Introduction
Heart disease is the largest single cause of death in Australia and contributes to significant illness, disability, poor quality of life and high healthcare costs1,2. Rates of heart disease in rural and remote areas are higher than in urban areas1,3. Whilst Australian Aboriginal and Torres Strait Islander First Peoples’ (Australian First Peoples/Indigenous peoples)4 disease rates, including heart disease and complex comorbidities, are higher, this only partially accounts for the disparity in health status between people in rural and remote and urban populations3,5. Disparity may be worse than reported due to people with poor health moving to urban areas for better services5.
There is significant evidence that cardiac rehabilitation (CR) is best practice for people with heart disease6-8. However, despite this and known higher levels of heart disease of people living in rural and remote areas, referral and access to CR remain low, and access issues are exacerbated by geographic distance, fewer health services and staff3,9, compounded by poor telephone and IT services to support alternative programs in rural and remote areas5.
Cardiac rehabilitation
CR is known to reduce reoccurrence of hospital readmissions, mortality and morbidity from heart disease, and improve general health and quality of life7,8,10. WHO describes CR as including physical, mental and social conditions for people with heart disease, so that by their own efforts, together with support through medical or clinical management, they may preserve or resume optimal function7,10,11. The term ‘cardiac rehabilitation continuum’ is preferred by the Heart Foundation of Australia7, due to the general perception that CR refers to short term, centre based exercise and education programs, usually run by hospitals. The CR continuum is a ‘coordinated system of long-term care’ necessary to help people with heart disease return to an active and satisfying life, and to prevent the reoccurrence of heart disease or new cardiovascular conditions7. This indicates the need for a lifelong individual commitment to healthy lifestyle choices, and adherence to medical advice with health service support7,11.
Costs and priority
Expenditure for hospital-admitted patient services for coronary heart disease, stroke and other cardiovascular diseases in 2008–09 was A$4460 million, and accounted for the highest level of healthcare sector spending, with coronary heart disease expenditure of A$1517 million2. Other costs associated with coronary heart disease were out-of-hospital medical expenses (A$223 million) and prescription pharmaceuticals (A$311 million). Costs of pharmaceuticals for males were nearly twice that of females, but comparatively similar for other out-of-hospital expenses2. Drugs prescribed for lowering cholesterol (statins) account for the highest number of Pharmaceutical Benefits Scheme prescriptions12 and are major contributors to the cost of all pharmaceuticals. Despite evidence that CR reduces recurrence of heart disease and hospital readmissions and improves general health, it is estimated that only 30% of people hospitalised with heart disease are referred to CR in Australia13. A recent cost–benefit analysis that considered the impact of increased CR uptake to the internationally acknowledged standard of 65%13, and included costs for CR programs, direct inpatient costs, burden of disease, informal care costs, and loss of productivity and earnings, estimated a net financial saving of A$86.7 million per annum6.
Multidisciplinary teams and staffing
A CR program based on a multidisciplinary team that includes a general practitioner, and if possible a cardiologist, nurse, physiotherapist, dietitian, psychologist and exercise physiologist, is recommended by the Heart Foundation of Australia and Australian Cardiac Rehabilitation Association7,10. Realistically, due to lack of resources, such a multidisciplinary team is only available in major centres14.
A range of issues negatively impact on recruitment and retention of allied health professionals in rural and remote areas. These include a lack of or inadequate (i) information prior to recruitment, (ii) ongoing education opportunities, (iii) career prospects, (iv) rural placements during undergraduate studies, (v) work–life balance, (vi) management and support – which all contribute to high staff turnover15. Staffing difficulties have also been identified by nurses in Australia’s rural and remote areas in northern Queensland such as excessive working hours, high levels of responsibility and resultant high staff turnover14,15. This leads to an increase in staff stress for inexperienced staff who are still learning, and unable to work to full capacity due to the unfamiliar environment14. Whilst the majority of health professionals working in these areas are nurses and Indigenous health workers14, it is likely that these issues impact on all health professionals and subsequently quality of services in rural and remote areas.
Major issues for cardiac rehabilitation services
Whilst it is estimated that throughout Australia only 30% of eligible people are referred to CR, and less attend10,16, rates cannot be substantiated due to a lack of data16,17. Negative impact on service delivery and access to CR due to large geographic regions is significant3,18,19. This is compounded by health professionals and potential participants’ poor understanding of the benefits of CR20-22. Distance and costs are identified as barriers to attendance in rural and remote areas18,23-25; however, with changing technology options these barriers may be more readily addressed. The major issues identified were limited and suboptimal CR services in rural and remote areas, with more information required to inform policy, management and organisation of CR for adults with heart disease living in rural and remote areas.
Methods
An integrative review is an established evidence based practice method for reviewing qualitative, quantitative and mixed method research26,27. The present integrative review was undertaken through systematic identification, analysis, critique and synthesis of selected peer-reviewed literature to facilitate the identification of a new framework and perspective26-28 of barriers, enablers and pathways of CR in all adults with heart disease in rural and remote areas of high-income countries, with a focus on Australia.
Searches and selection criteria
Electronic database searches used to identify relevant studies included CINAHL, SCOPUS, Informit, PsycINFO and Medline (OVID).
