Introduction
Ireland has one of the fastest ageing populations in Europe, with those aged more than 65 years projected to reach almost a quarter of the total population by 2041. This will increase demands on healthcare services1, particularly in terms of caring for an increasing number of people living with chronic diseases. Currently in Ireland, 38% of people aged more than 50 years have at least one chronic disease, with instances rising with age. Chronic illness accounts for 40% of hospital admissions and 75% of hospital bed days as well as 80% of all GP visits2. A significant feature of the shifting demographics in Ireland concerns the proportion of older people living alone (27% overall and 43% in rural areas)3. This presents additional challenges for meeting service needs. Among persons aged 75 years or more, 35.3% live alone while almost 45% of persons aged 85 years or more also live alone4.
The general practitioner (GP) out-of-hours (GPOOH) service is a fundamental part of primary health care, providing continuity of care for people with urgent medical needs who cannot wait until the next working day to see their doctor. People aged 65 years or more attend the GP on average seven times each year, with the number of consultations increasing with age5. Evidence shows that older people are significant users of GP services, but little is known about their use of GPOOH care. As the number of older people increases, so does use of hospital emergency services by this cohort6. Existing service use patterns suggest the traditional model of hospital-dominated care will become unsustainable. The greater the extent to which the GPOOH service can be accessed, the greater the proportion of older people’s care needs that can be met in the community, with less reliance on hospital-based emergency services7.
Government policy aims to support older people to live at home for as long as possible, and out-of-hours primary care is central to this objective. Being ill at night can, however, be accompanied with more anxiety than experiencing similar symptoms during the day. GPOOH services have, therefore, an essential role in supporting older people to live independently in their own homes, but this is only the case if people are able and willing to use them. When older people present themselves at GPOOH services, they are most likely to do so with problems they accurately self-assess as urgent8. Nonetheless, older people are reluctant to ask for help, even when such help is clearly needed, often believing that if they were well enough to travel they could manage without bothering a doctor until morning9,10.
Private choices are also shaped by environments11. One challenging aspect of rural and remote environments concerns access to transport, a problem found to impact 37% of rural households with residents aged more than 65 years in Ireland12-15. Family, friends and neighbours provide over 80% of general transport needs for older residents in rural Ireland14,15, and the majority of older adults (90%) report they could call on a neighbour or family member if in need16. Looking more closely, however, it is not clear if such reports include either the confidence of a response, or the willingness to make such a request for help were it needed for a health crisis at night, rather than during daytime hours.
How these or other factors impact the willingness or capability of rural-dwelling older people to access GPOOH care has not been examined until now. There is no literature examining the use of GPOOH services in Ireland by older people. Meanwhile, the limited literature from elsewhere relates primarily to general patient populations without addressing issues arising for older people in particular. Likewise, an early study of the impact of rurality on patient satisfaction with GPOOH services in Ireland17 did not specifically explore the views or experiences of older service users. Furthermore, studies of healthcare access challenges for older people often omit examination of GPOOH services. This study sought to fill this gap by exploring the challenges facing older people in accessing and using GPOOH services.
Methods
Definitions used in the study
GPOOH services: GP cooperatives are independent, private, cooperative organisations, state-funded under contract to provide urgent, non-emergency care on a shared rota-basis during the hours GP surgeries are closed. Referred to as Doc-on-Call (DOC), the GP cooperative approach has been the established model of out-of-hours care provision in Ireland since 2000. It operates with a single contact number for the region, and GP membership is drawn from the local geographical area. Service users are expected to visit the out-of-hours treatment clinic, instead of the GP conducting home visits.
Rurality: The Irish Central Statistics Office considers all areas outside clusters of 1500 or more inhabitants as rural18. ‘Rural’ and ‘remote’ are concepts often linked and sometimes used interchangeably. While the term ‘rural’ usually denotes a context of living, the term ‘remote’ is generally more concerned with issues of inaccessibility19 resulting from deficits in physical infrastructure and social provision. This includes greater distances from service centres, often leading to experiences of inequality and social exclusion13. This study was concerned with the lived experience of rurality for participants, in relation to accessibility of DOC. Given that the single out-of-hours treatment centre for each county region is located in a large town, participants were asked if they lived within 15–30 minutes driving distance from the closest treatment centre. Remoteness was considered where participants lived more than a 30-minute drive from their closest DOC treatment centre.
