Introduction
Despite the existence of universal health care for Canadians, rural and remote communities have proportionately fewer health services and providers available1 and experience disparities in health outcomes as a result. This problem is not unique to Canada; rural disparities are noted in many settings globally. Australia, for example, has long encountered recruitment and retention issues for rural areas2,3. Reasons attributed to these difficulties have included professional isolation2 and a lack of local resources3, leading to health inequities similar to those found in Canada. Many services have become centralized to more urban areas, requiring rural patients to travel longer distances for care. Compared to their urban counterparts, those residing in rural areas are the least likely to access specialist services4. A lack of availability of health services for rural patients can result in higher all-cause mortality rates5, higher rates of avoidable deaths6, and a three-fold increase in risk of death in the emergency department7. These gaps and differences in services are most important when considering trauma care for rural areas because trauma situations require a large amount of immediately available resources.
Teletrauma has been recognized as a possible solution for extending the geographical reach of regionalized trauma systems8 and has been consistently adopted in rural areas9-13. For example, the implementation of teletrauma has been found to lead to a reduction in unnecessary transfers by identifying only those patients most in need of transfer, while stable patients are evaluated and eventually discharged locally9. Additionally, rural clinicians can perform otherwise unfamiliar procedures and develop professional skills, despite residing in areas with low user densities and less trauma exposure.
However, the current knowledge base on teletrauma for rural and remote areas is limited. To provide an overview of the empirical knowledge on teletrauma research and support knowledge synthesis, a systematic search of the literature was conducted. Knowledge gained from this literature review provides an understanding of the current state of teletrauma literature, and identifies gaps and potential directions for future teletrauma studies. Understanding why teletrauma is being utilized may permit insight into how programs may be used more effectively and judiciously in rural areas, promoting efficient use of limited resources.
Methods
This literature review was guided by Arksey and O’Malley’s14 scoping review methodology. This method was selected to identify, describe, and summarize the knowledge base of relevant literature on teletrauma.
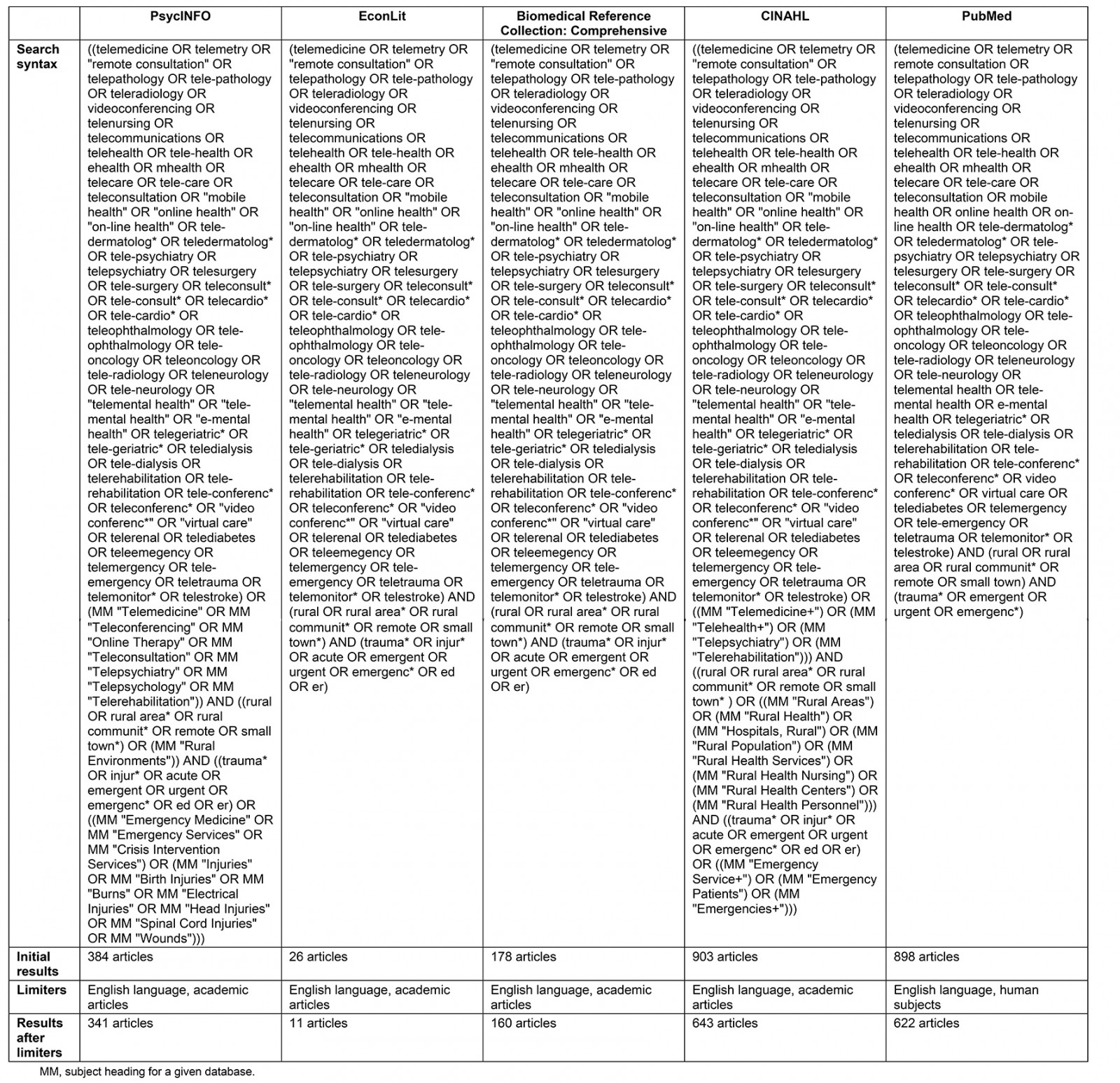
Five electronic databases were searched: Cumulative Index to Nursing and Allied Health Literature (CINAHL) Complete, Biomedical Reference Collection: Comprehensive, PsycINFO, EconLit, and PubMed. Keywords included terminology related to any telehealth service, trauma, and a rural setting, while relevant subject headings were used according to the database searched (Supplementary table 1). The search was peer reviewed by a health sciences librarian. No date or age limiters were used, because limited research was available. The search was restricted to peer reviewed articles available in English, and human subjects. Inclusion criteria consisted of care provided in a clinic, hospital, or emergency department and articles having a telehealth component to retain a focus on telehealth services provided within rural institutions. Articles were excluded if there was no acute or emergency care situation, or if there was no real-life clinical component. A matrix was created with clearly defined rules for the screening process to ensure reliability of the review. The number of excluded articles was recorded at each step. After an initial screening of titles and abstracts, full-text articles were reviewed according to the eligibility criteria (Fig1).
