Introduction
Many aspects of industrial health have received attention within the literature from early descriptions of industrial-related illnesses such as silicosis and high injury rates through to more recent literature which describes mental health and social concerns related to large numbers of fly-in, fly-out (FIFO) workers. The volume of literature on this topic has failed to include the needs of those health workers charged with caring for this special population of workers who experience specific health consequences as a result of their workplace/workstyle. This research has addressed this gap in the literature by providing an understanding of the experience of working in an industrial health role.
History of industrial health
Industrial health care is not a new concept, with links between occupation and employee health being described as early as 50 BCE1. The acceptance of major injury or loss of life in the pursuit of profit from acquisition of natural resources has become increasingly unacceptable in the modern industrial workforce. This has resulted in the comprehensive occupational health and safety legislation applied today. Early literature from the nursing and medical professions described industrial health as a specialisation and advocated for further research to support this role2-7.
The search to acquire natural resources forced industrial organisations into developing countries and difficult environments such as the North Sea, frozen tundra, jungles and deserts. In these locations, the health role consisted of mostly male first aiders or ambulance personnel employed to provide emergency care. Their education was facilitated by short courses and remote medical advice via phone or videoconferencing. Industrialisation, combined with numerous major incidents, particularly within the oil and gas industry, prompted an increasing focus on worker safety as opposed to overall health. The general health of workers has been largely missing from the now familiar title of health and safety8-10.
Cost of illness and injury
The remoteness of many locations means that evacuation of an ill or injured worker from a worksite may cost thousands of dollars, even before they are further repatriated to a requisite standard of care. Lost time injuries became the litmus test for good occupational safety practice and every effort was made to minimise these occurrences as they needed to be reported to regulatory agencies and could involve penalty for the industry. This paved the way for temptation to minimise the extent of some workplace injuries and illnesses11; therefore, any onsite health management was helpful in avoiding costly evacuation for minor conditions. This, however, required health workers to have great confidence in their ability to differentiate which cases they could manage and those they could not. Globally, mobile workers have been blamed for the spread of diseases such as measles12, tuberculosis13 and avian influenza as they frequently commute internationally between work and home. Thus, there has been a move away from predominantly trauma and injury response to primary health, hygiene and health education activities.
Long-distance commute workforce
Long-distance commute (LDC) staff work long hours in compressed rosters and are excluded from their social network and their home environment for days and weeks at a time. Many organisations choose to fly staff in to remote industrial sites worksites for roster periods rather than face the challenge of accommodating families in undesirable locations. Globally there are large numbers of workers engaged in LDC arrangements. In turn, these workers are well remunerated; however, this ‘workstyle’ may have a limited lifespan. Arguably the LDC workforce comes with numerous social implications such as increased risk of alcoholism, depression and suicide, obesity, gambling, and loss of social and family networks14-17. The present study supported many of these concerns including recent media and research attention regarding depression and clusters of suicides attributed to LDC work. FIFO worker suicide rates have been the subject of a recent Parliamentary enquiry in Western Australia18. Erny-Albrecht et al. showed that industrial workers lack access to often limited health services in remote areas19, while McEwan anecdotally noted that remote workers relied on emergency department services20, therefore lacking consistent integrated care because of a tendency to prioritise limited family time at home over seeking routine health maintenance.
Professional isolation and the health worker role
Coleman and Lynch defined professional isolation as ‘… physical distance, separation from learning environments and detachment from peers’21. For remote industrial health staff working across disciplinary boundaries, separation from peer networks is compounded by a lack of discreet professional identity. As Coleman and Lynch assert21, the opportunity to network with peers supports the culture and knowledge unique to a specific professional identity and development of more tacit concepts relevant to culture and communication, as identified by Trede22. Therefore, physical isolation and lack of appropriate professional association can lead to inappropriate and even dangerous perceptions of the industrial health role.
Differentiated health worker presence varies depending on the type and size of the industrial site. However, it is mostly nurses and paramedics employed in the health worker role who experience varying degrees of work typically associated with physiotherapy, occupational health, compliance monitoring, return to work coordination, workplace hygiene, health education and health promotion activities. Professional isolation, lack of specific role definition, education and support for the role, along with a lack of clear clinical and competency boundaries, predispose this group of health workers to coercive practices that could pose patient safety risks.
