Introduction
Foetal alcohol syndrome (FAS) is a term initially coined by Jones and Smith1 to describe facial and other birth anomalies, growth deficiencies and developmental delays in a cohort of children with mothers who consumed alcohol during pregnancy. Since that time, a broader understanding of other neurodevelopmental impairments, resulting from alcohol exposure in utero, has led to the use of the overarching term ‘foetal alcohol spectrum disorder’ (FASD)2. FASD encompasses a range of irreversible physical, cognitive, developmental and emotional deficits that can have lifelong consequences for the affected individual, their family and broader society3. Diagnosis of FASD requires a multidisciplinary assessment that identifies severe impairment of the central nervous system in three or more functional/structural domains, in the context of prenatal alcohol exposure. Functional domains relate to overall cognition, behavioural regulation and adaptive functioning4. Individuals from all socioeconomic and cultural backgrounds can be affected by FASD and individuals with FASD may also have a number of comorbidities including chromosomal abnormalities, and mental and behavioural disorders5. Furthermore, individuals with FASD may experience higher rates of negative outcomes including poor school performance, illicit substance use, involvement with the justice system and incarceration3 In Australia, the prevalence of FASD is unknown6; however, two previous studies have documented the prevalence of FASD in high risk populations in Western Australia. The first study was conducted in the remote Fitzroy Valley region of Western Australia where Fitzpatrick and colleagues7 reported that 21 out of 108 (19.4%) school-aged children met diagnostic criteria for FASD. The second study, conducted in a youth detention centre in Western Australia, reported that 36 out of 99 (36.0%) young people had an FASD diagnosis8.
Children affected by FASD may also experience postnatal environmental adversity such as being removed from their biological families and placed within foster care environments9,10. As at June 2017, 17 664 Aboriginal and Torres Strait Islander children (a rate of 58.7 per 1000 children) in Australia were in out-of-home care. During 2016–17, 68% of Aboriginal and Torres Strait Islander children were placed with family members or other Indigenous caregivers. Furthermore, children in very remote areas were at twice the risk of being in out-of-home care compared to children in major cities, and Aboriginal and Torres Strait Islander children living in remote areas were nine times more likely to be in out-of-home care11. In addition, living in remote locations can adversely affect development, with young people being as likely to experience developmental issues compared to their counterparts residing in metropolitan areas12. The burden of early disadvantage can be challenging to reverse ,therefore early interventions structured at improving children’s development can benefit individuals, families and broader society13. Furthermore, effective interventions addressing early disadvantage and vulnerability in Aboriginal and Torres Strait Islander children must be structured around the needs of the children and their families with cultural identity, a pivotal aspect of effective change14.
Taking on the role of a caregiver may present a range of challenges, particularly when caring for a child diagnosed with FASD15-23. Numerous studies have found strength-based approaches mitigate some of the adversity, as explained by caregivers who have developed and adapted strategies appropriate for their home environment and families17-21. Providing routine and consistency has been reported by caregivers as an effective strategy for managing aggressive and chaotic behaviours such as damaging property, impulsive behaviours, violent outbursts to family members and defiance16-20,22. The benefit of family and peer groups to support caregivers of children with FASD has also been documented16,19-22 in addition to recognising the wisdom and practical experience caregivers can provide to health professionals and the broader community18,24. While not specific to FASD, Aboriginal caregivers of children with disabilities have articulated the importance of kinship care for fostering cultural connection as well as providing respite25. In Australia, kinship care is a fundamental aspect of the child placement principles26, where it is appropriate for extended family members to nurture each other in an Aboriginal community context27.
Creating awareness of the many social issues impacting children’s development is important to help families adapt and maintain stability in caring for a child with complex needs19. Understanding the experiences and recognising the valuable knowledge that caregivers have obtained through caring for children with FASD is critical for establishing appropriate supports. Although experiences of caregivers raising children with FASD have been documented in general populations internationally, there is little research documenting the experiences of caregivers in a remote Australian context. Additionally, there is scant reporting describing experiences from an Indigenous perspective, specific to FASD. Therefore, the objective of the present study was to examine the experiences of caregivers residing in a remote Australian community who were currently or had previously cared for children with or at risk of a FASD diagnosis. The findings will be valuable for informing programs at the family, community and broader policy level that can help enhance children’s development and wellbeing.
