full article:
Introduction
Worldwide, over a billion people suffer from some degree of impaired vision and blindness, 80% of which is considered to be avoidable1. According to global estimates from 2018, 39 million people are blind and 285 million are at risk of severe vision loss, with Sub-Saharan Africa having the highest levels of blindness due to a high prevalence of uncorrected refractive errors (myopia, hyperopia and presbyopia)2. Uncorrected refractive errors are one of the most common ocular problems and a major cause of visual impairment and visual loss worldwide2. Addressing issues of vision impairment is essential for achieving overall health and wellbeing, as having diminished eyesight can negatively impact individuals in all aspects of their lives.
While many types of vision impairment are either preventable or manageable through simple refractive error corrections and, for some cases surgeries, many health systems around the globe suffer from deficiencies on both the supply side and demand side that contribute the global burden of vision impairment3. On the supply side, there is a shortage of both skilled personnel and an inadequate distribution of personnel within each country. Other important supply-side constraints for vision care include infrastructure and technology development.
On the demand side, data show that access to vision care in many parts of the globe is extremely low due to issues of accessibility, awareness, and affordability. An important factor that hinders access and utilization of eyecare services, particularly in low-income countries, is accessibility of eyecare services, primarily in remote areas4. Moreover, affordability continues to be one of the leading barriers for the uptake of eyecare services, especially among individuals lacking insurance coverage and those living in rural areas5. Data from 2016 have shown that more than 2.5 billion people in the world need eyeglasses due to refractive errors and, of this number, 1.1 billion (almost half of them) lack access to vision care3. Awareness is another key determinant for accessing eye care: an individual has to be aware of a service in order to access those services. Brise and de Leeuw (2016) highlight three aspects of awareness that influence if and how a patient accesses eye care: service awareness, eyecare insurance awareness and awareness about the importance of eye care6. Strengthening demand for vision care by addressing accessibility and affordability issues can increase access to eyecare services and vision centers.
A number of global initiatives have focused on eye care over the past decade. International organizations such as the WHO and the International Agency for the Prevention of Blindness jointly developed a global initiative to eliminate avoidable blindness by 20207,8. These initiatives identified three major components to achieve the Vision 2020 Right to Sight: specific disease control, human resource development and infrastructure, and appropriate technology development. These three initiatives focus on key supply-side constraints. Most recently, the WHO published World report on vision, which promotes a systematic and integrated approach to vision care, embracing both the supply-side and demand-side investments in vision care to enhance eyecare services and utilization1,9. The same report notes that rural communities experience both higher prevalence of vision conditions and greater barriers to access than urban areas9.
The Gambia is a small country located on the west coast of Africa with a population of 1.9 million people10, with 50% living in rural areas. The Gambia, like many other African countries, is still struggling to address persistent health system challenges. According to the WHO report of 20141, non-communicable diseases are estimated to account for 32% of all deaths. Among the poorest countries in the world, The Gambia is ranked 173 out of 188 on the Human Development Index (2016)11, with a third of the population living under the international poverty line of US$1.25/day and two-thirds below US$2.50 per day. According to the International Agency for the Prevention of Blindness, only four optometrists served the entire country in 2014, mostly based in what is considered the more urban area12. Data show that although one in every three Gambians need refractive error correction, only half of them are aware they have a vision problem. Due to their level of poverty, the cost of a pair of eyeglasses is considered prohibitive3.
This article uses a framework developed by van Olmen et al (2012)13 that utilizes and combines several different health system frameworks, including the WHO building blocks framework, to think broadly about strengthening health systems. This article adapts Olmen’s framework to add, as part of service delivery, a focus on awareness, accessibility and affordability through a public–private pilot partnership in order to achieve improved vision care and vision outcomes. The framework is then utilized and applied to a vision program that has been implemented through a joint collaboration between non-profit organization OneSight and the Government of The Gambia3. The framework and study results from The Gambia are used to provide an example, from a particular country context, of a public–private pilot partnership that can improve vision care for all.
Methods
This study used three main methods. First, a desk review was conducted to understand key health system frameworks and which ones were most appropriate for vision care. Based on this review, a framework presented and used by van Olmen et al13 was enhanced with several key system components. Second, key informant interviews were conducted with OneSight staff on aspects of vision care implementation in The Gambia and the information was incorporated into the results section. Third, several databases were analyzed to provide qualitative, summary data on the vision care situation in The Gambia. Several data points were extracted from a 2017 household questionnaire that was conducted in The Gambia in coordination with the University of Gambia. The survey collected data from 3574 households with 20 608 members across seven administrative regions in The Gambia. The questionnaire gathered socioeconomic information on the households, as well as the following vision care areas: refractive errors prevalence and access, awareness, accessibility, and affordability of eyecare services. The following variables were extracted and analyzed from the OneSight Household Survey14 (2017):
- refractive error prevalence – percentage of people in a household self-reporting a refractive error (myopia, hyperopia, and presbyopia)
- access – how many people in the household reported having access to a formal eyecare center
- awareness – having existing knowledge and information on eye healthcare services and service providers
- accessibility – distance from the household or village to the formal eyecare center
- affordability – how the price of eyecare services related to individual ability to pay and willingness to pay for that service.
In addition, OneSight provided data on human resources, types of health workers that are trained to work in vision centers, including senior ophthalmic medical assistants, nurses, optometric technicians, community ophthalmic nurses, and Diploma in Ophthalmic nurses, as well as the financial records from one vision center. All Gambian Dalsi were converted to US dollars using the conversion factor from the average over four quarters in 2017 from XE currency exchange of 46 GMD to 1 USD15.
