Introduction
Behavioral health workforce shortage has been a huge public health issue for decades in the USA1, but a number of recent trends such as opioid epidemics pushed the issue to the forefront of healthcare reform. Previous studies have found that the supply of behavioral health professionals in rural areas is inadequate to meet the demand for services2-6. Because of the increasing demand for behavioral health services, it is critically important to accurately measure the shortage of behavioral health professionals and develop policy measures based on the shortage estimates. One of the most commonly used approaches is to use licensure data on psychiatrists to estimate workforce supply and needs5,7. Although this approach is an inexpensive and easy way to estimate the supply of providers, it has many limitations, including (1) not all licensed professionals are actively practicing, (2) information on specialities is not available, (3) clinical contact time information is not available, and (4) satellite practice locations are not specified. An alternative is to implement an active surveillance system, which uses primary data collection in addition to licensure data to obtain detailed information.
In 2010, 19% of the US population lived in rural areas8. In the mid-western state of Nebraska, close to 30% of the population was living in rural areas8. In 2016, there were 258 Health Professional Shortage Areas (HPSAs) in Nebraska9. Because Nebraska is a more rural state and behavioral workforce shortage has been recognized as one of its priorities10,11. there is a better opportunity to study how to address workforce challenges in this environment. In 1995, the Health Professions Tracking Service (HPTS) program was established as a joint effort between Nebraska Department of Health and Human Services Office of Rural Health and the University of Nebraska Medical Center to document the retention of healthcare professionals practicing in the state.
HPTS was designed to assist with identification of federal and state shortage areas, workforce planning, emergency preparedness and formulation of health policies. HPTS is an active surveillance of healthcare professionals practicing in Nebraska through surveys of providers and healthcare facilities. HPTS data have been used as a primary source for bi-annual behavioral workforce reports since 201312-14. The objectives of the study are to (1) compare the behavioral health workforce estimates based on licensure data to estimates based on HPTS data, (2) examine the potential impact on workforce supply estimates when part-time and clinical hours are considered, and (3) examine the potential impact on shortage designation when multiple practice locations are considered. Potential future directions for workforce supply and needs assessment in the context of the integrated care movement and continued expansion of telehealth use have also been discussed.
Methods
Provider types
The behavioral health professionals examined in this study include psychiatrists, psychologists, advanced practice registered nurses (APRNs), physician assistants (PAs), licensed independent mental health practitioners (LIMHPs), licensed mental health practitioners (LMHPs) and licensed alcohol and drug counselors (LADCs). Psychiatrists included in this study are those individuals board-certified by the American Osteopathic Board of Neurology and Psychiatry or by the American Osteopathic Board of Neurology and Psychiatry and board-eligible (ie has completed an accredited program of graduate medical or osteopathic education in psychiatry or child psychiatry) allopathic or osteopathic physicians specializing in psychiatry. Residents and house officers were excluded from the analysis.
APRNs providing behavioral health services include those who self-identified psychiatry as their primary or secondary practice specialty. Thus, APRNs practicing psychiatry include both those who are and are not board-certified in psychiatry. APRNs who are board-certified in psychiatry hold a national board certification from the American Nurses Credentialing Center. PAs practicing psychiatry include those who self-identified psychiatry as their primary or secondary practice specialty15,16.
Independent behavioral health professionals include psychologists and independent mental health practitioners. Independent behavioral professionals may hold more than one license. Psychologists included in this study are those who hold a license to practice psychology and are actively practicing psychology. Independent mental health practitioners include those who are licensed and actively practicing as independent mental health practitioners. Services to individuals, couples, families, and/or groups provided by licensed independent mental health practitioners include providing treatment, assessment, psychotherapy, counseling, or equivalent activities for behavioral, cognitive, social, mental, or emotional disorders, including interpersonal or personal situations with or without consultation with a qualified physician or licensed psychologist17,18.
