full article:
Introduction
Medical education changed from the pre-Flexner period of apprenticeship model of medical training, to the Flexner era of biomedical approach to medical training, to which the approach of community-oriented medical education (COME) has recently been added1. The traditional method of training health professionals, which relied heavily on academic teaching hospitals, is being reviewed. Distributed approaches that enable the training of health professionals away from these academic teaching hospitals are becoming increasingly common2,3, with more evidence recently emerging4. This approach aims to train a team of health graduates with considerable knowledge and skills to work effectively in both rural and urban areas, as well as to provide comprehensive health care.
COME prepares health professionals to address the priority health needs of a community. The emphasis of COME is on health promotion and disease prevention, with a focus on populations. Such education could be situated in community, university or other settings and be augmented by distance learning. When located in a community setting, it is termed community-based education. A community is a small or large social unit that has something in common, such as norms, values, identity or religion. Communities often share a sense of place that is situated in a given geographical area. Community-based education is an instructional format where trainees learn professional competencies in a rural community setting, focusing on individuals as well as population groups, their everyday problems, and provide service that meets identified community needs.
Community-based education and service to address underserved populations
There is a wide diversity of how ‘rural’ is defined, and these definitions can be conflicting5. The nature of ‘rural’ varies from place to place and from context to context. It often refers to areas in a country that are less densely populated. There are different types and/or definitions of ‘rural’ areas, depending on how different the associated economic, environmental and social factors are from those in urban areas. ‘Rural’ is defined using distinct characteristics of a rural area, including isolation, limited access to healthcare resources, small population, significant distances between services and providers, and informal social structures6.
Community-based education generally takes place at a community health centre or rural hospital. A so-called community-based education and service (COBES) program describes ‘learning activities that use the community extensively as a learning environment, in which not only students but also teachers, members of the community, and representatives of other sectors are actively engaged throughout the educational experience’7. COBES not only exposes students early in their training and throughout their education to the public health and primary healthcare needs of rural communities, but also provides them with unique opportunities to learn in an environment that ‘typically resembles’ what they will encounter in later professional life. Through these activities in the community, trainees not only learn but also provide service to the community, thus addressing some human resources gaps of the community8,9. Student contributions to health delivery at facilities and in communities have become inevitable in bridging the gaps in services at the primary healthcare levels, given the gaps in human resources for health, especially in the rural areas and lower levels of service delivery in Africa10.
Career choices, recruitment and subsequent retention of healthcare professionals in rural areas are a major challenge to the health sector; this is a worldwide concern leading to human resources shortages, resulting in poor healthcare quality for rural communities. There is a skewed distribution of healthcare professionals in favour of urban-based facilities for a number of personal and professional reasons11. This maldistribution of health personnel and services has been reported not only in the developing world, but also in industrialised countries such as the USA and Norway12,13.
The search for solutions to this global problem has been central to the policies of many governments and stakeholders in health professions education. Some middle-and low-income countries have implemented several strategies to motivate health workers to accept rural postings. The Ghanaian government has offered a 20–30% salary top-up and a staff vehicle hire purchase scheme for health staff in an effort to attract and retain health workers in rural areas. However, neither of these initiatives has yielded the desired results in addressing the lack of health professionals in rural areas. There is, however, evidence that COBES can help attract healthcare professionals to rural areas and bring equity in the distribution of health professionals to benefit rural communities14,15.
The abovementioned societal changes and modifications in medical education are likely to impact the content of conceptually different undergraduate medical curricula. A WHO report has indicated the need for an estimated 14 million additional health workers adequately trained to meet the needs of communities they serve15, and there has been a call for medical education institutions to innovate in the way they train health professionals16. Curricular innovations such as problem-based learning (PBL), community-based education and multidisciplinary team-based learning are emerging in many medical schools. Structured community exposure and community-based education provide students with the requisite experiences working with underserved populations, which subsequently prepares graduates to deal with national health issues17. When health personnel are able to address the health needs of the communities they serve11, they will be regarded as being ‘fit for practice’18 and socially accountable to the community19.
Problem-based learning
The characteristics of the curriculum to which students are exposed influences the way in which they approach learning20. In a traditional, discipline-based curriculum, lectures are the main instructional format, during which students passively acquire knowledge. Students consequently adopt a surface learning style such as rote learning and memorisation, and consequently do not deliberately reflect on their learning experience. Contemporary medical training is becoming more student-centred, which emphasises active learning, and the assessment of clinical competence rather than the ability to retain and recall facts21. PBL evolved out of the ‘learning by discovery’ approach and the ‘case study method’22 as a way of acquiring knowledge about subject matter23. PBL is an instructional method characterised by the use of patients’ problems as a context for students to learn problem-solving skills and acquire and apply their knowledge of basic and clinical sciences24.
