Introduction
Gestational diabetes mellitus (GDM) is a condition of pregnancy characterised by maternal glucose intolerance and hyperglycaemia1. GDM affects approximately 10–15% of pregnancies in Australia2,3 and occurs as a result of hormonal changes in pregnancy that alter glucose metabolism and decrease insulin sensitivity1. Poorly controlled GDM is associated with increased risk of adverse perinatal outcomes such as macrosomia and large for gestational age, perinatal mortality, pre-eclampsia and caesarean birth4.
Management of GDM aims to optimise blood glucose levels through frequent engagement with a multidisciplinary service facilitating diabetes education, nutritional and activity recommendations and medical management such as hypoglycaemic agents5. Consultations for GDM occur in addition to standard antenatal care consultations. Patients in rural and regional settings, including women with GDM, incur challenges of access to health services due to their geographical location6. Telehealth offers potential to mitigate these issues by increasing access to healthcare services and reducing the cost incurred for rural and regional communities7,8.
Telehealth may be defined as ‘telecommunication techniques for the purpose of providing telemedicine, medical education, and health education over a distance’9. Telehealth services may be internet-based, telephone-based or conducted by videoconferencing or a variety of modes9-12. A previous randomised controlled trial (teleGDM) in an urban setting demonstrated that telehealth significantly reduced time to achieve glycaemic targets in women with insulin-managed GDM, as demonstrated by stabilisation of insulin dosage13. TeleGDM utilised an internet-based portal to allow data sharing and communication between pregnant women with GDM and clinicians, enabling timely advice and feedback for optimal GDM care and management(13}. Quality and safety of care in this trial were not compromised, and were consistent with other literature14,15. A recent study targeting affected women’s education in GDM management showed similar clinical outcomes but superior engagement when telehealth was compared with routine care16. Despite this, the views of women with GDM on telehealth modes of care, as well as applicability of these models in rural/regional settings, is lacking15,17. A recent systematic review found an inadequacy of evidence concerning the acceptability and feasibility of telehealth for GDM management from the perspective of clinical staff17.
Stakeholder engagement and involvement is an important ingredient in the design and production of health service improvements (co-decision)18. Prior to adapting and offering this service to a regional setting, it was important to determine the proportion of women with GDM who would be suited to provision of GDM care through telehealth. Consideration of the views of women and health service staff is important in the design of an appropriate intervention, as well as identification of barriers and enablers for women and clinicians in accessing telehealth services. This study aimed to examine clinical and demographic profiles of women with GDM accessing care through a regional health service. Through semi-structured interviews, the study aimed to contribute to the evidence on the views of women with GDM and health service staff regarding telehealth in GDM management. The study also aimed to solicit views on feasible and acceptable modalities and types of telehealth ventures for women and clinicians in a rural/regional setting and uncover the potential barriers and enablers for stakeholders in accessing telehealth.
Methods
The study setting was a tertiary teaching hospital providing care to a large rural and regional geographical area in regional Victoria, Australia. The GDM clinic is embedded within the outpatient women’s health service. Women with GDM are referred into the service from outpatient services or general practices following a positive oral glucose tolerance test. The clinic is staffed by a credentialled diabetes educator registered nurses, a dietician and an endocrinologist. The level of a woman’s glycaemic control dictates the frequency of appointments and care continues in the clinic until birth. Multidisciplinary input is also provided by midwives, obstetricians and lactation consultants.
A mixed-methods approach incorporating a clinical record audit and semi-structured interviews was utilised. The audit included medical records data of the GDM clinic for a 12-month period between October 2016 and 2017.
The authors aimed to recruit a convenience sample of up to 15 pregnant women with GDM, aged 18 years or more, who were current patients of the GDM clinic between November 2017 and January 2018; and up to 10 clinical staff and personnel from the health service’s IT department. Women meeting the inclusion criteria (GDM diagnosed by oral glucose tolerance test) were approached by clinic staff and, if they were interested in participating, were directed to a member of the research team and invited to participate. Written consent was obtained from participants prior to each interview.
Semi-structured, one-on-one interviews were conducted in person or over the phone depending on each interviewee’s preference. Duration of the interviews was between 15 and 45 minutes and interview questions were guided by a schedule for clinician, women and IT support staff respectively. Interviews were audiorecorded and transcribed verbatim.
