Introduction
Myocardial infarction (MI) continues to be a leading cause of death worldwide1. According to the British Heart Foundation, in 2013–2014 there were 187 421 hospital visits in the UK due to MI, which translates to someone in the UK having an MI every 3 minutes2. ST-segment elevation MI (STEMI) represents a high risk of early death and myocardial damage due to acute occlusion of a coronary artery3.
Treatments to open a blocked coronary artery are called reperfusion therapies (RT) and include pharmacological thrombolysis (TL) that is administered intravenously4 or primary percutaneous coronary intervention (pPCI)5, performed in a cardiac catheterisation laboratory (cath lab). Optimal RT (ORT) with pPCI6 or TL7 given sufficiently early (within 120 minutes for pPCI and within 30 minutes for TL) reduces morbidity and mortality. If ORT is not delivered promptly then the risk of death increases, and left ventricular (LV) systolic impairment, causing heart failure and an increase in mortality, is more likely8-10.
pPCI is the preferred RT (due to mortality and morbidity benefits)11,12, although TL still has a role in the treatment of some patients due to the lack of availability of a cath lab within the recommended time frame13. The European Society of Cardiology guidelines suggest pPCI should be carried out within 120 minutes14; if this is not possible then pre-hospital TL (PHT) should be given. In practice this will translate to a maximum transfer time of 90 minutes to a cath lab. Patients who have an MI diagnosed in the pre-hospital setting and are unable to get to a cath lab within 90 minutes should be given TL, otherwise immediate transfer to a pPCI facility should occur11. The delivery of TL in remote areas (>90 minutes’ travel time from a cath lab) could therefore be considered the ORT.
The delivery of ORT in remote areas is not consistent15, and the exact proportion of patients who receive ORT and the relationship to time of day and remoteness from the cardiac cath lab is currently unknown.
Barriers to ORT are poorly understood but can include staffing (lack of paramedic crews), education and training (lack of confidence to deliver PHT) and equipment issues (unable to transmit an ECG for telemetric support)16. Similar barriers have been described in other healthcare settings such as those of rural emergency practitioners in Canada17. These are recognised to be complex, but also dynamic and potentially remediable with education, support and improved collegiality 18. By identifying local modifiable and non-modifiable barriers to ORT and exploring the factors that might contribute to potential difference in clinical outcomes between central and remote patients, recommended strategies can be employed to try to overcome such barriers and mitigate the impact of remoteness in patient care.
This study aimed to investigate ORT delivery in a remote region in the north of Scotland in relation to location of STEMI and time of day, and to identify potential barriers to optimal care.
Methods
Participants
Patients who had an STEMI during a 12-month period (March 2014 and April 2015) were included. Patients were identified from their final diagnosis code on discharge from hospital or death. Data from patients who died prior to attending hospital were not included.
Setting
The study was set in the north of Scotland (classified by the National Health Service as Highland). This area represents 41% of Scotland’s land mass (30 660 km²) with only 4% of the population (232 132)19. There are several hospitals in the area. The regional centre (Raigmore Hospital) is located in the south-east and has a cath lab that operates between 0830 and 1800 on weekdays. There are three rural hospitals (Broadford Hospital in Skye, Belford Hospital in Fort William and Caithness General Hospital in Wick) that admit acute cases. Out-of-hours access to a cath lab is obtained from three tertiary centres (Aberdeen, Glasgow and Edinburgh), all greater than 90 minutes’ travel time by vehicle from any NHS Highland health board location.
Study design
This was a retrospective case series review.
Data collection and handling
The list of potential patients was obtained from the Scottish Morbidity Record (SMR), which includes dates of admission/discharge and locations of admission. SMR is an episode-based record relating to all inpatients and day cases discharged from Scottish hospitals. The inclusion criterion was any patient diagnosed with STEMI. Exclusion criteria included diagnosis of a non-STEMI, unknown diagnosis or living outside of the north of Scotland region. Further clinical details were obtained from the patients’ discharge letters through Scottish Care Information Store (a data repository that retains patient information at a health board level). Any missing information from patient discharge letters were obtained from other bespoke clinical reporting systems (echocardiography and PCI). Self-presenting patient data were obtained from the hospitals’ accident and emergency departments.