Thus PBL, which focuses on how students work and learn together in a collaborative environment, fits well into the theory of social constructivism25. Social constructivists take the view that a person’s knowledge is internalised as a result of their interactions with the social environment26. Collaborative learning assigns learners an active and constructive role in their own learning27. Consequently, collaborative learning fits in with constructivist views of learning.
Research findings on PBL consistently show that the closer the resemblance between the situations in which something is learned and the situation in which it is applied, the better the performance28. The social constructive theory also places an emphasis on the importance of the environment – the ‘context’ in learning and behaviour. According to Schmidt, there is a close relationship between COBES and PBL, in that they both provide an authentic and contextual environment for students’ learning28. COBES, just like PBL, provides an opportunity for collaborative learning among students on the one hand and the people in the community on the other hand29.
In Ghana, not all medical schools use a PBL/COBES curriculum in the training of doctors. Research on medical students’ preferences to work in rural areas after being trained with either the traditional curriculum or PBL/COBES curriculum in Ghana is limited. Will students using PBL/COBES curriculum be more willing to work in the rural area after graduation as compared to students using the traditional curriculum?
This study explored medical trainees’ preferences regarding place of work and choice of specialty in two medical schools, one of which uses the traditional method of teaching and the other the PBL/COBES methodology.
Study setting
Ghana is a developing country with a population of over 25 million people, according to the 2010 national census. In Ghana, most health care is provided by the government and this is largely administered by the Ministry of Health and Ghana Health Services. The Ministry of Health has assigned specific levels of care to health facilities depending on the category of staff managing the facility. Level M refers to maternity homes (managed by midwives), Level A comprises community-based health planning and services compounds (managed by nurses with public health backgrounds), Level B1 includes health centres without a doctor and Level B2 is health centres with a doctor, Level C is district hospitals and Level D comprises regional and tertiary hospitals. These facilities are funded by the government of Ghana, internally generated funds and donor-pooled health funds30. Hospitals and clinics run by the Christian Health Association of Ghana also provide healthcare services. Some for-profit clinics exist, but they provide less than 2% of healthcare services.
Heath care is very variable through Ghana. Urban centres are well served and contain most hospitals, clinics and pharmacies in the country. Rural areas often have no modern healthcare facilities. Patients in these areas rely on traditional African medicine or travel great distances to assess health care31.
Medical school training
The four medical schools in Ghana graduate over 300 doctors annually. The medical education system in Ghana aims at training holistic doctors who, after internship, will be capable of serving a community anywhere in the world. Usually, doctors are posted to all parts of the country and most do accept such postings. In order to keep doctors in the country and prevent them from seeking opportunities outside the borders of Ghana, the Ghana Postgraduate Medical College was established to draw up curricula for the various disciplines in medicine. In 2002, this became the Ghana College of Physicians and Surgeons, which is the main college for postgraduate training of specialist doctors.
Ghana’s medical education is mainly concentrated in the cities. The universities and medical program are located mostly in the larger urban centres, notably Accra and Kumasi, where most of the physicians stay. The University of Cape Coast, School of Medical Sciences (UCC-SMS) and the University for Development Studies, School of Medicine and Health Sciences (UDS-SMHS), located in Tamale in the north, and recently the School of Medicine at the University of Health and Allied Sciences (SOM-UHAS), located in Ho in the Volta region have been established. However, as with most developing countries, Ghana has great difficulty extending modern medical care to smaller towns and rural areas.
UDS-SMHS and UCC-SMS adopted a PBL/COBES curriculum, whilst University of Ghana School of Medicine and Dentistry (UG-SMD) in Accra and Kwame Nkrumah University of Science and Technology School of Medical Sciences in Kumasi use the traditional method32. In Ghana, undergraduate medical training consists of 3 years basic sciences and 3 years clinical training.
