Introduction
Community acquired pneumonia (CAP) is an acute infection of the pulmonary parenchyma which occurs in people who do not live in long term care facilities and have not been hospitalised at least 14 days before the manifestation of symptoms, such as fever, rigors and cough1. Streptococcus pneumoniae is the pathogen most commonly identified as aetiologic factor of CAP, although various other pathogens can also cause the disease2,3.
Disease management largely depends on the individual clinical assessment of each patient. Typical symptoms indicating CAP are cough, dyspnoea, fever, chills, rigors and chest pain, and examination includes chest radiography, blood tests and oxygenation assessment4,5. Patients with low risk pneumonia are managed as outpatients, medium risk pneumonia requires hospitalisation, and high risk pneumonia usually requires admission to an intensive care unit (ICU)5.
CAP imposes a high disease burden to the population, with its incidence being higher in children and the elderly6,7. CAP mortality ranges between 1% and 48%8,9. The global burden of lower respiratory tract infections, which include CAP, has been estimated at 91.8 million disability-adjusted life years (DALYs), causing more than 2.3 million deaths worldwide in 20167. In Europe, CAP is the first cause of death related to infections and its incidence is expected to rise as the population ages10. In Greece, there has not been any organised effort to record and investigate the disease epidemiology at a national level. However, a recent study in a rural setting has estimated that hospitalisation rate for CAP patients amounts to 32%, and the median hospitalisation duration is 7 days11. In another study, the mean hospital stay for CAP in Greece was estimated at 9.6 days12.
As well as a high burden of disease, CAP entails a significant economic burden for health systems worldwide. In Europe, CAP costs more than €10.1 ($16.8) billion each year, with hospitalisation accounting for more than 50% of it, especially for elderly patients8,10. European studies have estimated a mean direct CAP cost per episode of between €432 and €1683 per hospitalised patient, while outpatient costs represented less than 10% of the total cost8,13,14. A comparative study across European countries showed that the mean hospitalisation cost per patient ranged from €1459.60 to €8443.89, while the corresponding cost for Greece was estimated at €3542.9212. (At the time period for the study, €1.00 was approximately A$1.50.)
Existing calculations for the economic burden of CAP in Greece have been based only on estimations rather than on real patient data, which are considered a more efficient tool for such analyses. Using primary patient data, this analysis thus aimed to estimate the cost per inpatient and outpatient of CAP in Greece based on the official resource prices of the Greek healthcare system. The study also aimed to investigate factors associated with the probability of hospitalisation and the determinants of inpatient and outpatient costs.
Methods
Data were collected from the Athens General Hospital for Chest Diseases (Sotiria), a national centre for pulmonary diseases, in collaboration with the 6th Pulmonary Clinic of the hospital.
Primary data for the analysis were based on a retrospective study of patients who visited the outpatient department of a tertiary hospital in Athens, Greece, with pneumonia symptoms. The data collection period was between October 2015 and March 2016, which coincides with the high incidence period in Greece. Inclusion criteria were (1) definitive diagnosis of community acquired pneumonia by the treating physician based on the necessary diagnostic tests, (2) eligible patients being at least 18 years of age and (3) patient capacity to consent. Exclusion criterion, according to the disease definition, was hospitalisation during the last 14 days before symptoms emerged1.
For each patient diagnosed with CAP, resource use patterns were collected. Resource use categories for estimating the inpatient care cost were diagnostic tests, medication, hospital stay duration, additional laboratory and radiographic tests during hospitalisation and discharge instructions. To calculate the cost in outpatient level, the analysis considered the following resource use categories: diagnostic tests, medication dosage and duration, and hospital visits. Moreover, the dataset included information on whether patients of both groups returned for reassessment. If this was the case, it further recorded the additional tests and medication they were provided. Further data collected in the study included age, smoking status, comorbidities, symptoms that led to the hospital visit and duration of symptoms before visiting the hospital.
Cost calculations were performed from a third party payer perspective, so only direct costs were estimated, while unit costs refer to 2016. The cost (C) for each resource use category derived from the official price bulletin of the third party payer and the total costs were estimated as follows:
Cinpatient = Cdiagnostics + Cmedication + Chospital stay + Cadditional tests + Creassessment
Coutpatient = Cdiagnostics + Cmedication + Chospital visits + Creassessment
Specifically, the cost units for laboratory and imaging tests derived from the official state prices issued by the Greek National Organisation for Healthcare Services Provision15, while the unit costs for medication were sourced from the Official Medication Price Bulletins which effective during the study period16,17. Concerning hospitalisation cost, unit costs derived from the Greek Diagnosis-Related Group system costs18, adjusted for hospital stay longer than the average expected in the system as well as for staff salaries, which are not incorporated in the cost system, and discounted at present values with a 3% discount rate.