Methods
Rationale
The aim of the study was to understand the experience of working in a health role in an isolated industrial setting. Phenomenology is a qualitative research methodology useful for understanding the lived experience of a specific phenomenon23. This study therefore sought to understand the experience of nurses and paramedics working for a single Australian mining organisation in variously remote onshore and offshore industrial settings. This research was necessary to fill the void between primarily statistical data on industrial illness and injury and looming changes to the regulatory requirements of an industrial health role.
Data collection
Following approval to conduct the study, seven industrial health workers were recruited: two industrial medics, two paramedics and three registered nurses (Table 1). Participants were a purposive sample of nurses and paramedics working for a single international mining organisation. Participants were selected to provide a mixture of semi-remote and remote onshore Australian and remote offshore experience. All participants were asked in semi-structured, face-to-face or telephone interviews about their experience of working in an industrial health role. A short list of prompting questions was available; however, each participant was encouraged to describe their experience. Each interview was approximately 1 hour in length and was transcribed and analysed using an amended Colaizzi’s framework24. The steps in the framework outline a process of attributing meaning to significant statements and organising them into groups with thematic significance. In keeping with a constructivist phenomenological methodology, Colaizzi’s final step of returning to participants was not used owing to a tendency for participants to become more editorial and less contemporaneous than during their original account.
Significant statements were ascribed meaning and then clustered into thematically significant groups. Three major themes emerged: ‘contested spaces’, ‘isolation’ and ‘gaining and maintaining skills’. This reflected the complexity for nurses and paramedics required to deliver health care in remote industrial environments. This article reports on the theme of isolation, which was significant in three domains: geographical, personal and professional.
Table 1: Characteristics of nurses and paramedics working in remote industrial settings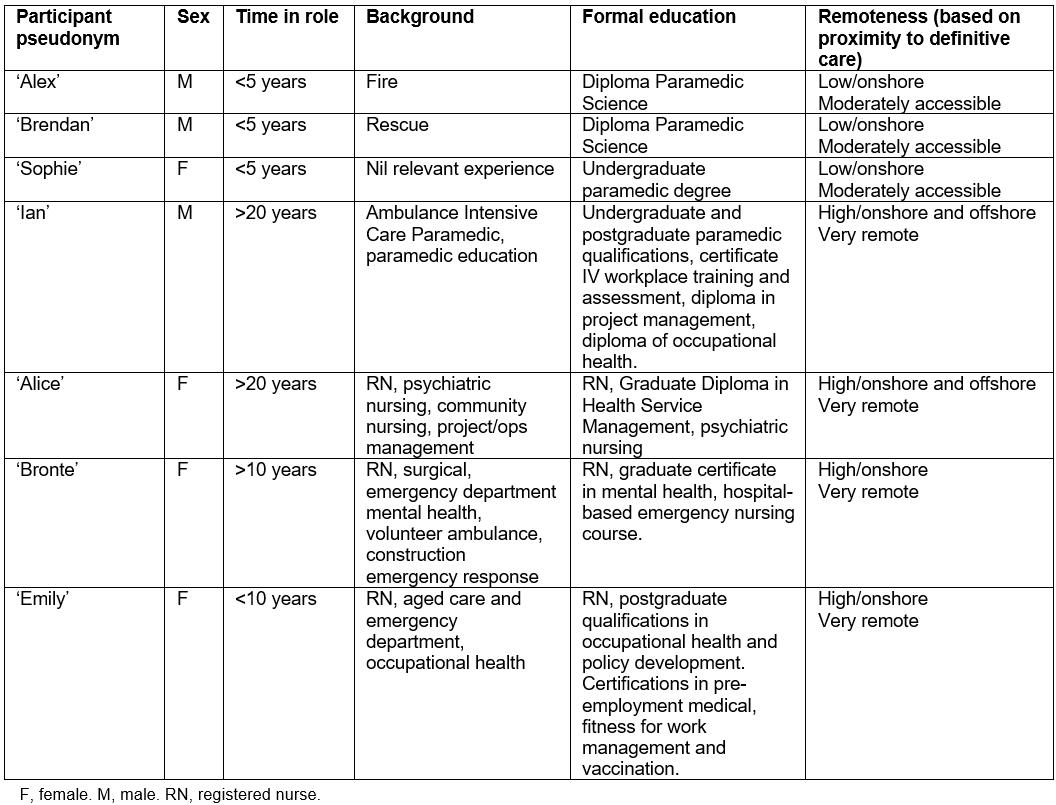
Ethics approval
Ethics approval was granted by Charles Sturt University Human Ethics Committee, approval number 406/2013/09.