COBES program
The COBES component of the PBL/COBES curriculum enables students to learn and also provide service to the rural community. The students spend 4 weeks on a yearly basis with predefined objectives in the community. In the first year, students learn to identify and explore the demographic, social, environmental and economic factors that affect the community’s health. In the second year, they conduct a study into the health needs of the community and this results in them making a community health diagnosis. In the third year, they undertake to resolve these needs by identifying resources available in the community. In addition, the students rotate through the various departments of the health facility, for example the dispensary, consulting rooms, maternal and child health clinic and the laboratory, as well as participate in scheduled immunisations visits by the health workers. Through this process they are exposed to ‘early patient contact’ and build their clinical skills. From fifth year, students are sent to the district hospitals for COBES, which has a different focus, mainly on clinical work. However, from this time, students in all medical schools, irrespective of the type of curriculum, are sent to the district hospitals for district postings, where they carry out public health activities and do clinical work.
The COBES program is iterative – each year builds upon the previous year’s experience, thereby updating, improving and expanding the activities of the previous year33.
Method
Participants and questionnaire
This study had a cross-sectional descriptive design, using a paper-questionnaire consisting of 25 items of both open- and close-ended questions, administered onsite to all students after their respective lecture sections. Students from UG-SMD and UDS-SMHS participated in the study.
A literature review-based questionnaire was developed to reveal the perception and willingness of students to work in a rural area and also their future choice of specialty34-36. The items of the questionnaire were construct-validated by FA, AS and WvM, all medical education experts. The questionnaires were administered on site by the first author to the two participating medical schools in Ghanaian to first-, third- and sixth-year students, either before or after lectures. Those who were present during these lectures were potential participants in the study. The study years were chosen to unravel the effect of the type of curriculum on students’ preferences of place of work and choice of specialty as they enter and progress through their medical school training. Participation in the study was voluntary, and confidentiality and anonymity was ensured. All participants gave verbal consent.
Data analysis
Results are presented as frequencies and proportions of the total sample recruited. Associations between gender, type of curriculum, choice of specialty and practice location were assessed using the χ2 test. Logistic regression analysis was performed to determine the association between medical school and curriculum type and students’ preparation for rural practice while controlling all other factors. Statistical significance was assumed at p<0.05. Data analysis was performed using the Statistical Package for the Social Sciences v18 (IBM; http://www.spss.com). Qualitative data analysis of answers to opened-ended questions was performed using Atlas TI v6.0.15 (Scientific Software Development; http://ww.atlasti.com), applying the principles of primary, secondary and tertiary coding37. AA and WvM read the responses independently, identifying common themes, trends and shared opinions among participants using thematic analysis. The independent codes generated by AA and WvM were cross-checked by the second and third authors (FAA and AS). In the process, researchers discussed all discrepancies until they reached consensus.
Ethics approval
The authors obtained ethics approval from the Tamale Teaching Hospital Ethics Review Committee (TTHERC ID No. TTHERC/17/11/16/03).
Results
The numerical results of the questionnaire of the qualitative analysis of the open-ended questions are consecutively described.
Quantitative results
Unanswered questions were considered as missing values and not included in the analysis. At UDS-SMHS, 281 students (100%) returned the questionnaire, whilst at UG-SMD 244 out of 275 students (88.7%) returned the questionnaire. Of the students from UDS-SMHS 63.7% were male, and from UG-SMD 52% (Table 1). The majority of students from UG-SMD who lived in the city prior to entering medical school indicated that having part of the medical training in rural areas would be useful. This was statistically significant (p>0.01) (Table 2). Students from UG-SMD were significantly less likely to indicate that their medical school curriculum prepared them for rural practice as compared to students from UDS-SMHS (odds ratio (OR)=0.19, 95% confidence interval (CI)= 0.13–0.28, p=0.001).
The willingness of third-year students at UDS-SMHS to choose to practise in rural areas after graduation decreased as compared to their colleagues in first and sixth years; however, the willingness remained almost the same for similar cohorts of students in first and third year at UG-SMD. In the sixth year, an increase in the willingness to choose to practise in rural areas was observed in both schools (Table 3).
The perception of students that the training curriculum prepared them for rural practice increased gradually comparing first- and sixth-year students, and was more prominent for UDS-SMHS students than students from UG-SMD (Table 4).
Students from both schools indicated that it would be useful having part of their training in the rural areas, especially UDS-SMHS students in first year (89.4%) and sixth years (85.0%). For students from UG-SMD, the usefulness in having part of their training in rural areas increased as they progressed with their training (Table 5).
Male students were 1.5 times more likely to indicate that they were willing to work in rural areas after graduation compared to their female counterparts (OR=1.6, 95%CI=1.23–2.29, p=0.009). Students who had lived in rural areas prior to entering medical school were almost four times more likely to choose to work in a rural area after graduation than those from the city (OR=3.91, 95%CI=1.75–8.75, p=0.001).