The following framework developed by van Olmen et al (2012) was used to analyze the system investments made in The Gambia to achieve improved vision care and vision outcomes13. That study considered organization and health services delivery as important elements for the framework, which also included governance and leadership as well as dynamic interactions with the population and other stakeholders. The framework combined the WHO building blocks (leadership/governance, resources, and access) with several key components of the WHO’s Vision 2020 framework7, including workforce development and vision financing. A key part of the framework added by the authors to describe the context for vision care in The Gambia was the public–private pilot partnership that has been part of the planning for vision care in The Gambia. Figure 1 shows the framework used in the analysis that follows. This figure shows one of the main components of the framework included leadership and governance, which encompassed policymaking, regulation, and coordination. The second component focused on the key resources for vision care including:
- human resources for eye health services, including all skilled ophthalmologists, proportionally distributed in both rural and urban areas
- financial resources for eye care (donor and internally generated from the sale of eyeglasses)
- infrastructure and technology, which would include equipment and supplies for visual impairment diagnosis, lenses and frames for eyeglasses, and reading charts for myopia and hyperopia patients.
The final component addressed issues of accessibility, affordability, and awareness, which includes knowledge of vision care. As shown in Figure 1, the organization encompasses all three pieces of the system and embraces a public–private pilot partnership for delivery of care. The box on the far right of Figure 1 suggests that if the three boxes on the left were aligned there would be improvement of vision care and vision outcomes measured through a reduction in avoidable blindness.
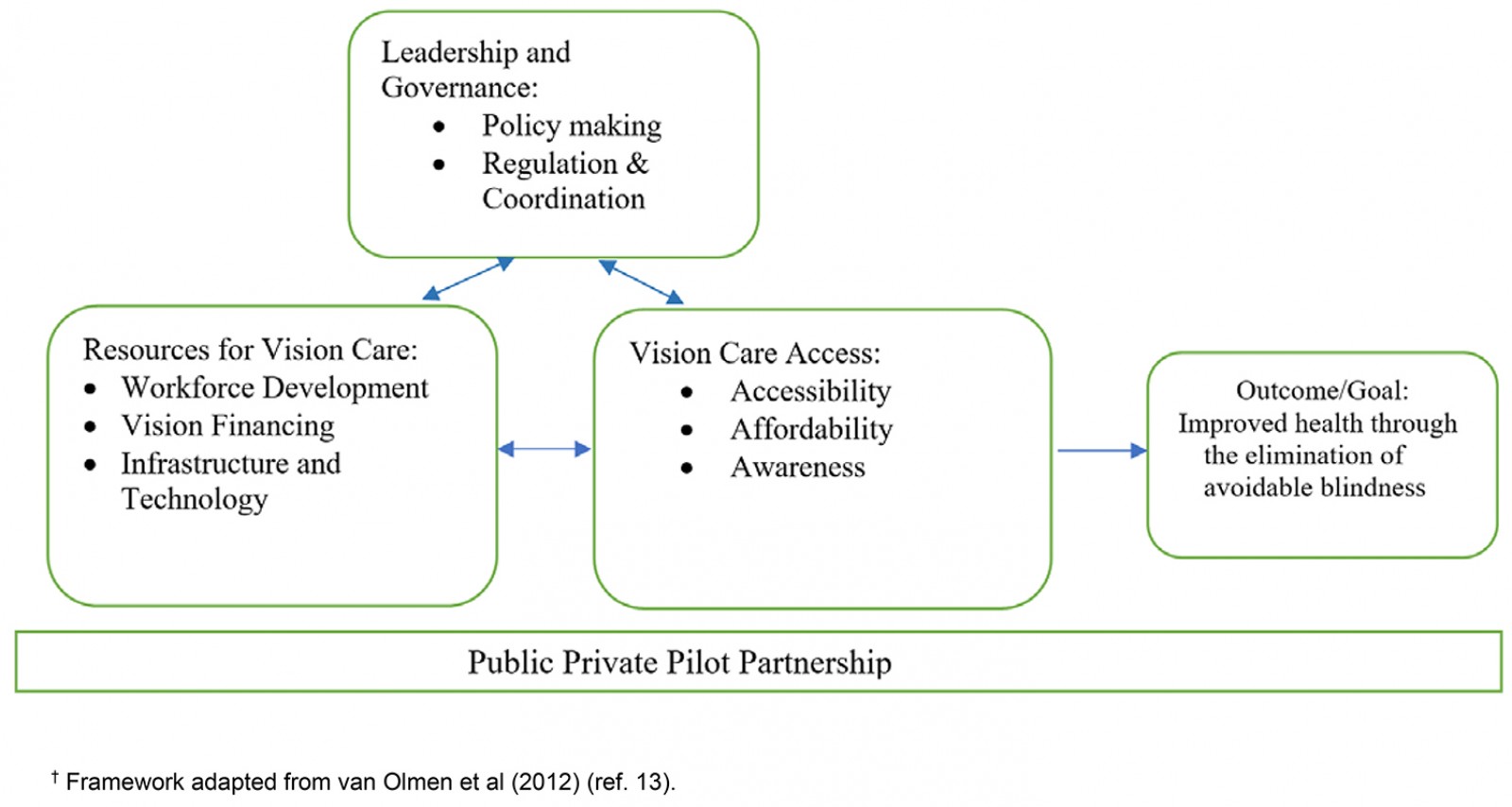 Figure 1: The health system framework for vision care13.†
Figure 1: The health system framework for vision care13.†
The results below use The Gambia as an example to present the key components of the framework. Applying the above framework in other countries would involve understanding their varying cultural, political, and environmental contexts.
Ethics approval
Ethics approval was granted by Brandeis University’s Institutional Review Board, which deemed the research exempt in accordance with 45 CFR 46.101(b) under IRB Protocol #19099R.