Apart from estimating the costs, the present analysis aimed to uncover the factors associated with the probability of hospitalisation. In doing so, a logistic regression model was employed, and the dependent variable of the analysis was inpatient admission (value of 1 if the patient was admitted to hospital, or 0 if CAP was treated in outpatient care). Further, this analysis focused on the determinants of inpatient and outpatient costs. Taking into account the distributional characteristics of healthcare costs, this study employed a linear regression model with a log-transformed dependent variable. The independent variables of the analysis were: gender, duration of symptoms, age, smoking, presence of comorbidities and number of symptoms.
Ethics approval
All necessary ethics approvals were obtained from the Scientific Committee of Athens General Hospital for Chest Diseases (Sotiria), as well as from the Bioethics and Research Ethics Committee of the National School of Public Health in Athens (1029/24.7.2015).
Results
Sample characteristics
The study sample consisted of 249 patients, 149 of whom were hospitalised (59.8%) and 100 were treated as outpatients (Table 1). The mean age of the total sample was 55.1 (standard deviation (SD)=18.764) years, while separately it was 61.4 (SD=16.80) years and 45.8 (SD=17.66) years for the inpatients and outpatients respectively. Additionally, 53.3% of the total sample were current smokers. As shown in Table 1, 67.8% of the hospitalised patients and 42.0% of the outpatients had a chronic health condition, with pulmonary and circulatory diseases being the most common for both patient subgroups.
Before visiting the hospital’s outpatient department, 71.7% of the sample had on average two to three coexisting symptoms, with fever, cough and shortness of breath being most commonly reported (Table 1). Mean duration of symptoms before hospital visit amounted to 4.8 (SD=3.054) days, ranging from 1 to 15 days of sickness.
Table 1: Study sample characteristics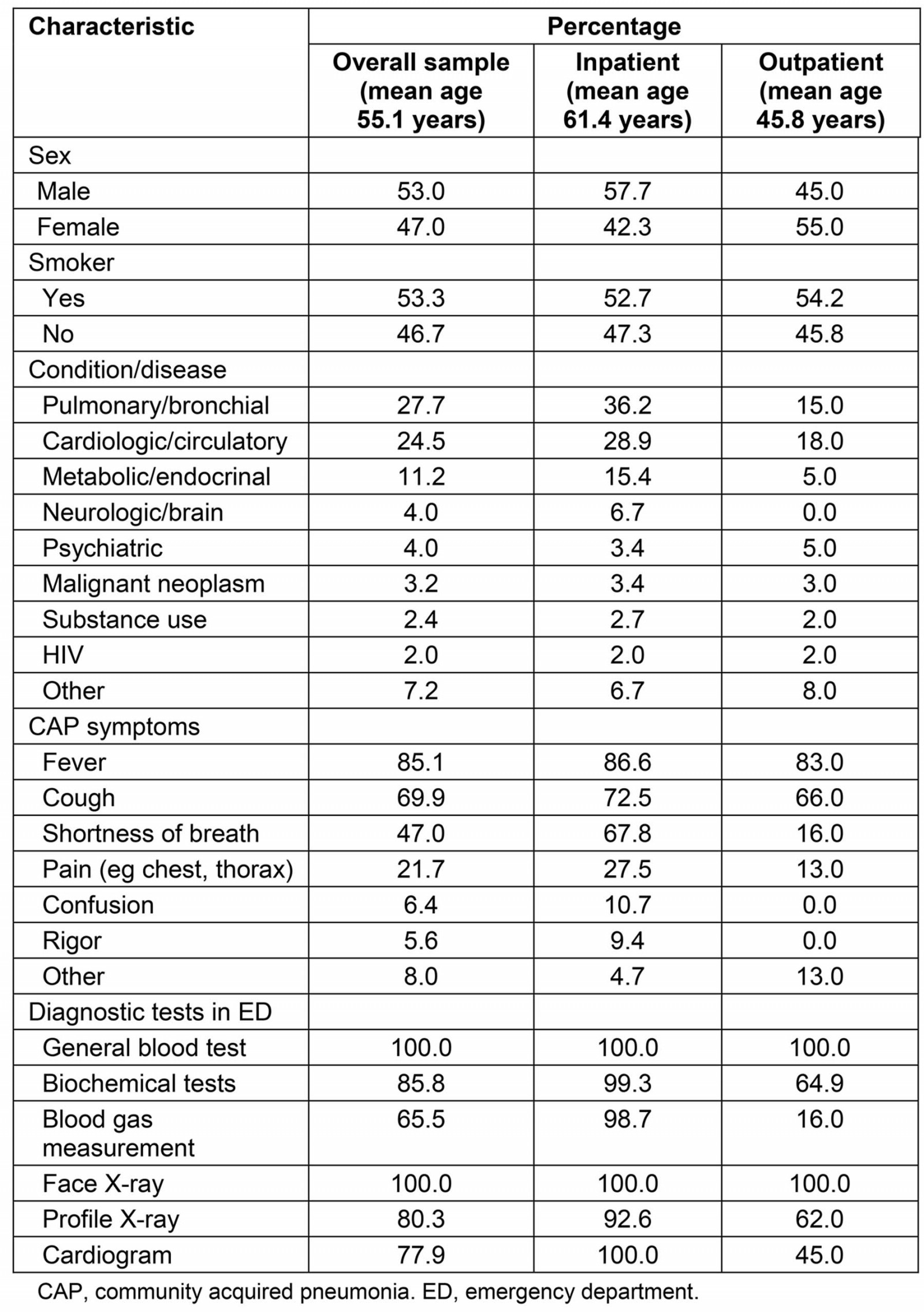
Resource use, cost analysis and regression results
In order to be diagnosed, every patient in the sample had a face X-ray and a general blood test. Additionally, a set of biochemical tests (eg urea, creatinine, alkaline phosphatase) was performed in 85.8% of the sample and profile X-ray in 80.3% of the sample, as presented in Table 1. Apart from general blood test and face X-ray, all diagnostic tests were performed at a much greater frequency for those who were hospitalised upon diagnosis.