Electronic searches were augmented by reviewing reference lists and citations of selected studies and professional networks (snowballing). Google Scholar was used in this process for forward searching of reference lists and citations to check for additional studies. The 107 articles identified through this process were due to a large meta-analysis29, identified by the database search. However, the abstract review of these references revealed only 13 studies eligible for critical review and thematic analysis. Following this process, only two extra studies were included for further analysis.
Search terms used were ‘cardiac rehabilitation’ OR ‘secondary prevention’ AND ‘rural’ OR ‘remote’; OR ‘Aboriginal and Torres Strait Islanders’ OR ‘Indigenous’ AND ‘enablers’ OR ‘barriers’. These key words were varied for specific databases, for example Medline (OVID), which uses medical subject headings (MeSH), which required that the terms ‘cardiac disease’ OR ‘coronary disease’ OR ‘heart disease’ be expanded and combined with ‘rehabilitation’ to identify articles about CR. Also, the Medline MeSH term ‘oceanic ancestry groups’ is used for First Peoples. The term ‘indigenous’ was used as a generic term because it is in common use internationally. The database searches identified a comprehensive range of studies: Medline (OVID) for wide ranging studies, Informit for studies that focused on Australian First Peoples, SCOPUS for international studies, PsychINFO for psychosocial and mental health and CINAHL for allied health. Limitations applied were studies in English, with human subjects and dated 1 January 2007 to 31 December 2016. Supplementary table 1 contains further information about the searches.
Inclusion criteria for papers were:
- published in English in peer-reviewed journals from 1 January 2007 to 31 December 2016
- focusing on cardiac rehabilitation in rural and remote areas of Australia and high-income countries internationally; barriers, enablers and pathways to CR; or First Peoples, indigenous (Australian and global) and general populations.
Exclusion criteria were:
- effectiveness of centre based and home based (technology-supported) CR due to available evidence of effectiveness7,8,10,17,30,31
- clinical cardiac procedures, acute treatment and interventions
-
non-high-income countries are equated to developing countries, according to the ‘List of developing countries as declared by the Minister of Foreign Affairs(2015)’32. This is because studies that focus on developing countries are considered to have little relevance in Australia, which is amongst the 10 largest advanced economies in the world, based on International Monetary Fund criteria33.)
- programs that include only one component of CR (eg exercise), rather than having a holistic view
- outside the date limit, to ensure a contemporary basis due to rapid changes in technology that have had a large impact on possibilities for CR in rural and remote areas and due to the recent decentralisation of health services in Queensland, the establishment of primary health networks and their impact on health service delivery.
Whilst this study includes all adults living independently in rural and remote areas of Australia as well as high-income countries, because of the known poor health status of Australian First Peoples1,3 studies were sought specifically for CR with Aboriginal and Torres Strait Islanders people and/or Indigenous people. Using this strategy, six studies with a primary focus on Australian First Peoples were identified. No international studies were identified specifically for Indigenous people.
Preliminary review and critical appraisal
Principles and processes of the Preferred Reporting Items for Systematic Reviews and Meta-Analyses (PRISMA) (Fig1) was used to describe the collection, review and identification of final studies for analysis34.
Following screening of abstracts, a full text critical review to assess research quality, outcomes and eligibility was undertaken on the remaining 56 quantitative, qualitative and mixed method studies. A modified process, suitable for critical review of all research methods, was developed based on the premise that all research includes clearly focused research questions, constructs arguments, collects data from appropriate participants, speculates about outcomes of data analysis35-37 and considers important outcomes and results38-40. To achieve this, McMaster’s qualitative research guidelines40, and the Critical Appraisal Skills Program quantitative review guidelines38, were combined. Studies were assessed according to McMaster’s guidelines for study design, type, methods, sampling and data collection38 and Critical Appraisal Skills Program quantitative research guidelines to assess the research question, including appropriate sampling, equal treatment of all participants, chance minimisation and research rigor, with all results presented to ensure epidemiological and statistical strength38. The critical review was further strengthened by a thematic analysis in which key findings were coded and grouped to identify ‘patterned responses’ or ‘themes’, to enable extraction of further meaning36.
Supplementary table 2 provides details of the critical review and thematic analysis carried out by the first author and peer reviewed by the other authors. This process of review and validation continued throughout.
Following the critical review and thematic analysis, a further analysis, evaluation and integration of findings from the 16 final studies that identified barriers, enablers and pathways was undertaken. These are synthesised in the results according to identified themes.