Table 1: Sociodemographic characteristics of respondents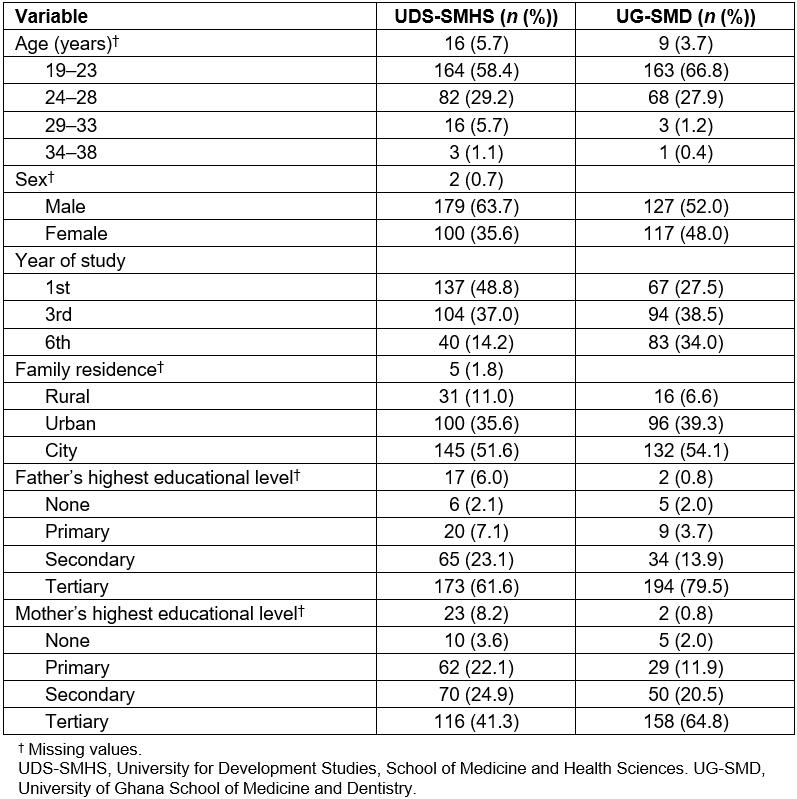
Table 2: Comparative analysis between UDS-SMHS and UG-SMD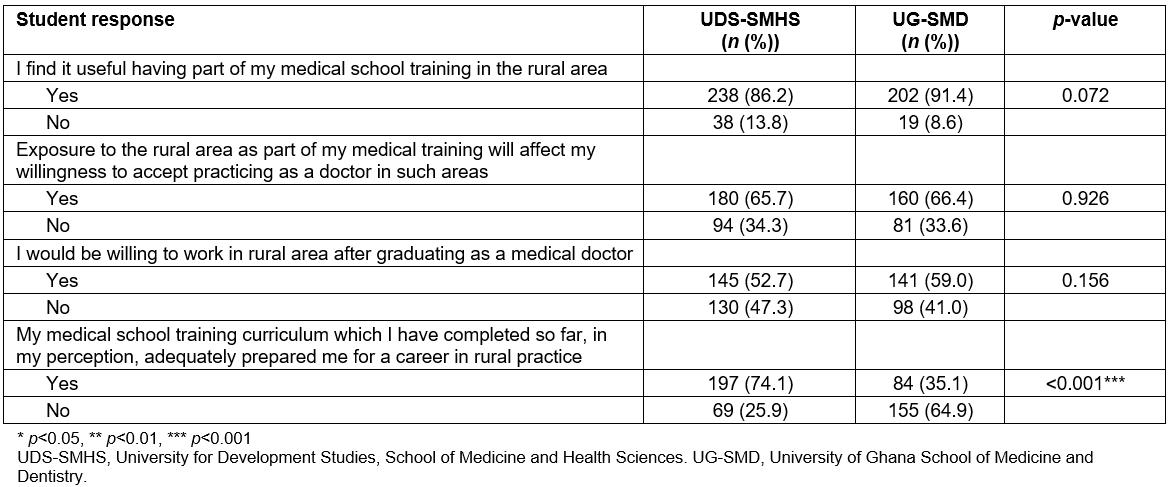
Table 3: Student responses to ‘I would be willing to work in the rural area after graduation’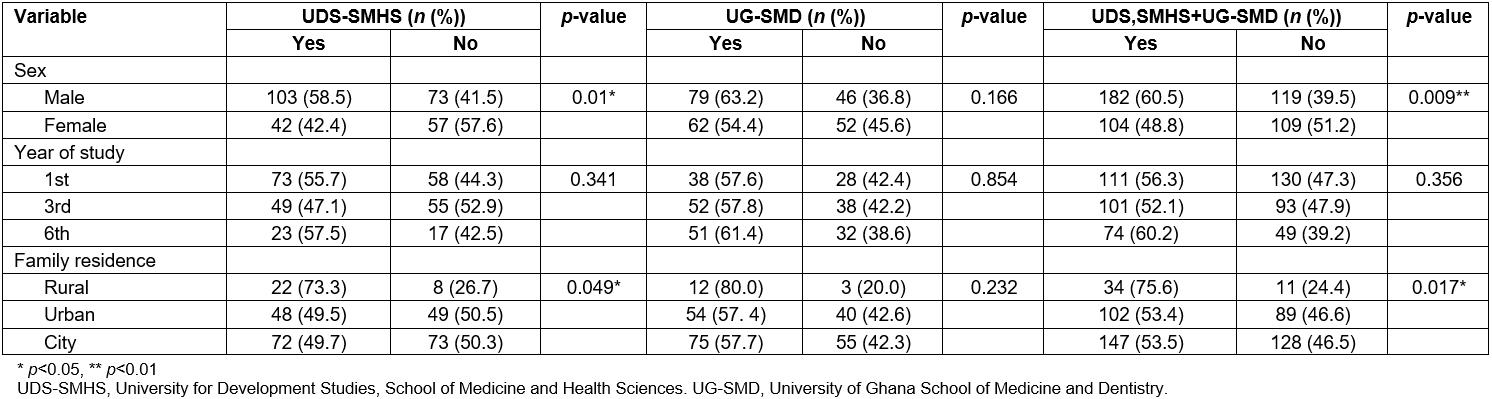
Table 4: Student responses to ‘My medical school training curriculum, which I completed so far, in my perception adequately prepared me for a career in rural practice’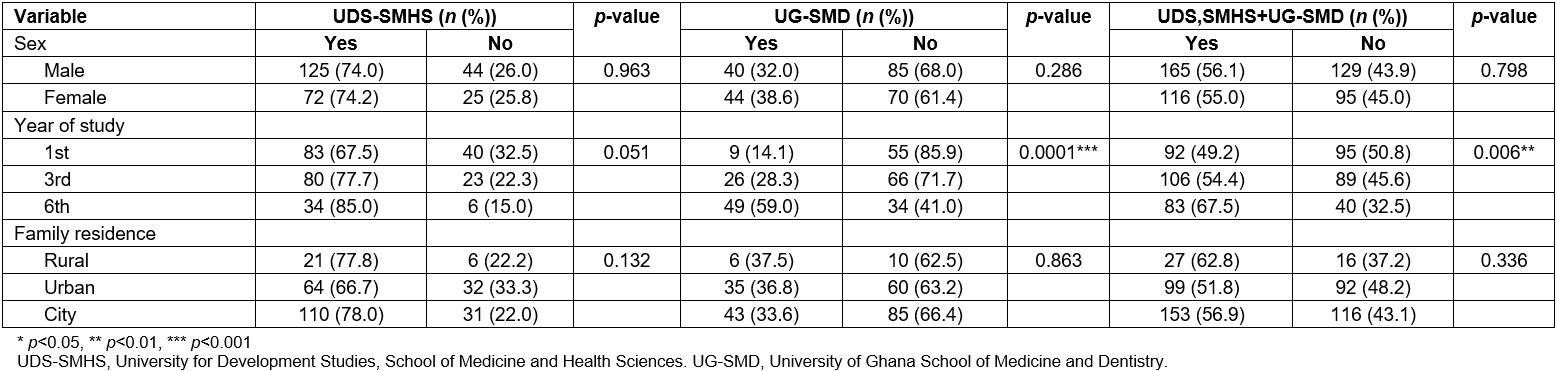
Table 5: Student responses to ‘Having part of my medical school training in the rural area is useful’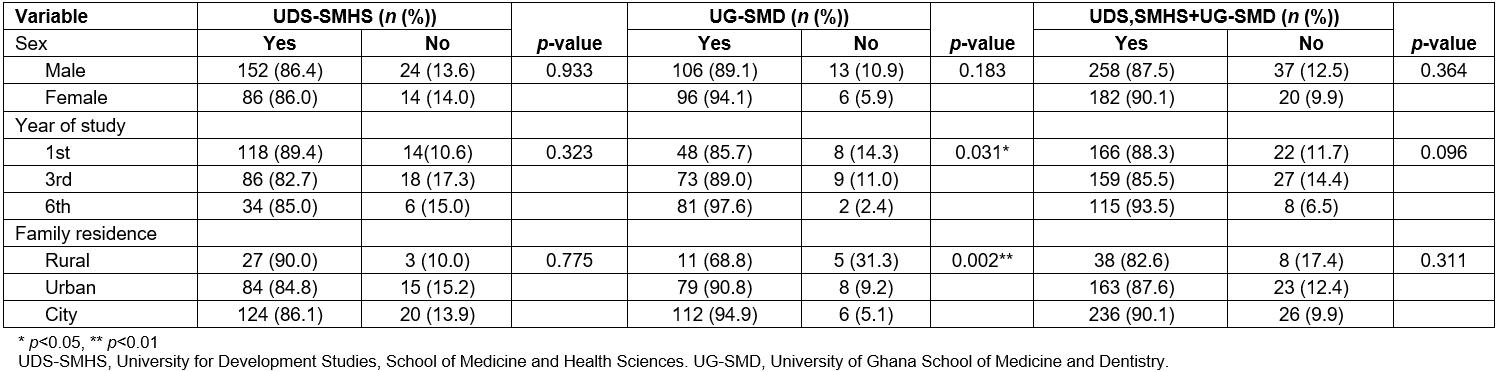
Qualitative results
The main themes that emerged from the qualitative analysis are presented here.
Usefulness of rural medical training in the curriculum: Students from both institutions indicated the usefulness of having part of their training in rural areas. They believed it prepared them for future practice, gave them the opportunity to understand the determinants of health in rural areas and broadened their knowledge base and clinical skills. They also perceived that it helped them develop empathy towards people living in rural areas.
It exposes us to the rural settings so as to have a fair idea of what is going on there with regards to the health of the people. This will help us if we are posted there to work. (Male, UDS-SMHS)
It has the tendency of engaging me to see more critical medical situations/conditions in the presence of less available facilities which, in a long run, will build my experience. (Male, UG-SMD)