Methods
This qualitative study consisted of semi-structured interviews underpinned by phenomenology28 embedded within a broader, community participatory action research project, namely Warajanga Marnti Warrarnja (‘Together We Walk on Country’). The project focuses on FASD diagnosis, prevention and therapy and employs a collaborative approach involving local Aboriginal community reference group (CRG) members and local Aboriginal community researchers to strengthen cultural security and appropriateness. The CRG was established to support adherence to community capacity building, empowerment, healing and ensuring cultural connectedness to Country, and has also been pivotal for disseminating concerns raised by the wider Aboriginal community in relation to harmful alcohol consumption in Port Hedland and surrounding communities. The CRG has also contributed to the Hedland FASD network to ensure the needs and priorities of communities are considered29. Understanding the priorities of communities is paramount for building sustainable partnerships and effecting positive change30,31.
Setting
The Pilbara region of Western Australia is a large and complex region spanning 507 896km2, consisting of larger coastal towns, smaller townships and remote inland communities32. Despite primary industries generating substantial wealth in the region, the sheer remoteness of the area, a high turnover of health and social service providers and limited air services creates logistical challenges for adequate service provision33. Socioeconomic disadvantage experienced in some areas of the Pilbara has resulted in higher levels of alcohol use, chronic diseases and mental health issues34. In 2007, The Australian Early Development Index (AEDI) collected data from 31 schools in the Pilbara region, to investigate the developmental trajectory of children attending their first full year of school. The average age of children included in the AEDI was 5.5 years. The AEDI measured five domains: physical health and wellbeing, social competence, emotional maturity, language and cognitive skills (school based), and communication skills and general knowledge. At that time, the AEDI reported 28.9% of children were developmentally vulnerable on one or more domains and 16.6% were vulnerable on two or more domains35. More recently, the 2015 Australian Early Development Census report suggests some children living in the Port Hedland region are experiencing developmental vulnerability36. The percentage of children who were considered developmentally vulnerable on one domain increased from 23.4% in 2012 to 29.8% in 2015. Developmental vulnerability in two or more domains increased from 10.0% in 2012 to 16.6% in 201535. Developmental vulnerability coupled with remoteness and limited service provision suggests a lack of sustainable programs and reinforces the need for appropriate supports and services that can assist in enhancing children’s development. The findings from the AEDI report initiated further investigations into health service provision, programs and practices at the request of schools and Wirraka Maya Health Service Aboriginal Corporation in South Hedland. These investigations resulted in the development and implementation of the Warajanga Marnti Warrarnja project focusing on FASD diagnosis, referral pathways, prevention and therapy supports for families in the Hedland region.
Participants
Parents or caregivers of children with or at risk of FASD diagnosis were identified through a FASD diagnostic clinic and a family support organisation. To be included in the study, participants needed to be residing in the Port Hedland area, including two remote communities, and be previous or current caregivers of a child with a clinical FASD diagnosis or at risk of FASD. Of the 16 potential participants identified, four were uncontactable and one was not available to participate within the timeframe. Out of the remaining potential participants contacted (n=11), seven agreed to be involved and provided written informed consent before participating in the interviews. A total of six interviews were conducted with two participants interviewed at the same time because they resided at the same home and cared for the same child. The caregivers shared their experiences relating to a total of 11 children aged between 3 and 15 years. Participation in the research was voluntary and the caregivers were advised they could withdraw from the study at any time. No birth parents were interviewed; five female caregivers and two male caregivers participated in the interviews. Five Aboriginal caregivers identified as kinship carers and two were non-Aboriginal caregivers. All caregivers had experience of caring for children for a period of 2 years or longer, with several having a number of children in their care. Demographic characteristics of caregivers and children are outlined in Table 1.
