Introduction
To fulfil medicine’s social mandate1 to produce physicians who can address the health concerns of the patients and communities they serve, family medicine residency programs provide physicians training opportunities to gain a wide range of skills and competencies. The vision of the College of Family Physicians of Canada (CFPC)2 is for physicians to provide a broad scope of family practice services to the populations they serve within the concept of a patient-centered medical home. To meet the social mandate and the educational goals of producing competent family physicians, training programs provide educational experiences that enable residents to build their own skill set through a variety of pathways.
In Canada, most universities have two programs: rural and urban. In urban family medicine programs, clinical experiences are based in large urban locations, whereas rural residency programs are based in rural areas. Rural family medicine training programs grew from one in 1973 to 12 in 2002, with the greatest increase occurring between 1997 (seven programs) to 2002 (12 programs)3. This growth was largely as a social accountability response to the shortage of family physicians in rural locations. There was also a perception that graduates from urban programs were not meeting the needs of rural populations4; therefore, rural residency programs are based on the premise that the appropriate skills and knowledge required for rural practice can best be acquired in rural environments5.
Residency training programs aim to ensure that residents are equipped with a broad range of skills sets by exposing them to diverse patient populations and to different care options in various settings (office, hospital, other healthcare facilities, rural and urban communities). While didactic and clinical teaching is often considered to be the main method of learning, other factors affect the creation of knowledge and acquisition of skills, such as mentors and the presence of role models. This combination of skills, knowledge-based and procedural, is a unique skill set that is also known as scope of practice.
The panel of skills or scope of practice is not immutable after completion of residency training. Research has shown that geographic factors (rural location, community size, distance to a large hospital) are strong predictors of scope of clinical practice6,7. Physicians who practice in rural locations have reported a broader scope of practice than those in urban locations, performing a wider spectrum of procedures, providing obstetrical and emergency care, and spending more time on patient care and on-call5,8-11. Recent data, however, has shown a declining trend over time in the provision of comprehensive care by family physicians in both urban and rural locations12 and in the number of rural physicians providing nursing home and obstetrical care13.
At present, Canadian accreditation standards do not differentiate between rural and urban family medicine program graduates in the expectations for proficiency and scope of care. There is an underlying assumption of equivalence of outcomes between rural and urban programs. The few published studies on rural family medicine program graduates have focused either on the location of practice or the broad nature of their practice. Rural program graduates have been found to be more likely to practice in rural areas than urban program graduates14. Compared to rural general practitioners who completed a rotating internship or an urban program, rural program graduates have reported feeling better prepared for the practice of family medicine in addressing common clinical problems, health maintenance, health promotion, psychosocial aspects illness, psychosomatic problem, emergency evacuation, and cross-cultural issues15. Comparisons of scope of practice between rural and urban training programs by practice location are lacking in the literature. An examination of the scope of practice of rural and urban program graduates would provide feedback for program planning and insight into similarities or differences between rural and urban training programs; in doing so, the examination of outcome equivalence could be explored. Such an analysis would also contribute to the literature by identifying factors that influence the development or maintenance of a generalist scope in family practice. As such, the purpose of this study was to compare the scope of practice of family medicine graduates who completed either an urban or a rural residency program by practice location.
Methods
Study design, participants and procedures
A retrospective, cross-sectional, self-administered survey was conducted of 651 graduates who completed family medicine residency training at the University of Calgary or University of Alberta during 2006–2011. The survey was carried out during July 2013 to December 2014 and each department mailed the surveys to their own graduates. Contact information for graduates was obtained from the Alberta Medical Directory or the Canadian Medical Directory. The study information letter, questionnaire and return post-paid envelope were mailed to each graduate. The questionnaires were numerically coded to enable follow-up of non-respondents, who were mailed a reminder notice and contacted up to five times by telephone, fax and/or email.