The interviewer and a second team member then performed the analysis of the transcripts, managed through NVivo v11 (QRS International; https://www.qsrinternational.com/nvivo-qualitative-data-analysis-software/home). The transcripts were analysed to identify codes and themes that aligned with the Evaluation Framework for Telehealth Implementation11, as well as identifying any emerging themes not currently captured within the framework. The framework consists of four primary dimensions: patient control, clinician quality of care, organisation sustainability and technology capability.
Ethics approval
This study had ethics approval from Bendigo Health Human Research Ethics Committee (LNR/17/BHCG/38) and was endorsed by the College Human Ethics Subcommittee CHESC, La Trobe University.
Results
Records for 205 women with GDM from the previous 12 months were audited. Clinical and demographic data are presented in Table 1.
Interviews were conducted with nine patients, three clinicians and two IT staff. Characteristics of the interviewees are presented in Table 2. Interview patients were demographically similar to the GDM population identified in the audit.
Major themes resulting from semi-structured interviews were aligned with the telehealth evaluation framework dimension11. Due to privacy, random pseudonyms were assigned to women being interviewed and used when quoting.
Table 1: Clinical and demographic profile of women with gestational diabetes mellitus in health service catchment (n=205)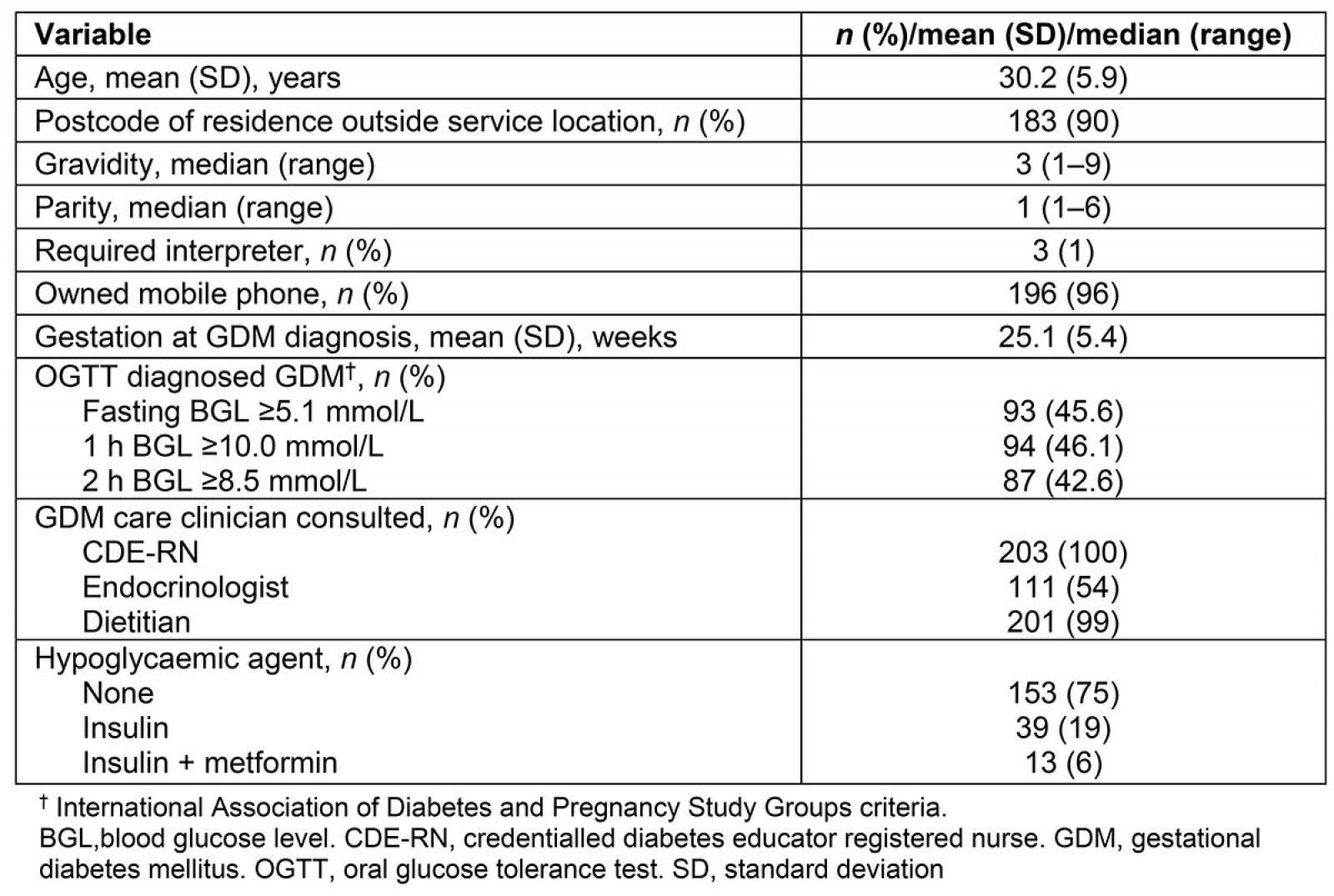
Table 2 Interviewee characteristics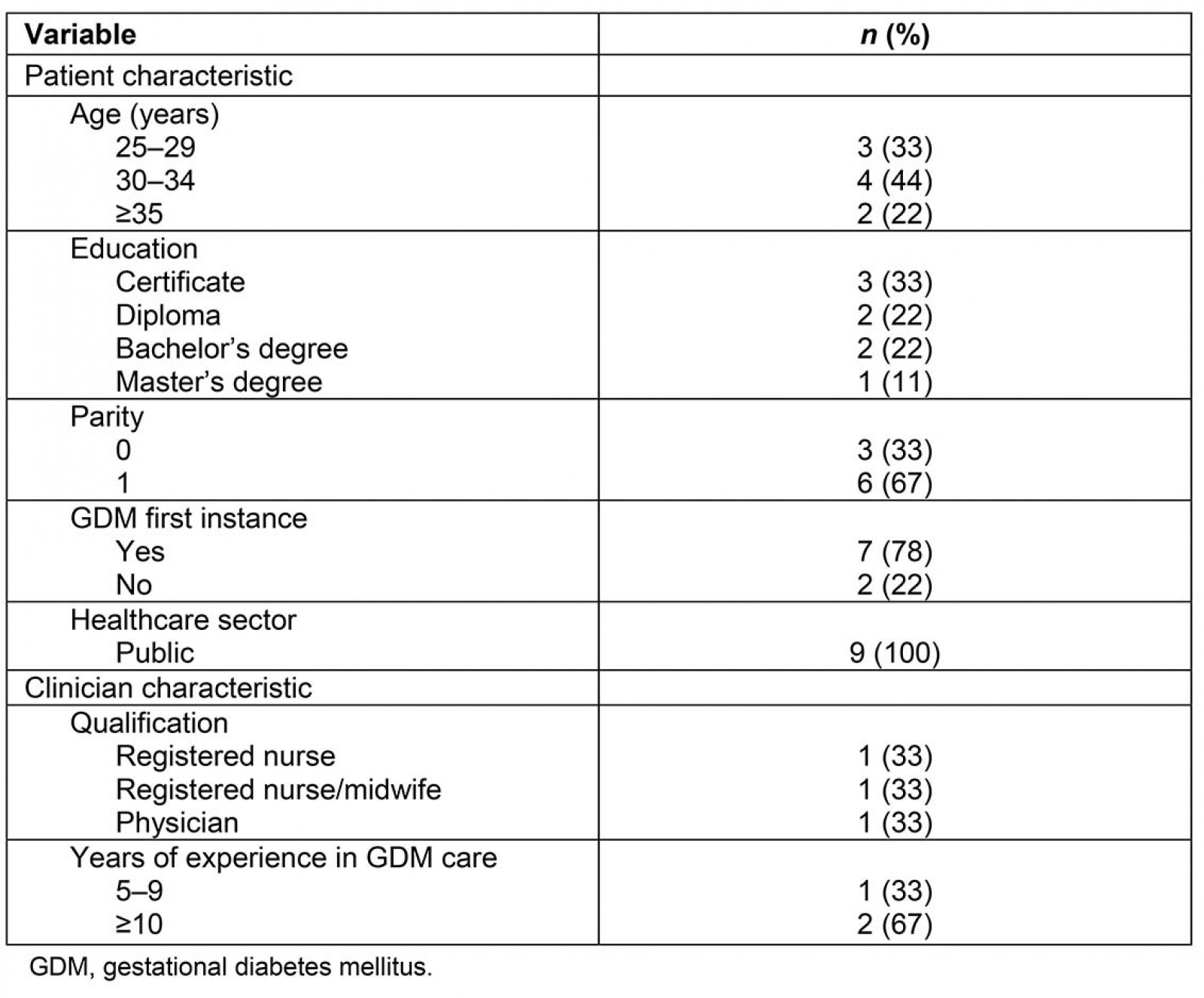
Patient control – Accessibility, continuity and responsiveness of gestational diabetes mellitus service