The primary outcome measure was whether ORT was received or not. Secondary outcome measures included death and LV function. Age, gender, postcode, time of presentation, date of admission and discharge, treatment type and location, distance and travel time from cath lab and LV function were obtained from case note review.
Travel times when driving a car were obtained using Google Maps20, although it should be noted that ambulance drive speed, road conditions and weather will impact on the actual drive times. Distance of patients from the cath lab was described as remote if they were more than 90 minutes of driving time from the cardiac cath lab and central if they were 90 minutes or less of driving time from the regional centre. There is no agreed definition of remote; for the purposes of the present study this definition pertains to geographical remoteness to a cath lab and not necessarily to other services. ORT was defined as the best possible RT for the specific patient at the specific time. Individualising ORT for each patient relied on several factors: drive time from the nearest cath lab, time and day of presentation, patient eligibility for PCI/TL and route of access to health care (eg self-presenters to hospital would not be eligible to receive PHT). pPCI was considered to have been ORT for all patients, while PHT was considered to have been ORT in all remote patients or central patients presenting out of cath lab working hours (when pPCI would not have been available). In-hospital TL was considered to have been ORT only in remote patients who self-presented to hospitals without a cath lab or central patients who self-presented out of cath lab hours. Patients who were deemed ineligible for either TL or pPCI were still deemed to have received ORT for the purposes of this study (eg ORT might represent no RT if the patient presented late).
For the purposes of this study, patient pathways were created after consultation with several local experts and refined through multiple iterative stages, based on location of presentation (ambulance or self-presentation), initial management (PHT, in-hospital TL or PCI), reperfusion outcome and subsequent management. New pathways were added where required after reviewing patients’ clinical letters. This led to the identification of 13 distinct pathways in total.
The reasons for lack of ORT were determined from the notes review, and they were recorded and described using descriptive statistics. Where the reason for lack of ORT was not explicitly recorded in the notes, the case was reviewed by a local subject expert (cardiologist) to determine the cause of lack of ORT. These were then characterised, quantified and reported using descriptive statistics.
Data analysis and statistics
The data set for continuous data was presented as mean ± standard deviation, while categorical data were presented as an absolute value, percentage or both. The χ² test was used for comparison of the relationship between remote and central location patients in terms of LV function and whether or not ORT was received. A p-value of <0.05 was considered statistically significant. All tests were performed using Microsoft Office Excel 2007.
Ethics approval
The study was approved by the ethical review panel of the School of Pharmacy and Life Sciences at Robert Gordon University (06/04/16/S17). Approval from the Caldecott guardian and NHS Highland Research and Development office were also obtained.
Results
During the study period, 627 patients were coded for acute MI. After applying the inclusion and exclusion criteria, 131 STEMI patients were identified (Fig1). Of the 131 STEMI patients, 83 (63%) were male (aged 64±13 years) and 48 (37%) were female (age 72±11 years). Thirteen distinct clinical pathways were identified (Table 1). Eighty two (62%) patients were central and 49 (38%) were remote (Table 2).