Setting
The family medicine residency programs at the University of Alberta and the University of Calgary are each 2 years in duration and offer training in urban and rural/regional settings. In 2000, the two universities established dedicated rural streams that, at the time of this study, were based in four regional centers in Alberta (Lethbridge and Medicine Hat for the Rural Alberta South (RAS) program at the University of Calgary; Red Deer and Grande Prairie for the Rural Alberta North (RAN) program at the University of Alberta). Residents in the RAN and RAS programs live in the regional settings in which they are based and also spend a considerable amount of time in smaller rural and remote communities for clinical experience. Residents in the urban program do clinical rotations in the cities of Calgary or Edmonton but are also required to spend a minimum of 2 months in a rural community in the second year of training. The requirement for a 2-month rural rotation was mandated for the first time by the College of Family Physicians of Canada in 200516. Table 1 outlines the 2-year clinical curriculum for both the rural and urban programs during the time the study cohort went through the residency program. Although the location of training differs, the rural and urban programs share a similar Triple C competency-based curriculum based on the requirements of the CFPC and focused on Comprehensive care, Continuity, and Centred in family medicine17. Generally, rural residents are exposed to more generalist physicians from many disciplines in regional hospitals with few specialty residents, while urban residents undertake hospital rotations in tertiary care hospitals under the supervision of specialists and their residents. For both programs, family medicine clinical experience is based in the community.
Table 1: Clinical curricula of rural and urban programs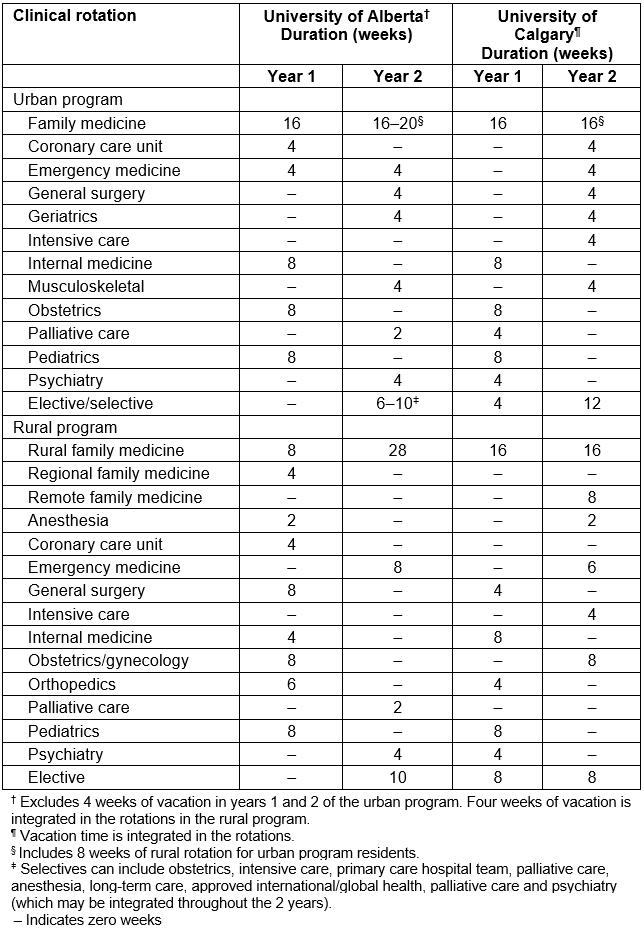
Questionnaire
The survey included questions on medical education and residency training, as well as career history and practice patterns after program completion. One question asked graduates to identify the route through which they obtained a family medicine residency position: urban program (CaRMS Round 1 or 2)18, rural program (CaRMS Round 1 or 2), Alberta International Medical Graduate (AIMG) Program19, Department of National Defence (DND), or other (eg transfers). Those who checked ‘rural program’ or ‘urban program’ were included in this analysis. Practice location was defined by the town/city in which the physician was practicing at the time of the survey. Scope of practice was ascertained through domains of care in four categories: (1) types of care, (2) clinical procedures, (3) practice settings, and (4) specific populations. Each element of the domains of care was rated on a five-point scale (1=‘not part of practice’ to 5=‘element of core practice’).