Results
Public–private pilot partnership for providing access to vision care in The Gambia
Vision care in The Gambia and each component of the framework presented in Figure 1 is supported through a public–private pilot partnership with OneSight and the Government of The Gambia that is driven to achieve sustainability. The organization believes sustainable infrastructure is essential to empowering communities for long-term success in meeting their goals. In order to achieve these goals and improve implementation on the ground, OneSight has a country office in The Gambia. This office works closely with local governments, health departments, school districts, and ophthalmic partners, equipping them to run vision centers in their own communities. OneSight defines sustainability in terms of financial stability and social-behavioral change for all its stakeholders: permanent government-owned vision care centers track financial stability by utilizing a true profit and loss report, companies offer products at true cost, skilled volunteers empower local staff through training, and patients pay an affordable price determined by the local market. Central manufacturing and supply chains support local demand for clinic supplies and eyeglasses.
Leadership and governance
Effective leadership and governance ensure the creation of strategic policy, framework and effective oversight of coalition building in healthcare services16. In addition, leadership and governance incorporate policymaking processes, regulations, and coordination to ensure there is equality and equity in healthcare services.
Policymaking
In responding to the WHO’s Vision 2020 global declaration17 aimed to eliminate avoidable blindness in all ages by 2020, the Government of The Gambia, like those in many other African countries, launched a national eyecare program, now known as the National Eye Health Program (NEHP), in 1987 following a prevalence survey of blindness and eye diseases18. The focus of the NEHP was to ensure that eyecare services were affordable, accessible, and appropriate to the Gambian population. The NEHP, working with other implementing partners such as OneSight and Sightsavers International, played key roles in the following activities: supporting government efforts and other partners for additional resources for eye healthcare services; supporting service delivery such as screening and distribution of spectacles in communities and schools; and supporting the procurement of ophthalmic equipment such as cataract surgery sets, operating microscopes, refractive kits, and visual acuity charts. One of the main objectives of the NEHP was to provide an integrated approach to reduce the national burden of blindness and low vision. The Gambia, like many other African countries, faced unmet eye care for its population; other factors that contributed to this problem have been a shortage of healthcare personnel, limited engagement from the communities, and limited support from the health systems19.
To address these challenges, in 2013 OneSight launched its first vision center in partnership with the Gambian Ministry of Health at Farafenni Hospital in the North Bank Region of The Gambia. To meet the vision needs of rest of the Gambian population, in 2014 OneSight and NEHP combined resources to set up new vision centers in Bansang in Center River Region, Kanifing in Banjul City Region, and Brikama in West Coast Region. To ensure that all parts of The Gambia had access to eyecare services, in 2015 OneSight launched two more sites in Basse and Bwiam, which provided access to eyecare services to people who live in Central and West Coast regions. The last site was opened in 2016, in Jarra Soma in Lower River Region. Two of the five vision centers, Bwiam and Jarra Soma, are very remote. Figure 2 shows a country map with the vision center locations. Prior to OneSight’s work in The Gambia, there had been effectively no vision care access in these communities.
 Figure 2: Map of The Gambia, showing vision center locations.
Figure 2: Map of The Gambia, showing vision center locations.
Coordination and regulation
To achieve effective and efficient health services programs, there must be a functional regulatory framework and coordination between the government and stakeholders. As stated in the Gambian Strategic Health Plan, the regulatory framework is guided by the Public Health Act18. In order to achieve this plan, the OneSight sustainable pilot vision care model was launched in partnership with the Ministry of Health through the NEHP. The objective of this project was to address a number of issues, such as strategies to create awareness about refractive errors, population preparedness to buy eyeglasses to correct refractive errors, and determination of affordable price for eyeglasses for those in need3.
The sustainable vision project included the following main components: the technical team, the staff within the vision centers, optical leads, marketing, and advocacy. To understand the needs of eye health services for the Gambians, the OneSight technical team visited all new vision center locations to assess the centers’ needs, including an assessment of the current available equipment, human resources, electricity supply to the eye unit, and the building space. This initial assessment was followed by a baseline survey to understand Gambians’ access and awareness levels to eye healthcare services. OneSight and NEHP pooled resources to set up the new centers after assessing these new locations. The government provided the human resources required to run the vision centers and was responsible for paying salaries and other incentives. When new facilities were constructed, OneSight and NEHP split the costs for the building and construction. OneSight financed the equipment for vision centers and the overhead costs for the first 6 months of operation3.
All the staff within the vision centers are managed by the government under the NEHP, while the optical leads consist of community volunteers, trained by volunteer doctors from around the world who work to identify basic eye conditions and make timely referrals to vision centers for further eye examinations. The marketing and advocacy team work to increase awareness of the services provided by the vision centers and all related costs to patients. Leadership personnel work with all partners, government, and the private sector to implement effective eye health in The Gambia.
Vision care resources
According to the framework outlined in Figure 1, there are three important components of vision care resources in The Gambia: workforce development, vision financing, and infrastructure and technology.
