Introduction
Mental health disorders commonly co-occur with substance use disorders and substance use1, with mental disorders typically occurring before substance use2. While epidemiological research has emphasized the heterogeneous etiologies of co-occurring conditions among patients with different mental health disorders3, there is wide consensus on the structural factors that make people more vulnerable to co-occurring conditions4 and that limit their access to treatment5.
Some evidence suggests that co-occurring conditions may be more prevalent in rural areas6,7. Biases within medical data collection8 and a lack of attention to gradations of rurality may have led to an underreporting of co-occurring disorders in rural populations6,7. In rural areas, the prevalence of mental disorders such as depression is also elevated – estimated at more than twice the USA average among rural women9,10.
Certain factors place rural people at heightened risk for behavioral health conditions. Economic shifts over the past few decades have impacted rural communities severely11, deepening poverty in certain rural communities already vulnerable from persistent poverty12. Disparities in available treatment options lead to lack of recognition and of timely treatment13. Shortages of mental health providers remain endemic in rural areas14,15, resulting at times in improper treatment16, and less treatment overall17,18. Likewise, rural substance abuse treatment facilities are underfunded, their counselors face extensive bureaucratic hurdles to delivering treatment, and their patients confront immense social challenges in transportation to treatment sites19.
Rural help- and treatment-seeking are further impeded by the stigma involved in mental health labels and service engagement13,20. In rural contexts characterized by persistent economic exclusion, the stress of shared hardship may make it difficult to recognize co-occurring disorders among family members21. Low-income rural women are particularly vulnerable due to scarcities in services13, and structural conditions that further their vulnerability to violence and abuse, which exacerbate their poor mental health22. When barriers to care seem insurmountable, treatment may no longer be considered an option20,23. Taken together, this research indicates that rural women face immense barriers to behavioral health treatment and adverse social conditions that increase their risk for mental health and substance use disorders.
This study examines how rural women describe the interaction between their co-occurring conditions in an environment with limited behavioral health services. More specifically, this study asks how women with co-occurring conditions who may not identify with a clinical mental diagnosis describe their experience of mental health, and how they relate their social context to their co-occurring conditions. With rural populations facing high rates of polysubstance use, opioid misuse, and death24, these questions address the need scholars have asserted to better understand the social and environmental context of the rural communities at risk11. This secondary analysis focuses on qualitative data from a larger intervention study in rural Appalachian jails that enabled sustained interaction with a hard-to-reach population. All incarcerated participants were women from rural central Appalachia, a subregion including counties in Kentucky, West Virginia, Tennessee, and Virginia with the highest rates of serious psychological distress and major depressive episodes, high rates of opiate abuse, and growing use of heroin8.
Methods
Participants
As part of a larger study, data were collected from December 2012 to August 2015 from rural women recruited from three jails located in Appalachian Kentucky. Jails were located in counties classified as non-metro, with small urban populations or completely rural (rural–urban continuum codes 5, 7, and 9), serving local residents from counties with similar rural designations. Inclusion for the larger study, described in more detail elsewhere25, included moderate risk for substance use disorder, self-reported sexual risk behavior in the 3 months prior to incarceration, Appalachian residence, and consent to participate. To enable secondary analysis, a purposive sample of active participants at the time qualitative data analysis began was generated from the broader sample. Participant demographics and behavioral health are included in Tables 1 and 2, respectively. Inclusion criteria consisted of completing four or more sessions, agreeing to have at least three sessions audio-taped (n=24 participants, n=87 transcripts) to facilitate qualitative data analysis, self-reported drug use, and endorsing co-occurring mental health symptoms (depression, anxiety, or post-traumatic stress disorder) as measured by Global Appraisal of Individual Needs criteria26.