Women outlined the negative impacts of physically attending the GDM clinic. Travel time and time associated with attendance for care were concerning for many (56%). Most of the women reported more than 30 minutes travel time to attend the GDM clinic, including three women who travelled for more than 2 hours. Most women were required to attend fortnightly, and appointment durations was 5–60 minutes depending on the complexity of care required. Clinicians also raised concerns about lengthy travel times and were aware of some women travelling several hours to access care.
Attending the GDM clinic in person required many women to take time off work (56%). The incurred costs of attending, such as loss of income, travel and parking costs, was a concern for the majority (67%). This was compounded when they attended appointments that did not result in new information or change of GDM care (44%), or when GDM appointments were not scheduled around routine antenatal appointments (33%).
… probably the time off work. My husband … he has to take the day off work, and he is a contractor, so he is losing a lot of money. (patient 1)
I had to shuffle around work or find someone to look after my son. It took [me] maybe half an hour to go in, and the appointment was only 5 minutes. It’s hard to find a car park, and the parking is quite expensive as well. (patient 9)
Clinicians reported that the GDM clinic was operating at capacity and impacting on follow-up care. Up to 40 patients would be seen each day, often with appointments with several practitioners, and there was no ability to accommodate increased demands.
We have adjusted [appointment] numbers, or I’ve changed the follow up arrangements for someone specifically because we didn’t have availability in a clinic. (clinician 2)
Telehealth was viewed positively by women and staff as a possible solution to the barriers and impacts of attending the GDM clinic in person. Many women were supportive of a telehealth venture in place of some face-to-face consultations, although some women outlined a preference for face-to-face appointments. Some highlighted that the inconvenience of standard maternity appointments not being aligned with GDM appointments could be reduced if some GDM consultations were completed by telehealth.