Workforce development: As shown in Table 1, 126 staff had been employed and trained through this collaboration. The vision center staff consisted of a senior ophthalmic medical assistant, a Diploma in Ophthalmic nurse, a community ophthalmic nurse, a dispensing nurse, a refractionist, and a registration nurse. All these staff were trained by OneSight’s highly skilled volunteers from the optical industry, including optometrists, lab technicians, finance specialists, and retail experts, who volunteered their time to train Gambians locally on topics related to how the vision centers operate, the sales model, and clinical protocols. The trainings were aligned with OneSight’s main objective of enhancing the capacity of government staff in vision centers to improve their performance in carrying out core roles and responsibilities. Table 1 shows the type of human resources trained and staffed in seven vision centers through the OneSight–Gambian Government collaboration over the period 2013 to 2017. The distribution of the trained personnel was across the whole country, including the two very remote rural vision centers. Of the 126 staff in The Gambia, 89 staff work in rural vision centers and were recruited and trained within the local communities around those vision centers. There has been no turnover among staff – all staff initially hired have continued to work in the vision centers. Additionally, OneSight developed an electronic data collection system. This cloud-based system allowed for remote ordering of spectacles in real time, which made the delivery of spectacles to the patient quicker, even if they were in the rural and remote areas. An IT staff member, employed by the NEHP, and the maintenance technician served all the vision centers. The addition of both these posts meant that even the most rural vision centers could be serviced quickly, ensuring that any downtime in service was limited.
Table 1: Human resources trained and staffed for seven vision centers in The Gambia, 2013–2017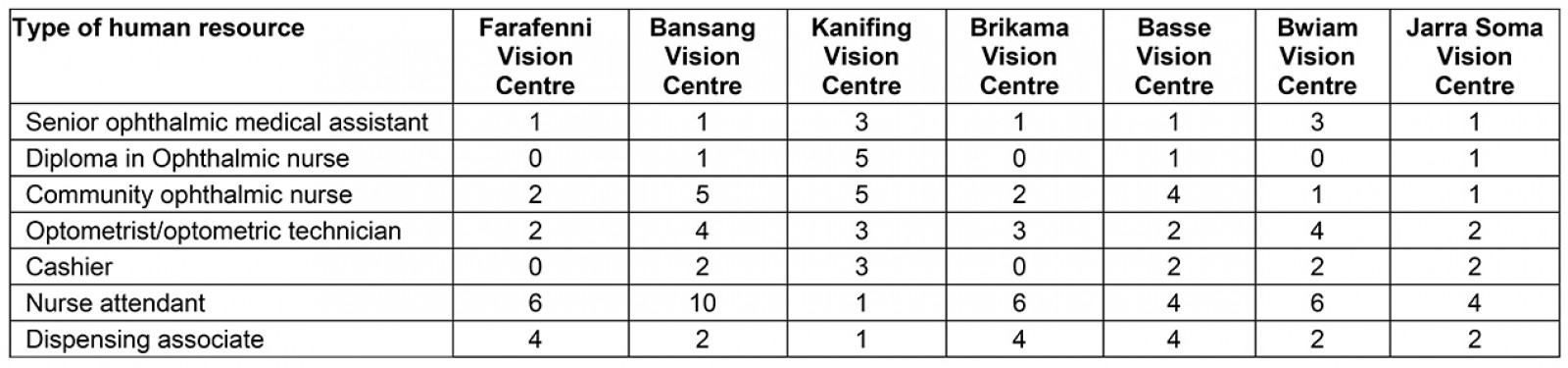
Vision financing: The financing of the vision centers is a partnership and collaboration between OneSight and The Gambia Ministry of Health. In addition to providing the start-up capital for the renovation, equipment, supplies, lenses, and frames, OneSight also pays for the training of the new healthcare workers. The most innovative and sustainable part of the financing of this partnership is that when the vision centers are operational, the sale of eyeglasses and other vision products in each vision center can fully cover the operating costs. Table 2 highlights the typical costs (in US dollars) of one of the vision centers, Kanifing Vision Centre, highlighting the revenues from the sales of glasses and accessories, and the gross margin of 41.70%. The total patients that visited this facility in 2017 for any refractive error analysis is 9480. Taking into consideration the operating expenses, the net annual income for the Kanifing Vision Centre is approximately US$11,900.
Another important financing input is the cost of the eyeglasses to the end user. Affordable eyeglasses cost at an approximate minimum price was US$3.25 and the approximate maximum price of US$8.70, not including accessories. Depending on the vision acuity of the patient, their particular diagnosis, and the price list for type of lens and eye accessories, the price of a pair of eyeglasses can vary. For example, at the time of the study, a general price for a pair of eyeglasses for a myopic eye was US$3.25; hyperopic eye was between US$2.70 to US$5.40, and for the presbyopic was US$8.70.
Regardless of the cost of a pair of eyeglasses or the specific vision diagnosis, individuals have their own willingness to pay for eyeglasses. Willingness to pay captures the amount an individual would pay for a pair of eyeglasses, taking into consideration their own assessment of their ability to pay. Figure 3 shows willingness to pay for a pair of eyeglasses in different regions, which can be compared with the prices previously listed. Figure 3 shows a considerable amount of variation in what individuals report they are willing to pay for eyeglasses. Willingness to pay for most regions is above the minimum threshold for the most basic pair of glasses (US$3.25). While the maximum amount that one is willing to pay (US$9.75) covers the cost of a basic pair of eyeglasses for most conditions, this amount may not cover more expensive glasses needed for specific conditions or desired accessories. The average general willingness to pay for glasses is US$5.07. Comparing the supply side finances and potential demand for glasses in Kanifing (9480 patients per year in 2017), the authors estimate that Kanifing Vision Centre could generate US$47,400 of revenue on the sale of glasses, which is almost exactly the actual revenue for the center for this year.