Out of the 149 hospitalised CAP patients, 91.3% were treated in the general ward and 8.7% required admission to the ICU. The mean length of stay was estimated at 11.35 (SD=9.170) days, ranging from 1 to 70 days. Mean length of stay for the patients admitted to the regular hospital clinic was 10.21 days (SD=7.200). For the subgroup of patients admitted to the ICU, the mean length of stay was much greater, approximately 23.38 (SD=20.197) days, 16.08 (SD=14.068) days of which were in the ICU and 7.30 (SD=7.952) days in the regular clinic.
During their stay in hospital, all inpatients were submitted to face X-ray, with a mean of 3.34 (SD=3.670) X-rays per patient; 92.6% to profile X-ray, with a mean of 1.77 (SD=1.179) X-rays per patient; and 99.3% to a general blood test. with a mean of 3.10 (SD=2.288) tests per patient (Table 2). A total of 99.3% of all inpatients were discharged (n=148) (one patient died in hospital) and 35.8% were prescribed further medication. Only 3.37% returned to the hospital for reassessment within a week after discharge, all of whom were submitted to face X-ray and all but one to profile X-ray. Of the outpatients, 95.0% revisited the hospital for reassessment of their condition. Face X-ray was performed for all patients, profile X-ray for 24.2% and thorax computed tomography for 7.4%.
For inpatients, the cost analysis included cost of diagnostic tests, hospital stay, medication during hospitalisation, blood and radiographic tests during hospitalisation, medication prescribed upon discharge and reassessment tests (if readmitted to the hospital). For outpatients, cost of hospital visits, diagnostic tests, prescribed medication, reassessment tests and additional medication after reassessment were calculated.
Hospital stay accounted for the greatest part of the inpatient cost, and admission to the ICU represented 37.0% of total hospital stay cost. Average cost per hospitalised patient was estimated at €7406.56 ($12,322.46), while the corresponding cost per patient in outpatient care was approximately €110.64 ($184.07) (Table 3).
Model 1 in Table 4 shows that the odds of hospitalisation for an elderly person are three times the odds of hospitalisation for an individual aged less than 65 years. In addition, the number of symptoms is positively associated with hospitalisation, whereas there was no statistically significant relationship between comorbidity and the probability of hospitalisation. Figure 1 indicates how the predicted probability of hospitalisation changes with age, while Figure 2 shows that the probability of hospitalisation increases with number of symptoms. According to Table 4 (Model 2), males tend to have higher hospitalisation costs compared to females, and the duration and number of symptoms are both positively associated with inpatient costs. For outpatient cost, comorbidity is a statistically significant determinant.