If there are [physical assessment] needs, like check the baby, check the bump, then I need to attend in person, but if they’re not going to touch me … they’re just going to read my reports or share something with me, it’s better [completed by telehealth]. (patient 7)
Aspects of GDM care considered appropriate for telehealth included endocrinology consults, diabetes education and dietetics, and any care not requiring a physical assessment in person (such as blood pressure measurement, antenatal examinations) capable of provision by a telehealth platform.
… if there is no change or they don't need to tell you anything and it’s just to check in, it’s [telehealth] important. (patient 2)
Four women reported they were already emailing and receiving feedback on blood glucose levels to credentialled diabetes educator registered nurses fortnightly. Clinicians reported most women would be suitable for elements of GDM care to be provided via telehealth, regardless of their proximity to the GDM clinic.
It’s just as valuable for those who live close by. They don’t want to spend all of their time trying to get to the hospital and look for parking and spend long periods waiting at hospital. (clinician 2)
Women and staff indicated potential further benefits for telehealth for GDM care. Some women indicated a desire for peer support in GDM care. They outlined that peer support in the context of current care was limited, but identified that, through telehealth ventures, this might be increased. Clinicians surmised that telehealth for GDM care could increase capacity for in-person consultations in the clinic by providing other care remotely.
Views on the type and mode of telehealth are presented in Table 3. Clinicians reported proficiency in use of all work-related technology and did not anticipate issues with capabilities in using telehealth technologies.