Table 2: Revenues and costs for Kanifing Vision Centre (US$ in 2017)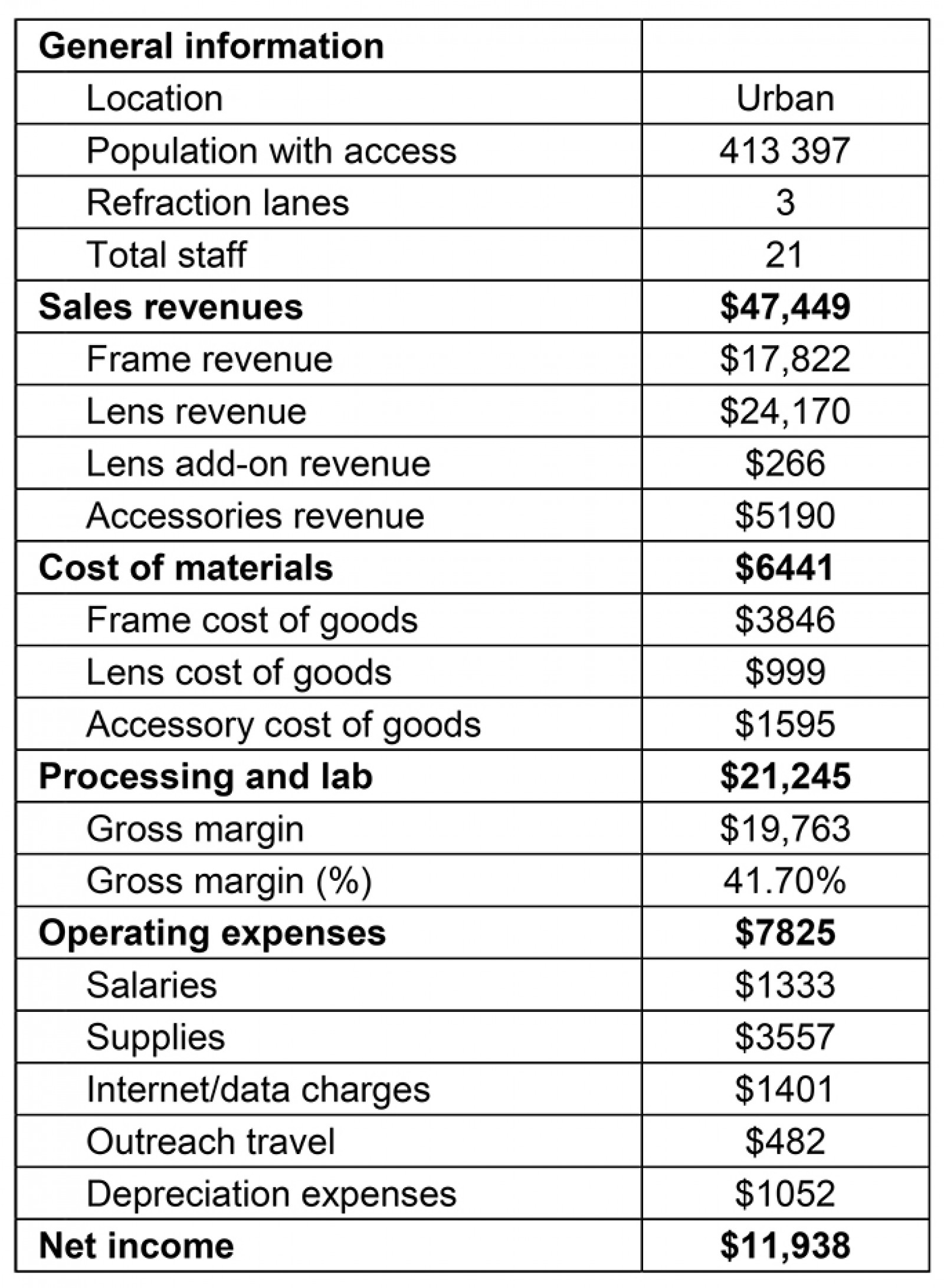
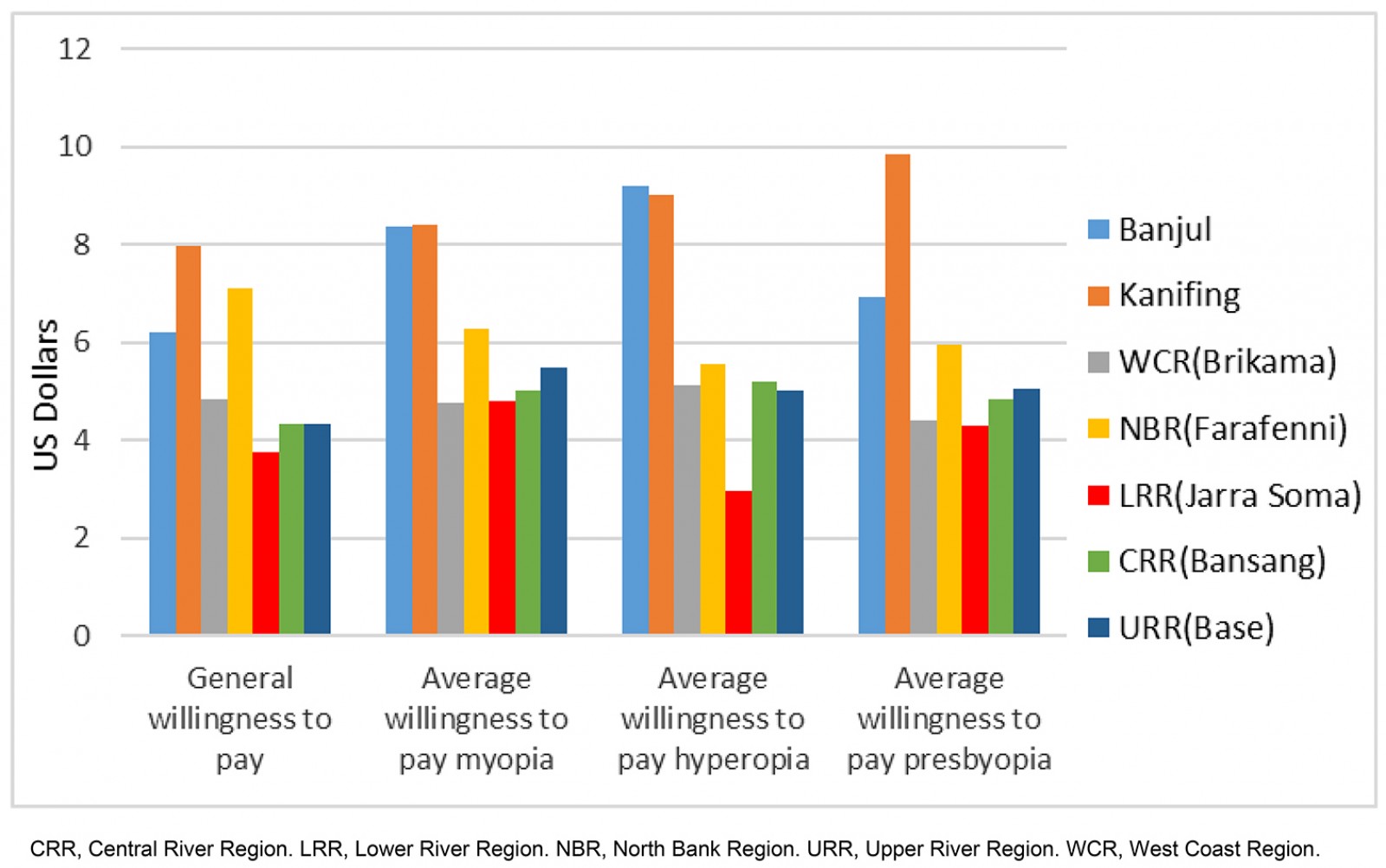 Figure 3: Willingness to pay for eyeglasses, by region (US$).
Figure 3: Willingness to pay for eyeglasses, by region (US$).
Infrastructure and technology: Over the period 2013 to 2017, seven vison centers and one manufacturing center were launched. During the first year, 2013–2014, 2239 eyeglasses were produced and sold. In 2017, the seven vision centers reported a total of 7248 eyeglasses were sold and a total of 63 620 individuals accessed vision care across all seven vision centers. The management and operation of the vision centers and manufacturing center has not been without challenges over this time period: the outbreak of Ebola in 2015, for example, affected the optical lead program and the timely production of spectacles.
Access to eye care in The Gambia
One of the main reasons for the partnership between OneSight and the Government of The Gambia is the issue of accessibility of eye care for the population. As of 2017, findings from the household survey showed that accessibility to eyecare services was still low. Almost 50% of respondents reported that formal eyecare service centers were located far from their households. Further research has shown that, in The Gambia, the majority of eyecare services are located in urban areas. Those living in rural areas need to travel long distances to access eyecare services. Poor road conditions, and lack of eyecare facilities and personnel, make access difficult in the rural areas3.
There have been several outreach initiatives to improve access to eyecare services and eye care products in The Gambia. As part of the initial vision center pilot, marketing of both the vision center and the services and products offered was implemented through radio, traditional communication such as billboards, and word of mouth. In addition, a sliding scale was used for pricing of eyeglasses based on ability to pay for each individual, as well as developing lower priced ‘ready-made’ eyeglasses. An urban outreach van, Mobile Urban Pop Up Eye Care, was used for outreach in urban areas, which helped with cross-subsidization of eyeglasses for lower income individuals3. A second van was added to make monthly visits to rural areas, eliminating the need for travel to the eye centers and making the eye exams and ready-made eyeglasses more accessible to those communities.