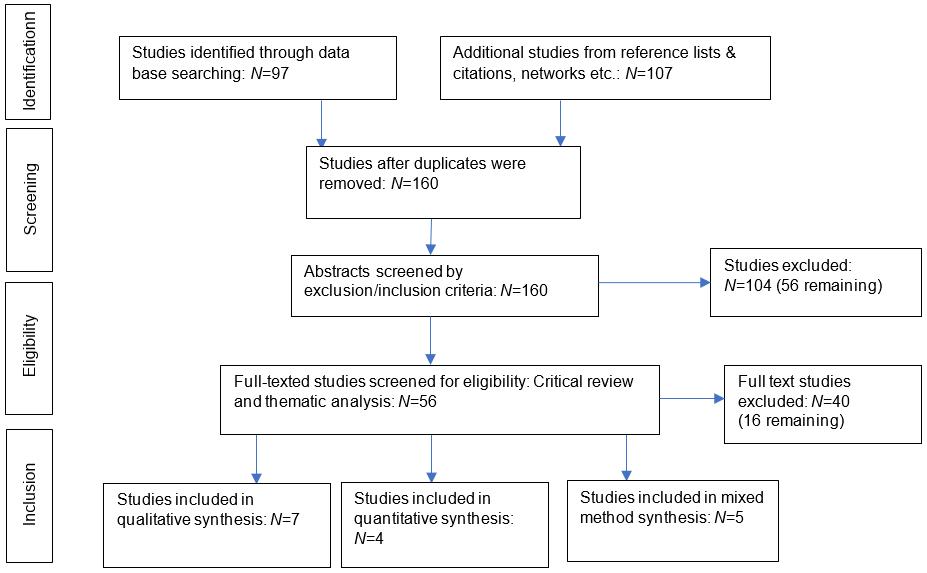 Figure 1: Modified PRISMA chart34: Integrative review of studies on cardiac rehabilitation for people in rural and remote areas
Figure 1: Modified PRISMA chart34: Integrative review of studies on cardiac rehabilitation for people in rural and remote areas
Results
The review and analytic process identified 16 studies, from which five themes emerged. Table 1 summarises the pertinent themes including factors that influence failure or success of CR. These factors provided the underpinning criteria for the emergent themes. The themes identified were referral, health service pathways and planning; cultural and geographic factors necessitating alternative and flexible programs; professional roles and influence; knowing, valuing, and psychosocial factors; and financial costs – personal and health services. Embedded in these themes are barriers, enablers and pathways for CR in rural and remote areas by general population and Australian First Peoples.
Table 1: Themes identified through critical analysis and underpinning thematic criteria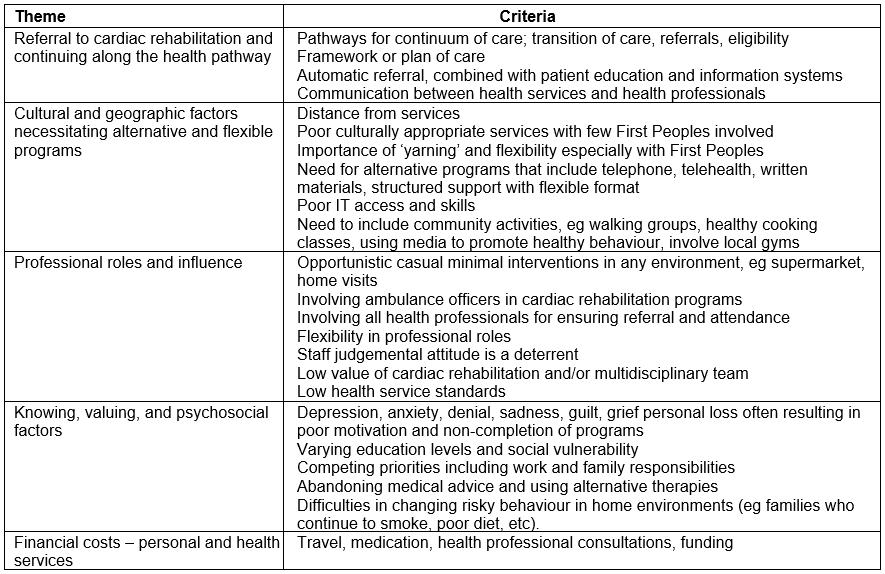
Referral, health services pathways and planning
General populations: Low levels of referral are commonly identified as barriers to CR18-21,23,24,41. Education and information about heart disease risk factors and the benefits of CR are an important part of hospital discharge and referral processes22-24. A transition of care framework and care planning, together with systematic assessment to ensure that participants have appropriate, and if necessary, individualised programs, is recommended21,23 (Table 2).
It is known that there is a lack of data on CR referrals, attendance and completion of centre based or home based programs16. At times the studies recommended that people ‘eligible’ for CR are referred by their treating doctor18,42. No eligibility criteria were identified in the selected studies. Many potential CR participants were deemed ineligible without explicit decision-making criteria18,42. Other barriers to CR include non-completion or delay in post-hospitalisation referrals, lack of information and prioritisation of CR21,23,24,41 (Table 2).