Most women reported a preference for at least one consultation delivered face-to-face during pregnancy. Many acknowledged that if this was the initial consultation after GDM diagnosis then they would be happy for subsequent GDM care to be delivered via telehealth, unless physical assessments were required. An IT staff member summarised the capabilities of telehealth in enabling access to healthcare.
It’s just really if you get back to why we’re in health ... patient needs and access, trying to make it as easy as possible for them. I would really like the continuation of Telehealth [due to ease] of use and access, rather than it being difficult and them having a bad experience and then potentially not wanting to do it again. (IT staff 1)
Table 3: Preferred modes and type of gestational diabetes mellitus care for telehealth delivery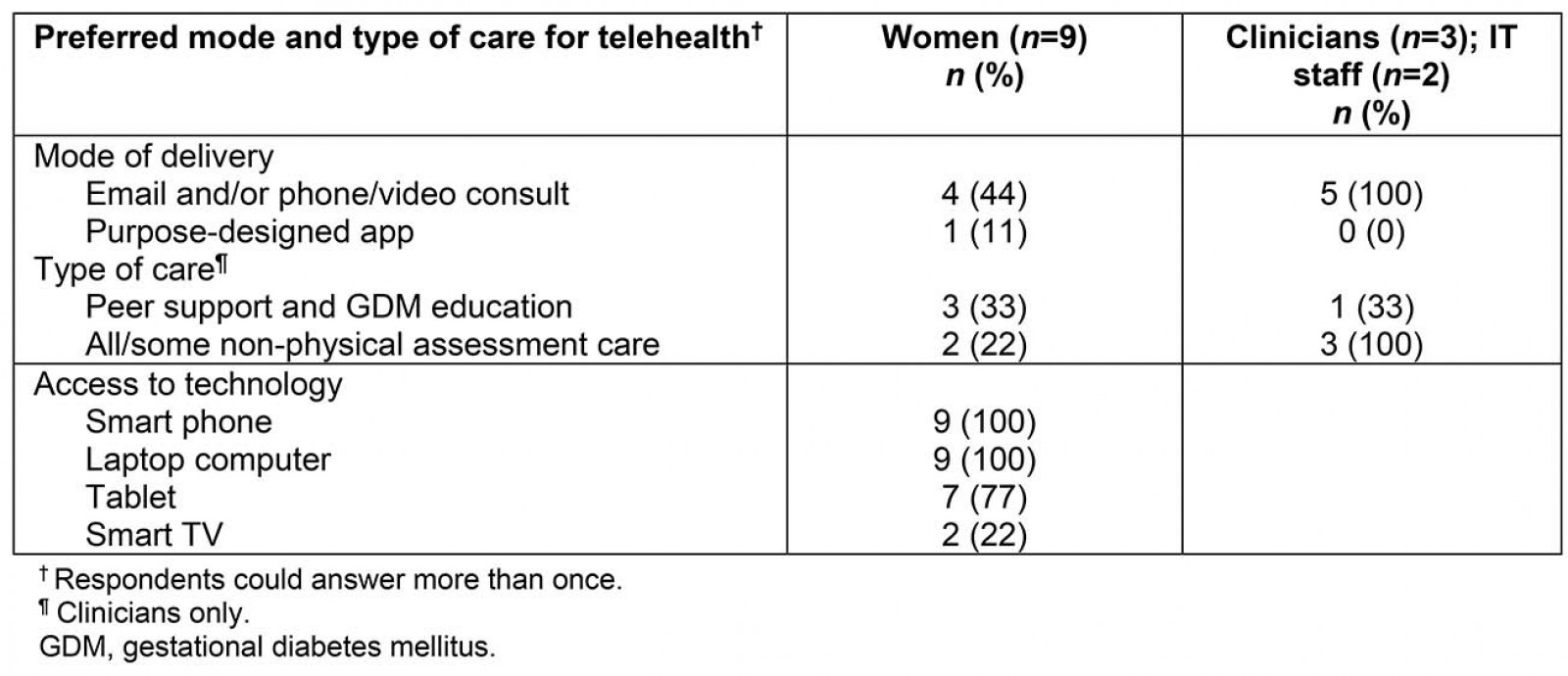
Clinical quality of care
Most women were not concerned that telehealth would affect the clinician–client relationship. Continuity of care, regardless of mode of care provision, was considered essential by some women, given its ability to promote a strong relationship between health practitioner and patient. One woman indicated a preference for continuity of care regardless of mode of care delivery.