The prevalence for three types of refractive errors (myopia, hyperopia, and presbyopia) for men and women is shown in Table 3. The prevalence levels, which range on average from 17.42% for male myopia to 44.05% for female presbyopia, can be compared with the regional figures from the International Agency for the Prevention of Blindness7, showing a 41.36% refractive error prevalence in Western Sub-Saharan Africa and a 39.76% refractive error prevalence in Southern Sub-Saharan Africa. Table 3 also shows that access, measured by how many individuals in a household report having access to an eyecare center, is on average 40% for men and women.
There is variation in refractive error prevalence across regions. As shown in Figure 4, both Kanifing and West Coast regions have high refractive error prevalence compared to other regions. Moreover, the findings revealed that, in The Gambia, the majority of eyecare services are located in the West Coast Region, including Kanifing. For this reason, both prevalence and access to services is higher due to differences in socioeconomic status. Although Banjul is also considered urban, the reported access to eye care is 7.52%.
Awareness is an important aspect of access to vision care, including knowledge of the vision centers, their location, and the services they provide, as well as how wearing corrective lenses can improve some vision issues. According to the Gambian household survey on eyecare needs and services conducted in 2017, 88.14% of respondents reported awareness that wearing eyeglasses can enhance eyesight. Given the findings, it can be inferred that a majority of respondents have some knowledge of refractive errors symptoms and know that eyeglasses aid vision. In The Gambia, 97% of those who know about vision care services report that their source of knowledge comes through normal social networking and government eye clinics, while 3% report that their source of information is from government eye clinic centers. It is important to note that, given the public–private pilot partnership between OneSight and the government, many government eye clinics are simultaneously OneSight clinics. Finally, according to the household survey, 90% of respondents reported that they would go to the health facility if a household member had a vision problem, with the remaining 5% reporting they would consult a traditional healer.
Affordability of healthcare services, including eyecare service, is influenced by income of the consumers. The cost of the eyecare services and other sociodemographic factors may vary from developing to developed nations. As highlighted by Naidoo et al (2014), affordability to eyecare services should go beyond the cost of spectacles, because there are other indirect costs associated with it20. This is especially the case if the patient has to travel multiple times for measurements and to collect the spectacles. In The Gambia, affordability to buy a pair of eyeglasses ranges from US$0 to US$43.00. The average price of a pair of eyeglasses is US$5.23.