Sample and setting
Due to the difficulty accessing older participants for research studies, convenience sampling is often used in studies related to older age20. For older research participants, ethical issues around trust and conducting research in a safe and familiar environment can also arise21. These considerations were addressed by locating field work in community day centre settings already regularly attended by older people. Inclusion criteria required that participants could provide informed written consent and could personally participate in the focus group. Nursing home residents or individuals being cared for by another person, who would be responsible for accessing and facilitating use of DOC on their behalf, were not included in this study as the focus was on self-directed access and use of the service. Study participants included those from outside the GP cooperative region, in more remote areas, whereas out-of-hours GP care is shared between individual GP practices in the area.
Design
This research was conducted in the mainly rural counties of Cavan and Monaghan (total population 137 462)3 in the north-east of Ireland, where up to 65% of the population live in rural areas16. The population aged more than 65 years is 14% in both counties, broadly in line with the national average16,22. A mixed methods approach was used in this study, including a series of focus groups (n=9) with people aged more than 65 years and questionnaires completed by all focus group participants (n=48).
Locations were identified to ensure a geographical spread in relation to the single DOC centre located in each county. All day centres were identified and distances calculated, using Google Maps. Locations were identified and selected on the basis of being closest, furthest and in the middle distance from treatment centres. A combination of direct contacts and referrals facilitated setting up the focus group visits at each site.
Focus group discussions were semi-structured with a core set of topics addressed in each group, including:
- ‘What do you do when sick?’
- ‘What is Doctor on Call for?’
- ‘How sick would you need to be to call the doctor?’
- ‘What do you need when you are sick?’
- experience with DOC
- information needed about DOC
- transport.
Topics were based on those initially identified through a review of the literature, informal discussions with service providers and a consultation process with older people in the region, which preceded this research.
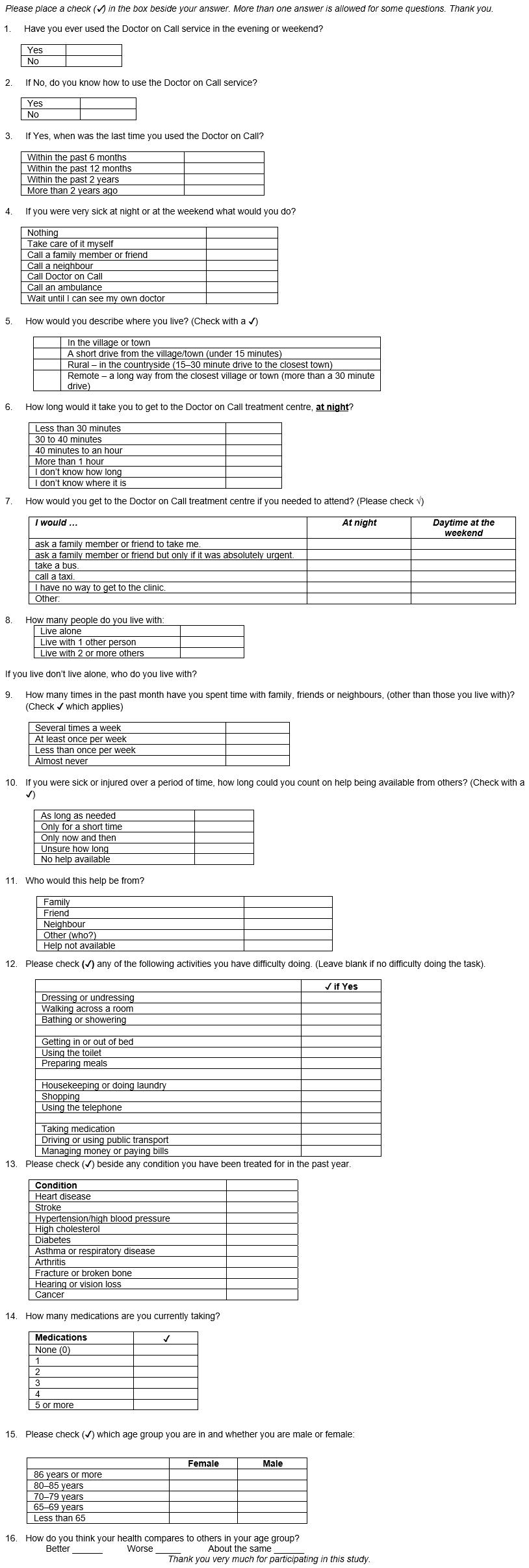
A questionnaire was designed to identify levels of DOC use and knowledge, as well as individual characteristics of participants that might influence attitudes and access to DOC (Appendix I). Participants completed the written questionnaire either before or after participating in the focus group. The questionnaire, in closed-question format, asked about DOC usage, illness response, geographical location, distance from the treatment centre, transportation, availability of a supportive social network, demography, morbidity, mobility, medications, residential conditions and evaluation of personal health.