You speak to a lot of people; I find that difficult. I’ve never once had the same (clinician). (patient 4)
Telehealth was not considered to impact adversely on quality of care; in fact, several women hypothesised that telehealth alone may improve glycaemic control.
It’s the convenience of doing it inside the house … one thing is that [at the hospital] it’s too long I felt … I felt sleepy, I felt hungry. I have to monitor my blood sugar every two hours after eating and then fasting, I [can’t] eat anytime I want. (patient 6)
Women reported that they would measure success of a telehealth initiative through achievement of glycaemic control, cost and time to attend care, while clinicians reported that patient satisfaction levels, care compliance and achievement of key performance indicators would be important performance feedback measures.
Technology capability
Clinicians and IT staff all considered their organisation and current infrastructure to be highly capable of delivering telehealth to support GDM care, with several projects and telehealth initiatives already operating within the hospital.
We actually already have a lot of Telehealth situations in place where we connect to smaller or more rurally located areas to assist with expertise in certain [clinical] areas … we’ve got pretty good infrastructure. (IT staff 1)
IT staff suggested that a GDM telehealth initiative would not greatly impact IT workload but outlined that early engagement with IT services was essential for successful design and implementation of the initiative.
Concerns were raised about the technical aspects of telehealth. Women worried about technologies that may be incompatible with their personal devices or incur additional costs as a result of obtaining or running the required technology, such as for those with limited data or a prepaid mobile service. Some women expressed a need for a telehealth initiative to be responsive for immediate feedback and advice to alleviate potential health impacts.
There was a time when I was having a problem with my machine and I didn’t hear back from them so there were a few days [when] I haven’t been able to test. [By the time] they got back to me I had got the machine fixed. I also tried to call but they weren’t available … if they had less appointments, they [could be more responsive]. (patient 1)
Clinicians reported that telehealth care would need to complement face-to-face care, due to the need to physically assess women, validate information provided via telehealth, and to ensure women had understood the care and information provided to them. They also highlighted the potential for technical issues that may interrupt delivery of health care, such as women’s access to technology, costs to run and proficiency with required technology.
We have some women who have got quite a low socioeconomic status, most of them still have phones … but not all have [mobile] data. (clinician 1)
We think that people are IT savvy and they’re all on their screens but at the end of the day, some of them don’t actually have credit to even look at a website or download a piece of information … that would concern me if they have to rely on their own devices. (clinician 3)
Organisational sustainability
IT staff reported previous challenges with telehealth initiatives included staff resistance and inadequate coordination of services. Telehealth services and projects were growing but there was insufficient governance to oversee these initiatives.
… at the moment there are a lot of activities and projects happening. However, I suppose each department at this stage is sort of responsible for their own upkeep and governance and clinical governance and we have highlighted that as a concern. (IT staff 2)
Staff indicated these issues could be addressed through creation of a coordinator role, recruiting staff telehealth champions to engage other staff, and identifying the most suited health service programs in which to embed telehealth services.
Clinicians expressed concerns about an increase in workload, such as the potential for an increased volume of emails and completing training around use of telehealth platforms. Clinicians highlighted a need to develop standardised criteria to guide patient suitability for telehealth for GDM care, and suggested patients requiring an interpreter, or who had poor prior attendance of healthcare services, may be unsuitable for telehealth due to the potential impact on engagement with healthcare services.
My concern would be that they might drop through the system or we might not see them for a long period of time. (clinician 2)
Coordination and scheduling of telehealth care around other appointments adds a further level of complexity to the clinic workload, which was summarised by one of the clinicians.