Table 3: Prevalence of refractive errors in The Gambia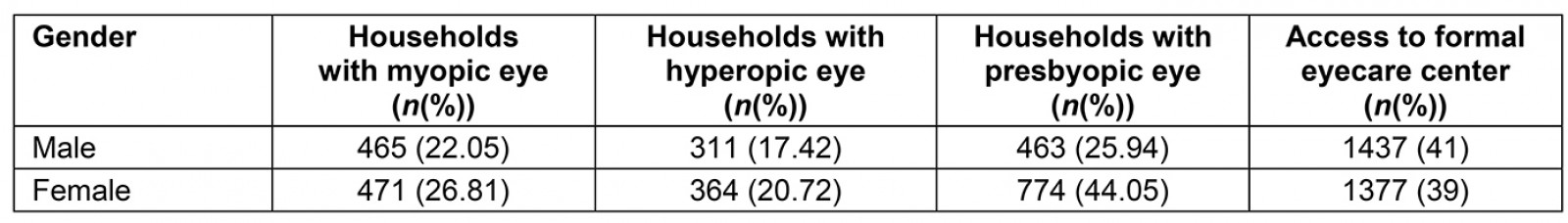
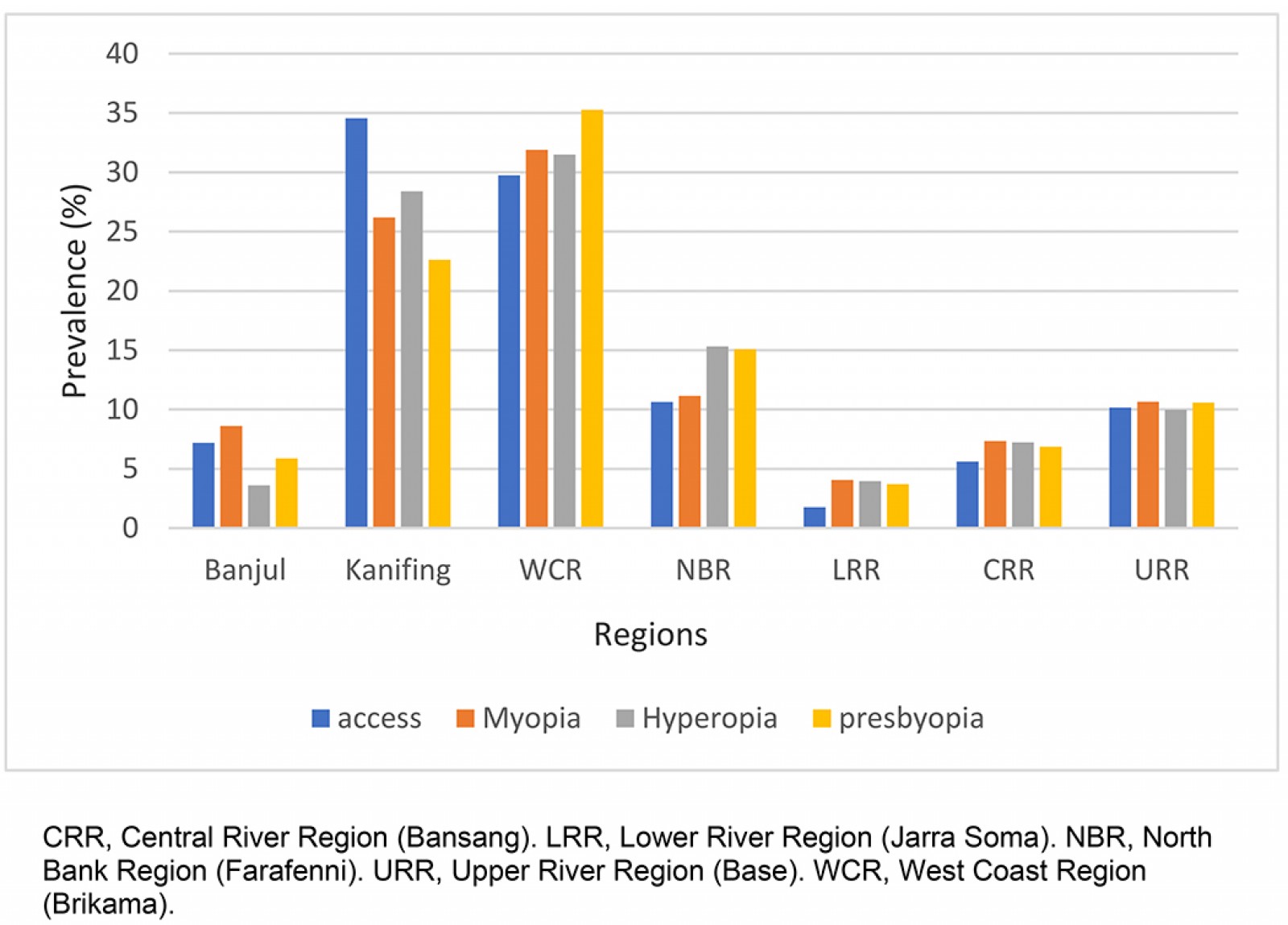 Figure 4: Access to and prevalence of refractive errors, by region, in The Gambia.
Figure 4: Access to and prevalence of refractive errors, by region, in The Gambia.