Table 1: Sample demographics (n=24)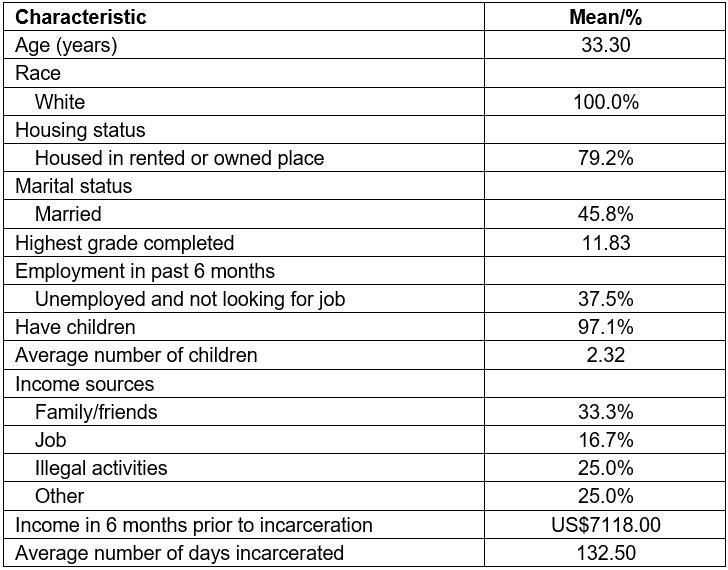
Table 2: Drug use and mental health in sample (n=24)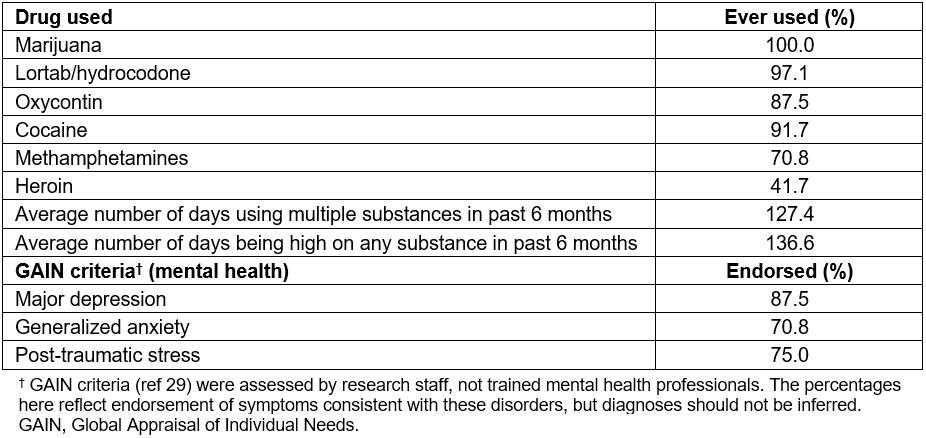
Procedure
Participants in the larger study provided informed consent, were screened for substance use, interviewed, and randomized to a brief intervention in which they worked with a study interventionist who engaged in four motivational interviewing sessions to reduce HIV/HCV risk through decreasing high-risk drug use and risky sexual behaviors27. Motivational interviewing, an evidence-based practice, facilitates empathetic communication and mutual respect, while identifying resistance to change28. With permission from participants, intervention sessions were audio-recorded and transcribed verbatim.
Analysis
This interdisciplinary team of researchers employed directed content analysis techniques29, generating codes that encompassed women’s understanding of the relationship between their co-occurring disorders, concentrating on women’s colloquial language about symptoms, and the trajectory of the co-occurring conditions (eg substance use to deal with mental health, perceptions of substance use as mental health ‘failure’). The team applied initial codes to a subset of transcripts to identify exemplars and exceptions and finalize code definitions. The team continued reading transcripts until concept saturation was reached, when no new themes emerged. Employing inter-coder reliability tests with Cohen’s kappa, all codes were discussed and revised, with each tested until agreement reached 0.8030. One team member applied codes line by line to transcripts, and the lead author checked the coding to further reliability. The lead author summarized the content generated in the first coding cycle and generated a second set of themes, which were attached line-by-line in a second coding cycle to capture patterns, extend theories, and test models about the co-occurring conditions31. For ease of reading, quotes presented in the text were lightly edited to remove false starts and filler words.
Ethics approval
This study was approved by the Institutional Review Board, which conducted a prisoner review (#12-0372-F6A).
Results
Several key themes were identified: (1) the social and structural conditions of women’s lives that made them vulnerable to poor mental health and substance use; (2) women’s experience of feelings as dangerous and desire to escape them through substance use; (3) the struggles that women identified in understanding themselves in the wake of substance use; and (4) the challenges of navigating stigma exerted by medical and justice systems, community members, and themselves. Because few women in this setting identify with a clinical mental health diagnosis, mental health is described through ‘emotions’ or ‘feelings’ in place of symptoms, while acknowledging the deep pain – and clinical relevance – in women’s experiences.