Other behavioral health professionals include licensed mental health practitioners and alcohol and drug counselors. Other behavioral professionals may hold more than one license. Mental health practitioners include those who are licensed and actively practicing as a mental health practitioner. Services to individuals, couples, families, or groups provided by a licensed mental health practitioner include providing treatment, assessment, psychotherapy, counseling, or equivalent activities for behavioral, cognitive, social, mental, or emotional disorders, including interpersonal or personal situations; and initial assessment of organic mental or emotional disorders for the purpose of referral or consultation. The major difference between LMHP and LIMHP is that LIMHPs can independently diagnose a major mental illness or disorder, whereas LMHPs cannot do the same without a qualified physician’s supervision or consultation19. Addiction counselors include licensed alcohol drug counselors, and could have a dual license including this and one as a certified disordered gambling counselor. However, individuals with solely the latter license were excluded.
Licensure data
Physicians in the USA are not licensed based on their specialty (state licensures are ‘undifferentiated’)20. This is why the specialty data are not required to be collected by the licensure board. Similarly, APRNs and PAs can practice psychiatry and other specialty areas without certifications15,16.
The state of Nebraska licenses, certifies, and registers various professionals and occupations including healthcare providers. All licenses are renewed every 2 years. Physicians need proof of graduation from accredited medical school, approved graduate medical education and licensing examination. A license is renewed with 50 hours of American Medical Association approved continuing education. Psychologists need a doctoral degree in psychology, American Psychological Association accredited internship, supervised postdoctoral experience, Examination for Professional Practice of Psychology and board-developed jurisprudence examination. A license is renewed after meeting the 24 hours of continuing education requirement. APRNs require a completed approved program, 30 contact hours of academic education in pharmacotherapeutics, a separate coursework in advanced health assessment and pathophysiology or psychopathology, credentialing examination and graduation or 2080 hours in a nurse practitioner role in the past 5 years. A license is renewed with the requirement of continued education. PAs are required to pass the Physician Assistant National Certifying Examination. The license is renewed with the completion of 50 hours of category 1 continuing education approved. The LIMHP license requires an accredited master’s degree, required examination for LMHP and least 3000 hours of post-masters experience. A license is renewed with at least 32 hours of mental health related continuing education. LMHP licenses require an accredited master’s degree in therapeutic mental health, 3000 hours of supervised experience in mental health practice and examination for LMHP. LADCs require completion of 6000 hours of supervised clinical work experience and completion of the Examination for Alcohol and Drug Counselors given by the International Certification & Reciprocity Consortium/Alcohol and Other Drug Abuse. A license is renewed with 40 hours of continuing education16.
Health Professions Tracking Service
The HPTS is located within the University of Nebraska Medical Center’s College of Public Health. The HPTS maintains a relational database of Nebraska’s licensed healthcare professionals including behavioral health professionals. Using the Nebraska licensure database as the sampling frame, annually HPTS surveys healthcare professionals practicing in Nebraska, located in Nebraska with an ‘unknown’ status, and newly licensed in Nebraska (regardless of location). The surveys for professionals practicing in Nebraska, pre-populated with previously identified practice information, provide professionals the opportunity to update their information. Also, practice locations for physicians, advanced practice registered nurses and physician assistants are surveyed semi-annually. HPTS verifies non-respondents to the semi-annual practice location surveys by periodically contacting the practice locations to verify and document the practitioners and contact information. At this time, the practice locations of psychologists, licensed independent mental health practitioners, licensed mental health practitioners, and licensed alcohol and drug counselors are not surveyed, and those results rely on cumulative responses to the individual survey.
Analysis
Providers may hold more than one license. However, each provider is counted only once in this study. In case a provider held more than one license, the health professional was assigned a license based on the following hierarchy: psychiatrist, psychologist, APRN, PA, LIMHP, LMHP, LADC. The HPTS database contains information on time distribution of the behavioral health providers. The time spent with patients was calculated as the percentage of hours out of 40 hours per week spent in clinical practice for full-time employed providers. For part-time employed providers, time spent with patients was calculated separately (Table 1). Full-time/part-time status for the providers was calculated and reported regarding full-time equivalent (FTE). Total FTE was calculated by counting a full-time provider as 1.0 FTE and a part-time provider as 0.5 FTE. Using 0.5 FTE to quantitatively represent the part-time provider contributions was considered the best approach as a consensus resulting from feedback from administrators of behavioral healthcare organizations and behavioral health providers.