Data analysis
Rural program graduates were defined as those having entered family medicine residency training through the RAN stream at the University of Alberta or the RAS stream at the University of Calgary, in either CaRMS process round 1 or 2. Those who entered via the AIMG Program, DND, or by other routes were excluded from this analysis as the limitation of the questionnaire did not make it possible to identify whether these residents completed the urban or rural stream. Practice location was grouped as either rural (≤49 999 population) or urban (≥50 000 population); small sample size in some cells did not permit more refined analysis of practice location. The major cities of Edmonton and Calgary in Alberta, each with a metropolitan population of approximately one million, and five regional centres, each with a population between 60 000 and 100 000, were classified as urban locations. All other locations were considered to be rural.
Data were analyzed descriptively using The Statistical Package for the Social Sciences for Windows, v24.0 (IBM; http://www.spss.com). Mean rating scores for items in the domains of care were compared between urban and rural program graduates using ANOVA and employing an alpha level of 0.05.
Ethics approval
The study was approved by the Conjoint Health Research Ethics Board at the University of Calgary (E-25213) and the Health Research Ethics Board (Health Panel) at the University of Alberta (Pro00034016).
Results
The overall survey response rate was 47.2% (307/651). Of the total respondents, 173 were categorized as urban program graduates and 59 as rural program graduates. Within each of the two universities, the proportion of rural and urban respondents was equivalent. Excluded from analysis were two respondents who did not record their program stream and 73 who entered residency training through the AIMG program or were transfers. Limitations of the questionnaire did not enable residents who entered residency training through the AIMG program to be classified as either rural or urban program graduates.
Just over 60% of the respondents were female and the mean ages were 36.4 and 36.7 years for rural and urban program graduates, respectively (Table 2). There was a statistically significant association (r=-0.411, p<0.01) between type of program completed and practice location, with 62.1% of rural program graduates practicing in rural locations and 81.1% of urban program graduates practicing in urban locations.
Comparison of each item within the four domains of care revealed that rural program graduates had significantly (p<0.05) higher overall mean scores than urban program graduates for providing postnatal care, intrapartum care/deliveries, palliative/end-of-life care, office-based clinical procedures, in-hospital clinical procedures, providing emergency care, in-hospital care, home visits, long-term care, and caring for rural or Aboriginal populations (Table 3).
Analysis of domains of care by practice location showed that those in a rural location exhibited a broader scope of practice than those in an urban location, irrespective of the program stream completed. In particular, care across the lifecycle, palliative care, emergency care, in-hospital care, home visits, and long-term care were a significantly higher core element of practice for rural program graduates in rural practice than for rural program graduates in urban practice (Table 4). Similarly, urban program graduates in rural practice had higher mean scores for providing palliative care, office-based clinical procedures, in-hospital clinical procedures, emergency care, in-hospital care, long-term care, and care of rural or Aboriginal populations than urban program graduates in urban practice (Table 4).
In both rural and urban practice locations, rural program graduates had significantly higher mean scores than urban program graduates for providing intrapartum care/deliveries and care of rural populations (Table 5). In rural practice, rural program graduates also had higher mean scores for providing prenatal care, emergency care and home visits.