Structural vulnerability
Women described how drugs enabled escape from prolonged mental distress emerging from stressful life conditions resulting from poverty, including unstable home environments, violence, and repeated grief. Drug use offered women an avenue to soothe negative emotions that felt otherwise unmanageable. One woman mentioned a traumatic event from childhood that she had never disclosed to anyone. When she first became high, she realized that ‘I found something that numbed the inside pain … and learned how to not hurt. But it helped me deal with things and so I stuck with that.’ Poverty forced some women into abusive relationships that left lasting emotional impacts. One woman, describing how she had always been forced to rely on men for income, commented:
When [you] gotta be with somebody that you don’t want touching you, you know, it makes you want to get high.
Many women described how drug use helped them navigate difficult social situations arising from poverty – such as having to share accommodations because of limited income or relying financially on emotionally abusive family members. Drugs allowed women to silence their frustration in these situations, explained one woman:
If I have a buzz I’ll just let it go, but being straight I have an open mouth.
Without substance use, women’s ‘open mouths’ might voice critiques within their social relationships that could threaten their access to housing and critical livelihood resources.
In a region where shortages in services and extensive poverty only furthered the importance of family relationships, many women felt responsible for managing intense family responsibilities that left no option for expressing vulnerability. In their families and communities, one woman explained, ‘you don’t feel like you can cry’. Prolonged, unresolved mental distress, women described, erupted into acute mental health crisis. One participant recalled:
I can be strong for a long time and then I break down all at once … it seems like everything falls on me at one time and then I just want to run to drugs.
Participants perceived mental health as poles of strength or total breakdown. In a context where women face immense social responsibilities and pressure to be strong for others, women elaborated how drug use offered social freedom:
It’s always been my comfort zone … It’s always been the one that makes me feel better.
In this freedom, women neither had to respond to social demands, nor demonstrated their strength for others.
Substance use to avoid feeling
Most participants described the immense, constant burden of their negative emotions, including being overwhelmed, angry, distant, worried, worthless, down, fearful of the future, or burdened with bad memories. Thus, many women associated ‘feeling’ with only these negative emotions and sought to escape or control feeling. Although women hoped to control these feelings, almost none described services or treatment that could help them – unsurprising in a region with extensive barriers to care. Given this challenge, women described how substance use seemed the only way to resolve emotional escalation. As one participant summarized:
I can’t find a way to calm down. Whenever I feel like I get to the point where it’s building and building I just wanted to go away.
Most women described how they sought to escape or avoid negative feelings that they wanted to ‘forget’ or did not know how to ‘deal with’.
Although most participants explained that drug use did not enable emotional recovery, it enabled women to avoid the pain involved in ‘feeling’. Gradually, drug use perpetuated a cycle in which ‘the reason you stay high is the stuff you hold inside’. Many women reported relief that, when using drugs, ‘I don’t have to feel nothing on them. Like anything, no pain, I don’t hurt or nothing’. Over time, some women did not trust their emotions without drug use. As one woman put it:
You can’t deal with nothing sober. It is not so much I want a Xanax.
Rather than pursuing a high, she sought Xanax because it enabled her to socially and emotionally function; the alternative was not being able to ‘deal’ with anything. Although women were frank about the emotional roots of their drug use, some morally censured it:
I just don’t like dealing with reality, plain and simple. That might sound like a wimp’s way out … but I just always got high so I didn’t have to deal with emotions.
In this moral framing, women advocated for ‘dealing with’ emotions but avoided naming how – perhaps due to limited social support and limited mental health services. After sustained drug use, many were ambivalent about the potential for exposing dangerous feelings. One participant explained:
That’s where I feel a lot of rehabs are wrong. They say focus on yourself. That’s not good for me. I just don’t know what else is hidden there that might open up.
Self-dislocation
Many women described actions related to their addictions that were distinct from ‘who they really were’. Although almost all women attributed their drug use initiation to the desire for relief from negative emotions, at the time of the interviews many were confused about how to emotionally engage in their lives. After long periods of drug use, many women were eager to pursue treatment and resolve the mental health challenges they thought sustained their drug use. As women acknowledged long-term drug use, many reflected on the difficulty of knowing who they were in the present. Their former drug-using selves, recalled nearly all participants, were unruly, unmotivated, or existentially absent:
I stayed strung out so long I don’t know if I’m still recovering from it or not.
