Introduction
Many western countries face a shortage of physicians in rural areas, especially regarding general practitioners (GPs)1-3. Studies indicate that the number of GPs will continue to decline further in the coming years. In Germany, this is based on two demographic factors. First, one-third of the currently practicing GPs will retire in the next 10 years. Second, only 10% of young physicians choose to work as generalists, so that not enough doctors will be available to fill the resulting gap4,5. In the past, short-term employment contracts and frequent position changes during postgraduate training discouraged young doctors to take up a GP career6,7. In addition to the general lack of interest in a postgraduate training as a GP8, there is a shortage of GPs who are willing to take up residence in rural areas9,10. Therefore, there is a growing concern that the continuously ageing society will not be provided with adequate, close-to-home health care in the future11,12.
Several approaches have been developed to counter this foreseeable shortage13-16. Most of them are based on three main approaches to redistribution strategies: normative approaches (professional support and development schemes), utilitarian approaches (one-off payments, increased income and job flexibility) and coercive strategies (educational loan repayment or scholarship in return for obligatory service)17. However, there is a need for strategies focusing on rural communities that seem less attractive to doctors looking for a practice18.
Several international studies and organisations have attempted to define ‘rurality’19-25. It seems difficult to find a generic definition of ‘rural’, since there are various rural regions that display different economic and social development23. The term therefore refers both to areas with a strong connection to cities and their infrastructure (eg semi-rural areas or commuter zones) and to peripherally located communities (remote rural areas)24. Additionally ‘rural’ is often defined by objective criteria such as certain forms of landscape, demographic structures and settlement, low population density, agriculture and sociocultural conditions22. The OECD, for example, regards an area as rural if the population density is less than 150 inhabitants per square kilometre21. The conceptualization of rurality has since been expanded to be defined as a subjective, social construct, rather than an objective, material reality25. Whether a region is regarded as rural seems to be, above all, a subjective interpretation26. Therefore the individual’s perception of rurality is an underestimated factor as it might influence one’s decision to want to live and work in an area. The aim of this study was to explore individual determinants that influence the perception of rurality and to elaborate strategies against GP shortage in rural areas.
Methods
For this study, a qualitative design was chosen to gain a profound understanding of individual motives and behaviour as well as insights into physicians’ subjective attitudes regarding rural areas27. This was achieved by using a combination of qualitative methods: brainstorming, focus groups and semi-structured interviews. A focus group is a moderated discourse procedure in which a small group of people is stimulated by an input to discuss a specific topic28. The first focus group was a brainstorming group. Brainstorming is a scientifically recognized tool, capable of generating relevant ideas and solutions to problems via creative group interaction29. The semi-structured interviews were added to the study to maximize the range of topics and to give the respondents the opportunity to bring forward unforeseeable points of view30. The discussion process was structured by key questions, which served as a semi-structured guideline and ensured that all important aspects were addressed.
Selection and description of participants
Medical students aged over 18 years as well as postgraduate trainees from the German university cities of Lübeck (federal state of Schleswig-Holstein), Dresden (federal state of Saxony) and Heidelberg (federal state of Baden Württemberg) were asked to participate in this study using email lists (eg student email lists of the respective universities or the postgraduate trainees’ forum). The groups were stratified based on demographic criteria (occupation, education, age). The aim was to create a homogenous group of same-class people, who are more likely to have similar attitudes and orientations during a discussion and are thus easily reproduced28,31. In total, three focus groups were assembled (F1–F3). The first two focus groups (F1 and F2) were made up of medical students from the University of Lübeck. Subsequently, a third focus group (F3) with postgraduate trainees was held in Dresden. Additionally, nine postgraduate trainees from Heidelberg were interviewed by telephone (1–9).
Data processing and evaluation
The focus groups took place in an uninterrupted setting. Every conversation (group or personal interview) was recorded on a digital recording device and subsequently pseudonymized, transcribed and analysed. The utilized evaluation method was the qualitative content analysis according to Mayring, which was focused around a category system. First, the categories were developed deductively based on a selection criterion, which is created by the key questions. Thus, immaterial, decorative or deviating aspects of the transcripts were excluded32. Afterwards, two independent researchers (LW and FI) inductively developed main and subcategories from the participants’ answers. These newly developed categories were compared and discussed with a third researcher (JS) until consensus was reached. Both the intersubjectivity and the replicability of the results were ensured by this method33. From the citations of the respective categories, individual, concise statements from the participants were selected for illustrative purposes. After three focus groups and nine interviews, no further recruitment efforts were required.