Students from both UDS-SMHS and UG-SMD indicated that lack of adequate resources, facilities for training and tools to work with, in rural areas, makes the rural outreach program not very useful to them. UDS-SMHS students indicated that they were demotivated by the inability to use data gathered during the COBES rotation for the benefit of a rural community.
Willingness to work in rural areas after graduation: The opportunity to improve on their knowledge base and clinical skills gave students the confidence to offer quality healthcare services, thus making them professionally independent in their future practice as doctors. The lack of human resources in the rural areas compared to urban areas makes them want to fill the void of non-availability of doctors in such areas.
Access to doctors in these rural areas is very poor. I would like to help bridge that gap. Also, I believe I would be more fulfilled bringing smiles to their faces. (Male, UDS-SMHS)
Physically, being a health professional is all about reaching out and helping people and how better to do this than providing my services at places where they are much sought after but which they do not have. (Male, UG-SMD)
Lack of social amenities such as accommodation, good road and transportation networks, good educational facilities and well-equipped health facilities will deter students from accepting work in rural areas after graduation. Students from UG-SMD specifically mentioned that the lack of rural experience during their medical school days would deter them from striving to go and work in a rural community. Issues such as language barriers and unwillingness to stay far away from their families were mentioned as factors that would likewise prevent them from accepting rural postings.
Because I have never lived there, adapting to that kind of life will be challenging; besides getting equally good schools, as prevails in the urban areas, for my children will also be a problem. (Female, UG-SMD)
Effect of exposure to rural areas as part of training on choice of specialty: Participants indicated that lack of access to quality health care as a result of inadequate human resources and myriad community health problems would make them specialise in areas that will help address the needs of rural communities.
This is because my encounter with patients in these areas will make me know the common diseases that affect them. This will increase my desire to specialise in an area that I can be of much help to the rural folks. (Male, UDS-SMHS)
Suggestions to improve the curriculum in the direction of rural training: Students from UDS-SMHS focused more on strategies that could improve the already existing COBES program. These strategies included proper student orientation towards COBES, scheduling and executing regular monitoring and supervisory visits, selection of well-resourced and well-equipped health centres in rural areas, orientation of health facilities staff on the objectives of COBES and making COBES compulsory in all medical schools in the country.