Table 1: Demographic characteristics of caregivers and children in the study 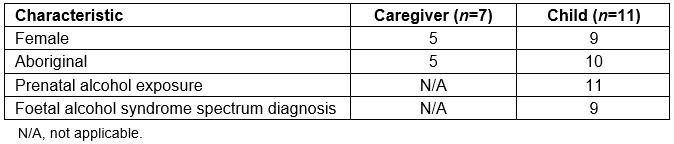
Interviews
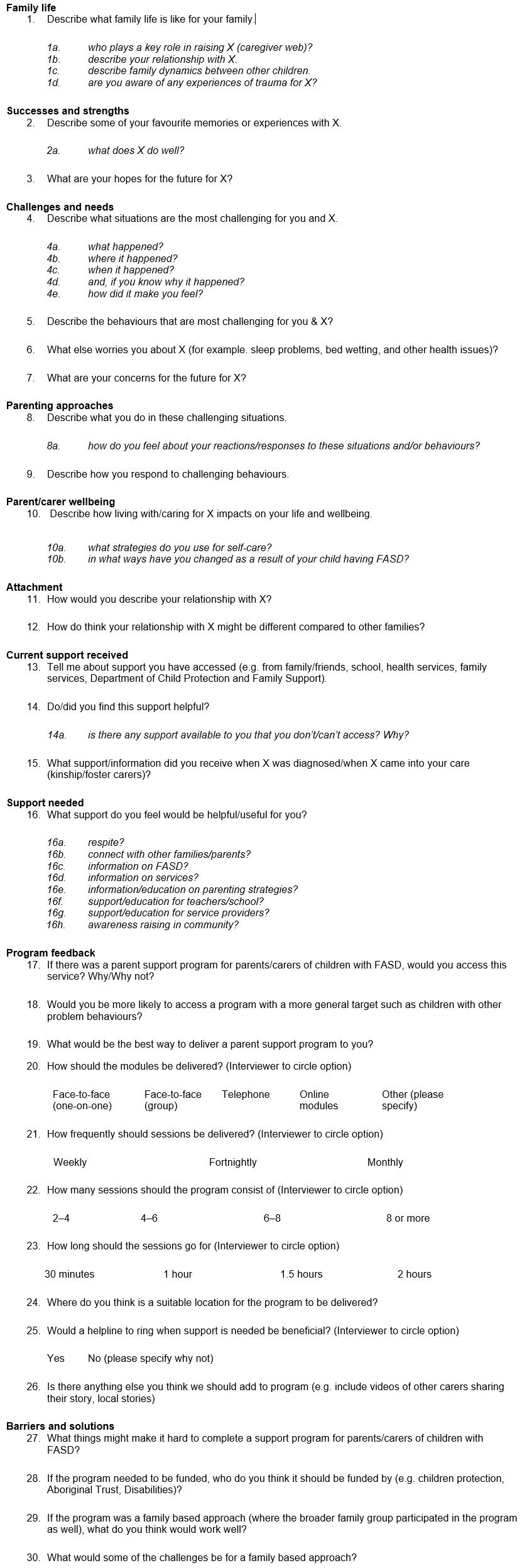
Semi-structured interviews were conducted to describe the lived experience, strengths and needs of families living with a child diagnosed with FASD. A semi-structured interview guide (Appendix I) was developed and subsequently reviewed by local Aboriginal community researchers and CRG members. Questions relating to family dynamics and support systems were added following the review. The participants were also asked specific questions relating to the development and implementation of an appropriate carer support program. Audio-recorded interviews were transcribed verbatim (TM, EA, EC) using NVivo v11 (QSR International; http://www.qsrinternational.com/nvivo) with all identifying information removed and cross-checked for accuracy by one of TM or EA, whoever did not transcribe the interview. A coding system was developed and guided by Bronfenbrenner’s bio-ecological theory. The theory was developed to explain how the intrinsic qualities of a child and their environment interact to influence their development over time37. Data were analysed with an inductive thematic approach by two researchers (TM and EA). Themes were then discussed and agreed by the researchers using an iterative process. To facilitate rigour, discussion and consensus of themes was undertaken with a chief investigator (RW) on the team. An Aboriginal researcher on the team (EC) verified all themes for accuracy and cultural appropriateness. The themes were then discussed with the CRG and Hedland FASD network.