Table 1: Reperfusion therapy pathways identified in the study (n=131)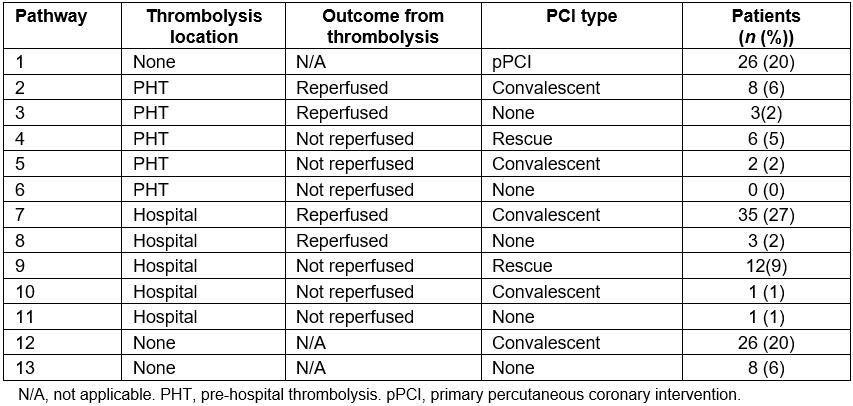
Table 2: Patient distance from regional centre based on drive time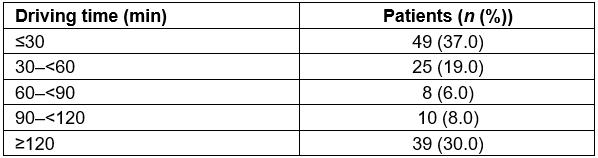
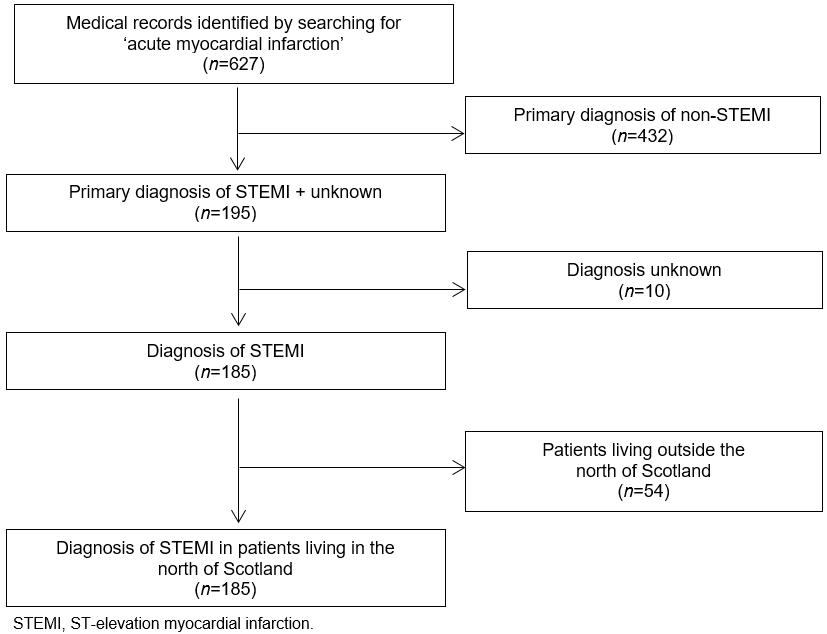 Figure 1: Study inclusion and exclusion criteria.
Figure 1: Study inclusion and exclusion criteria.
Place of definitive treatment
The majority of patients (102 (78%)) were treated, at some point in their journey, at the regional centre, some patients (3 (2%)) were treated at the rural hospital only while 26 (20%) were admitted out of working hours, did not reperfuse after TL and were transferred to the tertiary centre, bypassing the regional centre.
Reperfusion therapy
Of the 131 STEMI patients, 26 (20%) received pPCI, 73 (56%) received TL and 32 (24%) received no RT. Of the 73 patients who received TL, reperfusion occurred in 48 (66%) and, among those, 41 (85%) received convalescent PCI. The 25 (19%) who did not clinically reperfuse were treated with either rescue PCI (21 (84%)) or conservatively (4 (16%); three had convalescent PCI and one had no further therapy). Of the 32 patients who received no initial RT, 24 (75%) received convalescent PCI (Table 1).
Optimal reperfusion therapy
In total, 71 (54%) patients received ORT. Of the 52 patients receiving in-hospital TL, 3 (6%) were self-presenters, while an additional 9 (17%) were not eligible for PHT and thus considered to have received ORT. Of the 34 patients who received no RT, 12 (35%) patients were not suitable for TL and 2 (6%) had reperfused by the time of first medical contact.
Influence of time of day and remoteness
Centralpatients were more likely to receive ORT than remote patients (53 (65%) vs 20 (41%); %uD835%uDF122=7.05, degrees of freedom =130, p<0.01). The influences of location and time of presentation on the initial treatment of remote and central patients are shown in Figure 2, comparing therapy in working hours and out of working hours.