However, students from UG-SMD centred their suggestions on the introduction of community-based education activities such as rural outreach programs into their curriculum. They advocated a curriculum that addresses the needs of the rural community, and promoted the idea of universities establishing medical schools in the rural areas. They also wanted the policy of recruiting specialists for rural communities to be looked at critically.
We need more experiential training. Training should influence students’ attitudes towards rural postings, engage students more in the community. Make COBES compulsory in all medical schools. The objectives of COBES to be discussed with the community. Ensure adequate monitoring and supervision. (Male, UDS-SMHS)
Take us on excursions to such places. Expose us to such training i.e. rural medical practice. Teach us the way of life and our culture to make us aware of the different people in our societies. (Female, UG-SMD)
Suggestions to refocus medical education towards rural practice in Ghana: Students of UG-SMD suggested that, to promote rural practice, medical education in Ghana should refocus on an innovative teaching methodology that incorporates rural outreach programs as part of the curriculum in general. Specifically, they advocated a policy of admissions of students from rural areas to medical schools and improvement of infrastructure of health facilities in the rural communities. UDS-SMHS students indicated that the PBL curriculum should focus on giving students more clinical skills training before the students go for COBES placement. They advocated that clinical staff should develop more interest in COBES and also participate fully in its activities.
Prepare us clinically before we go to the communities. PBL should focus on clinical skills. Skills should be tailored towards addressing rural challenges. Clinical staff should participate in COBES activities. Medical doctors should be posted to the facilities during the period the students stay in the communities. (Female, UDS-SMHS)
The medical training should be more geared towards resolving the ailments in our own localities, make us interact more with the rural folks and case studies should focus more on the rural areas. (Male, UG-SMD)
Discussion
This study assessed preferences regarding place of work after training as doctors in either a traditional or a PBL/COBES curriculum. The study is unique in that it compared results from two established medical schools in Ghana. This study revealed that the type of curriculum used by medical schools in Ghana may have an effect on the preparedness of students to choose to practise in rural Ghana after graduation. The majority of the students from UDS-SMHS indicated that their PBL/COBES curriculum adequately prepared them for rural practice. The UG-SMD students indicated that lack of rural experience during their medical school training deterred them from wanting to work in rural communities after graduation. The study was unable to determine the net influence of the choice of teaching and learning methodology (ie PBL and traditional) on students’ acceptance to work in rural areas. It is possible that students who use the traditional curriculum in their training and also implement COBES may produce similar results to students using the PBL/COBES curriculum. This is an important area for further research.
The usefulness of COBES as an integral part of the medical curriculum has been reported in studies from Ghana, South Africa, Australia and the USA38-41. Some studies have shown that medical schools that have a rural-oriented and innovative16 curriculum and offer a repeated rural experience and decentralise training at district hospitals and community health facilities16 to their students are more successful at graduating physicians who choose rural practice as a career42. A study on the influence of community-based education on undergraduate health professions students’ decision to work in underserved areas in Uganda showed that the proportion of students who expressed the desire to practise in rural communities increased after the students had undergone COBES placement36. There is thus some evidence that COBES can be used to prepare and acclimatise healthcare professionals to work in rural areas and bring equity in the distribution of health professionals to benefit rural communities14,43.
Another important finding of this study was that the willingness of students to choose to practise in the rural area as they progress through their training was lower in year three as compared to years one and six. This was unexpected – the authors anticipated a gradual increase in the willingness to choose to practise in rural areas.
For students in year one, the excitement of rural exposure and the experience of ‘early patient contact’ might have influenced their desire to want to practise in a rural area after graduating. For year three students, although they have been exposed to the community for three consecutive years, the challenges experienced during COBES might have outweighed the clinical experience gained. The sixth-year students spent an additional 6 weeks in year five, where they were posted to the district hospitals for mainly clinical work, although they carry out public health activities as well. Therefore, it is not surprising that the willingness to choose to practise in the rural areas in sixth-year students increased. The experience gained and the inadequate staffing in these hospitals, and the local societal consequences, may have influenced their decision. The same holds true for the sixth-year students from UG-SMD.
The citing of lack of accommodation and other social amenities by students in this study as reasons for not wanting to accept work in rural areas is not new. The international literature is quite unambiguous about this fact and states that the absence of adequate living conditions in the rural areas, particularly in the low-and middle-income countries, adversely affect retention of health workers in these areas44,45. However, there is evidence that when students are exposed to COBES, the rural exposure has the potential to increase the number of graduating students likely to want to work in such areas by changing their attitude towards the relative importance of social amenities as an influencing factor for their decision to choose rural placement38.