The results of the following key questions are presented:
- How do you personally define ‘rural’?
- Do you have personal experience with rural areas and if so what kind of experience?
- Which factors would make you want to or prevent you from practicing in rural areas?
In the responses, F denotes ‘focus group’, T denotes ‘pseudonymized participant’. Unlettered responses took place by telephone.
Ethics approval
The study was approved by the ethical review committee of the University of Luebeck (AK15-109).
Results
Altogether, 33 participants were included in the study (16 medical students and 17 postgraduate trainees, comprising 24 women (73%) and 9 men (27%). The average age was 28 (range 22–36) years (Table 1).
Table 1: Sociodemographic structure of study participants (N=33)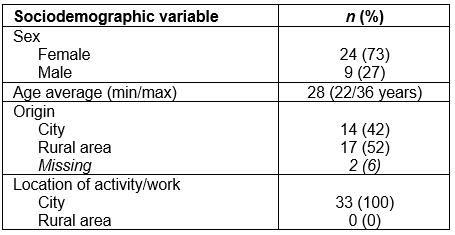
Determinants of the subjective perception of rural areas
General associations: The participants tried to define ‘rural’ by means of population density, a certain landscape such as a farming with dairy cows, fields, forests and animals in the meadows, childhood memories or the accessibility to infrastructure.
For me, an area is rural if the population density is low […], if I had to come up with a number, I would estimate 5000-10,000 inhabitants. 2.24
One of my early childhood memories is this farm, where we always went to get our milk. F2.T7.62
Positive associations: These were mostly descriptive, relating to nature, peace, vastness and space. Other factors mentioned were favorable property prices, the ability to own a house with a garden, to be a self-supporter and to be close to leisure actives such as hiking or mountaineering.
Large plots of lands, pastures and forests. People are not living in terrace houses but in their own ones. You have a certain vastness, a feeling of space and of vegetation. F2.T1.153
In addition, some professional benefits that the countryside offers were addressed, such as less competition, being able to pursue your individual working style, to have a secure income and a special occupational challenge. Also, the support from municipalities and mayors was perceived as positive.
There will be support from the communities in the village. If you want to open or inherit a practice there, you're more likely to get help. 6.126
The social environment of a village community had positive as well as negative associations. Although there are beneficial aspects such as getting help from the villagers or being able to socialize more quickly, particularly the ‘everyone knows everyone’ stereotype was perceived ambivalently. Most notable was associated social control, lack of anonymity and gossip. Furthermore, the prospect of living with people who may have a different mentality, a lack of ‘out-of-the-box’ thinking and open-mindedness was mentioned as challenging. Moreover, the absence of friends was mentioned repeatedly.
This has both advantages and disadvantages. You get more help if you need it but I think it’s just terrible that every step you make is observed and judged and everyone knows what you are doing. F2.T5.165
All your friends are somewhere else and/or too far away. F1.T5.311
Negative associations: An initial and frequently emphasized negative aspect of rural areas was an everyday life in which a car is essential due to predominantly poor accessibility to public transportation.
So even if you’re mobile and have a car, it is exhausting to rely on it all the time. […] Where I originate from, the buses stopped running at two o’clock in the afternoon on Saturdays. F2.T4.108
Another disadvantage is seen in the lack of possibilities and choices that the countryside offers with regards to leisure or educational institutions. The absence of cultural offerings like cinemas or restaurants/pubs and the lack of possibilities to pursue exclusive hobbies was relevant to the students, even if they were admittedly rarely used.
A lot of variety is missing. There are, for example, usually only one or two restaurants, and bars that you can go to. And cultural activities are missing too. It would be nice to have access to plays, for example, even if you are not making use of them very often. F2.T4.298
Further disadvantages of working in rural areas were the age of patient clientele, the allegedly ‘boring work environment’, increased service offerings and the concern of not having a good connection to specialists, hospitals and pharmacies, among other things.