Ethics approval
Ethical approval for this study was obtained from the University of Western Australia Human Research Ethics Council (HREC RA/4/1/8465), Western Australia Aboriginal Health Ethics Committee (HREC 801) and the Western Australia Country Health Service Human Research Ethics Committee (HREC 2015/35).
Results
A thematic analysis approach highlighted four major themes emerging from the interviews: the importance of daily routine and structure, the importance of family support, the benefits of peer support groups and the broader societal issues impacting children’s development. The caregivers provided suggestions for a suitable support program that could be of benefit to themselves and others.
Routine and structure
When asked to reflect on what family life was like for the caregivers, they each explained how chaotic and challenging daily life was when they first began caring for their child. Each caregiver articulated the challenges they had faced and described how over time, and through trial and error, they discovered the benefit of establishing and maintaining routine and structure to assist in creating a stable, well-functioning home environment. Strategies differed between participants; however, they all displayed a sense of validation at discovering the strategy that was appropriate for their child and home environment.
Following the same routine for school: Simple strategies such as following the same routine each day when preparing for school had positive effects and helped children settle:
… our job was to get up every day, make sure there’s petrol, car, food, clothing, um [their] little bag you know enjoying every day, making sure [they] got everything. And [they] got used to that routine so it helped [them] settle. (participant (P) 03)
Eating dinner at the same time: Another caregiver explained that travelling the same route to and from school each day and eating dinner at the same time each night provided stability:
[We] had to have a set routine for them and that helped ‘em a lot, ‘cause if there were any changes [it] sort of seems to throw them off. So even the way we drove to school … and at dinner time it was around about the same time … they have to have a stable place, with a routine, [and] a fixed routine. (P05)
Rules for consistency: Throughout one of the interviews, the caregiver reiterated several times the importance of setting rules and not deviating from them:
See with FASD kids, you gotta be very consistent, very very, they gotta have very ... set rules … you gotta be consistent with FASD. You gotta be really – I know you can’t deviate. Once you … draw that line in the dirt you’ve gotta try, try the best you can to stick with it. I mean it’s very hard sometimes, you know. But you’ve just gotta try. (P02)
Not changing plans at the last minute: Maintaining routine and consistency helped to reduce aggressive or out-of-control behaviours. In one interview, the caregiver explained one of the challenges they faced was to constantly ensure their child’s routine was maintained and any change of plans needed to be articulated to their child well in advance:
If I haven’t pre-warned [them] about something [laughs], that’s probably the most challenging, ‘cause you get caught up, especially having other kids, you get so caught up in what you’re doing as a mum and trying to get stuff organised and get out the door in the mornings, if you don’t have that constant reminder to [them] and then you spring something on [them] it’s like whooo [voice sound] where’s this come from? So it’s that constant trying, me trying to remember to make sure [they know] what’s going to happen for the day, yeah, not just spring it on [them]. (P07)
Support and respite
When asked to reflect on the support systems caregivers had received over time, several spoke positively of the support they had received from schools and medical professionals and how support from their families had been well received by the caregivers. Several caregivers explained that family support had been their only form of respite where the benefit was two-fold: it provided time out for the caregivers, and it allowed the children to maintain cultural and family connection.