Women’s narratives made clear the long-term process of self-dislocation that followed them even as many sought to end their drug use.
Many women had turned to drug use to escape the painful mental health effects of trauma, only to incur further trauma during their drug use that had its own mental health effects. One woman, recalling how she engaged in sex work to support her drug habit, reflected:
I used drugs to forget but I got so addicted that I become someone that I know I wouldn’t be.
The trauma she had experienced from rape and the drug use that followed made her feel that ‘It’s like I’m two, three different people in one body’. Many women mourned the fact that although now, without drug use, they might be different than who they were while using drugs, they still had changed. Describing her mother’s reflections on her transformation, one woman commented:
I wasn’t who I used to be and she [my mother] would always say, ‘I want the old you back’.
Some reflected with ambivalence on changes in their personalities after they no longer used drugs. Having become accustomed to the gregarious personality that drugs engendered, one participant reflected:
I would like to find that happy medium, the social butterfly that doesn’t get into all this trouble, and still keep my head about it.
Some women were frustrated with the social reactions they received after ending substance use:
You take me as I am. Maybe on drugs I was more mellow. I mean I was me. But maybe I wasn’t as apt to knock the crap out of my family.
With their minds ‘clear’, women described full emotions and aspects of their personalities they struggled to negotiate.
Navigating stigma
Women reflected on how their social class and sense of respectability shifted after drug use. One woman explained:
I was raised good, that’s how I was brought up. I don’t think anyone growing up says ‘I wanna get high’ or ‘I wanna be a drug addict’.
Some responded with disgust and disorientation to the physical manifestations of their drug use:
You have track marks everywhere, I mean it’s just dirty. And you feel so nasty and I’m not that type of person originally.
Even as women faced stigma for using drugs, many described a continuum of substance use, in which some use was characterized by more extreme consequences. Several women recalled humiliating poses of people falling asleep in their food after using drugs. Others pointed to depths of use that they characterized as taboo:
It’s like a junky, they will just jerk [drugs] out right with the kids there, they are so used to doing something. [But] no, my kids never seen me drink. I was actually a good mom.
This mockery of a supposed lack of self-control among people who use drugs (sometimes including themselves) was contrasted to emotions that were properly managed. At the same time, self-identifying as a ‘good mom’ responded indirectly to stigma against women who use substances by asserting their continued ability to fulfill gendered care-giving obligations.
A few women described drug addiction as a disease, but the majority endorsed ideas about self-control more common to interventions based on abstinence, which remains the predominant form of treatment in the region. Women expressed disapproval of others who could not control addictions:
If you sit and tell yourself you can’t [quit], you can’t. You can do anything you tell your body, and your mind, to do.
Other women chastised themselves as they imagined themselves relapsing, arguing that they should ‘know better’. Some participants judged these tendencies negatively:
I was weak with my emotions. I went back to the dope to handle the emotions I was going through.
Others articulated similar ‘choices’ with respect to how women dealt with their mental health:
Real life is, you learn how to deal with things and you don’t have to go and get high to deal with them.
Yet, there were few options to learn to ‘deal with things’. One woman differentiated between the positive work she accomplished in rehab and the difficulty of applying her mental health plan at home:
In rehab, it’s kinda like your safe haven. You’re in the bubble, you’re not out with the real world. You got everything kinda like handed to you. Ain’t gotta worry about nothing.
Women’s narratives revealed how they wrestled with stigmatizing expectations about social class, gender, and the ‘proper’ management of co-occurring disorders. Although at times women named the structural constraints that furthered such stigma (eg the expectation to ‘deal with things’ outside of rehab without support), they also responded to stigma by differentiating themselves from the supposed real ‘junkies’ and censured themselves for not fulfilling the immensely challenging task of ending substance use and managing mental trauma without treatment, or economic or community supports.