Table 2: Final analysis, evaluation and integration – general populations18-24,41-43 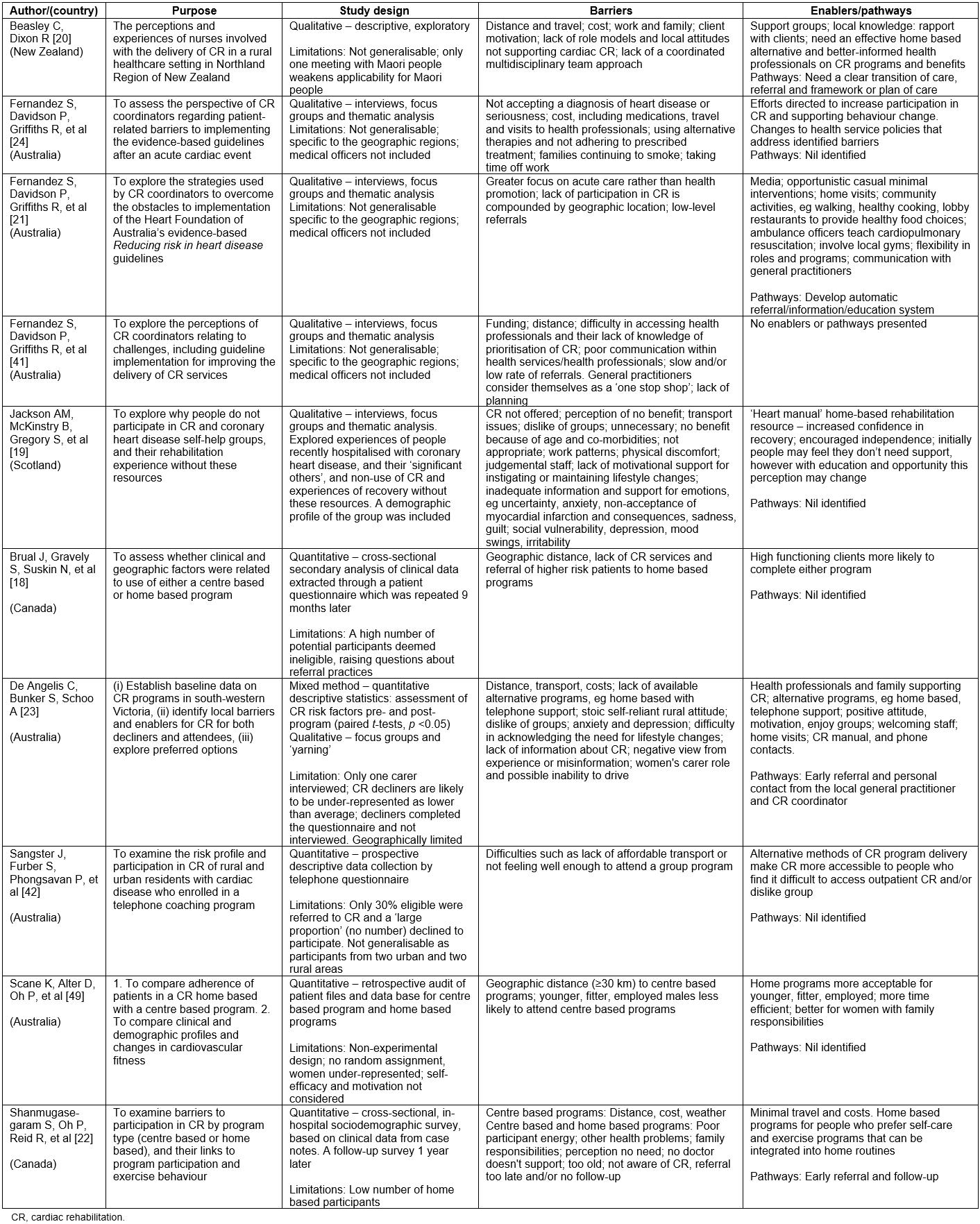
Australian First Peoples: Lack of data on referral rates and poor discharge planning were identified as barriers to CR for Australian First Peoples43,44. Lack of services, low levels of involvement of Australian First Peoples staff and culturally inappropriate services are identified as contributory factors to low rates of CR referral and access43,45-47. In one community in Western Australia, the number of people who attended CR was reported as being augmented by self-referral of people interested in learning more about health and risk factors rather than formal referrals or involvement in CR46,47 (Table 3).
Table 3: Final analysis, evaluation and integration – Australian First Peoples43-48 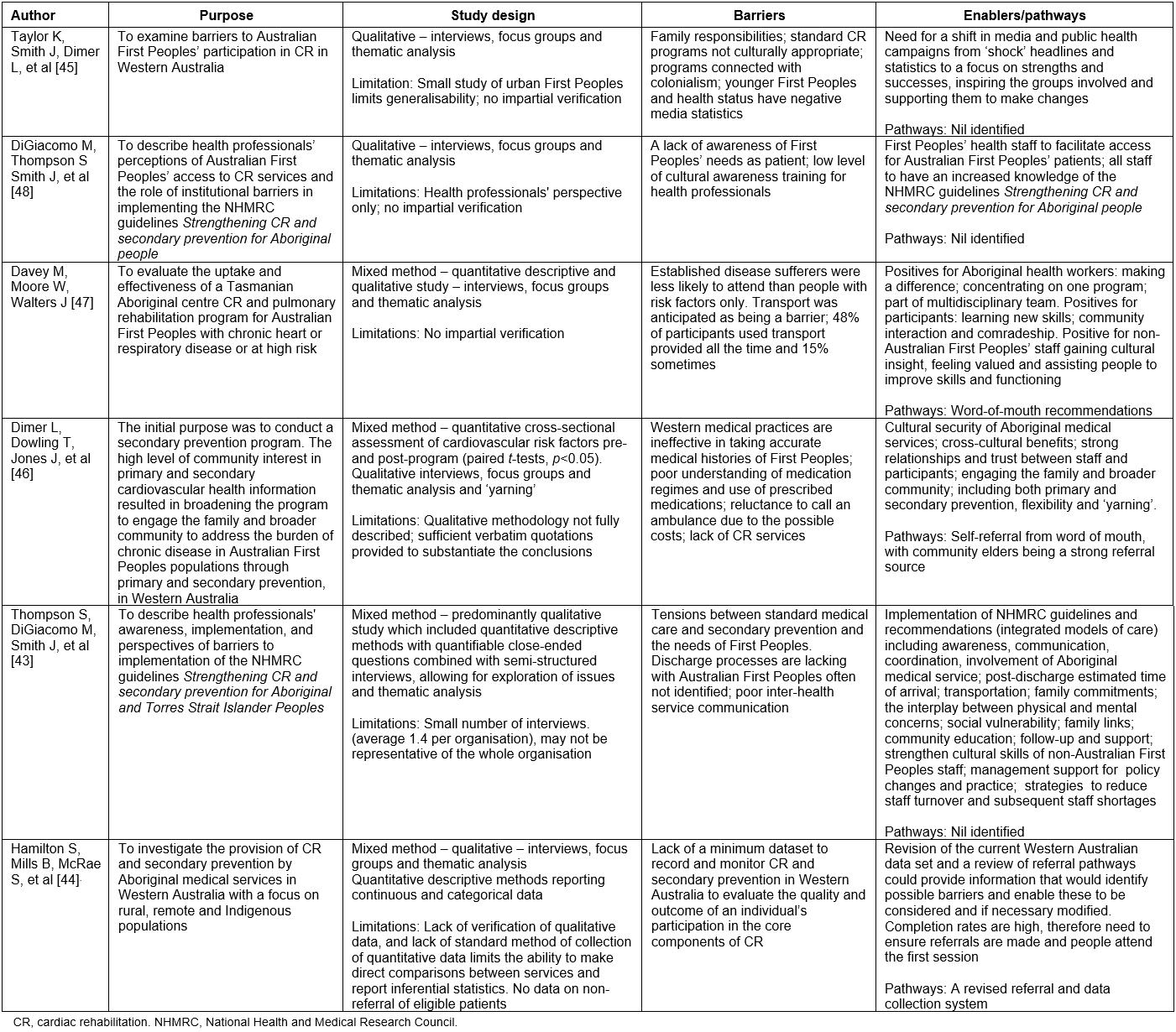
Cultural and geographic factors necessitating alternative and flexible programs
General populations: A range of studies identified that alternative approaches to CR are required due to low levels of geographic access in rural and remote communities18,19,23,41,42,49. It is known that distance from services impacts on access to CR18,21,23. Technological or personal support home based programs are identified as alternatives to centre based programs20,22,23. There is a demonstrated need for flexible and individualised programs to accommodate factors related to employment, age and gender, supported by community involvement19,20,24. The use of a ‘heart health’ manual combined with home visits has been shown to be of benefit19. Innovative management policies are recommended to enable alternative and flexible models necessary to meet individual and local needs23,24 (Table 2).
Australian First Peoples: Studies repeatedly found that First Peoples programs must be of high standard, culturally appropriate, holistic, flexible and include family and community43,45,48. Indigenous health workers are identified as an essential part of the health service team, which needs strong relationships and trust within the team and program participants46,48. Strong links with mainstream health services are necessary whilst retaining flexibility and individuality, such as ‘yarning’ or storytelling to encourage attendance43,46 (Table 3).
The barrier of distance from services is not identified by First Peoples to the same extent as for the general population18-23,23-25,41 (Table 2). In one Tasmanian First Peoples study, transport was provided for participants. This was regularly used by 48% of the participants and by 15% ‘some of the time’47 (Table 3).
