed significant differences in nerve conduction results between farmers and controls53,54,56,58. These studies demonstrated the difference in distal latencies and wave amplitude of peripheral nerves53,54.
Neurological symptoms were detailed in four studies43,48,50,51. Each of these studies reported that people applying organophosphates were more likely to report neurological symptoms in comparison to controls. These symptoms included dizziness, sleepiness, watering eyes, altered sensation and headache43,48,50,51. In one study, organophosphate-induced neurotoxicity was detailed, with described symptoms including insomnia, headache, anorexia and numbness51.
In the abovementioned studies, chronic organophosphate exposure had some effect on the peripheral nervous system but the symptoms, signs and nerve conduction studies revealed inconsistent results. The level of evidence presented for the 14 articles reviewed were weak in their design as they were mostly cross-sectional studies (Table 1). Further investigations need to be conducted to understand a consistent pattern to chronic health effects of organophosphate pesticides.
Non-neurological effects
Studies involving farmers focusing on the non-neurological health effects of exposure to organophosphates reported on respiratory symptoms, cancer risk, endocrine disruption, cardiac issues, chronic fatigue and infertility.
Respiratory conditions were detailed in nine articles59-67. Six of these articles reported significant associations between respiratory conditions and organophosphate exposure59,60,62,63,66,67. Findings included symptoms such as wheeze and a decrease in lung function59,60,62,63,66,67. The three remaining articles reported inconsistency, indicating no correlation between prolonged exposure and asthma prevalence or spirometry changes61,64,65.
Three articles in the databases evaluated cancer risk associated with chronic organophosphate use68-70. All of them found positive associations. How et al reported that reduced blood cholinesterase levels from exposure to organophosphate pesticides was significantly associated (p<0.05) with an increase in chromosome breakage69. This has been linked to increased susceptibility of a person to develop cancer69. Another article reported an increased risk of chronic lymphoid leukaemia (OR 2.7, 95%CI 1.2–6.0)70.
One article reviewed the effects on the endocrine system in relation to diabetes prevalence. It reported a positive association between chronic exposure to organophosphate pesticides and prevalence of diabetes (OR 1.24, 95%CI 1.02–1.52)72.
One article looked into the incidence of myocardial infarction with exposure of organophosphate pesticides72. There was no significant evidence to show a relationship and no dose–response effect of organophosphates in relation to morbidity and fatality of myocardial infarct amongst farmers72.
There was only one article relating to chronic fatigue met the criteria outlined in the methods73. This article showed a high prevalence of chronic fatigue and organophosphate exposure amongst those who were exposed to organophosphates, but that finding was not strong due to the nature of the research conducted73.
Lastly, fertility was investigated in this review. Two studies showed a significant effect on this system74,75. One article demonstrated a significant decrease in the semen parameters, with decreased sperm concentration (p=0.002) and vitality (p<0.0001)75. Both articles highlighted an increase in follicle-stimulating hormones and luteinising hormones74,75. Neither study investigated effects on female fertility.
Discussion
The non-neurological health concerns of long-term organophosphate exposure were limited and involved predominantly NHMRC level IV except for the cardiac and endocrine articles, which were cohort studies. Possible areas of concern are respiratory, cancer, endocrine, chronic fatigue and fertility, but further investigations need to be conducted to determine if there is a significant effect due to chronic organophosphate exposure.
Methodological critique of articles reviewed
Summaries of each article, including their limitations, are shown in Tables 1–7. Of the 70 articles reviewed, 73% of articles were designed as cross-sectional studies. This is a weak research design being a level IV NHMRC level of evidence. One study by Fortenberry et al was a progressive study that tracked the progression of results45. This is a stronger research design as it excludes the influence of associating a casual relation from retrospective studies.
For the cross-sectional studies reviewed, the majority of the articles included less than 500 subjects, which means a study has minimal power. Six studies included more than 10 000 subjects, which enabled a good representation of study participants, including both farming populations and their controls, and increased the validity of the results44,45,50,63,71,72.
There were two documented methods, in the articles reviewed, to define organophosphate exposure: self-reporting and by geographical location/occupation. However, these methods allowed for reporting bias. Some articles also used questionnaires to report symptoms, increasing the bias of these studies47-54,59.
Furthermore, studies did not consistently represent one country, causing inconsistencies with environment and regulations of pesticides. Most represented among the studies were the UK and USA, providing a consistent environment across these studies9,10,12-15,20,22,25,27,33,34,39-47,49,50,52,55,57,60,63,65,71-73. However, more research is required for other countries including Australia especially as they have a large farming population.
Overall, the conclusions drawn from this literature review were not well supported – the majority of the studies had weak designs, limited power and confounders.
Applicability to Australia
Organophosphates are widely used in Australian agricultural settings and production methods1. Some changes to use and restrictions have occurred over the last decade through the regulatory agency the Australian Pesticide and Veterinary Medicines Authority. For example, a regulatory decision in December 2016 means a ban on the use of omethoate products in the garden at home, on food-producing plants, horticultural crops, pastures, grain legumes or cereals78.
Whilst no research from Australia fitted the present review’s selection criteria, there are still lessons to be taken from this research:
- Organophosphates may result in acute poisoning but have an accumulated exposure effect on human health.
- Chronic exposure to organophosphates appears to particularly affect the neurological system in particular cases.
- Handling organophosphates requires education and appropriate protective equipment to both prevent acute poisoning and reduce the risks associated with chronic accumulated exposure effects.
Limitations
The aforementioned findings are restricted by limitations of a standardised method of testing of organophosphate exposure and the methods of data collection. Only the agricultural population was investigated for this review. Therefore, other areas of population exposure to organophosphate such as fly spray, human head lice treatment, public health, vector control programs and other insect sprays were not included.
Conclusion
This literature review appraised relevant articles concerning the chronic health effects of organophosphate exposure between 1991 and 2016. Internationally, studies have suggested that chronic use of organophosphate affects neurobehaviour, neurodegeneration, neurodevelopment and the peripheral nervous system. Unfortunately, the methodological design of majority of the studies in this review were poor, therefore providing limited support for the results that were reported. Further research should be focused on early identification of an individual’s risk of organophosphate exposure and early detection of symptoms.
Global agricultural production continues to use organophosphate pesticides due to both increasing resistance of pests and the increased production pressures to feed and clothe growing populations. The use of organophosphates in Australia continues due to their efficiency as an insecticide in broadacre cropping, horticulture and livestock operations. Whilst restrictions for use have increased for this chemical group, organophosphates are unlikely to be discontinued in the short term. Understanding the consequences of prolonged exposure and establishing safety measures to prevent harm is critical to balance the demands of agricultural productivity with human health.