Older respondents can experience practical challenges to questionnaire completion, as a result of physical or sociocultural conditions impacting their ability to read or write responses. To improve data reliability, older respondents should be supported in completing questionnaires23,24. Some participants chose to self-administer the questionnaire while others preferred to have the researcher ask the questions and fill out the questionnaire sheet for them. This strategy sought to emphasise the purpose rather than the process of the questionnaire method to gather relevant and accurate data.
Some interview questions or discussions may have potential to cause distress to older participants24,25. Interview and focus group questions were, therefore, adapted in recognition of vulnerabilities identified during focus group engagement. For example, repeat questioning about what one would do if ill at night was avoided, where it was considered likely that to persist with such questions might cause worry for participants afterwards. Details for support resources were provided to participants in case they later became distressed by anything that had arisen during the focus group discussions.
Data analysis
Focus groups were conducted until saturation was reached, with no new themes emerging from discussions. Group discussions were audio-recorded and transcribed verbatim. A thematic analysis was conducted on the transcripts, using NVivo v10 software (QSR International; http://www.qsrinternational.com/nvivo). Coding was conducted from both written transcription and the audio-recordings, to ensure consideration of tone, context and emotion in the application of codes to content. Following general theme coding, each transcript was coded further using a line-by-line approach. Codes were then clustered into themes and duplicate themes merged. Two researchers independently cross-coded a sample of transcripts and the final list of themes was formed by consensus. Questionnaire data were collated in an Excel spreadsheet and analysed using NVivo software.
Ethics approval
Ethics approval for this research was granted by the Ethics Review Board at Dundalk Institute of Technology and by the Healthcare Research Advisory Committee of the Health Service Executive under the Irish Department of Health.
Results
Study population
As a purposive sample, identified through day centres, it is not surprising that those who participated were generally active older people. Almost all reported at least once-weekly social activity, while 33 participants (69%) reported they socialised with others several times weekly. Participants were eager to engage in the study and to contribute to the discussion around DOC as an essential service in their communities. This was reflected in a 100% questionnaire completion rate from participants (n=48), with only two questionnaires submitted partially completed.
Participants comprised mainly older women (n=32, 67%). A high proportion of the participants were aged more than 80 years (n=21, 44%) and more than half of all participants (n=28, 58%) were living alone. Counties Monaghan and Cavan are largely rural. It is, therefore, unsurprising that 50% of the participants (n=24) reported living more than a 30-minute drive away from their nearest DOC centre. Most of these remote-dwelling older people (n=15, 63%) also reported living alone.
Health challenges associated with older age include co-morbidity, activities of daily living and polypharmacy. Multimorbidity, with health conditions such as hypertension, heart disease, arthritis, hearing or vision loss and high cholesterol, was present in 25 participants (52%). Furthermore, 27 people (56%) reported taking three or more medications daily. Participants were, therefore, well placed to consider what symptoms might prompt a need for a doctor out-of-hours and what health-related concerns might arise when contemplating accessing and using DOC.
Sixteen participants (33%) identified challenges with at least one activity of daily living, including 14 (29%) who identified inability to drive or use public transport. As expected, these complex health challenges were represented to a greater degree among the older participants. Nonetheless, despite multiple health issues, co-morbidity, polypharmacy and activities of daily living challenges, most participants (n=43, 90%) rated their health as better or about the same as others the same age.
Almost half of participants (n=21, 44%) had previously used DOC but of those living more than a 30-minute drive from the closest treatment centre (n=35, 73%), only seven (29%) had previously used the service. Despite the numbers who had previously used the service (n=21, 44%), only 13 focus group participants (27%) stated they would call DOC. Furthermore, of those stating they would call DOC, all except one person lived within a 40-minute drive of the closest treatment centre.