Table 2: Frequency of testing and mean number of tests per patient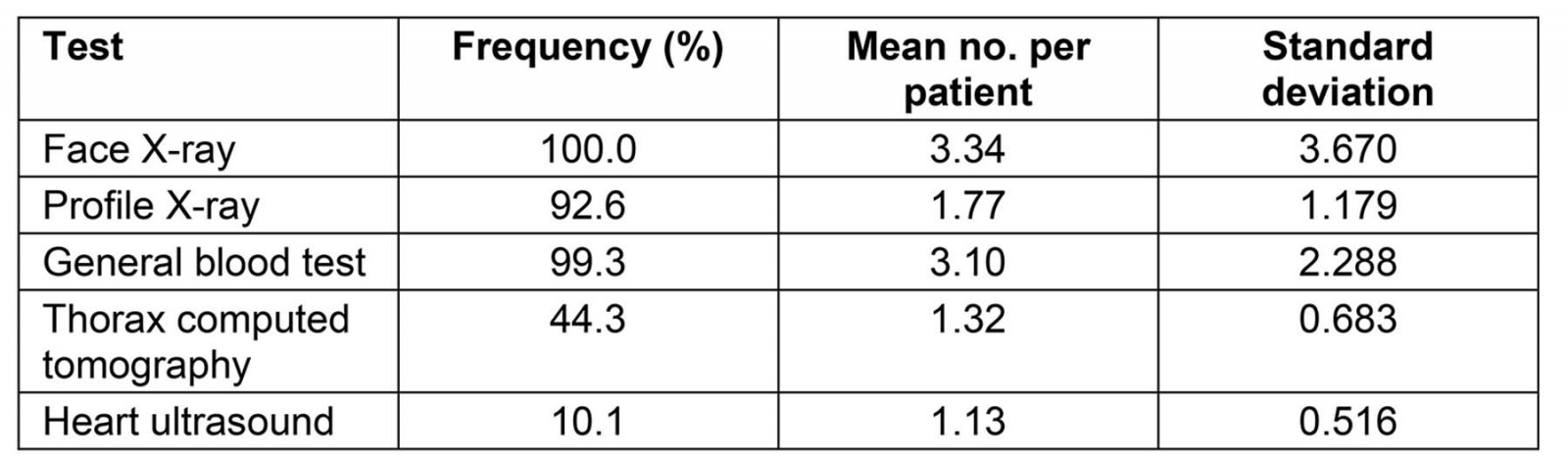
Table 3: Cost per patient and cost distribution per category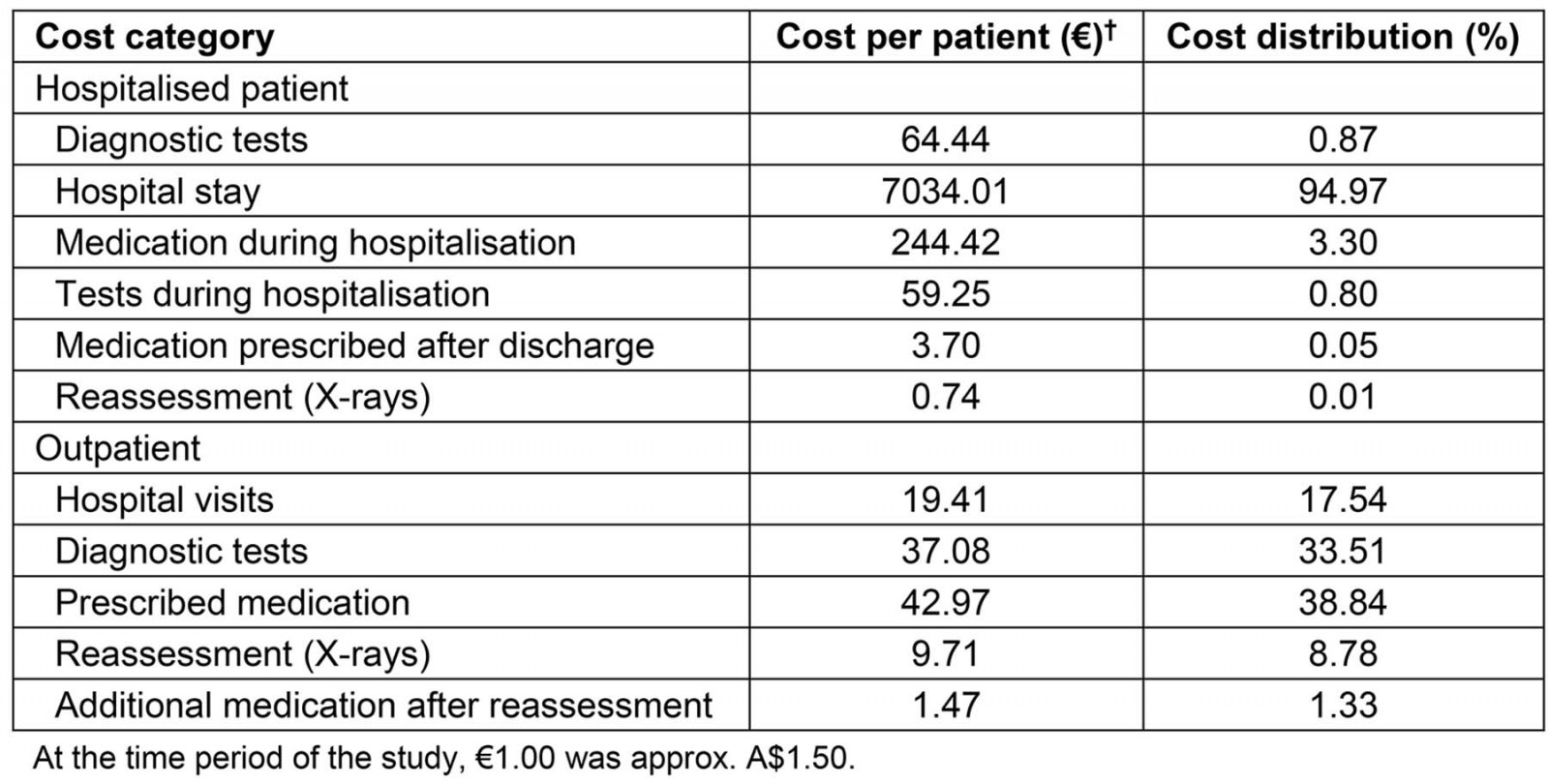
Table 4: Study regression models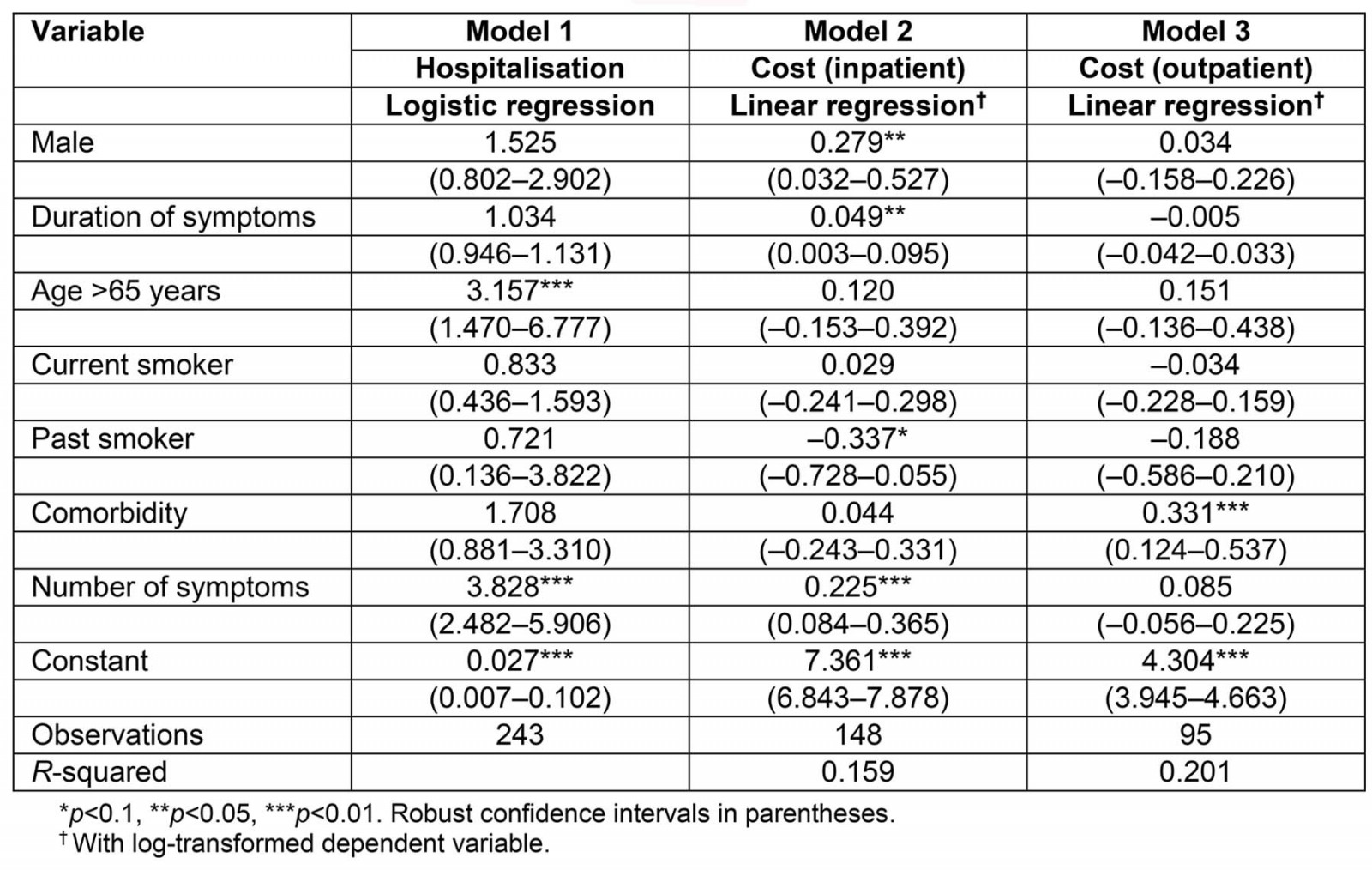
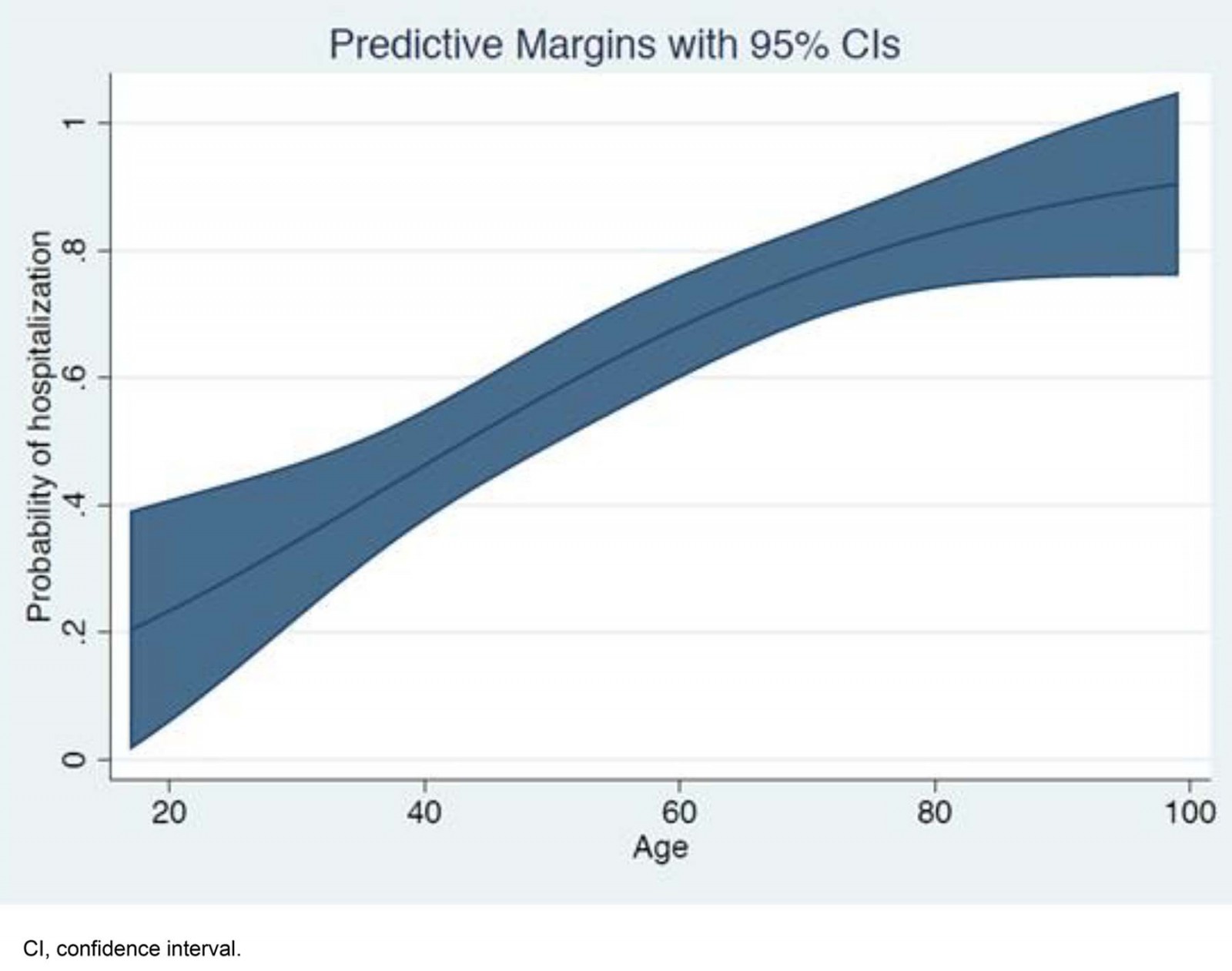 Figure 1: Predicted probability of hospitalisation, by age.
Figure 1: Predicted probability of hospitalisation, by age.
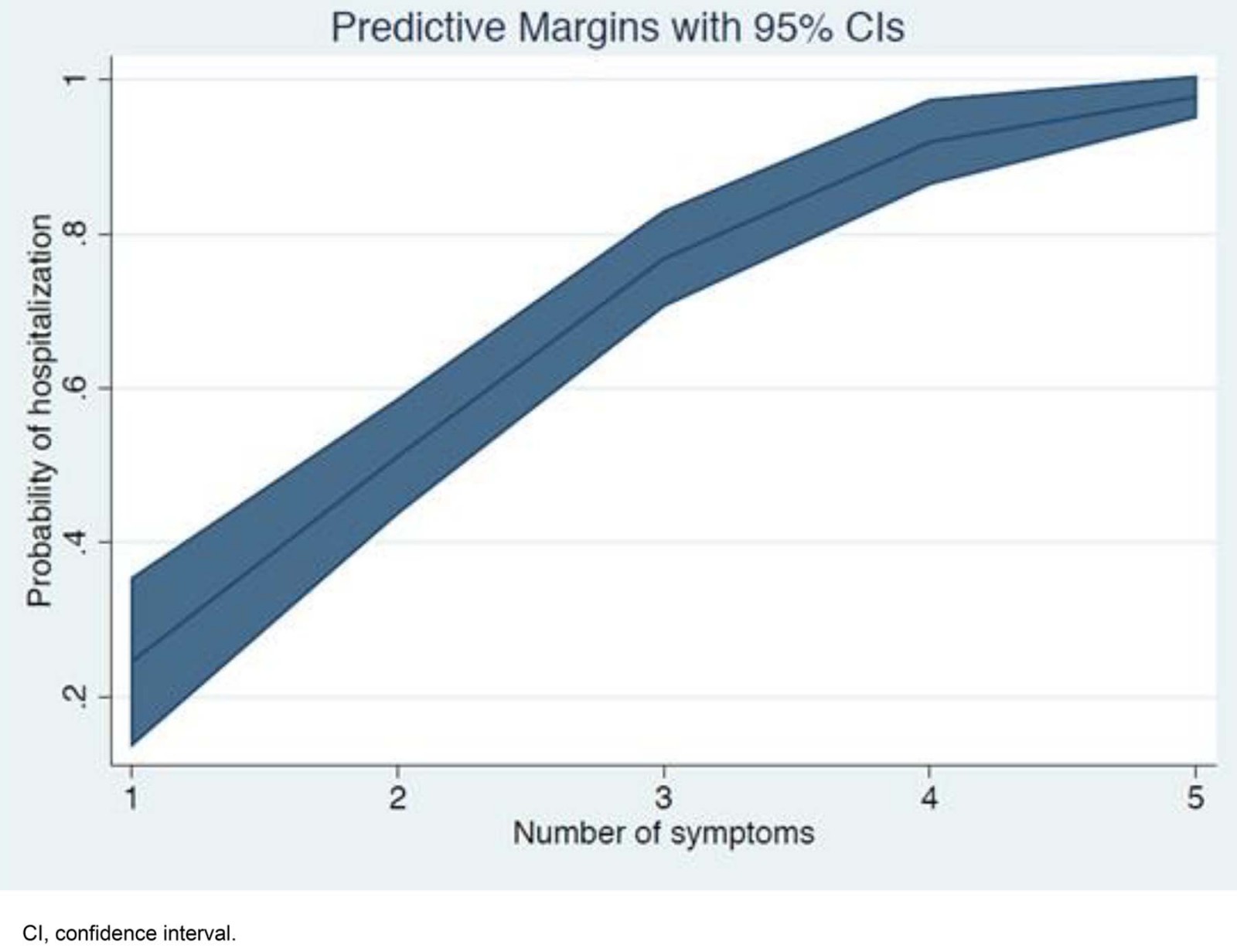 Figure 2: Predicted probability of hospitalisation, by number of symptoms.
Figure 2: Predicted probability of hospitalisation, by number of symptoms.
Discussion
Community acquired pneumonia is a disease associated with high clinical and economic burden. The management of CAP patients and its derived cost mainly depend on the need for hospitalisation, based on the severity of the disease.
In general, the sample characteristics of this analysis (eg respondents’ age, smoking status and comorbidities) are similar to the ones recorded in other studies11, while hospitalised individuals are generally