Results
Although industrial health workers were exposed to the same risks from geographical and personal isolation as other remote workers, these factors had implications for their requisite scope of practice within the industrial context and will be discussed from this perspective. Emphasis is given to the effects of professional isolation consistent with the topic.
Geographical isolation
The lack of understanding of this practice environment meant that many health staff were unaware of the demands of the role and the extent of the scope of practice expected by the employer. Many were attracted by the high wages and had given little thought to the impact of remoteness on their practice. They described disillusionment with the role and a need to return to the ‘normality’ of home life. Based on their experience of remote industrial settings, participants offered some unique definitions of remoteness, noting that underground mines and ships in the middle of an ocean also constitute remote environments when needing to provide health care.
… even if you’re only two kilometres from the portal [underground mine entrance] or that portal is only fifteen minutes from the hospital, if you’re on foot and you’re in a compromised atmosphere relying on your breathing apparatus, then two kilometres away is remote. (Diploma-qualified industrial medic)
Remoteness, climatic extremes, snow, low cloud and high rainfall were all cited by participants as potential reasons that they may experience delays in being able to evacuate patients, which also extends the need for experience in prolonged care of patients.
We waited eleven hours for the flying doctors to come. So, for me, that’s the remoteness. (Postgraduate registered nurse)
Some participants had worked in mining in developing continents/countries such as Africa, Indonesia, China, Russia and Papua New Guinea. This meant that the adjustment to the environment and the influence on their practice was magnified and more complex. Due to the volatility of regional and tribal politics, many offshore industrial sites sit behind high fences with barbed wire or razor wire, with security personnel and guard dogs. Although many camps provide entertainment, gyms and a wide variety of food, there is a rigid structure, little leisure time and poor communication systems, which limit connectivity with home and little privacy.
But generally, you are restricted, you can’t go outside the fences. So, you’re locked up for four weeks. And when you get to some of the bigger sites, you’ve got to have breakfast at five-thirty, that’s your allocation. If you come at six o’clock you miss it because yours was at five-thirty ... (Postgraduate paramedic)
Personal/emotional isolation
Participants emphasised the loss of social and family interaction and attendance at significant events that can never be regained. They described feeling powerless to help when problems occurred at home and constantly thought about what would be happening at home.
... you’re around your kids you can make decisions and you can do things. But now all of a sudden, you are removed from it. But you worry about it, you worry about your children. Did they go safely to school today? You’re still trying to fix the problems while you’re a thousand miles away ... (Postgraduate paramedic)
Compromising social interaction in return for well-paid work sometimes fails to consider the wider ramifications on the whole family, not just the individual worker. One participant described the loss of personal identity as a husband and father and the disconnect that occurs during periods of time away where communication is often limited. A participant who had worked at both FIFO and non-FIFO sites had observed dramatic increases in the number of presentations to clinics at FIFO sites for minor illnesses and another noted their role in crisis counselling for family and financial issues.
… I think FIFO’s not good for relationships and I don’t think it is good for families, either. I don’t think it’s very good for your mental health. (Postgraduate registered nurse)
In many cases, health workers without specific mental health assessment education felt overwhelmed by emotionally distressed staff and inadequately prepared to adopt skills to manage them within their practice.
Professional isolation
Significantly, all participants in this study admitted to not having any idea of the full extent of the role and all felt unprepared for the ill-defined scope of practice.