Table 2: Characteristics of study respondents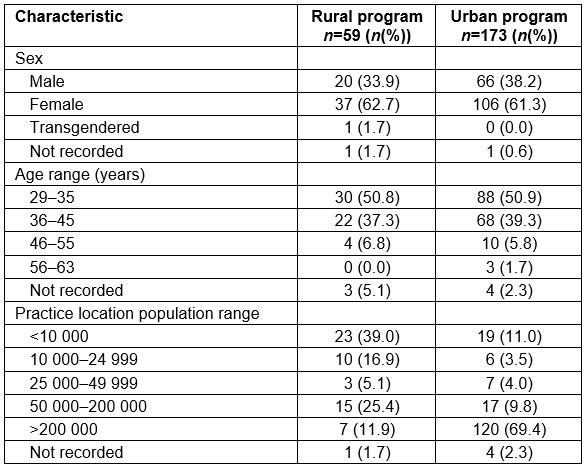
Table 3: Mean scores for domains of care by rural versus urban program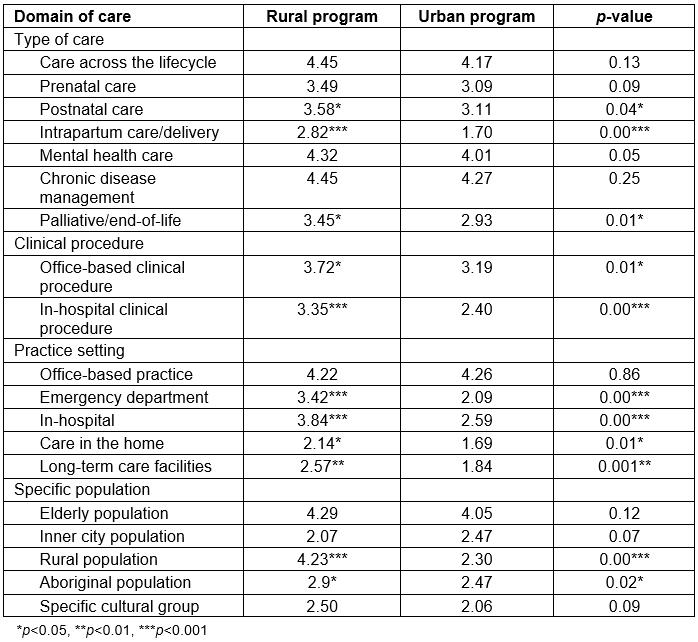
Table 4: Mean scores for domains of care for rural versus urban program graduates by practice location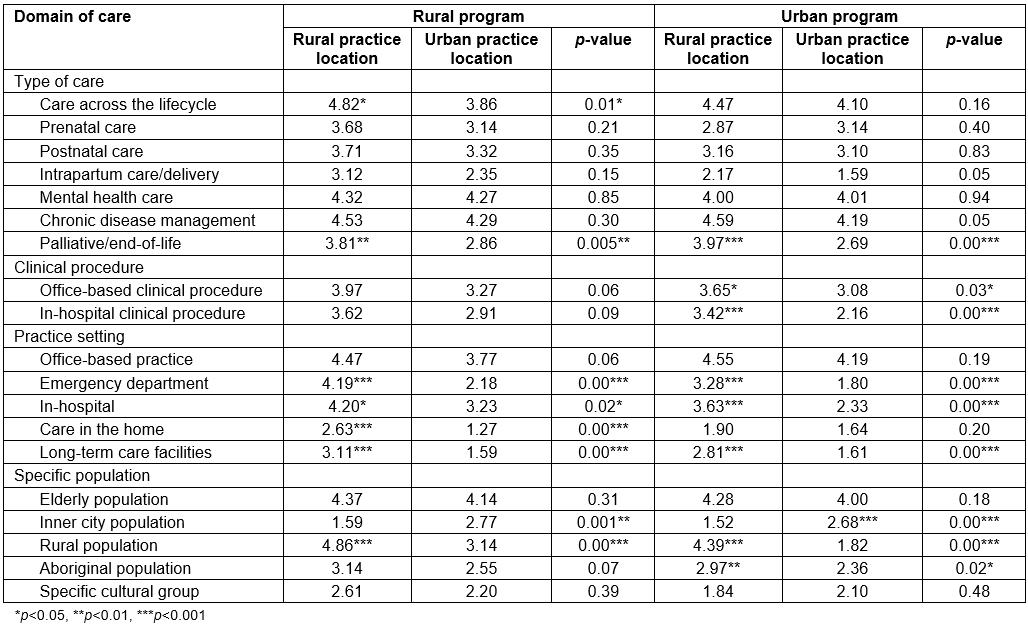
Table 5: Mean scores for domains of care for practice location by rural versus urban program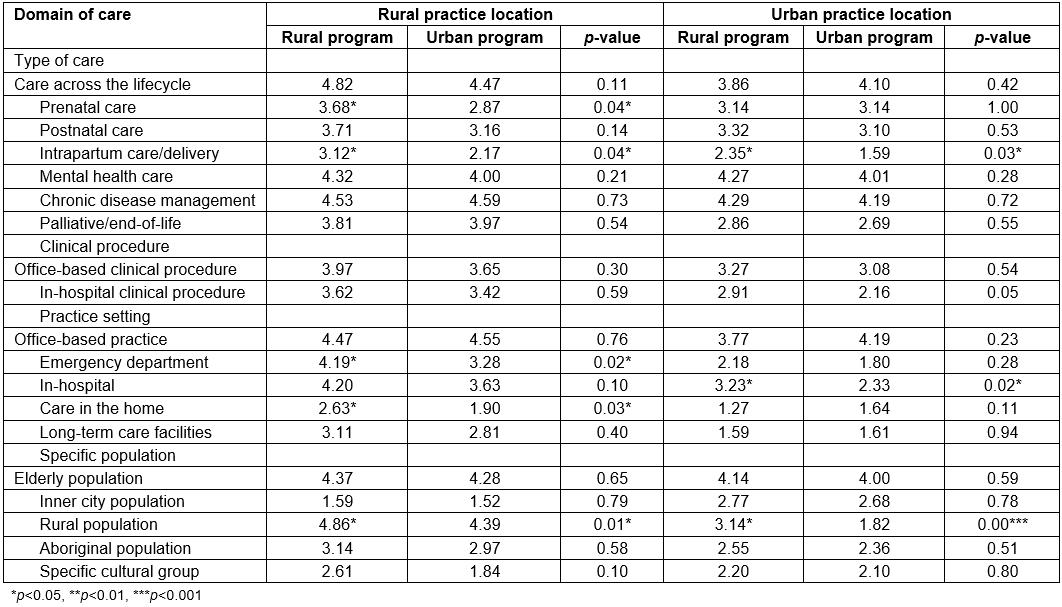
Discussion
The new finding from this study is that, even within a similar practice location, rural program graduates tend to have a broader scope of practice than urban program graduates. This is particularly evident in the provision of prenatal care and intrapartum care/deliveries. Rural program graduates in rural locations also included emergency care and home care as a core element of their practice to a greater degree than urban program graduates in rural locations. These findings may be attributed to a number of factors, including the explicit role modeling that rural program graduates receive from rural family physicians who themselves perform broad scope, comprehensive clinical practice. Exposure to rural physician role models may have considerable influence on graduates’ future practice styles 20. As such, rural program graduates likely gain considerable confidence and skill in performing obstetrical deliveries or for providing care in different practice settings. In contrast, urban program graduates primarily do clinical rotations with urban family physicians who themselves have more focused or limited scopes of practice and who, given the shared care model that dominates urban centers, may not provide intrapartum obstetrical services. Although urban program graduates who practice in rural communities also have a broader scope of practice than their urban graduate colleagues who practice in urban areas, it is highly likely that selection bias of residents into the respective programs occurs, with those interested in a broader scope of practice and possibly in obstetrical care opting for the rural program.
The study findings demonstrate that both rural and urban program family medicine graduates have a broader scope of practice in rural than in urban locations, signifying that practice location and the needs of the community have a major influence in determining the scope of clinical practice. This is supported by other studies reporting a broader scope of family practice in rural locations5,6,9. Geographic factors are reported to account for 30.5% of the variance in scope of family practice, and limited access to specialists is positively associated with scope of practice7. Practice location appears to operate to either broaden or place constraints on the scope of clinical practice, perhaps through the combination of availability or lack of medical resources and/or clinical or professional support systems and the healthcare needs of the community. Given that rural family physicians generally have less access to specialists and medical support systems than urban physicians, the practice environment compels them to practice a broader set of clinical skills than those in urban practice. It is reassuring that urban program graduates in this study who practiced in rural locations adapted to the broader scope of rural practice; in part, this may reflect the similarity of the curriculum content between the rural and urban programs in this study.