Cultural connection: Children would spend time with biological or extended family members, allowing children to experience camping, hunting and bush tucker:
She takes [them] bush and gets [them] to experience … hunting and bush life out there, you know, camping out or bush tucker out there. (P03)
Family was a big support for caregivers: In one interview the caregiver explained how family support and connection had allowed their child to spend quality time with family whilst providing well deserved time out to the caregiver:
I had no support from … the community just my family and my family was a big support. We’d go out bush camping … outdoor stuff or they’d just take [them] and give me weekends off so, so there was more support from my family. (P01)
In another interview, the caregiver described how family support was also beneficial to the children:
Well that’s, when you’ve got a very large extended family like we are, I’m the main carer, [family member’s name]’s a softie, I’m the ogre. … but see, they're very lucky my children, they’ve got my big grandchildren, you know, they got all those [community member surname]’s kids, [community member name], all those people, support me with what I do. (P02)
Issues with respite: All caregivers acknowledged respite was crucial for their own wellbeing, yet several articulated the negative aspects that kept them from accessing it. Several caregivers were content to provide continuity of care for their children rather than facing the challenges of respite:
We don’t – we've never used respite at all … it wasn’t really worth it for us. If anything’s out of [child’s] routine or anything [is] different it just sparks it up for the next week anyway, so to get an hour would’ve cost us the next week and a half of drama so there was really no point in having the respite, yeah. (P07)
I don’t like respite because you don’t know what someone else is gonna to do to your child because if they’re aren’t equipped with ‘em it could come back worse than what it is. (P01)
Another caregiver was explicit about not accessing respite:
Oh no I hate respite … I fret for ‘em [child]. (P02)
Peer support groups
Supporting each other: The interviewers aimed to better understand the needs and experiences of the caregivers, in addition to forming a basis for developing an appropriate support program for the caregivers and their families. While caregivers didn’t state that they felt alone on a personal level, when discussing what supports were needed a recurring comment shared was that anything that could make people feel like they were not alone would be useful. Caregivers articulated that what people needed was someone to talk to and somewhere to go. Much of these discussion points eluded to carers wanting a ‘peer support’ type of group. Several caregivers explained that sharing their stories with others would be beneficial given they had all experienced similar circumstances:
Maybe I could help someone. Give them a little bit of advice, or they might have a different view to me or [would] be able to help me support is the best, … [as] long as these people know there is support out there and it’s, you’re not on your own. You know? (P02)
Well maybe sometimes group things are alright because sometimes people need support, that kind of help from others, they need to know that there’s other people out there with the same, same kind of [experience]. (P06)
I think just having that option to catch up like just be able to … go if you need to go if you’re having a really bad day or whatever and at least … [you] know you’ve got someone there to talk to that’s in the same situation and is having equally as bad a day or they’ve had one yesterday or yeah, yeah just being able to talk about it half the time. (P07)
I don’t know whether we all go through this same thing or different thing, I can’t … think of what the other person might have, what are problems that other child might have so yeah, you know it might be a good opening of the mind and heart of that parent if they [were] to hear our side of the story an’ we hear … the sides of the story of the other people. (P04)
Sharing stories: Similarly, another caregiver pointed out that even though medical professionals have been forthcoming with providing advice, having the opportunity to share stories and strategies between caregivers who have experienced similar circumstances would be beneficial. Experiencing first hand some of the aggressive and out-of-control behaviours and exploring what strategies work or may not work, caregivers have developed the wisdom and insight of knowing how to pre-empt and react to certain situations:
I think the stories help ‘cause I think people can relate and then know that somebody else is going through the same thing. … ‘cause I know with us a lot of the time at the start we were getting told ‘oh try this try’ – and I know everything is trial and error, but sometimes when you get told ‘oh try this strategy, try this strategy’ and you go home and it’s just a failure like it just doesn’t work and … you just think to yourself ‘well what’s the point? … and it’s been told by a professional to you so then you’re like where do I go now if this professional’s told me this and it’s not worked? So, I think definitely the stories help to hear them from other parents and other carers. ‘Cause you know that they’ve been through it they haven’t just read it from a book and gone ‘okay let’s try this’. (P07)
Broader societal issues
Complexities within society: Although caregivers were not directly asked questions relating to broader issues, societal issues relating to alcohol consumption, overcrowding in homes and illicit substance use were discussed. Concerns were raised by the caregivers regarding the complex environments impacting children’s development in addition to sharing their positive support for FASD prevention strategies to encourage healthier drinking behaviours in the community. For example, one caregiver stated that FASD could not be appropriately addressed without first dealing with issues such as overcrowding, violence and substance use:
All this baggage, the trouble, the alcohol, the drugs, fighting and before you know it that person is evicted, there’s no house … If you can prevent [the overcrowding] first, then that person will keep their home and then you can address the FASD need. (P03)
Addressing blame and stigma: Caregivers shared their experiences openly, whilst showing respect towards the child’s biological family and the complex environments that had impacted their child’s development to date. Several caregivers showed compassion towards the biological parents of the children and believed that blame should not be fully extended to the biological parents, as historically there has been a lack of awareness in communities regarding drinking during pregnancy:
They’re still finding different things with these children that have been affected by alcohol. … a lot of the times you cannot just blame the parents, it’s society … This is happening with your child and you don’t understand why it’s happening and you gotta make them feel that it’s not really their fault, ‘cause they didn’t know that if they drank when they were pregnant that this would happen to their children and then they’re made to feel guilty. (P02)
Even a lot of older ones they’ll … [Information about] Foetal alcohol [spectrum disorder] was never around so a lot of the older parents, the mums, did drink while they were pregnant, and it shows in their adult children, and the adult children don’t realise they’ve got that. … it wasn’t advertised … apparently it was OK to have one or two glasses of wine or a couple of drinks a day for pregnant mums. So there’s a lot of grown adults with foetal alcohol [spectrum disorder] and they don’t realise they’ve got it. (P05).