When I first started, it was a little bit of a shock. I don’t think I was quite ready for it. (Diploma-qualified industrial medic)
In particular, industrial medics who have not had the advantage of working within traditional public health frameworks and, as part of an unregulated industry, held a different impression of their skill level to that congruent with traditional health practice environments. They more readily stepped outside of their scope of practice to meet organisational needs, regardless of their education and competency assessment for those tasks. Normative behaviours, attitudes and professional self-regulation are very difficult for some employees, particularly those who do not know or do not feel the need to conform to regulatory boundaries.
… they save the employers a lot of time and money by us dealing with those, instead of taking them to a doctor who is just going to give them the same treatment that we do anyway. (Diploma-qualified industrial medic)
In contrast, those with more experience in traditional health frameworks had a greater understanding of other health roles and held concerns about stepping outside of their practice boundaries.
I think that’s the best way of getting communication and then you will get the right diagnosis. [Discussing communication with onshore health professionals] I think it’s a partnership. I don’t see you out there as Robinson Crusoe, which a lot of people like to think they are. (Postgraduate paramedic)
The unique role of industrial health limits career mobility and career progression as the skills and knowledge developed as part of the role are not recognised outside of that environment. Participants described situations where they were offered ‘retraining’ to move back into traditional healthcare settings in spite of their ability to manage a wide range of health care autonomously. Some industrial health workers had even been responsible for setting up healthcare services in developing countries but there is no correlation between skills developed in this area and the needs of more traditional health practice environments.
Because professionally you reach a dead end, and where do you go after that? And if you do come back into mainstream nursing you are then limited because you haven’t followed a pathway in the health care setting to get promoted and to develop a lot, because in health care they don’t see what you did outside of health care as valid. (Postgraduate registered nurse)
I have been away for probably about seventeen years; I learned all these other things only to come back to Australia to find out that I can’t even teach first aid because I’m not qualified. (Postgraduate paramedic)
Discussion
This study highlighted two dominant and overarching concerns related to the experience of the health worker role. First, there is a persistent perception of remote industrial operations as ‘risky business’, (therefore primarily requiring emergency response) and, second, the health role is considered a ‘necessary evil’ (as a business cost). These findings necessarily frame the discussion of this study and influence each of the specific study results.
Personal/emotional isolation
High suicide risk and mental health concerns were substantiated by participants who claimed that they were responsible for mental health assessments and provision of counselling. Even in less remote locations, participants noted the need for skills for assessing presentations related to mental health concerns. Additionally, Diss noted that many staff with pre-existing mental health conditions were failing to take prescribed medication for fear of detection in routine compliance drug testing25. Bowers et al. also noted that many workers feared prejudicial employment and were reluctant to seek help on site for fear of identification26.
Accident prevention education and health promotion education have likewise been subjected to risk management approaches, with some participants noting that staff and community education initiatives were conducted without sufficient skills and understanding of the health staff tasked with delivering such programs. This has led to poor information delivery and initiatives that were not sustainable, but did ‘tick the box’ on service provision. Some participants with skills in health promotion and health education were frustrated by the inability to contribute where they perceived a need existed, due to a failure by management to value the contribution that a health role could make. Goater et al. recommended that health workers should work with industry and policymakers to create change in the health status of workers but stressed that, in keeping with WHO initiatives, every effort should be made to encourage individual workers to take responsibility for their own health and for accessing appropriate care27. The dominant risk management discourse has directed a largely reactive approach to social and chronic health issues, which could benefit from a more rigorous and comprehensive planned approach in order to improve industrial efficiency and effectiveness8-10.
Industrial staff placed in very remote locations lack access to other services; therefore, the limited services available on site are of great importance in forming a link between health behaviours and available resources at their place of residence. The higher health needs of this population of LDC workers indicate that health staff need to be equipped to manage consequences of the LDC ‘workstyle’. Additionally, the participant experience shows that the limited onsite health presence must be equipped to help workers manage physical and mental health challenges when they occur. Many organisations fear a dependency for onsite services, which would contribute to business costs. Therefore, this fear divides opinion as to the extent of the organisation’s responsibility for maintaining worker health. The provision of primary health services is contentious amongst employers and leaves employees with disparate care, poor follow-up and referral as there is no integration with offsite services or referral pathways.