Discussion
This study explored how rural women reported using drugs to deal with mental health issues. Similar to other studies on rural women’s substance use32,33 and other populations of incarcerated women34, women in this study commented that, in the absence of emotional support or therapeutic tools, drug use enabled them to escape emotional pain. However, drug use introduced new mental health challenges: the guilt of lost opportunities, social disappointments, and a sense of dislocation. While affirming research on the gendered social determinants of co-occurring disorders for vulnerable women35, this study offered several contributions. First, rural women’s narratives were highlighted, a perspective under-emphasized in the literature on rural co-occurring disorders7,8. Second, literature concerning rural women’s ‘self-alienation’ in substance use32,33 was built upon. Finally, this study commented on the appropriateness of studying co-occurring conditions among rural women within an incarcerated population.
This study’s findings are located within the larger research on rural health, as well as within Appalachia specifically. Study participants mostly did not comment overtly on their rurality in these interviews – either as an aspect of their identity or a characteristic shaping their behaviors. Central Appalachia has one of the lowest net migration rates in Appalachia, with low population change and less out-migration than previously36. Studies with other central Appalachian populations show intensive interactions among kin in terms of social networks37 and social support21, suggesting that participants might be likely to identify themselves within these relationships. In addition, with the interviewer as a therapist from the region, it makes sense that identity was not highlighted as an area to be explained, as can be the case when interviewer–interviewee identities do not concord. Despite the fact that rurality was not overtly discussed, there is not resonance between participants’ perspectives and research on Appalachian and rural social dynamics. Interviews illustrated the tension between how women hoped to manage their emotions and how they actually did – through drug use. Echoing previous research in Appalachia describing the desire for independent endurance20, a central theme was women’s longing to ‘control’ their thinking: ‘dealing with’ their pain and ‘knowing better’. Women’s aspirations for control emerged in part from gendered expectations to be a strong family member without emotional vulnerability21. At the same time, women’s emphasis on control echoed moral discourses communicated in justice and healthcare systems framing substance use as an individual choice – even as it clashed with their accounts of social conditions shaping their health. While other research has emphasized the ‘erosion of the power of family and community networks to assist in personal coping skills’ in rural areas8, there is a need to caution against pointing to diminishing social capital of families and communities without an equal emphasis on the high burden of care placed on rural families in the absence of more extensive services.
Previous research on rural women who use drugs or alcohol describes ‘self-alienation’32,33 – the ‘unarticulated, all-consuming, continuous, and escalating meaninglessness of the women’s existence’32 – as a cause and result of substance use. This theme was developed further in research on rural women’s limited self-esteem13. As with the participants in the original work on self-alienation, many women in this study described extensive trauma and grief emerging from cumulative stress of poverty and demanding relationships that contributed to their emotional pain. The intense, unceasing emotional pain that women experienced made them hesitant to ‘feel’, leading them to ‘run to nowhere’33 through substance use. Before, during, and after drug use, women described being outside of their minds – trying to escape painful feelings, enduring the dissociation of trauma, looking at different versions of themselves, fearing their minds without the calming effects of drug use. In this way, participants seemed reticent to embrace their ‘real selves’, arguing that they needed to be controlled.
In contrast to Boyd and Mackey’s work on self-alienation, which focused on alcohol use33, women in this study confronted deeper stigma due to the nature of the substances they used: substances that were criminalized and resulted in incarceration, sometimes involved separate social networks to access, and posed greater immediate risk of overdose. Such stigma existed in spite of the fact that substances were sometimes used in women’s immediate families or communities. Study findings indicate that, as a result of this stigma, women experienced what might be more appropriately described as self-dislocation into multiple selves. Such multiplicity is evident in the way that they struggled to recognize themselves at times, descriptions of themselves as distinct from their original selves, and in assertions that their current awareness morally demarcated them from other users. Women’s portrayal of their drug-using and non-drug-using histories as actions of separate selves may respond to the pressure to distance themselves from drug use seen to defile their feminine identity38. Their non-drug-using selves enabled women to fulfill idealized family roles. Their selves that used drugs responded to the inherent stress of their families but also inflicted damage on their families. Still, many described how their identities had become hybrid: shaped by continued struggles with addiction and haunted by the same unresolved mental health challenges that caused them to initiate drug use. Women’s entrenchment in different social networks during periods of drug use and abstinence furthers this hybridity23,39. In contrast to the self-medication hypothesis that posited that individuals with mood disorders used substances to self-medicate40, the complex trajectories participants described emphasized an overall sense of mental disorientation that could no longer be resolved by substance use.