To add … complexity, you’ve got to go into a room, you’re going to be teleconferencing through there and coordinating the timing of all that would be difficult … the [telehealth] clinician would take priority over the ones you’ve got on seats, which I think is greatly unfair. Another obstacle is having that reflected in admin time … and jobs behind the scene. (clinician 3)
Discussion
This study involved a clinical audit of women accessing the GDM service at a large regional hospital and explored the feasibility and acceptability of a telehealth venture to enhance management of GDM from the perspectives of women with GDM and health service staff. The clinical audit demonstrated that 75% of women attending the GDM clinic were not managed with hypoglycaemic agents, and are a potential target cohort for GDM care via telehealth because of less intensive management regimes associated with diet-controlled GDM19. However, all women with GDM, including those requiring hypoglycaemic agents, would arguably benefit from a telehealth service if it reduced costs and time associated with attending the clinic in person in addition to enhanced clinical outcomes.
The present study provides a novel insight into the perspectives of women with GDM on telemedicine for GDM care, which has been limited in previous research15,17. Through semi-structured interviews, the authors found that women and organisational staff were receptive to telehealth for GDM management. Both parties identified many potential benefits and enablers of telehealth for enhanced GDM care, including possibility for reduced expenses and time required to attend care in person. Additional advantages would be gained if telehealth increased the ability of the service to provide continuity of care as this was a highly desirable aspect of care for women and clinicians. Women in this study also recognised that peer support, considered lacking in current care provision, may be increased through telehealth via specifically designed ventures.
GDM consultations by telehealth may increase the capacity of the organisation to meet service demands and conduct more urgent and complex consultations within the GDM clinic. The present study’s results are consistent with the findings of a recent systematic review demonstrating that telemedicine in GDM management can reduce the number of consultations, increase clinician efficiency and improve quality of life for pregnant women, resulting in time and cost savings17. Telemedicine in GDM management may also contribute to improved psychological measures in relation to care provision. A recent small study in France explored women and health professionals’ experiences in using a purpose-designed mobile app for GDM care20. Women felt reassured and empowered in their GDM management through the app, and it contributed to reduced anxiety and stress relating to diabetes management20.
Previous research has demonstrated further clinical benefits of telehealth for diabetes care, such as improvements in glycated haemoglobin (HbA1c)15, earlier optimisation of glycaemic control and fewer insulin dosage titrations13, without impacting on quality or safety of care. The majority of women in the present study did not consider that telehealth would impact on their relationship with clinicians or the quality or safety of care. This is in contrast with the systematic review by Fantinelli et al, which found that some studies reported a detrimental effect of a decrease in face-to-face contact between women and clinicians17.
Barriers to telehealth services were also identified by women and staff, such as the potential for financial disadvantage in accessing the service, and level of technological literacy. Clinical staff highlighted that a proportion of women accessing the service may not have required levels of digital skills to engage in certain telehealth initiatives. Likewise, many women have limited mobile data access and could be unable to afford certain technologies. This emphasises a need for careful consideration of appropriate telehealth service designs that does not disadvantage women, and rather facilitates engagement and positive self-management choices. These factors may in turn amplify the positive impacts of telehealth on clinical outcomes in GDM management.
Clinical and IT support staff recognised that a telehealth coordination role was desirable in streamlining service provision and managing the workload associated with implementation and maintenance of telehealth ventures. Staff workload, governance, acceptability and cost associated with implementing and coordinating these services were frequently raised concerns, consistent with other literature on this topic21, although a previous trial has demonstrated no impact of telehealth on service provider costs13.
Whilst this study contributes important findings of the perceptions of pregnant women with GDM, clinical staff and IT support staff regarding telemedicine for GDM care, it is not without limitations. The small number of participants and certain characteristics may limit generalisability of the findings beyond these particular cohorts. However, a relative strength of the study is the inclusion of a diverse but small group of pregnant women capturing a mix of age groups, education levels and primiparous and multiparous women.
Conclusion
This study addresses an important gap in the evidence by providing the views of pregnant women with GDM, and clinical/IT staff on a potential telehealth venture in a rural/regional setting. A telehealth-based GDM service offers choice and potentially important benefits to women with GDM, such as improving equity and access to care, earlier achievement of glycaemic control, increased peer support and mitigation of perceived adverse impacts of attending care in person. Telehealth ventures can assist healthcare services to increase capacity and meet demand and may improve consumer satisfaction with care through provision of continuity of care. Balancing these benefits against the cost, accessibility and ease of use of telehealth initiatives for both women and staff is essential. Similarly, adequate infrastructure within organisations to support such a venture is crucial for their success.