I associate a lot of old people with rural areas and the care of the elderly is very different than in the city […] I would not enjoy that. 3.31
I get the impression that many think […] it is supposedly boring to work in the countryside, that it is not varied, that you don’t have exciting patients, etc. F1.T8.285
Advantages of the city: These negative associations with living in rural areas added to the advantages participants associated with living in a city. The variety of cultural and leisure activities and the comfort that comes with good accessibility to infrastructure and educational/professional possibilities were emphasized. Convenience was seen as something that you learn to appreciate over time and that would be difficult to give up.
The almost six years [at the university] have changed me a bit. Now I say: ‘A big city is cool; I can do anything here like going to the movies or something.’ I think this has a lot to do with the fact that some say, ‘I’ve studied in a big city and have learned to appreciate it all, now I do not want to go back to a small town where there is nothing.’ F1.T1.36
Prejudices: This category includes two different aspects. First is the one addressing the personal image of ‘rural’ in general and second is the alleged image of GPs by other colleagues.
Prejudices against ‘rural’ The ‘rural’ image was mentioned as influenced by the media, especially by television. In this context, everyday life was perceived as romanticized and with unattractive everyday life conditions.
It’s presented [in TV] as exaggeratedly idyllic, but on the other hand not attractive for the personal impression. … They’re not displaying a bad picture per se, because it all looks very nice … but just not attractive for young people’s notions … for what they want professionally. F2.T3.708
Additionally, the simplicity of the people, the mostly elderly population in rural areas and the lack of prospects and emigration were illustrated. One participant described her attitude as follows.
Also, a lot of people, not all of them, who still live in the country … I don’t want to say don’t evolve – that sounds so condescending – but they don’t adapt so well, socially. Most of the young people who are still there are kind of … I don’t know … not mobile … or are drawing off Harz 4 [unemployment benefit] and the kids having ADHD. F3.T4.410
Prejudices against GPs in rural areas The participants pointed out that family medicine has a bad reputation, which is often influenced by other colleagues. This mindset is aggravated further when it comes to the family doctor from the country, who is often depicted as particularly incompetent.
‘Oh, the GP has admitted [the patient] to the hospital. Nothing good is going to come out of this.’ And then [if the GP is] from the country, which I think might intensify itself [be even worse than if the GP was from the city]. F1. T1.375
Factors influencing the ‘subjective perception’ of rural areas and subsequent residential environment choice
Personal connection and life stage were particularly tied in with participants’ associations with and perceptions of rural areas.
Personal connection: An essential factor for interest in a rural area was primarily a personal connection. This especially pertains to the person’s childhood and whether part of the family still lives in the rural area. Other factors influencing that decision were partners, friends, hobbies and a positive first exposure to rural areas (eg vacation or internship). Without a personal connection, it was very unlikely for participants to imagine or choose a life in rural areas.
Whether or not you move to the countryside strongly depends on what is familiar to you. You don’t just go somewhere and build a life in the middle of nowhere. You usually go there if you have some sort of connection to it. F2.T1.375
Life stage: Another factor was perception according to life stage. Students prefer to live in the city. In addition to experiencing university life and being able to obtain an education, students are mainly looking for entertainment and diversity in this life phase. The relative ease of finding a partner in the city compared to in a rural area was also discussed. If there was a relationship, the compatibility with the partner’s job could also be a limiting factor. If he or she was not able to work in the countryside, a relocation was said to be more unlikely.
At the moment, I would rather move to an area where I have more opportunities to meet someone…. That’s why I am currently close to a big city again. 9.214
But I believe that what the partner is doing and what he prefers can make or break the decision. Not only that he would get a job, but also that he wants it [to move to the countryside]. F1.T1.464
For the life stages of family planning and of being young working parents, help a family can provide was perceived as a strong asset. In those life stages, it was often decided to move closer to the relatives. The future living environment must offer good educational facilities and leisure activities for the children, which they can ideally reach on their own. If parents are concerned that there are not enough opportunities for their children in a community or village, they are more reluctant to settle there.