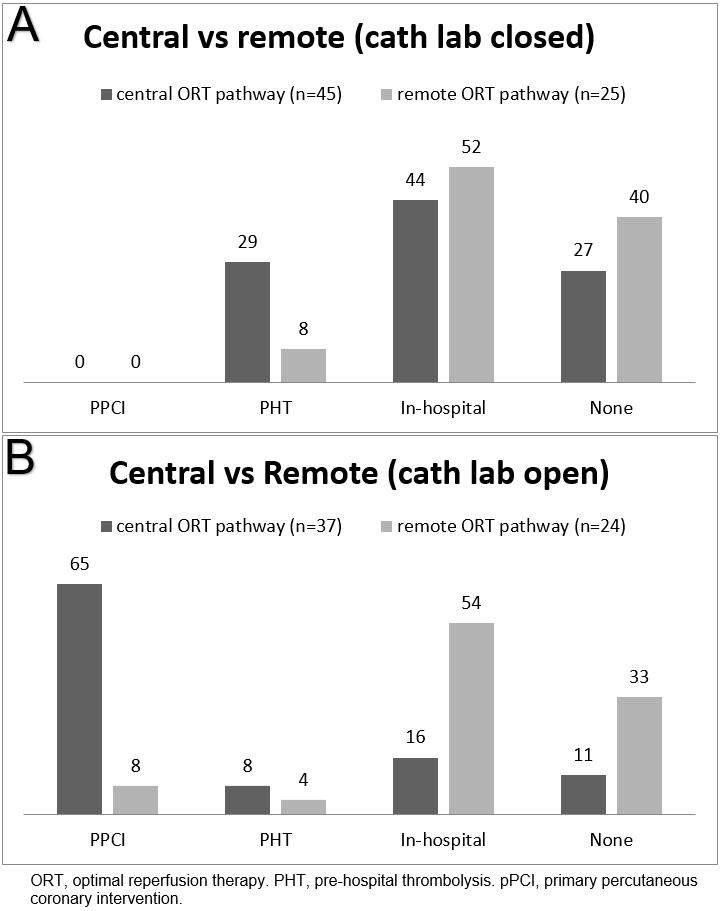 Figure 2: Initial reperfusion therapy when cath lab at regional centre (a) closed, (b) open.
Figure 2: Initial reperfusion therapy when cath lab at regional centre (a) closed, (b) open.
Left ventricular function
Of the 131 patients, 33 (25%) had a normal LV function, 43 (33%) had a mild LV dysfunction, 29 (22%) a moderate dysfunction and 14 (11%) a severe dysfunction. The majority of patients who had normal LV function or mild LV dysfunction after STEMI were from the PHT group (79%), while in the pPCI group 58% had a normal LV function (Fig3). There was no difference in LV function between central and remote patients (45 (62%) vs 31 (53%), p=0.35), although the study was underpowered to show differences.
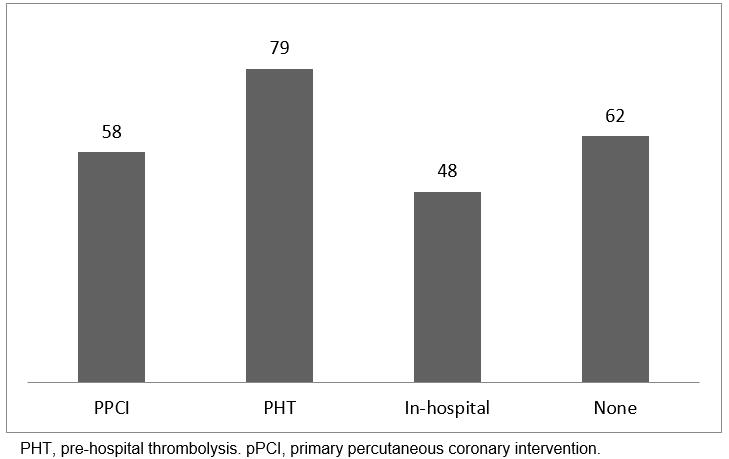 Figure 3: Percentage of patients with normal or mildly impaired left ventricular function post-myocardial infarction by initial reperfusion therapy.
Figure 3: Percentage of patients with normal or mildly impaired left ventricular function post-myocardial infarction by initial reperfusion therapy.
Barriers to optimal reperfusion therapy
Each of the 60 cases in which ORT was not delivered was discussed with a cardiologist and the reason for ‘no ORT’ identified. These included include 38 (63%) cases where PHT was not given (due to lack of trained staff), 4 (7%) cases where poor interhospital communication led to no RT and 9 (15%) cases where the patients presented late. In 7 (12%) cases there was either a non-diagnostic ECG or atypical symptoms.