Students from UDS-SMHS, having experienced the benefits of COBES, nevertheless advocated that students should be properly oriented before they are sent to the communities. They were of the view that regular monitoring and supervisory visits by faculty, selection of moderately well-equipped health facilities and orientation of the staff of health facility to be visited on the objectives of the COBES program will go a long way to enhancing the students’ experience as well as desire and willingness to accept future rural postings. UDS-SMHS students suggested that COBES and reforms incorporating rural outreach programs should be made compulsory in all the medical schools in Ghana. This suggestion is in line with those of previous reports that indicate that sending medical students to non-tertiary care settings for clinical rotations and decentralising clinical training16,46 as part of the undergraduate curriculum is the way forward in not only decongesting educational facilities at teaching hospitals but also bringing equity in the distribution of health professionals to rural areas .
Another key finding in this study is the relationship of students’ rural background (those who were born and grew up in rural areas) and their future career choice. This study revealed that students who had lived in a rural area prior to entering medical school were four times more likely to accept work in the rural area after graduation than those from the city. This is consistent with all other studies in the international literature47-49. It would be prudent for Ghana to consider students with rural backgrounds during the selection and admission process into the medical schools.
In Ghana, strict policy for admission into universities mainly considers the best aggregate score on six subjects (three core and three elective). The problem is compounded by the huge numbers of applicants vying for the few places to study medicine, making entry into medical school very competitive. Most students who gain admission to medical schools are typically from the cities, where the pre-university schools have the best educational facilities and better and well-trained teachers compared to those from the rural areas. It is thus not surprising that the majority of the students in this study are from the cities. Most of these students have not lived in a rural area before, and taking a rural career after graduation is very unlikely. However, when such students are exposed to the rural communities to undertake some of their educational activities, they are more likely to develop a positive attitude towards rural communities38. Therefore, a rural practice experience introduced early during medical school training can positively influence students’ attitude towards rural practice.
Another key finding was that COBES had more influence on males than females. Male students were 1.5 times more likely to indicate that they were willing to work in a rural area after graduation as compared to their female counterparts. This has been reported in similar studies conducted in other countries38,47,50. Some potential explanations may be that they have stronger ties with, as well as more responsibilities towards, their families and therefore are unable to travel far away, they are unwilling to work alone in rural areas except if accompanied by their husbands, their inability to keep two separate homes, and the unavailability of good schools in rural areas for their children.
As shown in this study, participants cited inadequate human resources and awareness of community health needs experienced during COBES as reasons that influenced them to make decisions to specialise in different fields of medicine relevant to rural practice. Both the lack of human resources and the health needs of the community have been consistently cited in literature as some of the factors that influenced students not only to make decisions as to which areas of medicine to specialise in but also invoked their willingness to work in rural areas33,51.
Study limitations
This study aimed to involve four Ghanaian medical schools; however, permission could only be obtained from two. Nevertheless, the findings provide useful insight into the opinions of students towards rural placements from the perspective of traditional and PBL/COBES curricula. The authors were unable to determine the net influence of the choice of teaching and learning methodology (ie PBL and traditional) on students’ acceptance to work in the rural areas. Furthermore, the study was carried out by staff of UDS-SMHS, with a positive attitude towards COBES.
Conclusion
Students using the PBL/COBES curriculum stated that the program was very useful and could influence their choice of future practice location. They underscored the fact that their PBL/COBES curriculum adequately prepared them for future rural practice. Nevertheless, they called for improvement in the COBES program to even more positively influence students’ attitude towards rural practice. Students using the traditional curriculum called for the introduction of innovative teaching methodologies that will incorporate rural outreach programs as part of the medical curriculum. This, they believed, will help them cultivate an interest for rural practice and also increase their willingness to choose rural practice after graduation from medical school.
Acknowledgements
The authors wish to express their sincere gratitude to the first-, third- and sixth-year students of the University of Ghana Medical School and Dentistry and University for Development Studies School of Medicine and Health Sciences for their support in answering the questionnaire. Our gratitude goes to the Dean of the Medical School at Korle-bu for granting permission to conduct this study. We also wish to thank Dr.- Anthony Wemakor and Mr.- Evans Paul Kwame Ameade for their support in the statistical analysis of this study. The authors want to thank Alina Smirnova for performing a language revision of the manuscript.
references:
You might also be interested in:
2012 - Extending the paramedic role in rural Australia: a story of flexibility and innovation