Without a child I would be a different person and would work differently than I am now. … Now, it is more important to look at the child’s well-being. 3.118
Also important is accessible infrastructure for daily life, which includes grocery stores, public transportation (train stations), day care, kindergartens, primary schools and hobbies for the children.
Where I live, I would like to have infrastructure and facilities that cover my basic needs. … at least a bakery, a pharmacy, a primary school, a kindergarten. And at least a normal supermarket, where you get the essentials. 6.86
Clinical insecurity: Clinical insecurity was found to be experienced specifically by recently graduated students. They subjectively felt too young and not professionally competent enough and therefore feared too much responsibility too soon in the case of working in a rural area.
I’m all alone, there is no one around that I can ask. I do not even have a colleague and … at least at this point this would scare me a lot. I would definitely say that this is a main reason for me not to work there [in rural areas]. F1.T6.105
Furthermore, participants imagined it being difficult to separate work and private life – especially as a GP in rural areas – and were thus afraid of little free time for themselves and their family. Also, the lack of collegial exchange and the fear of missing a comprehensive education was mentioned.
It’s challenging to make sure that you don’t end up just living for your patients while your own life as well as relationships come too short. F1. T1.264
Strategies to increase the attractiveness of working in rural areas
It has been suggested that getting people who are already connected to rural areas to study medicine has the greatest benefit, as they are most likely to go back home.
Luring someone to the countryside who has never been there is difficult … I think it’s more important to motivate as many people as possible who derive from rural areas to study medicine. 6.48
Additionally, the idea of establishing a personal connection with rural areas, if not already existing, has been mentioned. An example was rural internships during medical school that should be supported financially and with housing opportunities to allow the participants to gain experience and exposure. Further suggestions were a paid voluntary social year or a research opportunity (doctoral thesis) in the countryside.
I’ve decided to do a GP internship, but theoretically I could have only done it where I have a place to sleep because I wouldn’t stay in a hotel the whole duration. Housing opportunities would therefore be a good incentive. F2. T6.506
Well he [from the city] has to experience it! That means he would have to do internships there.... I think he could only imagine it, if he worked there. 6.108
Another strategy was to improve the confidence that students and young postgraduate trainees are lacking, so that they start considering working as a GP in rural areas. This included working as an employee or in a group practice, having a vacation replacement, providing a mentor for background help, improving communication infrastructures (internet connection) and implementing structured training and ‘work preparation’ tutorials during school. Purely financial incentives were not enough for the participants.
It would be interesting to get involved in a joint practice [T1 and T4: ‘yes’], where you have one or more colleagues, with whom you can meet and exchange. That way, you are not alone from the beginning and don’t have to take care of everything by yourself. F1.T8.134
To be paid €60,000 as an incentive is well and good … but [with it] I cannot buy a school for the children or get a better internet connection. F1.T9.209
A final approach involved the invalidation of prejudices. Participants suggested more transparent information on municipalities and their existing offers (presentation of the region, ‘rural days’). In particular, regions with benefits of both the city and the countryside should display their options. Also, the attractiveness of local work conditions could be highlighted by means of role models, for example.
The local possibilities and that you have more than you think should be highlighted more …: ‘We have the infrastructure, we support you, we give you financial and other incentives, the education for your children is good’. If this was communicated, then you would perhaps think about working there for a second. F2.T3.735
Table 2 shows the category system elaborated from the statements of the medical students and postgraduate trainees.