Discussion
This is the first article to report differences between remote and central patients in an area that employs a hybrid reperfusion approach to STEMI care (both pPCI and TL). The results show a clear variation in care between remote and central patients. What was not expected was the lower proportion of patients who received no RT during office hours at the regional centre compared with all other periods. While there was no obvious difference in clinical outcomes measured by significant LV dysfunction between theremote and central groups, the numbers are too small to be able to draw any definitive conclusions about any potential harm.
Results from this study are generally comparable with the Euro Heart Survey Acute Coronary Syndromes (EHS-ACS)21 and the Global Registry of Acute Coronary Events (GRACE)22. In both studies, the majority of patients were male with a mean age similar to that in the present study. Interestingly, more central patients in the present study received pPCI than in the EHS-ACS study, although these data are older and, according to a more recent national audit of PCI,91% of patients located within 90 minutes of a PCI centre were treated with pPCI23. This percentage is significantly higher than that for the central pPCI patients in the present study, which can be explained by in-hours only availability of the cath lab.
pPCI is the gold standard treatment for STEMI and has been shown to have mortality advantages over thrombolysis in several trials6,24. However, the majority of trials showing superiority of pPCI have compared pPCI with hospital TL, not PHT, although equivalence has been shown more recently with PHT; presumably, the earlier the TL is given, the more likely it is to be effective. In the present study, the proportion of STEMI patients who received pPCI was heavily influenced by the cath lab opening hours (limited to office hours), therefore the majority of STEMI patients did not receive pPCI. There was evidently a major difference between remote and central patients in this regard, with no remote patients receiving pPCI.
Thrombolysis as a treatment for STEMI was established in the 1980s after the International Study of Infarct Survival trials using streptokinase25, and until the emergence of pPCI was the mainstay of reperfusion treatment. It is well recognised that TL is most effective when given early (within 1 h of artery occlusion). In practice this is rarely achievable due to several factors, including delayed calling for help and sometimes limited availability of pre-hospital staff to deliver TL. This is a particular issue in remote areas in the UK where there is a relative lack of trained paramedics. Thus remote patients are potentially at a double disadvantage, being too far from a cath lab and served by ambulance staff with a lower chance of having paramedic crew. The present study’s data reflect this reality, with fewer patients in remote areas receiving PHT.
Despite the differences noted in the use of pPCI and TL there were no obvious difference in outcomes; indeed, LV function was numerically more often ‘normal’ in the TL subgroup, although the numbers were small making firm conclusions more difficult. There were only a small number of deaths in the cohort and it is therefore difficult to draw conclusions about mortality. Prior studies have reported higher mortality in remote MI patients26. The reasons for this are unknown but likely to be multifactorial.Due to the small numbers, in many studies, of remote and rural patients it is difficult to draw firm conclusions, although one study suggested the increased mortality rates for remote acute MI patients did not appear to be related to lower quality of care27. A simple explanation for the higher mortality rates could be related to the older population that resides in remote areas, while studies suggest that variation in STEMI treatment could be attributed to the fact that patients with advanced age and comorbidities are less likely to be treated with RT, despite the data confirming that these patients would benefit significantly from such treatment28,29. Pre-hospital deaths were not included in the present study’s cohort and therefore the overall death rate from acute MI cannot be determined.
The present study identified several barriers to ORT: poor communication between hospitals, late presentation, non-diagnostic ECGs and atypical symptoms. However, the barrier encountered most frequently was the lack of PHT administered by paramedics, most commonly due to a lack of a paramedic on ambulance crews. Paramedics are experts in pre-hospital care and play a vital role in PHT administration. A study to test paramedics’ ability to identify patients eligible for thrombolytic therapy, thus reducing call-to-needle time, concluded that a mean potential saving time of 41 minutes is achieved30. Service providers need to take this into consideration. In the present study’s sample, the majority of non-ORT patients were eligible for PHT if trained paramedics were in place – this demonstrates a health inequality in remote areas with regard to STEMI patients getting access to ORT. The NHS Highland area therefore needs to ensure that all PHT responders are trained to provide appropriate treatment to individual patients and to ensure that all ambulances are staffed with paramedics. This is not an insurmountable issue: with better staff training, PHT administered by trained paramedics or dual-response primary care physician/general practitioner (GP) could likely be increased. Training primary care physicians in remote areas showed a significant reduction in delay from call-to-needle time, by an average of 17 minutes. Diagnosis made by the GP was reliable and safe, with 95% of the initial STEMI diagnoses being confirmed31. In our area a telemetric and decision support service is delivered from the coronary care unit, but the results from this study demonstrate that more work is needed to increase use of PHT in remote patients.