Professional roles and influence
General population and First Peoples: Medical officers and/or CR coordinators’ personal involvement, accessibility and follow-up, together with supportive and non-judgemental attitudes, were found to be enablers for CR attendance19,20,23. Further enablers identified included health professionals’ knowledge and prioritisation, their willingness to share information and work as part of a coordinated multidisciplinary team, as well as ensuring effective interhealth services communication47 (Table 2).
There is evidence that professional relationships between Australian First Peoples and general population staff are strengthened when they are based on trust and respect, with Australian First Peoples in primary professional roles43,46,48. Improved cultural skills of general population staff are of primary importance in this process. These are identified as core components for effective CR and secondary prevention for Australian First Peoples43,46. Two studies involving Australian First Peoples also identified multidisciplinary teams as being important, together with flexibility of professional roles45,48 (Table 3).
Knowing, valuing, and psychosocial factors
General population: Public perception generally demonstrated that CR is unnecessary for younger, fitter people49, or not suitable for people with comorbidities or advanced disease24,42. Lack of information, few positive role models, negative local attitudes, poor experience or misinformation, and insufficient health professional support, have all been identified as limiting the perceived value19,20. It is also noted that people experience difficulty in acknowledging the need for lifestyle changes, especially if families continue with risky behaviour such as smoking24. People may opt to deny the need for risk modification, cease taking their prescribed medications and seek alternative therapies21 (Table 2). Depression, anxiety, denial, sadness, guilt, grief and personal loss have been found to result in poor motivation and non-completion of programs23 (Table 2).
Australian First Peoples: Inequities in First Peoples health services are compounded by ‘Western’ medical practices reported to be ineffective in taking accurate medical histories43,46 and to mirror a ‘power inequity that resembles colonialism’42,47,48. The need for flexible and innovative programs that consider all aspects of chronic disease risk factor minimisation, with a possible focus on primary and secondary prevention and consideration of mental as well as physical health, to address these barriers has been identified43 (Table 3).