HPTS tracks professionals who have a primary or satellite practice location in Nebraska. Primary practice location is defined as the location where the professional spends the majority of his/her practice time. Using the primary Nebraska location reported in the survey avoids counting a professional more than once, while not excluding professionals that only have satellite locations in Nebraska. Two choropleth maps were created for a visual exhibition of shortage areas in Nebraska. To designate an area as a shortage area, the federal HPSA criteria were used. An area was designated as an HPSA if it exhibited a ratio less than one psychiatrist per 30 000 population. The first map, an enumeration of psychiatrists, was based on the primary location only. The second map, the enumeration of psychiatrists’ primary and satellite locations, counted the psychiatrists once if the primary and satellite location fell in the same county. With primary and secondary locations in separate counties, each county was considered to have one serving psychiatrist. The data were analyzed using SAS v9.3 (SAS Institute; https://www.sas.com/en_au/home.html) and maps were created with ArcMap v10.4.1 (Environmental Systems Research Institute; http://desktop.arcgis.com/en/arcmap).
Table 1: Percentage of hours spent weekly in clinical practice by provider type in Nebraska based on Health Professions Tracking Service data, 2016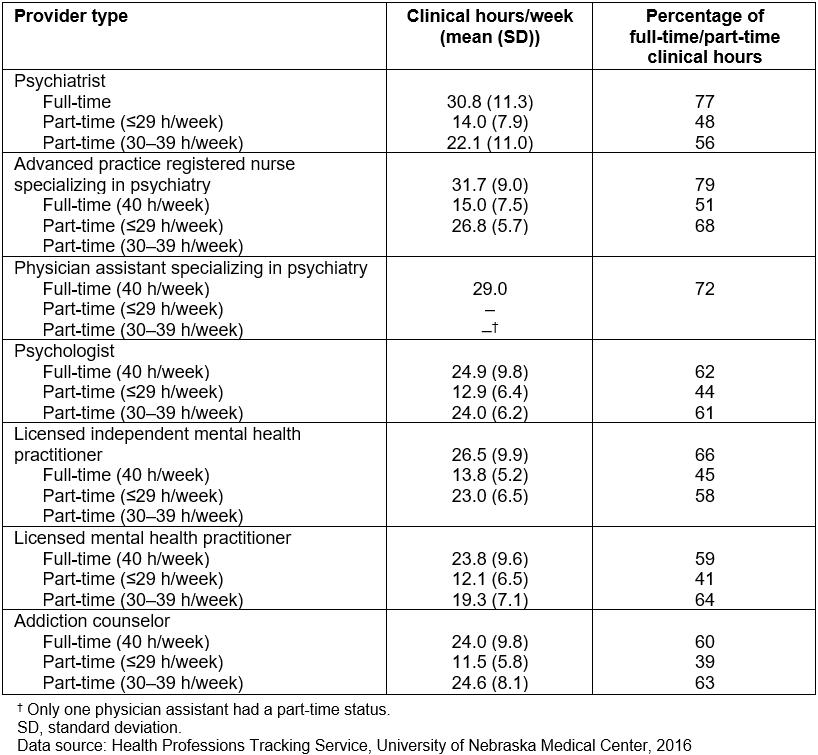
Results
Table 2 compares the number of providers based on the state licensure database and HPTS data. According to HPTS data, there were 164 psychiatrists, 113 APRNs specializing in psychiatry, and 15 PAs specializing in psychiatry identified as practicing in Nebraska in 2016. The information for these provider types was not available from the licensure database because licensure does not record specialty information. For the remaining provider types, the licensure database identifies providers licensed to practice in Nebraska; however, licensure does not identify if providers are actively practicing in Nebraska. If only the licensure database is relied upon, the supply for the active providers will be overestimated by 24.1% (LIMHPs) to 57.1% (addiction counselors), thus underestimating the shortage of behavioral health professionals.