older compared to the patients using outpatient care. In addition, all disease symptoms – and especially shortness of breath – are more frequent for hospitalised patients. Both of these findings are supported by the regression model for hospitalisation, which is potentially indicative of the reasoning behind physicians’ decisions about whether patients are admitted for hospitalisation or not.
As already mentioned, diagnostic tests were found to be generally performed more frequently for hospitalised patients. This finding can be potentially attributed to their clinical condition at the time of hospital visit and to their older age. Nevertheless, all patients were submitted to face X-ray and general blood test, which is the standard clinical practice for the diagnosis of pneumonia and reported in previous research19. A potential interpretation for the high rate of hospital admissions within the sample potentially relates to the fact that patients quite significantly delayed their visit to the hospital. A significant mean duration (7 days) of symptoms before hospital admission has been also observed in a relevant previous study20.
The analysis for the two patient subgroups demonstrates significant differences between outpatients and inpatients both in clinical and economic terms. Regarding outpatients, it is clear that their treatment only includes diagnostic tests and medication – usually with the patient participating to the respective cost – while virtually the only challenge for the hospital and the treating physician is to ensure the patients’ return for reassessment of their condition and the effectiveness of the therapy.
The clinical management of hospitalised patients is more complicated as it entails various therapeutic means, due to the severity of the patients’ condition, while hospital stay is the main driving factor of the inpatient cost, especially when admission to ICU is required21. This finding is in line with previous research, as hospital stay accounts for 61.0–94.3% of the total inpatient CAP cost22-24. Apart from the economic burden, hospitalised patients are at risk of in-hospital infections, which can further worsen their condition and lead to longer duration of hospitalisation.
The mean hospitalisation duration of the present study (11.35 days) is higher than that reported by other studies in Greek settings, which have estimated mean hospitalisation durations of 715 and 9.6 days12. Nevertheless, relevant research findings in other European countries support the present findings, estimating a mean length of stay at 1219, 12.125 and 14.62 days20. Furthermore, the present study estimated a lower rate of ICU admission (8.7%) compared to a recent study where 22.7% of hospitalised CAP patients were admitted to ICU[24}, but a higher mean length of stay in ICU (16.08 days) compared to 5.1 and 7 days estimated elsewhere24,26. Given that ICU stay has been found to influence hospital costs27, it could partially explain the higher cost per patient calculated in the present study. Also, the finding that the duration and number of symptoms are positively associated with inpatient cost is expected, as they indicate a worse clinical condition, which leads to more intensive health care.