Discussion
The present study has shown how a health system framework can be used toward achieving improved vision care services in The Gambia. There are few studies that take a holistic view of the health system and vision care services. One study by Bozzani et al (2014)21 also adapted the van Olmen et al (2012)13 framework to analyze the Zambian eye health services. Their study found that 32 out of 74 eyecare facilities were owned by the government and supported by international non-government organizations (NGOs) (such as Sightsavers), while 16 facilities were owned by NGOs and 26 were owned by private for-profit NGOs. Most of the government facilities received both financial and technical assistance from the NGOs, such as training of optometrists, and some of the spectacle manufacturing labs were located in these government facilities.
To avoid challenges and gaps in access to timely diagnosis and eyecare treatment, Braithwaite et al (2018) highlighted the importance of the role of the central government in the provision of care as well as ongoing coordination with the private sectors22. Moreover, they identified priorities for eyecare system strengthening by using a health system framework. Their study stresses the importance of having a multi-stakeholder approach to eyecare services and ensuring their interests are made clear. Furthermore, the role of the government remains important in monitoring health systems, intervention in case of market failures, and re-distributing resources among the population to ensure there is access to health care, including eye care, to all. The Government of the Gambia took over operations of the vision care infrastructure in mid-2019. Since then, regular communication with the Minister of Health continues, all vision care and eyewear services have been maintained, and data collection and reporting standards have been upheld. Data transfer to the digital database from the vision centers in rural Bansang and Basse does face delays due to frequent internet connectivity issues. In addition, outreach efforts continue to help improve access in rural areas, with 19 events held in the first year after transition.
Although access to eyecare services in The Gambia was reported at 50%, it is on the rise, especially due to important collaboration between different stakeholders in The Gambia. As indicated by Khan et al (2010), through the integration of eye care in primary care and the interaction of different stakeholders there was a 297% increase in eye outpatients, and outpatient attendances increased by 375% in rural Pakistan23. The study also revealed that the number of eye surgeries performed over the period 2006 to 2008 increased from 13 579 to 50 882. Lilian et al (2018) reported that more than 50% of the population in rural South Africa have access to eyecare services in nearby facilities due to the coordination of different health system strengthening efforts24.
Other studies have similarly shown that individual and community awareness of the location of eyecare services can also influence utilization of eyecare services25. Furthermore, awareness of eye diseases can play an important role in seeking and accessing available services.
Affordability of eyecare services also impacts the utilization of eyecare services in many areas. For this study, affordability is measured through the willingness to pay for eyecare services, which includes purchasing a pair of eyeglasses. Marmamula et al (2014) revealed that affordability continues to be the leading barrier for the uptake of eyecare services in South India, especially among individuals who have no insurance coverage and those living in rural areas5. Their study found that, among 251 individuals with services-related barriers, 76.1% reported that unaffordability was the major barrier, while only 12.7% reported the lack of accessibility as the major barrier in utilization of eyecare services.
In Ethiopia, the main barrier to accessing eyecare services is the indirect medical cost of the services. Melese et al (2004) found that only 27.9% of those included in their study reported that they had been using eyecare services, while others reported indirect costs, including transport cost to health centers, inability to pay for eyeglasses, and having no one to accompany them to the health centers as reasons for not utilizing any eyecare services26. Laviers et al (2010) highlighted that the main barrier for utilizing eyecare services was lack of funds, resulting in only 17.6% of their population in Zanzibar with presbyopia having eyeglasses27.
Despite increasing eye care in The Gambia, there is still a large demand and a certain percentage of people who cannot pay for such services. A 2015 steady state analysis showed that differences in the cost of ownership for a pair of glasses at the OneSight eyecare centers between urban and rural locations was driven by the cost of transportation, which was significantly higher in areas with low population density and a dispersed population. Inability to pay was found to be a barrier to access, particularly for subsistence farmers28.
An individual’s willingness to pay for eyeglasses limits their ability to purchase spectacles, hence additional financing mechanisms are needed to address this issue, especially in rural areas. Willingness-to-pay factor and ability-to-pay factor are beyond just the initial decision of whether or not to purchase glasses. In the more rural vision centers, patients who did purchase eyewear were most likely to purchase the basic glasses only, whereas in the more urban areas they were more likely to purchase higher-tier products, more than one pair, accessories such as cases and cleaning cloths, and even sunglasses. Over time, increasing patients’ willingness to pay is necessary to help ensure the financial sustainability of the rural and remote vision centers28. A broad awareness campaign is a next step, including social behavior change approaches to encourage people to visit a vision center for refractive error correction, and not just when a more serious eye heath issue arises. This kind of awareness work could also help demonstrate the value of glasses to improving rural Gambians’ education, work, and quality of life.
Conclusion
Using a health system framework to understand service delivery is useful to identify strengths and weaknesses of population-based programs. This study in The Gambia is offered as an example of a unique implementation of a system-strengthening program for vision services. The results reported show the importance of including measures of access to rural and remote eye care, such as willingness to pay and cost of services, to capture variability across a country. The cultural, political, and environmental contexts need to be considered closely when applying similar system analyses in other settings.
As much as access to vision care has strengthened the health system in The Gambia, additional policy change can help drive higher utilization in rural and remote areas, such as strong integrated school health vision screening programs and a policy that makes vision screening mandatory before receiving a driver’s license. Further research is needed to assess the long-term sustainability of the vision center approach to integrating eye care into health systems, as well as the impact of the eye health infrastructure on the educational, economic, and social outcomes of rural and remote communities.
Acknowledgements
The authors wish to thank Clifford Scott, President Emeritus, New England College of Optometry; and Judith Williams, Program Manager, Americas, Vision Impact Institute for the information they provided and for their time in answering questions. They also wish to thank Vision Impact Institute for its support.
references:
You might also be interested in:
2016 - Health promotion and empowerment in Henganofi District, Papua New Guinea