The largest difference between the licensure database and HPTS data is observed for addiction counselors holding only the licensed alcohol and drug counselor license. Less than half of licensed individuals are identified practicing in Nebraska (245 in licensure database v 105 in HPTS database). Provider licenses are renewed every 2 years and if somebody retires or discontinues practicing in Nebraska, there is no way of knowing the status of practice unless providers or clinics are surveyed. In some cases, providers may choose to maintain licenses in multiple states (ie Nebraska and another state) although they are not actively practicing in Nebraska. Again, the status of practice in Nebraska cannot be known unless the providers or clinics provide such information.
Table 3 shows the supply of behavioral health providers by full-time and part-time status and estimated full-time equivalents (FTEs). Here, working 0.5 FTE was assumed as part-time. If only the number of providers is used without taking into consideration part-time status, the workforce supply is estimated by 10.0% (PAs) to 17.4% (LMHPs). A further analysis of HPTS data shows that the importance of examining clinical hours each provider spends seeing patients (Table 1). On average, full-time behavioral providers spend anywhere between 23.8 (LMHPs) to 31.7 (APRNs) hours per week seeing patients. What this means is providers such as full-time LMHPs and psychiatrists who spend about 23–30 hours as clinical hours respectively are spending only about 59–77% of their time seeing patients. Even the providers who spend more time (full-time APRNs) are spending only 79% of their time for clinical services.
Figure 1 shows the number of practice locations reported by providers. Of the total 2,667 professionals practicing in Nebraska, 370 or 14% had more than one practice location in the state. Figures 2 and 3 illustrate differences in shortage area designations when satellite practice locations are considered. Figure 2 is based on data where only the primary practice location of the provider is used. This shortage area map based on primary practice location of the psychiatrists shows that 87% (81 out of 93) of counties in Nebraska do not have a psychiatrist serving as a primary practice place. Two counties, Hall and Douglas, are below the HPSA designation of psychiatrist-to-population ratio. Nine counties (9.6%) are at or above the HPSA designation ratio of psychiatrist-population. The majority of the rural counties (91.6%, 77 out of 84) do not have a psychiatrist or are below the Federal HPSA ratio. Furthermore, 66.6% of the urban counties (6 out of 9) do not have a psychiatrist or are at below the federal HPSA ratio. Figure 3 is a shortage area map based on all practice locations of psychiatrists (primary plus satellite). It shows that seven counties shifted from having no psychiatrist to a status of at or above the federal HPSA ratio, indicating some care is being provided through satellite locations.