Speed of access
Difficulty negotiating multiple telephone calls, computerised processes, and worries about being taken seriously, were concerns identified by participants; however, the underlying challenge was being able to access a consultation with a GP as quickly as possible. Having to answer the same questions each time they spoke to another person in the system was experienced by participants as slowing down access to care:
… why do they have to ask all these questions, why can’t they just come on out?’ (participant 2, county Cavan, focus group 4 (2C4))
There was worry about the time it took to see a doctor; ‘I think less time on the phone could save somebody’s life‘ (2C6)
Participants who lived furthest from the treatment centre expressed the most emphatic frustration, about time to access a doctor:
… if you’re seriously ill … there’s no point going to Doc-On-Call. You are better off going straight to Cavan [the single hospital A&E serving both counties]. (participant 3, county Monaghan, focus group 4 (3M4)).
It was considered more efficient to go directly to the hospital, since it would save time if likely to be referred there by DOC anyhow:
Other people, now, what they do if they feel unwell, is get into the car and … get them direct to Cavan. (3M3)
Some participants expected they should receive a home visit by the GP, reflecting a view that if sick enough to need the doctor outside surgery hours, they would be too ill to travel to the treatment centre for care:
I certainly wouldn’t expect [doctor] to come out if I could go in at all, unless I felt I was going to exacerbate the condition I had by going in. (3C1)
This is supported by previous research9,10 and was emphatically expressed by one woman:
They should come out! When you call them they should come out! … If it says ‘Doctor-on-call’ it should mean on-call. (4M7)
Notwithstanding the belief that a home visit may be appropriate, participants living most remotely from the centre noted that having someone transport them to the treatment centre or hospital was preferable to waiting for a home visit:
… if you had an emergency crop up … you would just be worried about the length of time really … [for the doctor to get to you]’ (4C6)
Don’t call anyone. Just go straight to the hospital … by the time you’d be there, you see, because it would be the best part of 30 mile to come to any of us … it’s out in the country. (6C3)
… it depends on where you live but it would be quicker than an ambulance which has to do the double trip. (1C4)
Transportation and social network
The issue of distance from the treatment centre raised the question of who would provide transport to DOC. Some participants (n=7, 15%) reported that instead of calling DOC they would call directly for an ambulance or press their panic alarm button, either because they had nobody they could call to transport them to DOC or because it would save time. Most participants (n=43, 90%) identified family members, friends or neighbours as their most likely source of transportation. Nonetheless, anxiety about being ‘a bother’ (4M4) or ‘a nuisance’ (4M2) or ‘annoying people’ (3C6, 6C6) indicated reluctance to call upon family or neighbours to take them to the doctor outside surgery hours, unless there was extreme need.
Concerns were voiced about the difficulties such a request for help might pose to family or neighbours who ‘have their own worries’ (3C6) or ‘are also in their eighties’ (2C4). Participants spoke instead about waiting: ‘… you hold on as long as you can’ (6C6). The most frequent reason for asking family or neighbours was to ensure the fastest possible access to treatment: ‘they would make the call and might get you into a hospital, maybe, quicker’ (3M1).
Lack of information
People who become sick when their GP’s surgery is closed have only two options to choose from: the DOC and the accident and emergency (A&E) services. Those who had not used the GPOOH service previously were concerned about not knowing what to do if ill at night:
… the biggest thing is, I don’t have a clue … (6C4)
… none of us have a clue, not for the night-time. (6C5)
Some participants, especially those who lived furthest from the treatment centres, expected that a call to DOC would result in a referral to the hospital, since they would only call for a doctor if ‘nearly dead’ (2C3):
… there is no point really … you would be ringing and annoying a doctor who wouldn’t see you anyway. (4M4)
Lack of information was especially evident in the area not covered by the GP cooperative. This included not knowing what number they should call, if the GP surgery number was answered at night and, if so, who they would reach. Furthermore, it was expected that a referral directly to the hospital was most likely where a locum GP was in place, who would not be familiar with their health history: ‘[doctor] would send you to the hospital, even if you came in’ (6C3). Lack of information about DOC, as well as lack of experience with the service, therefore, stopped remote and rural-dwelling participants from considering DOC as a realistic option for urgent out-of-hours care. Such reluctance was succinctly expressed by one woman, who had never used the service:
‘I would think a long time before I would call [DOC] …’. (4M4)
Social networks supporting access
About a third of participants (n=14, 29%) said they would call DOC themselves, if needed, but for many (n=23, 48%) calling a family member, friend or neighbour would be their first response. Worries about their own ability to manage when ill, and the need for support when dealing with the logistics of accessing the service, were clearly stated challenges when considering what to do when sick out-of-hours. For some, as already noted, this was because they were unsure about what course of action to take and sought the input of another party. Others saw family members as being ‘better able to explain’ (4C6) because of the sense of panic and anxiety they themselves would be experiencing when sick.