Delivering a support program
The caregivers provided their views on how best to deliver a support program and although they were supportive of a program being developed and implemented, they believed a peer support network group would also be beneficial. One caregiver expressed that a support program would have been beneficial when their child first came into their care, as they had developed their own strategies over time to help maintain a stable home environment and improve their child’s development.
I just think it would be awesome though to yeah to be able to give support to the families it shoulda been round three years ago [laughs] yeah, no [it would] be awesome, definitely. (P07)
Discussion
The findings presented in this article outline the challenges caregivers may encounter when raising a child diagnosed with FASD. The experiences described by the caregivers provide evidence of the crucial knowledge they have to share with health professionals and the broader community. The caregivers in the present study reflected on their own lives and experiences, whilst also displaying respect for the biological families and the complex environments impacting their child’s development to date.
The importance of maintaining routine and consistency to help reduce aggressive or chaotic behaviours of children with FASD has been well documented in the literature17-20,22. Strategies such as following simple routines similar to those described in the present study, for example getting ready for school and having set mealtimes every day, have been integral for establishing a stable environment and they help to optimise children’s development19,20. Although maintaining routine and consistency was challenging at times, it was important, as disruption to daily routines was likely to trigger outbursts and problematic behaviours. As described in the literature, and similarly in the present study, outbursts and problematic behaviours can be better managed when children are made aware of any change to routines in advance19,20.
Support systems that caregivers in the present study have accessed over time were discussed in all the interviews. Even though several caregivers spoke positively of the support they had received from schools and medical professionals, support from their families had been valuable during challenging times. Previously reported literature affirms the role kinship care25 and family support19-22 can have in establishing a stable home environment. Similarly to the literature, caregivers in the present study reiterated the importance of family support to facilitate informal respite, which they found to be beneficial for their wellbeing19.
Maintaining family and cultural connection is critical in Aboriginal communities and underpins the standards of practice outlined in the Aboriginal Services and Practices Framework26. All kinship caregivers ensured their children spent time with their biological families to facilitate cultural connection. In addition, family support presented the opportunity of respite to several caregivers, similar to that documented by DiGiacomo et al25. Aboriginal caregivers in their study explained how support and respite had only been received by trusted family members and not sourced via formal means25. In the present study, caregivers explained how respite was necessary; however, several caregivers were hesitant to source respite out of concern for their child’s wellbeing and the problematic behaviours that result from disruption to routine.
The caregivers were respectful of the support they had received from medical professionals over time, yet they also pointed out that sharing stories and strategies with other caregivers in similar situations would be beneficial. This point is reinforced by previous research where peer support may instil a sense of connectedness and empowerment, as reported by Coons et al19. Caregivers in their study believed that sharing stories, venting frustrations or just having a laugh with others in similar circumstances had been beneficial for their wellbeing. Caregivers are also highly experienced in dealing with the challenges of living with a child diagnosed with FASD15-23, therefore it is important for health professionals to understand and acknowledge their capacity, and work in partnership with the caregivers to optimise service care18,24.