Financial costs – personal and health services
General populations: On a personal level, travel costs, medications, visits to health professionals and potential loss of income due to work commitments are identified as significant barriers to CR19,21-23 (Table 2).
Australian First Peoples: Current studies do not identify the same financial issues for First Peoples, who largely attend local Indigenous medical services or government health services, which, whilst accessible, provide few CR or secondary prevention services43,46 (Table 3).
Limitations
The methodological quality of articles was assessed and demonstrated validity in research methods, with some limitations (Tables 2,3). The majority of qualitative and mixed method studies used purposive sampling and semi-structured interviews19-21,24,41,43,44,46-48, with data analysed and themes identified using NVivo software. However, many studies were limited in their generalisability due to specific geographic location of data collection19,20,23,41. Other limitations were non-inclusion of essential representatives (eg medical officers, carers and local indigenous people (Maori of New Zealand) 20,23,24,41,49 ), and lack of data verification45,47. Three quantitative studies were limited by lack of exclusion criteria (CR eligibility)18,43,50, with one sample not randomised45. One mixed method study relied on a small and possibly non-representative sample43.
Results are assimilated according to themes, barriers, enablers and pathways to provide information as a basis for developing a revised framework and perspective for CR referral and access models that will ultimately improve health and quality of life for all people with heart disease in rural and remote areas (Tables 4,5).
Table 4: Themes, barriers, enablers and pathways – general populations18-25,41,42,49 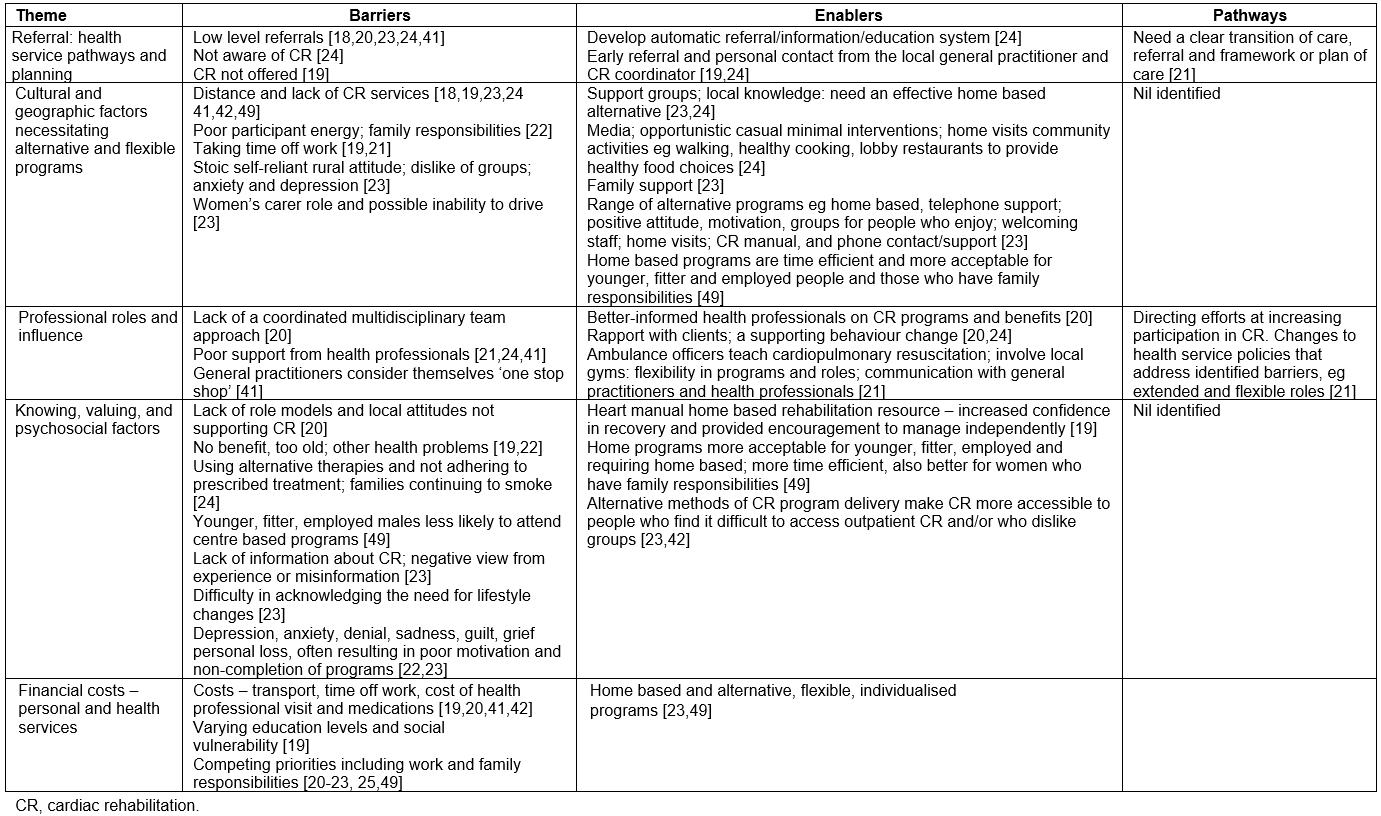
Table 5: Themes, barriers, enablers and pathways – Australian First Peoples43-48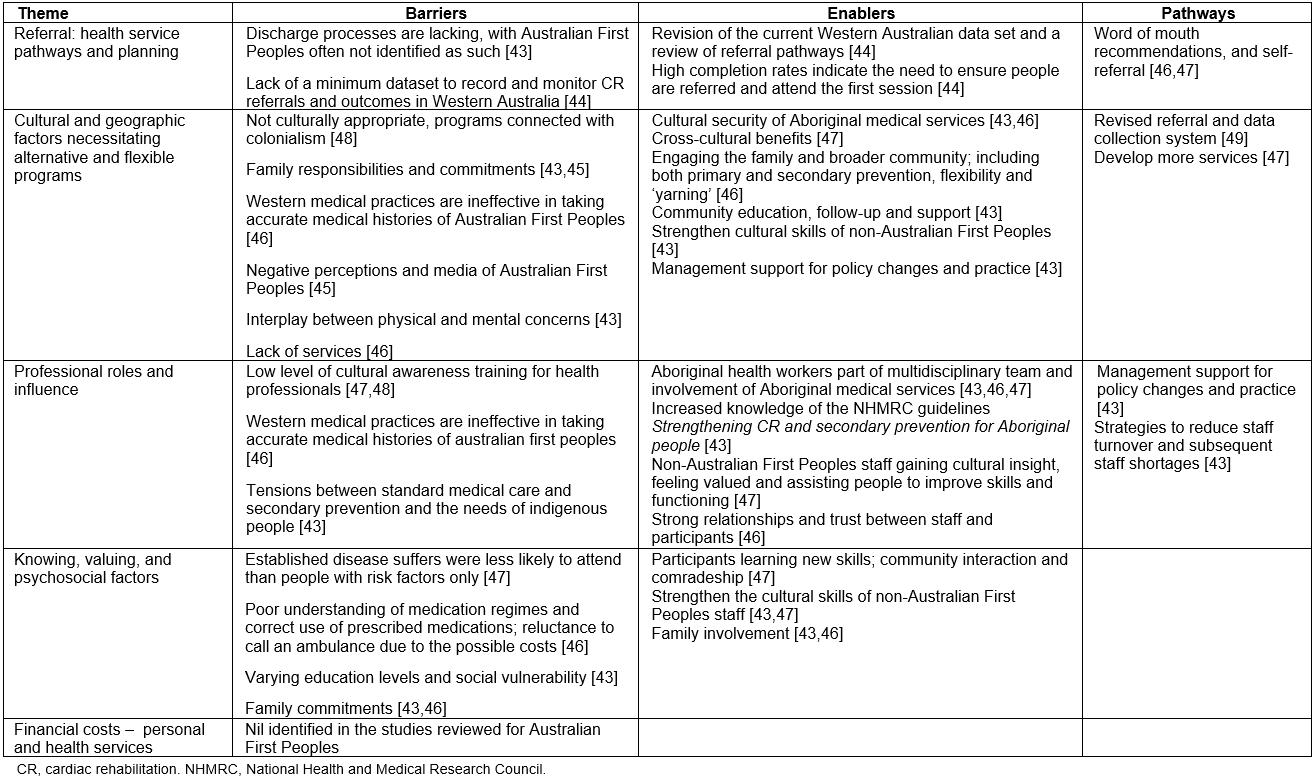
Discussion