Negotiating multiple phone calls, as well as answering repeated clinical triage questions, were highlighted as especially difficult: ‘but you have to explain and you don’t know if you are explaining right or wrong’ (4C2). Another person talked about needing the help of a third party to negotiate the complexity of the system, due to their own vulnerability when ill;: ‘you need someone fairly fit to go through the hoops’ (3C2). A common initial response was to wait it out for as long as possible;
You’d need to not be too bad to have to go through all of that … you wouldn’t want to be too ill. If you could do all that you could manage till the morning. I would stick it out because I wouldn’t be able for all of that. (4M2)
Dependence on someone else to make the call to a doctor at night, however, requires that a person has a social network of people who could fulfil this role.
When asked what they would do if they became seriously ill at night participants were clear that for any action to matter it must take place quickly, but it was not expected that this was likely to occur. The ability to access care quickly was seen as an essential feature of urgent medical care, especially outside surgery hours. As one person put it: ‘…When you call the doctor-on-call you want him (now) instead of waiting two hours for him’ (3M1). Where no social network was available, a combination of frustration and resignation was noted, suggesting that either there was nothing to be done or they didn’t know what to do:
What are you going to do? wait till some neighbour comes? God knows when that would be!’ (6C2)
‘Sure, what could you do? Just lie there and die!’ (3M1)
The majority of participants reported they would ‘want to be nearly dying’ (3C4), ‘half dead’ (2C3) or ‘on my last legs’ (3C6) before they would call for a doctor out-of-hours. The reasons for such reluctance were varied but consistent. Challenges to accessing and using DOC included fears about not having urgent needs met quickly enough; the logistics of accessing the service, specifically transportation and lack of information; and the availability of supportive networks. The findings outlined show how rurality impacts the intersection of some of these challenges.
Discussion
People rely on their experiences, expectations and the accounts of others to inform themselves about available services. When the GP cooperative service began in Ireland, in 2000, a general publicity and information campaign was undertaken, but participants said ‘we were younger then and didn’t need it’ (6C4). For those with shrinking social networks and limited community access, the acquisition of accurate current information can be difficult. If people are reluctant to use existing services, lack of experience of DOC further contributes to lack of information, which in turn represents a challenge to using the service.
In the lived experience of participants, each challenge identified was interlinked with others, forming a web of connected issues that serve to frustrate attempts by older people to access or use DOC. These findings suggest that little has changed since Foster et al9 examined the experience of older people with GPOOH services almost two decades ago. Given a preference to see their own GP, older people remain likely to postpone calling DOC until symptoms become alarming or severe and the prospect of an extended wait to see their own doctor becomes too onerous. If unable to access DOC, the remaining option may be to call an ambulance, but this course of action will not be taken until symptoms are severe. The focus on ambulance and A&E services during focus group discussions suggests there may be little perceived practical difference between A&E and DOC, where receipt of care from an unfamiliar doctor is expected in either case.
Anxiety about ambulances getting lost, however, and worry about the length of time before eventually seeing a doctor add to the list of challenges faced by rural-dwelling older people, when faced with a late-night illness. Issues of facility location are central in the decision about which service to call. This is because a call is unlikely to be made to any out-of-hours service until urgency is reached, by which time speed of access may be of higher priority than type of service, especially if the difference between services is unclear.
Participants acknowledged the need to have someone else to call on if they became ill at night, and many expressed anxiety and a sense of vulnerability where they did not believe they had such a person to call. Limited social networks and reluctance to call on family and neighbours, except when in desperate need, makes seeking help from a third party stressful and difficult. Despite consistent reports of needing to be ‘at death's door’ or at least ‘bad enough’ to warrant calling the doctor, participants rarely offered a clear definition of what would qualify as ‘bad enough’. The approval of a third party was required for many participants to legitimise the decision to seek help. King and Farmer26 have suggested that a perception of vulnerability, once acknowledged, also makes accessing services seem too complex and siloed without the support of a third party, but what happens to those who do not have a trusted third party, such as a neighbour or family member, to hand?