Table 2: Category system elaborated from participant statements 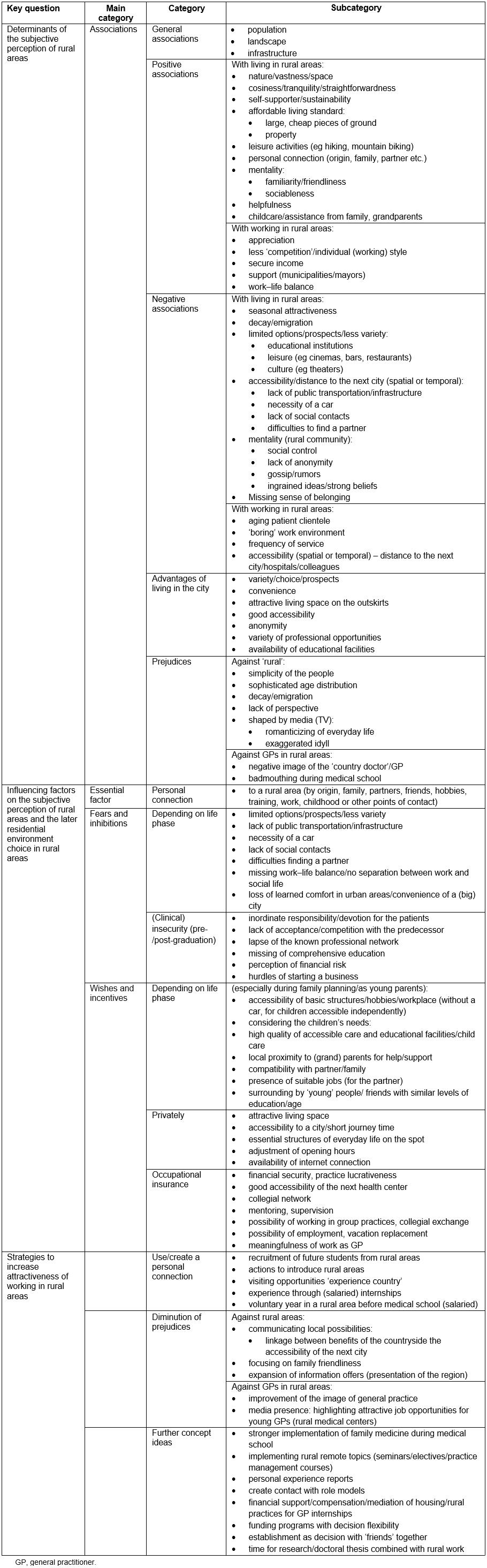
Discussion
In order to develop tailored strategies to counter physician shortages in rural areas it is necessary to understand the determinants influencing the later residential environment choice. Therefore, the aim of this study was to explore which aspects are implicated in facilitating or hindering choice of residence. The most decisive factor here is the subjective perception of rural areas. This in turn builds on general associations, positive and negative associations and benefits of urban life. In the process of this study, three main pillars were identified that significantly influence subjective perception: personal connection to a certain area (eg origin), life stage (eg study, family planning) and prejudices associated with rural life. Considering the work as a GP in rural areas, increasing attention was paid to the clinical insecurity that students feel after graduation.
Participants in the present study showed a respresentative degree of variation in gender regarding the ratio of men to women and a good reflection of the general distribution among medical students34.
Whether a region is regarded as rural is a subjective interpretation26. Concepts associated with rurality in this study included general ones such as population size and infrastructure, with some positive (eg nature, peace and quiet) and some negative (eg social control, gossip and a more difficult everyday life). They are comparable to former studies, where ‘nature’ as well as different aspects of the social fabric were also predominantly associated with rural areas35-37. In the literature, the two opposite perceptions of rurality have been conceptualized as ‘rural idyll’ and ‘rural dull’35.
On the one hand, the rural idyll combines all positive aspects about the countryside. In the present study participants associated it with higher standard of living for less money, near-home leisure activities in nature (eg hiking) and professional aspects, such as stronger relationships with and appreciation from patients, as well as community support. These positive associations were mainly stated by participants who originated from rural areas. They felt familiar with the environment and the social fabric and were more likely to select rural areas as their work locations than participants from the city38.
Thus, the personal connection that one has to the ‘rural’ (eg through family, partner, early experience) strongly influences how a rural area is perceived and has an important impact on the later residential environment choice. Previously developed strategies partially addressing have been referred to as, for example, ‘rural pipelines’ which recognise that place of birth and rural experiences in life shape a preference for rural living in the future39,40. Approaches such as recruiting students with rural backgrounds, establishing rural clinical schools and establishing universities in rural areas such as the Northern Ontario School of Medicine show that fostering this correlation can increase the probability of rural practice41,42. Although studies already indicate that a certain amount of time must be spent in rural areas to form a connection, the length of contact needed to have an effect is still uncertain43,44. However, these initiatives target people and medical students who already have a connection to rural areas.