CR is known to be effective in improving quality of life, reducing mortality, morbidity and hospital readmissions7,8,10, and consequently reducing costs for hospital treatment for heart disease7-10,51,52. The true value of CR is not realised in rural and remote areas due to poor access and/or attendance to CR services18-21,23,24,41. Whilst this integrative review provides information on barriers, enablers and pathways to models of referral and access to CR, there remain many unanswered questions, including why referral and attendance rates continue to be low despite the significant evidence of CR effectiveness. Whilst the reason for this is not completely understood, contributing factors identified in the selected studies include poor understanding of the benefits of CR by health professionals and potential attendees, compounded by low levels of referral19,21,23,24,42. Whilst some pathways of referral and transition of care planning are reported, referral rates are not known in many areas of Australia.
Early results of a recently instituted Queensland Health CR database are insufficient to draw conclusions about referral rates in Queensland. It is anticipated that as data collection increases, this information will become available16,53.
Australian First Peoples experience many of the same barriers as the general population, compounded by cultural issues, lower socioeconomic and educational levels, and greater geographic isolation1,3. However, they have a greater need for CR, primary and secondary prevention due to higher levels of heart disease and comorbidities1,54,55. To provide Australian First Peoples adequate and effective CR, their increased involvement, together with non-Australian First Peoples’ improved cultural awareness, mutual trust, respect and two-way learning is required, as well as improved support and access to specialist services43,46-48. Many of these issues are not well investigated and described.
Costs associated with recurring heart disease are high and it is known that these costs can be reduced with improved systems that facilitate referral, accessibility and CR attendance6. To improve services, more information is required about hospital discharge and CR referral processes, including eligibility, inpatient education, perceived benefit and meeting participant needs.