Additionally, the outpatient cost represents only a small fraction of the total CAP cost (1.47%), which aligns with other study findings14,21,28. Regarding outpatients, the main cost drivers were medication and diagnostic examinations, which is in line with previous relevant research23.
In the face of the demographic transition that is observed globally, especially in the developed world, the burden of CAP is expected to steeply increase. Respiratory infections are one of the leading causes of morbidity and mortality globally, with Streptococcus pneumoniae accounting for more deaths than all other respiratory aetiologies combined29. However, although there is a reduction of the global respiratory infection burden, improving the disease ranking (fourth in 2017 compared to third in 1990)29,30, in Greece there is an opposite development (six in 2017 compared to ninth in 1990)31,32. Bearing in mind the fact that older people often have underlying conditions, the proportion of complicated CAP patients requiring hospitalisation is also expected to increase33, unless an effective strategy against the disease is adopted.
Greece is a country with a significant proportion of the population dispersed in its rural parts, usually of higher age, as reported in the most recent national census34. Also, healthcare services are unevenly distributed across the country, as they are highly concentrated in a handful of large cities, while almost half of the country’s hospitals and healthcare professionals reside in the capital, Athens35. As a result, the rural population face obstacles in their access to healthcare services36-38. In the case of pneumonia, as well as other infections and diseases for which timely diagnosis is vital to the overall treatment and prognosis of the patient, these obstacles are most likely to cause a significant delay in seeking and/or reaching healthcare services39. This leads to a higher probability of the patient presenting with a worse clinical condition and a higher probability of hospitalisation with its accompanying costs. The results of the present study, which despite its urban setting noted a remarkably high proportion of patients requiring hospitalisation, raise concerns about how much worse the situation might be in rural parts of Greece. Although there are no data available on the residents of the sample, it has been highlighted elsewhere that the majority of rural residents in Greece prefer to travel long distances to use urban care services instead of rural ones, which suggests that a proportion of the present study sample comes from rural areas40.
In general, CAP can be prevented on a large scale with proper vaccination41. Nowadays, a few different vaccines are available, which are effective in the prevention of the disease42. The influenza and pneumococcal vaccines have been extensively studied as preventive tools against CAP occurrence. The existing findings suggest that the use of vaccines on different groups of the population, either alone or combined, can successfully reduce the incidence of the disease11,43,44 and lead to reduced hospitalisation rates and lower length of hospital stay19. Apart from clinical effectiveness, existing evidence demonstrates that vaccination against pneumonia is also cost effective, when specific population groups (eg infants and elderly) are vaccinated45-47.
Despite the wide availability of effective vaccines, their optimal use is yet to be achieved48-50, while a nationwide health survey in Greece has reported that less than 20% of the adult population is vaccinated within the recommended timeframe51. In order to achieve an adequate uptake of vaccination in Greece, the formation of an organised vaccination program is considered necessary. Given the high proportion of the population residing in rural regions, mobile units should be available to reach the remote parts of the country and especially the elderly.
Study strengths and limitations
The present study was conducted in a national referral hospital for respiratory diseases, which indicates that the study sample is quite representative of the overall population. However, the small sample size limits the external validity for generalisability of the results. Furthermore, the study does not include indirect costs, such as productivity losses, which have been identified as an important source of cost in previous research20.
Implications
Based on these study results and bearing in mind the current economic environment in Greece, it is very important for the national health system to identify and encounter avoidable cost sources. As described in the present analysis, in the case of CAP, this source is mainly identified in hospitalisation. Consequently, information for and education of the public are essential so that people are aware of the importance of vaccination against the disease, especially for vulnerable and remote groups of the population. Timely identification of CAP symptoms and prompt referral to a physician would contribute to reduction of avoidable hospitalisations. Further research on the inequalities of healthcare access and utilisation between different groups of the population would potentially reveal shortcomings of the healthcare system that should be addressed.
Conclusion
The results of the present study highlight the fact that CAP is a disease that is a significant economic burden on the Greek healthcare system, the main determinant of which is hospitalisation rates and duration. Interventions toward reducing the influence of the contributors to the incidence and probability of hospitalisation are essential from a clinical and policy perspective. Furthermore, hospitalisation rates and overall costs have been found to be associated with number and duration of symptoms.
The findings of the present study highlight the attention that should be given to high risk populations, especially the elderly, as well as those who reside in remote areas of Greece, regarding the prevention of the disease, mainly through vaccination, and access to proper and timely health services.
References
You might also be interested in:
2014 - Non-physician communities in Japan: are they still disadvantaged?
2010 - A tribute to John A J MacLeod
2009 - The changing nature of nursing work in rural and small community hospitals