Since positive associations increase the probability of later rural environment choice, a new aspect of this study was the necessity of new strategies that create a positive connection and awareness of rural areas, especially for those who have never had contact with these areas.
On the other hand are the negative associations with rural areas, which fit the concept of ‘rural dull’. It refers to the aspects of fewer possibilities, social control, gossip and backwardness35. Personal experiences reveal the potentially negative side of living in rural areas: distance to the next city, need for a car, feelings of loneliness, difficulties of finding a partner and the perception of a special mentality of the people. Those aspects are perceived as particularly aggravating by juveniles37 and point out the essential influence of life stage on whether ‘rural’ is rated as positive or negative.
The attitude differs between adolescents/students and young parents: younger people often prefer living in the cities where education choices are greater and they can enjoy the metropolitan advantages that are not available in rural areas. However, when entering a new life phase with a new job or partner, and particularly with the intention to have children, they aim to move to a quieter and safer rural residential environment39. Additionally, participants expressed the wish to return to their families, where more organizational possibilities and support are available for the children. Rural communities should therefore emphasize their ‘family friendly’ surroundings, especially to young parents or couples intending to start a family15.
Participants, especially those who didn’t originate from rural areas, seemed poorly informed about their local conditions, which are much better than expected in many places45. This might be due to media and cultural influences. These prejudices might be aggravated by passing on negative associations to others.
Additionally, the subject of family medicine and the occupation as a GP in rural areas is plagued by prejudices. These surround the concept of rural work and are intensified by colleagues who stir up negative associations with the subject. Often, young doctors who express a desire to be a GP are advised to opt for a ‘decent’ field of medicine46. This ‘badmouthing’, defined as ‘unwarranted, negative, denigrating, even sarcastic comments made by doctors about other doctors’, can have an influence on the current career choice of medical students46. Moreover, persistent negative perceptions of income disparity, workload, and stress, appeared to counter the positive perceptions of meaningful work and esteem47. There is probably an additive effect for people who are not convinced about living in rural areas: negative perceptions intensify with the image of working as an unaccredited rural GP. Therefore, the high job satisfaction of GPs and the high satisfaction of patients with their GPs needs to be pointed out more intensely48,49.
An interesting new aspect was the clinical insecurity that participants expressed. They were concerned that they were not competent enough due to a lack of specific education during their studies. There is indeed evidence that newly qualified GPs in Germany are missing major competencies50. Therefore, clinical-practical abilities should be a more important aspect of under- and postgraduate studies in Germany to strengthen postgraduate trainee self-confidence. In some European countries this aspect is already addressed, for example by introducing departments of postgraduate education at medical faculties51.
Strategies that might be started by universities in Germany include a wider range of practical elective courses and a culture of feedback and supervision. These important approaches were also taken up by government and are reflected in the Federal Ministry of Education and Research’s Master-Plan 2020 and the building of excellent centers for family medicine specialty training52.
Participants feared a lacking professional anonymity and therefore no work–life balance. Although they could imagine living in the country, most of them did not want to practice in the same place because it was too ‘close’ to the patients. This is primarily due to the change of the perception of the medical profession in the younger generation: work today must rank alongside quality of life in the form of work–life balance53. Real working hours as a GP in rural areas need to be communicated in contrast to the perceptions that GPs in rural areas have longer working hours than counterparts in cities54. Being able to work as an employee (with part-time jobs and vacation replacements) or in a group practice could further reduce these concerns and help with mentioned fear of missing collegial exchange.
Limitations
Selection bias may have been an issue in this study as participants might have been highly motivated to choose a career as a GP. Additionally, results might not be generalized for other countries because of the special situation in German medical schools and the infrastructure of German rural areas.
Conclusions
Four important determinants shape the perception of rural areas in Germany and need to be addressed to counteract physician shortages: personal connection to rural areas, different life stages, prejudices towards rural areas/family medicine and clinical insecurity.
Acknowledgements
The authors thank Alana Nicole Loh for native speaking support in the review process.