While the curriculum accreditation requirements and expected outcomes for graduates of both rural and urban programs are the same, the training environments differ. In view of the study findings and the paucity of research examining the impact of family residency training programs on scope of practice, various questions arise. How influential is the training environment on the scope of practice? To what degree do differences in the learners themselves affect scope of practice, irrespective of the training curriculum? Is it reasonable to entertain the possibility that rural and urban programs have individually evolved on divergent tracks to meet the needs of their own unique communities? If so, to what degree has this evolution been influenced by system pressures that see a predominance of subspecialties in urban tertiary care facilities, resulting in few role models of the generalist tradition?
There is little literature on the impact of factors outside of the community location on scope of practice. Both the published literature and this study have established that practice location appears to influence scope of family practice. Other studies have also identified that personal physician characteristics and professional factors influence family physicians’ scope of practice6,7. Moreover, the patient-centered clinical method denotes that patient factors affect clinical practice 21. In addition, the findings of this study suggest that family medicine residency training programs also likely play a significant role in affecting graduates’ scope of practice. A study of internal medicine residents has found that the nature of the residency training environment (high v. low practice intensity) had an effect in formulating the practice style of residents22. Each resident has an impending potential at graduation that is realized through the impact of the communities where they work. The scope of practice may evolve according to the demands placed on the practitioner and it is possible that these demands also may change over time. Figure 1 is proposed as a summary framework of the factors that have been reported to be associated with scope of family practice.
With respect to program planning implications, the study findings suggest that the number of residents trained in the rural program should be increased to fulfil family medicine’s social accountability mandate to increase the supply of rural physicians with a generalist scope of practice. Moreover, consideration should be given to increasing the number of rural faculty members, as well as obtaining rural family physicians’ input into program design. With respect to the urban program, the exposure of residents to broad scope family practice could be enhanced through targeted selection of urban preceptors who model a comprehensive scope of practice. An evaluation of the current 2 month mandatory rural rotation for urban program residents should be undertaken to assess the effect of this rural experience. On a wider scale, the issue of maintaining generalism and comprehensiveness of care in family practice needs to be supported at a systems level by removal of barriers that impede full scope practice.
This study is limited by its retrospective, cross-sectional nature that provided a synopsis at a particular point in time. Scope of practice was self-reported by respondents and not objectively verified, therefore reporting bias may have occurred. Scope of practice was determined at the time of survey completion, which ranged between 2 and 7 years after residency program completion for different graduates; as such, it does not reflect scope of practice at specific intervals (eg within first year of practice). Items within the domains of care were not defined, but left to the interpretation of the respondents, therefore items could have been interpreted differently (eg office-based clinical procedures). Limitations of the questionnaire did not enable IMGs who entered residency training via the AIMG program or those who were DND residents to be classified as either rural or urban program graduates; these were excluded from analysis and the findings may not be applicable to IMG or DND family medicine graduates. It is possible that a few residents may have switched between rural and urban programs during the residency period and were inaccurately categorized in the present analysis.
Further research is warranted to examine the scope of family practice by graduates of other family medicine training programs, IMG family medicine graduates by program completed, as well as of rural program graduates who practice in urban locations. How and why these choices change over time is a further area to research.
 Figure 1: Framework for factors influencing scope of family practice.
Figure 1: Framework for factors influencing scope of family practice.
Conclusion
This study contributes to the currently minimal literature about how the scope of a family physician’s clinical practice is affected by the type of residency completed, broadly categorized in this study as urban or rural program. The findings suggest that the combination of the site of training and the site of practice affects the final breadth of the clinical practice of a family physician. The study also advances conceptual understanding by proposing a framework that summarizes the factors that have been reported to be associated with the scope of family practice.
Acknowledgements
Funding for this project was provided by the Alberta Rural Physician Action Plan. Research assistance for the survey was provided by Jacqueline Torti and Emmanuel Appiah Anokeye.