Table 2: Comparison of number of behavioral health providers in Nebraska based on licensure and Health Professions Tracking Service data, 2016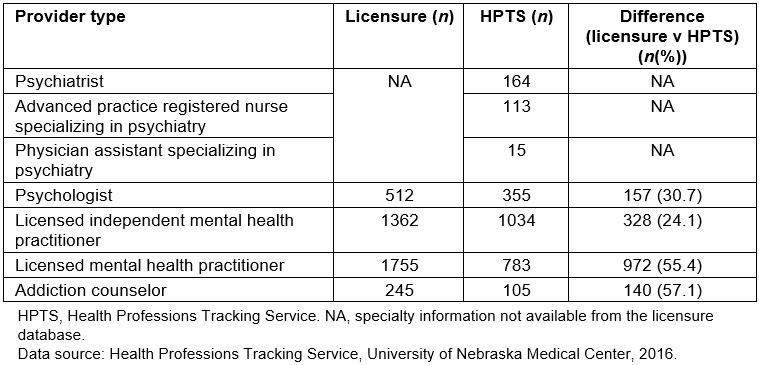
Table 3: Supply of behavioral health providers by work status in Nebraska based on Health Professions Tracking Service data, 2016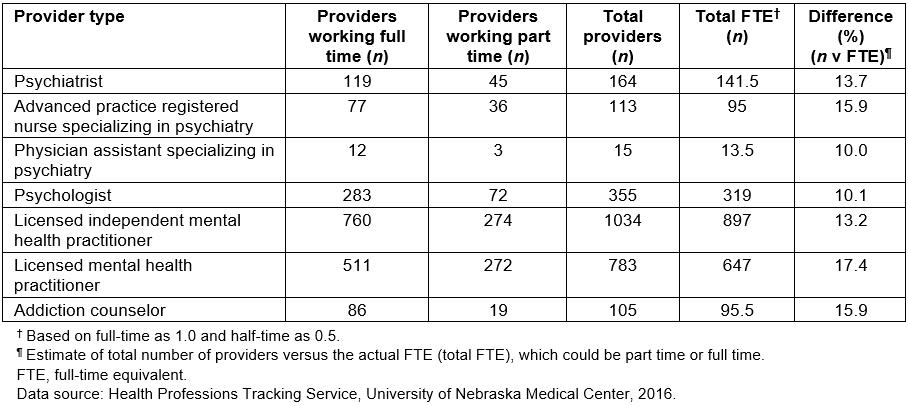
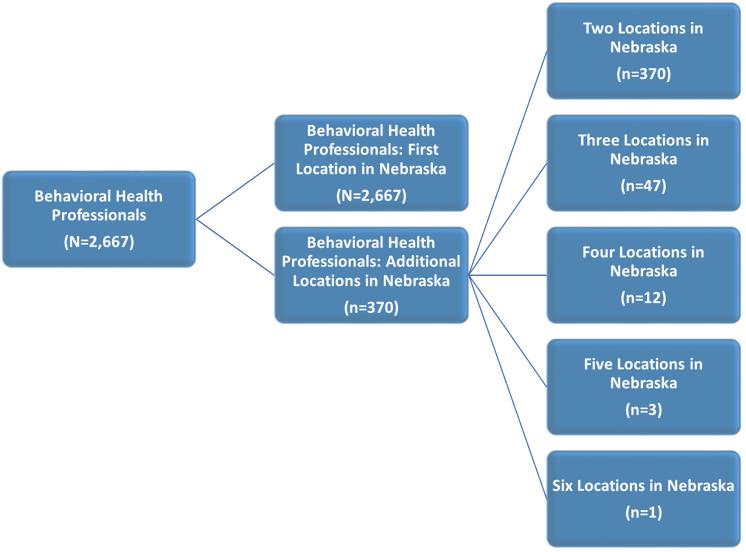 Figure 1: Behavioral professionals with multiple practice locations, Health Professions Tracking Service 2016.
Figure 1: Behavioral professionals with multiple practice locations, Health Professions Tracking Service 2016.