The physical lack of available services in remote locations19, and the tendency for workers to adhere to reactive rather than proactive approaches to their health noted by McEwan20, illustrates the importance of consideration of the LDC population amongst other remote populations. Industrial employees should be included within such statistics as they also experience higher than average health needs and poor access to scant services, even though their permanent residential address may be within an urban environment19. Weeramanthri and Jancey called for the inclusion of LDC workers within broader health promotion frameworks that recognise place-based effects on the incidence of chronic health concerns for FIFO workers28. They also advocated for LDC workers to make conscious decisions regarding sustainable health maintenance activities. This could be facilitated by educated, proactive industrial health workers with the ability to assess, promote and link LDC workers to appropriate health promotion attitudes and services.
Although industrial organisations must remain vigilant for risks of traumatic injury, greater risk to organisational efficiency and effectiveness may now arise from communicable diseases, vector-mediated conditions and chronic mental and physical conditions. This will necessitate a shift in the way health services are provided in remote industrial contexts where staff may be responsible for care for prolonged periods of time and for primary health and chronic healthcare concerns. Although the health role is perceived as a necessary evil, participant experiences supported the need for enhanced skills and involvement at a strategic level in order to reduce business costs by averting the consequences of disease and illness through properly delivered health promotion strategies.
The current climate of increasingly remote, high-risk environments combined with low social tolerance of risk is driving changes to industrial health provision8-10,28-30. There are three key reasons for industry to now consider changes to the way health and safety is addressed within their organisations. First, increasing pressure related to low risk tolerance is driving regulatory changes to the provision of industrial health care. Safety case legislation is set to filter though industrial organisations29, which will require that organisations go beyond minimum compliance with safety legislation and demonstrate site-specific responsiveness to the impact of their operation on their workers29. The increasing discussion relevant to LDC worker health has recently taken on greater significance owing to media reports and research outcomes. Although the line is blurred between personal and industrial responsibility for one’s health, recommendations from the Western Australian Parliamentary inquiry into LDC worker suicides18 have blurred the line even further by seeking changes to legislation that mandate that remote industrial organisations must take responsibility for all onsite staff, even during offduty hours. Interestingly, this report allocated little attention to how the health worker role could engage in management of mental health concerns. Thus, more rigorous legislation will influence the industrial health worker role beyond simple adherence to broad safety legislation in favour of more rigorous risk management. This should see the beginning of a trend away from simple compliance management towards greater attention to more inclusive provision of health as well as safety systems. Likewise, this should have implications for the industrial health role with an opportunity to return to where education and research into a comprehensive industrial health role subsided in favour of simple compliance measures.
Second, increasing remoteness creates a need for health workers with greater experience and qualifications with an ability to deliver a broader range of services autonomously. Owing to the remoteness of many locations, health workers will need to be prepared to care for patients over a more prolonged period of time. This could be until an ill or injured worker can be retrieved onsite or could involve escort of the patient via helicopter, road ambulance or even commercial flights to an appropriate level of care. Risk-averse workers will be difficult to attract to very remote locations if they are not assured of adequate, accessible health care, particularly in developing countries experiencing endemic diseases and political tension. Third, increased remoteness will likely require attention to the changing nature of providing industrial medical services from one of primarily emergency response to increased primary healthcare services and health education and promotion. This study recommends situating emergency response within current fire and rescue roles, thereby allowing for a specialist/generalist health role, which would have greater capacity to meet the changing needs of their operations.
Professional isolation
A variety of terms are used to describe the industrial health worker role. Nurses, paramedics, medics, emergency services officers and emergency medical technicians are all clinical roles that may work under the title of ‘medic’. For health staff who are completely unprepared for the breadth of their scope of practice on commencement of the role, the additional professional isolation was often overwhelming, leading to poor retention rates for health staff similar to that documented by Williams31, in relation to rural and remote public health sectors. Professional identity relates to a shared understanding of discipline-specific knowledge, values and practice, which allows for tacit communication within specific disciplines. Socialisation into a workplace culture creates a sense of belonging to a specific profession32,33, which is problematic for staff working in singular, isolated roles.