Due to the severity of their health crisis, by the time help is sought older people contacting DOC may believe they should be seen at home, but most understand they will probably be required to travel to the treatment centre and many worry about being too ill or not having transportation or social support to do so. When comparing rural and urban GPOOH service callers of all ages in the UK, Turnbull et al27 found that deprivation was a greater barrier than distance for urban-dwelling callers but distance was the major barrier for callers in rural areas. For rural-dwelling older people in Ireland, the impact of living remotely from the DOC treatment centre manifests not only in terms of distance to the treatment centre but also in how that distance influences the decision to seek help and where such help might be sought, such as from A&E, the ambulance service or DOC. Findings show that those living more than a 30-minute drive from the treatment centre were less inclined to call DOC. Neither of the DOC treatment centres are centrally located in either county. When combined with transport difficulties and shrinking social networks, the location of only one DOC treatment centre per county effectively excludes older people, particularly in large remote and rural regions of both counties, from practical access to the GPOOH service. Limited national health service resources mean that this situation may not change soon, thereby severely limiting the out-of-hours medical care options available to older people living in rural communities in Ireland.
Limitations
Findings from this research provide a snapshot of a service that continues to evolve. Nonetheless, the consistency of these findings, when considered with previous research in this area, suggests that service changes to date have not addressed many of the issues of concern for older people. The absence of data examining the experiences of urban-dwelling older people with GPOOH services limits the exploration of whether the barriers identified in this study are also pertinent for urban-dwelling older people in Ireland and, if so, to what extent and in what ways. It is also noted that isolated older people who live alone in remote areas and with significantly limited social networks do not have a voice in this research. Even though addressing the challenges highlighted by this study could be assumed to benefit such isolated older people, an absence of data relating to this cohort of the older population is not only an omission in this study but in the field in general, highlighting a need for further research in this area.
Conclusions
For an older person living in rural Ireland, becoming ill outside GP surgery hours is complex. The obstacles encountered are both real and personal when deciding if and how to seek help. As the social networks of rural-dwelling older people shrink, and available neighbours and friends also become older and less available for transportation and other support, the impact of these challenges on use of A&E and ambulance services may need to be examined. If ill out-of-hours, A&E may be an appropriate healthcare choice for many older people, given the illness severity deemed necessary before they would call for help in the first place. Whether older people choose A&E over DOC because they have accurately assessed the urgency of their healthcare need, because their lack of understanding about DOC has resulted in delayed help-seeking until A&E was required, because it was an easier or more expedient option, or for some other reason, requires further consideration.
Availability of transport is an important factor in both the decision to use DOC and in the ability to access it. This is an aspect of the transport issue, especially for rural-living older people, which has not been discussed adequately to date. Transport challenges out-of-hours add another dimension to the discourse about transport and older people living in rural communities. Such consideration goes beyond the issues of regular rural transport for shopping and social activity or daytime transport needs relating to doctor or hospital appointments or visits. It requires expanding consideration of rural transport to a 24-hour proposition, which needs attention if rural communities are to be truly age-friendly.
The findings have shown that rural-dwelling older people are reluctant to use DOC and that lack of direct experience with DOC is linked with reluctance to use the service. Examining the nature of this connection, measuring the extent to which concerns expressed would ultimately prevent a call to DOC and comparing the barriers for older people in both urban and rural areas warrant further research. When experiencing severe illness, increased vulnerability can undermine even the strongest resolve, best-laid plans and depths of self-sufficiency. An absence of neighbours or family to call for assistance leaves some feeling they have little option other than to ‘wait it out’ or ‘lie there and die’. Reducing reluctance and worry about calling for help requires addressing the challenges of rurality identified in this study and empowering older people in rural communities to access and use existing GPOOH services.
Acknowledgements
The authors acknowledge the funding received from the Cavan and Monaghan Age Friendly County Alliances, NetwellCASALA Research Centre and Dundalk Institute of Technology. Thanks to Dr David Getty for critical guidance during the research process. The support of the Northeast Doctor on Call, CAREDOC and the Health Service Executive regional call centre is also recognised, as are the various groups and organisations that facilitated access to participants for this study.
References
appendix I:
Appendix I: Participant questionnaire
You might also be interested in:
2018 - Lessons for Health Program Monitoring and Evaluation in a Low Resource Setting
2008 - Alcohol harm and cost at a community level: data from police and health