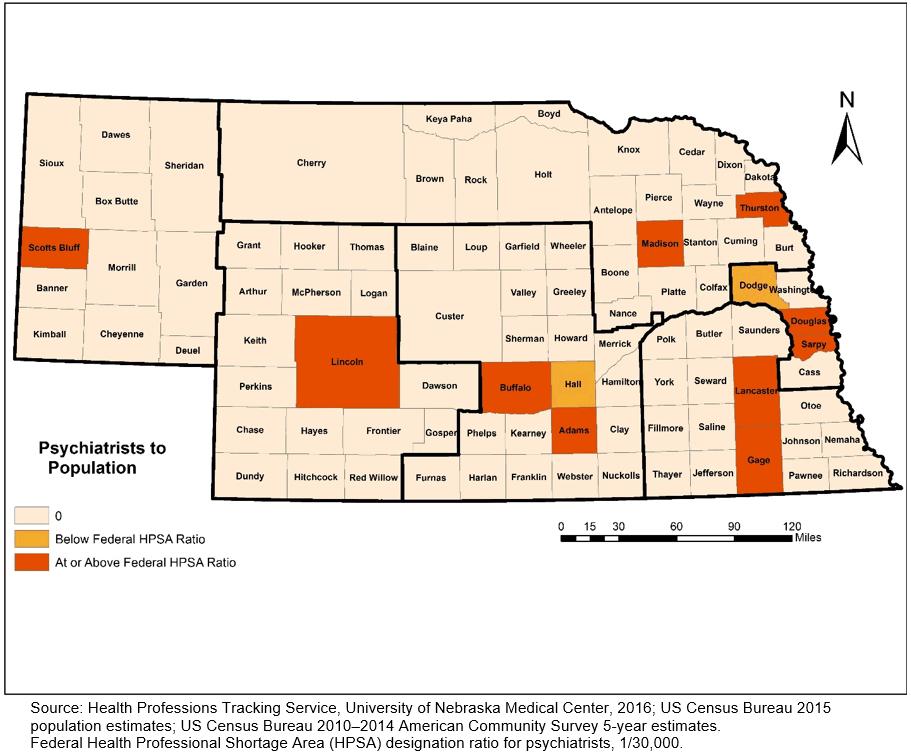 Figure 2: Psychiatrist-to-population ratios based on primary practice locations in Nebraska, 2016.
Figure 2: Psychiatrist-to-population ratios based on primary practice locations in Nebraska, 2016.
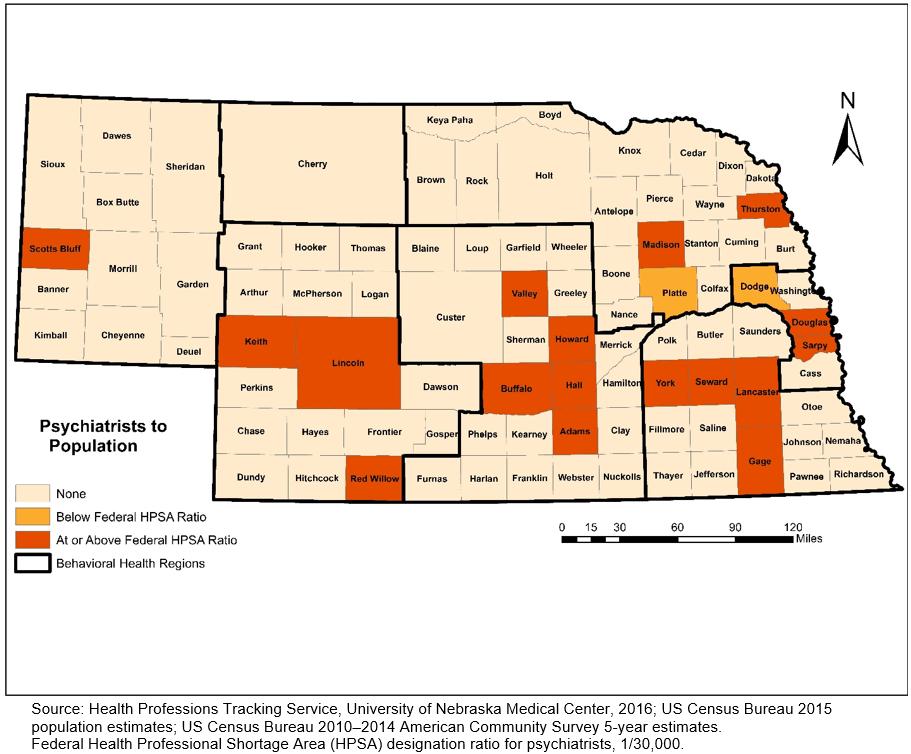 Figure 3: Psychiatrist-to-population ratios based on all (primary plus satellite) practice locations in Nebraska, 2016.
Figure 3: Psychiatrist-to-population ratios based on all (primary plus satellite) practice locations in Nebraska, 2016.