Raising children with FASD can differ from other disabilities given the stigma associated with drinking during pregnancy18,20. Although none of the caregivers in this study were biological parents, several acknowledged the complexities for maternal mothers of children with FASD and the need to avoid placing the blame, which is consistent with previous research18,22. Their responses to biological parents differs somewhat to those reported by Sanders and Buck18 where several caregivers in their study acknowledged the difficulties maternal mothers can experience, and others displayed frustration and blame towards the birth mother for drinking during pregnancy. Whilst no biological parents were interviewed in the present study, previous research highlights the guilt, shame and extra stress experienced by some biological parents due to knowing FASD was a result of their drinking during pregnancy20. Therefore, it is important that a compassionate, non-blaming approach is adopted by both caregivers and service providers when engaging with biological parents.
The themes discussed in this study align with previous research, and they also highlight the complexities experienced by Aboriginal and non-Aboriginal caregivers raising children with FASD in a remote context. The caregivers in this study articulated a peer support group would be beneficial for families living with children with FASD. This kind of group should provide a culturally appropriate and safe space for caregivers to share their experiences and learn from each other. Although online resources are available and support groups have been established in other regions of Australia, there is currently no group or service provision of this kind in the Hedland region. Addressing this gap to support families living and caring for children with FASD residing in this region would be beneficial. Preliminary conversations have taken place with members of the Hedland FASD network, local service providers and the local Aboriginal community controlled health service regarding the findings from this study and the importance of a local organisation adopting peer support groups through their wellbeing program. Providing caregivers with access to FASD resources using local referral pathways will strengthen support and networks for families with children diagnosed with FASD. Further, insightful observations provided by caregivers in this study highlight broader social issues impacting children’s development, such as alcohol and drug use, overcrowding in homes and violence that should be considered at the community level. The narratives also highlight that, although times can be challenging, the ability to adapt to adversity can have a positive impact on the children’s environment, development and well-being, despite the neurodevelopment impairments associated with having FASD. Building the capacity of caregivers and families experiencing adversity is crucial to optimise children’s development. Therefore, effective supports need to incorporate family and peer support, increase access to programs and advocate for supportive and positive community attitudes and practices14.
Strengths and limitations
Although from a small sample, these rich and descriptive narratives provide a deeper understanding of how caregivers and their families have overcome challenges and developed their own strategies to maintain a stable home environment to enhance the development of their children. The rich narratives reported here reinforce the need for local community-driven initiatives such as peer support groups or resources for families experiencing challenges associated with FASD in a remote context. There are currently no support services and limited resources available specific to FASD. The caregivers in this study were all experienced caregivers, therefore the findings presented here may not be relevant to new caregivers or to those not caring for a child with FASD; however, drawing on their learnings can benefit future service provision and resources.
Conclusion
Caregivers have valuable knowledge and wisdom that needs to be considered when health professionals and community organisations interact with families of children with FASD. The caregivers in this study had developed their own strategies through trial and error with minimal support, therefore tailoring services to support caregivers during the early stages of caring for a child with FASD would be beneficial. As formal respite was not utilised by the caregivers in this study due to the child’s safety, inconsistent parenting strategies and interrupted routines, further investigation into training respite caregivers in the area of FASD would be beneficial. Furthermore, respite services should consider provisions to include extended families and kinship relationships in a formal context to enable ongoing cultural and family connection, consistent parenting strategies and routines. A high turnover of health and social service providers coupled with the remoteness of the Pilbara region can create challenges for sustainable programs and supports to be implemented in a remote context. Therefore, building capacity and empowering caregivers to collaborate with health service providers is critical for ensuring sustainable support services are developed and implemented.
Acknowledgements
The authors gratefully acknowledge Emma Douglas, previous research officer; Coral Charles, a community researcher who assisted with the interviews; Wirraka Maya Health Service Aboriginal Corporation; Hedland Community Reference Group; and Hedland FASD network for their contributions; and all the caregivers who shared their experiences and knowledge with the study team. This research has been funded by BHP.
References
appendix I:
Appendix I: Semi-structured interview guide
You might also be interested in:
2016 - Household structure, maternal characteristics and childhood mortality in rural sub-Saharan Africa
2010 - Transfer of learning to the nursing clinical practice setting