The current situation demonstrates weak or poorly implemented systems. These include models of health services delivery, referral processes as well as inconsistent knowledge and value by health professionals and potential participants14,15,19,23,40,48, plus a range barriers to access and appropriateness of services. Many of the issues identified are common to health service provision and access to services in rural and remote areas of Australia56. As such, findings of this integrative review potentially have broad applications. To address the deficits, the following priorities need to be considered.
Referral, health services, pathways and planning
A systematic referral process based on well-defined criteria, individualisation of CR, personal contact, trust, information and support from health professionals13,22-24,46,49 needs further investigation. The systematic referral process, based on eligibility criteria, education on heart disease and risk factors, needs to commence prior to hospital discharge20,22,57.
Cultural and geographic factors necessitating alternative and flexible programs
Flexibility in CR is essential because of the diversity of demographic profiles, geographic location and health status in rural and remote areas23,41,47,48. Alternative models of CR, including home based programs with telephone support, such as Queensland Health’s Coaching Patients on Achieving Cardiovascular Health (COACH)17, telehealth, purpose designed apps and community involvement, are all known enablers for CR31,41. However, attendance rates remain low10,16,17. In Australia there is little evidence of CR being provided by Aboriginal/Indigenous medical services, compounding poor access to CR by Australian First Peoples who live in remote area communities. This highlights the need for further advocacy and a review of systems of health care for Australian First Peoples in remote area communities. In line with a holistic and culturally appropriate approach and scarcity of resources, consideration of an integrated, flexible primary and secondary prevention model that is appropriate for Australian First Peoples as well as the general population needs further investigation.
Professional roles and influence
Key issues identified include ongoing staff shortages14,15, indicating the need for increased professional role flexibility and modified multidisciplinary team models, supported by appropriate management policy15,43. A further priority is including a primary role in CR, supported by further education, for Indigenousl health workers working with Australian First Peoples43,45,47. These are all key issues that need further consideration to work towards optimal effectiveness of CR in rural and remote areas.
Knowing, valuing, and psychosocial factors
Poor understanding of the concepts and benefits of CR contributes to low attendance rates19,21,23,25,41,57,58. This is exacerbated by the general perception that acute care health services are of greater importance than primary and secondary prevention services24. Lack of knowledge and negative perceptions of CR need to be addressed. Mental as well as physical health issues are of primary importance and currently not prioritised in many CR programs19,21,23. A holistic approach to CR, primary and secondary risk factor prevention and use of resources need further consideration46.
Financial costs – personal and health services
Through effective CR it is known that healthcare costs can be significantly reduced through a reduction in reoccurrence of heart disease and hospital readmissions6. To achieve increased CR participation, improved professional understanding and support is essential41. The cost factors for general populations include travel, loss of work, cost of health services, professional consultations and medications19,23,24,42. It is also reported by James Cook University, Cairns and Apunipima Indigenous health services (unpublished internal report, 2016) that Australian First Peoples are faced with financial costs, practical and cultural barriers when attending centralised specialist services that require them to travel and stay away from their families and community. The overall low level of health services in rural and remote areas results in poor access and overloaded services, and resultant staff turnover and cost implications14,15,42,59. Reconsideration of the system, current health services and resource allocation is required.
Limitations
Due to the predominantly qualitative or mixed method research the results are not outcome focused and have limited generalisability due to the specific geographic areas and small purposive contextual samples of the studies. Therefore, conclusions drawn by this integrative review on health service systems and services are based in part on selected studies’ discussions, findings and conclusions, and subject to the limitations of the study. No northern Queensland or Northern Territory studies on CR were identified in this integrative review. These are extensive regions of Australia with large rural and remote areas. This and the overall low number of studies indicate the need for further research to improve information that will facilitate decision making and identify further CR enablers and pathways and minimise barriers specific to rural and remote areas of Australia, so that service improvements can be achieved.
Conclusion
The purpose of this integrative review was to explore barriers, enablers and pathways for access to CR, with the aim of optimising services, improving health and quality of life for all people living independently in rural and remote areas. The review indicates that CR services are fragmented and lack a systematic policy driven approach, with resultant low levels of referral and access. Even when alternative services are offered in Australia (eg COACH), attendance rates remain low.
To address this, the following elements for improved referral and access to CR need further investigation and development:
- referral systems and eligibility criteria
- availability and access to flexible centre based and home based CR programs including telephone/personal support and technology based programs via telephone apps, with distance support
- education/awareness/training on CR for providers and potential participants, family/significant others
- information systems for CR referral and access
- improved education and training for general populations staff on Australian First Peoples’ cultural issues
- improved workplace support and education for Indigenous health workers
- greater flexibility and extended professional roles supported by management policy and protocols
- consideration of combined CR primary, secondary prevention and risk factor management
- improved funding.
CR works to improve health status and reduce costs, and there are a range of ways to provide effective services for more people. These include a systematic, policy driven approach that includes referral, eligibility and access. This is necessary if CR is to fulfil its role as a valuable tool in substantially lowering coronary heart disease morbidity and mortality. Understanding and addressing these factors has the potential to reduce costs, through reduced cardiac events and hospital readmissions as well as improved quality of life and contribute to improved CR and/or secondary prevention services and ultimately health outcomes for all people living independently in rural and remote areas of Australia.