The literature describes four aspects that contribute to professional isolation:
- physical distance from peers34
- separation from learning environments34,35
- decreased opportunity for professional socialisation to normalise professional culture and practice boundaries32,33,36
- lack of informal information-sharing9,21,31,37-40.
Every participant in this study referred to at least two of these domains, with at least two participants mentioning all four. This supports numerous comments from participants that indicated they did not know what professional group they belonged to, as well as the willingness of some health professionals to work outside of their assessed competencies. Yuginovich blamed the limited numbers and wide dissemination of remote nurses’ voices for the lack of development of a specialist remote nursing course34. Although this could be extrapolated to the industrial context, Mellor et al. claimed that the industry-specific occupational health nurse role had been restricted in Australia because of managerial preoccupation with safety and production costs, which restrict more holistic care concepts41. A recent US review has called for a reinvigoration of the occupational health role supported by updated curriculum and research to meet the needs of contemporary work environments42, which could provide some useful concepts for the Australian context.
The role of healthcare professionals in industrial contexts is similar to the autonomous, expanded scope of practice roles of rural and remote nurses. In the rural context, it was described as practice that occurs while isolated professionally as well as geographically21,43,44. Therefore, the complexity of these workplaces requires a very broad skill set that covers primary health care, health education, health promotion and a plethora of other tasks in addition to the assumed emergency response role, all the while lacking specific education or the support of similar healthcare professionals. Participants explained that as they are not part of public health networks, they are further separated from learning environments by exclusion from hospital-based courses that could support their role. Lack of recognition for accumulated skills45 and poor transferability of skills38 experienced by rural and remote nurses is also consistent with the experience of industrial health workers. The similarity of these contexts of practice could provide a useful nexus not only for professional association, but also for recognition and career mobility. The advent of registration for paramedics in Australia will see an extension of opportunities for paramedics to work in expanded community and primary healthcare roles46-48. This may provide opportunities for paramedics with some expansion of capacity in primary health care and health education; however, many broad scope of practice roles are typically restrained by legislative, professional, organisational and administrative boundaries36,49,50. Further research into the efficacy of emerging roles will be required to establish the value and place for these roles48,51-53 without creating duplication of services.
Limitations
This research was a small qualitative study confined to nurses and paramedics working for a single international mining organisation. Further research is needed to identify scopes of practice relevant to the remoteness of different sites. Owing to the changing nature of both the type of work and the regulatory environment, it is timely to consider which type of health professional would be most appropriate for this role given that particularly, the occupational health nurse role was not addressed in this study. Opportunities exist to examine a more rigorous program of education for this role that extends beyond first aid and compliance and would support the broad scope of practice in highly autonomous environments.
Conclusions
Although industrial health staff experience the same geographical and emotional isolation as other remote workers, they are further affected by additional professional isolation due to the singular nature of their roles and lack of inclusion within a broader health framework. Professional isolation is further compounded by a requirement to carry out a broad range of sometimes infrequently used skills in largely autonomous practice environments. Improved education for the role would help health workers alleviate stress related to professional isolation and enable them to provide improved health services to staff affected by working in an isolated environment. Industrial organisations should consider how professional isolation could be mitigated in the workplace as this will have implications for patient safety and operational efficiency. Inclusion of industrial health workers within a rural health framework would greatly assist them to identify and communicate with other staff working in remote practice contexts. This would also provide them with opportunities to access additional training to support their practice needs, allow access to professional development opportunities as well as prospects for collegial interaction. Although many aspects of their role would make them a specialist subset of remote practice, the similarities between rural health scopes of practice and the industrial environment may provide opportunities for career mobility and integration within rural health education programs.
This study recommends:
- inclusion of industrial health workers within broader health frameworks to mitigate professional isolation, assist in formation of professional identity, improve access to professional development and provide opportunities for collegial interaction
- specific education for the role to improve the overall health of workers and improve operational efficiency
- greater integration within rural health practice to provide opportunities for career mobility for industrial health workers.
Acknowledgements
The authors wish to thank study participants for their valued contributions to this project.