Is there something to be learned about co-occurring conditions in rural populations from rural women who are incarcerated? Indeed, incarcerated women experience significantly higher prevalence of serious mental disorder and co-occurring substance use disorders than the general population35, related in part to the disproportionate rates of interpersonal violence and poverty they face34. However, community-based samples of rural people who use drugs in Appalachia have high rates of previous incarceration: 71% to 80%41,42. In rural areas, particularly the US South, the rate of women’s incarceration increased by 43% between 2004 and 2014 even as crime has declined, driven by the financial incentives of incarceration to local governments and limited diversion alternatives43. These systemic factors driving rural incarceration suggest that, as the rural incarcerated population grows, its composition may also be changing – including women who previously may not have been jailed.
Based on research on incarceration, it is anticipated that, compared to rural women with co-occurring disorders in the community, incarcerated women with co-occurring disorders would be harmed by incarceration’s immediate impacts on mental health and long-term impacts on overall health through limiting access to housing and employment44. However, high rates of incarceration among people who use drugs, particularly in regions such as Appalachia, indicate that the vast majority of women who have co-occurring substance use and mental health disorders are incarcerated at some point. Those who are not immediately incarcerated may bear the secondary impacts of incarceration on family or community members45. In light of these increasing rates of rural incarceration and its community-wide impacts, there is much to be learned about rural co-occurring conditions even from an incarcerated subset of the population. Moreover, the overlaps between these findings in the rural context and the broader research on incarcerated women with co-occurring disorders indicates the importance of comparing across vulnerable populations, while drawing attention to the particularities of contexts that shape experience and access to treatment.
Limitations
This study may be limited by the secondary analysis of therapeutic sessions, rather than directed interviews. Data may have concentrated disproportionately on behavioral change, potentially restricting further discussion of women’s understandings. Second, the sample was drawn from several jails in Appalachia and is entirely white; therefore, some aspects of study results may not be transferable to a broader sample of rural women. Third, while the motivational interviewing sessions encouraged participants to formulate strategies for managing their co-occurring conditions, questions did not engage directly with women’s treatment-seeking behavior.
Conclusion
A wealth of research has demonstrated the effectiveness of cognitive behavioral therapy for low-income women similar to those in this study46. Specific versions of cognitive behavioral therapy may be most relevant for rural women with co-occurring conditions, such as those that are adapted for particular mental health disorders, in combination with substance use treatment47 and trauma-informed approaches to address the long-term impacts of violence experienced by many women in this population48. Yet reviews of research on behavioral healthcare for vulnerable women underscore the fact that treatment is not even an option for the vast majority of women, not due to individual attitudes but to immense social and structural barriers that prevent women from identifying their co-occurring conditions as capable of treatment, reaching treatment, and sustaining the course of treatment necessary to address their extensive challenges49. Practitioners must both receive support for their work and be familiar with the cultural variable experiences of behavioral health among rural residents50. Mental health technologies, such as smartphone applications, may reduce some of the barriers that rural vulnerable women face in seeking treatment; however, further research and community input must be used to understand remaining questions about accessibility, literacy, and clinical support51. Although the study’s goal was not to examine women’s experiences in treatment, it was found that few women described the option of treatment in their narratives about mental health – in spite of the fact that treatment can be court mandated for incarcerated women – confirming existing research on the need first and foremost to increase the capacity of rural behavioral systems and decrease structural barriers5. In an era of evidence-based behavioral healthcare, study results indicate that, in addition to the need to attend to the dimensions of effective treatment, the need to identify and test the implementation strategies best suited to engaging rural women with co-occurring conditions in treatment is perhaps the most urgent. Such investigation must encompass not only the logistics of getting women to treatment, but also how to keep women in treatment when the social and economic demands they face make prioritizing one’s own care so difficult.
Acknowledgements
We would also like to recognize the cooperation and partnership with the Kentucky Department of Corrections and the local jails including the Laurel County Detention Center, Kentucky River Regional Jail, and the Leslie County Detention Center. Finally, we greatly appreciate the editorial assistance of Dr Sheila Clyburn and comments from Dr Mairead Moloney.