Delayed calling for help is a well-identified barrier to ORT, which was outside the scope of this study due to poor and inconsistent documentation of this parameter. The GRACE registry of 11 543 patients with acute coronary syndrome indicated that the median time between symptoms onset and call for help was 139 minutes, suggesting that, even with the most advanced systems of care, some barriers are difficult to overcome22. The reason could be that published guidelines attempting to standardise STEMI care are not individualised for each facility, thus adherence to STEMI guidelines might not be feasible in remote sites. According to the study of Bata et al., ORT can be achieved through rapid pre-hospital diagnosis and improving systems of care32. However, little effort has been made in identifying the causes of such challenges in remote areas, and this is an area for future research.
Although transfer distance has a major impact on ischaemic time33,and PHT is the optimal therapy if door-to-balloon time is 90 minutes or more11,12, PHT was not utilised for most remote patients, and a higher use of PHT was seen in central patients, with considerable variations between working and out of working hours. Holmes et al. reported that a successful regional care model can reduce the disparity of care between after hours and working hours for patients with STEMI34. Therefore, establishing a local policy to provide consistent quality of care might be a key factor in providing ORT.
While achieving 100% ORT should be the aim, it is well recognised that there are unique logistical issues when delivering health care in remote areas. Some of these are obvious, such as weather, roads, availability of transport and staff, while others are more subtle, such as patient choice factors, staff training and experience, and communication barriers with specialist centres. Some of these barriers can be overcome by innovative models of working with rotational posts between the rural district hospitals and the regional centre and increased protected learning time in the regional centre. Technology support such as app-based algoythms and real-time, online support for ECG recognition may also be helpful.
Limitations
The retrospective design of this study depends on the quality of routinely collected data, and certain parameters such as time from symptom onset to call for help were not consistently available. Nevertheless, it was possible to include all STEMI and, due to the national radiology reporting system and electronic patient discharge letters, to report clinical data for all patients. Google Maps20, used to measure travel time by car, is not a validated tool for an ambulance. Paramedic crews might be quicker due to their training, road use and advanced driving skills. Furthermore, volume of traffic at different times of the day or year will affect travel times. Notwithstanding this limitation, Google Maps provided a systematic approach. A further limitation was that, although data was available on hospital of first admission and home address, it was not always possible to confirm that MI had occurred at the home address; a small number of patients may have had their event elsewhere. However, any large difference in location would have been obvious as a disconnect between home location and local hospital, which was not found. Finally, the study sample included patients diagnosed with STEMI and admitted to a hospital. Any patient who did not survive a STEMI before being admitted was therefore not included. This may affect interpretation of the data and conceal mortality differences, but addressing this limitation was outside the scope of the study.
Conclusion
This study has shown that ORT delivery is sub-optimal in the whole study region; furthermore, a clear difference in access to ORT exists between central and remote patients, demonstrating a health inequality between patients living in central and remote areas. Disappointingly, remote patients, while geographically unable to reach an available cath lab in time, were also less likely to receive PHT and therefore potentially exposed to higher risk. Reassuringly, during working hours the vast majority of central patients received pPCI, which reflects ORT, but more needs to be done to improve PHT use out of hours. This study confirms that communication and pathways could be improved (eg bypassing non-PCI capable hospitals) and that the major barrier identified to the delivery of ORT was the lack of trained paramedics, which should be addressed with some urgency.
Acknowledgements
The authors would like to thank the staff of the Scottish Ambulance Service and Coronary Care Unit. A. Peace, R. Bond and S. Leslie are supported by the European Union’s INTERREG VA Programme, managed by the Special EU Programmes Body.
References
You might also be interested in:
2019 - Analysis of a decade of skin cancer prevention using a mobile unit