Discussion
The analysis conducted for this study indicates that the sole use of the licensure data can potentially produce a substantial overestimation of behavioral health workforce supply, and thus an underestimation of behavioral health professional shortage. The discrepancy was largest for addiction counselors (57.1%) and LMHPs (55.4%), followed by psychologists (30.7%). These differences are mainly due to the licensure data including those who are not actively practicing in the state (ie retired, inactive or having multiple state licenses and only practicing in another state). HPTS data were further analyzed on actively practicing providers by examining the full- and part-time status. When this practice status was taken into consideration, the estimated supply of actively practicing behavioral health professionals was further reduced by an additional 10–17%. Again, the reduction was largest for addiction counselors. Also, without taking the provider’s clinical hours spent with patients into consideration, the actual shortage of behavioral health professionals may be underestimated as well. Healthcare providers do not spend all of their working hours seeing patients in a clinical care setting. Some providers may have a heavy administrative workload or may be involved in teaching and research. For example, it was found that on average, full-time psychiatrists spend 30.8 hours per week in clinical care. Healthcare shortage area designations have a potentially large impact on policy development and assessment because it is often tied into resource allocation. On the other hand, without counting satellite practice locations, the shortage of behavioral health professionals may be slightly overestimated. HPTS data were analyzed to compare the shortage designation based only on primary location to the designation based on all practice locations. Of 81 counties with ‘no provider’ status, seven counties moved into at or above shortage status ratio.
There has been continual debate on ideal or adequate level of workforce supply to meet population demands for behavioral health care21-23. With a movement toward team-based integrated care, it has become apparent that simply counting the number of psychiatrists to calculate the provider-to-population ratio approach has limited value. In a team-based integrated care model, primary care providers play a larger role in prevention and management of behavioral health problems24-26. In this model, psychiatrists and other behavioral health professionals function as members of teams. As indicated in this study, over 10% of the behavioral health providers are practicing in multiple locations, some of which are in integrated care clinics. To understand the workforce supply and unmet gaps fully, perhaps there is a need to start examining the care team as a unit. This approach, however, calls for collection and examination of data at the healthcare facility and county level to see if patients in the coverage area have access to a care team that includes behavioral healthcare expertise. For example, the Nebraska survey includes questions about whether the physician clinics have access to behavioral health professionals to provide immediate care within the clinic or can schedule care with behavioral health professionals within the clinic.
Another study recently conducted in Nebraska also indicates that an increased number of providers are using telehealth for behavioral health care (unpublished data). Approximately half of Medicaid providers surveyed indicate that they have used telehealth to deliver some behavioral health services. Interviews of providers and administrators show that telehealth is a well-accepted mode of delivery from both provider and patient point of view. Lastly, more attention should be paid to quality of care and experience of patients and their families from diverse cultural and linguistic backgrounds27.
There are some limitations that should be noted when interpreting the results of the study. The number of clinical hours used in the analysis is based on self-reported data from providers. The accuracy of the information has not been verified with another data source. Another limitation is lack of information about telehealth. There are out-of-state mental health providers who provide behavioral health services via telehealth to Nebraska residents. In the future, in order to accurately estimate the ‘supply’ of behavioral health workforce and understand the unmet behavioral health care needs of the population, it would be important to quantify the behavioral health services provided through telehealth.
Conclusions
The USA has a shortage and maldistribution of behavioral health professionals, particularly in the rural areas of the country28. For Nebraska, primarily a rural state, the behavioral health workforce shortage is one of the priority issues. To make better policy decisions, the number and distribution of the actively participating workforce need to be accurately estimated. However, the most common enumeration method is not free from deficiencies and inaccuracies. State licensure data lack information on multiple licenses, practices that have more than one location, and there is loss to follow-up. These problems lead to inaccurate information. The enumeration method must consider the multiple practice locations of the providers and the actual time they spend with patients. Ongoing surveillance and information collection on top of what is already collected by the licensure data, such as HPTS, removes many of the barriers and substantially improves the accuracy of designating shortage areas and changes in future behavioral health workforce policies.