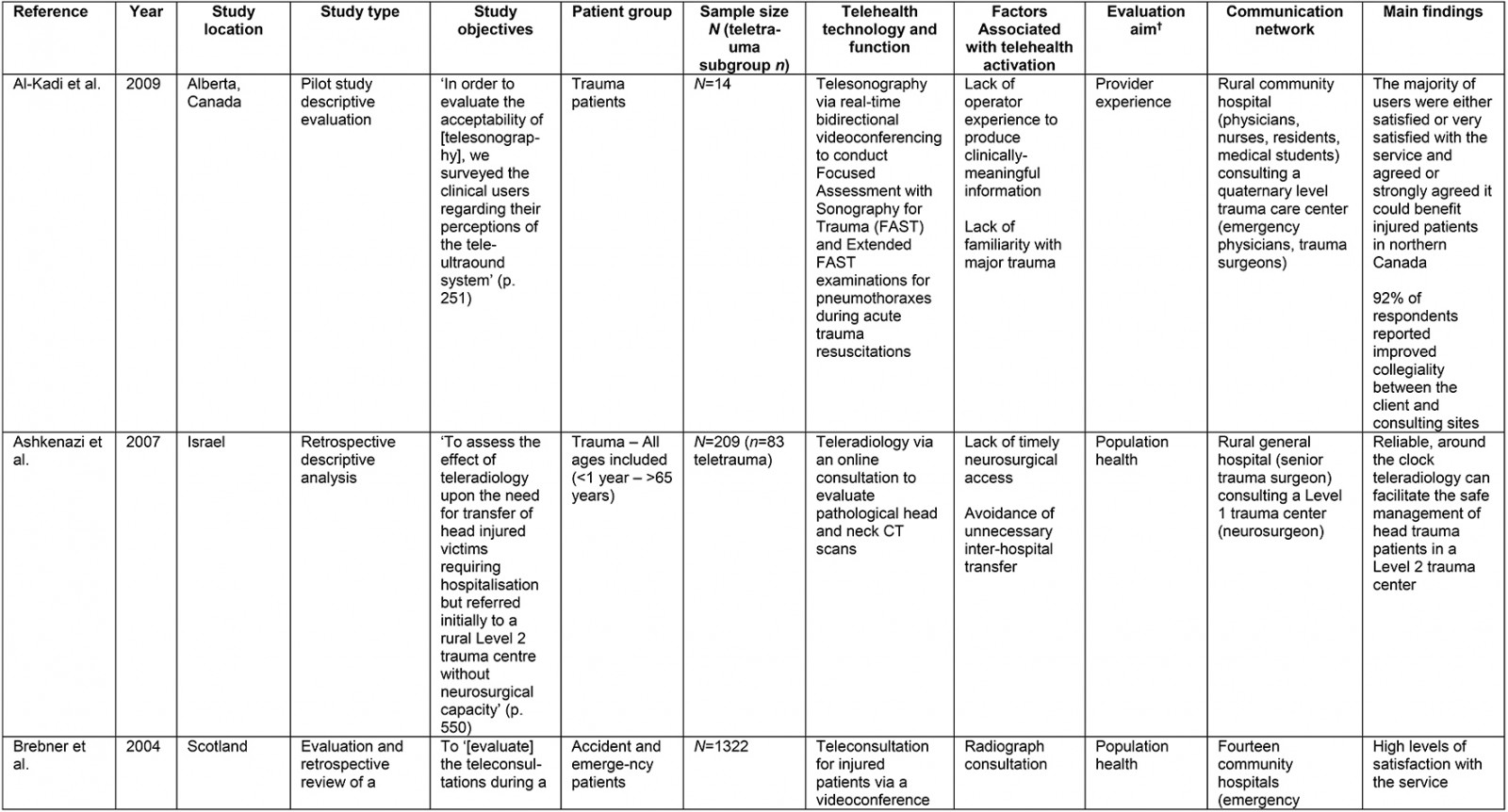
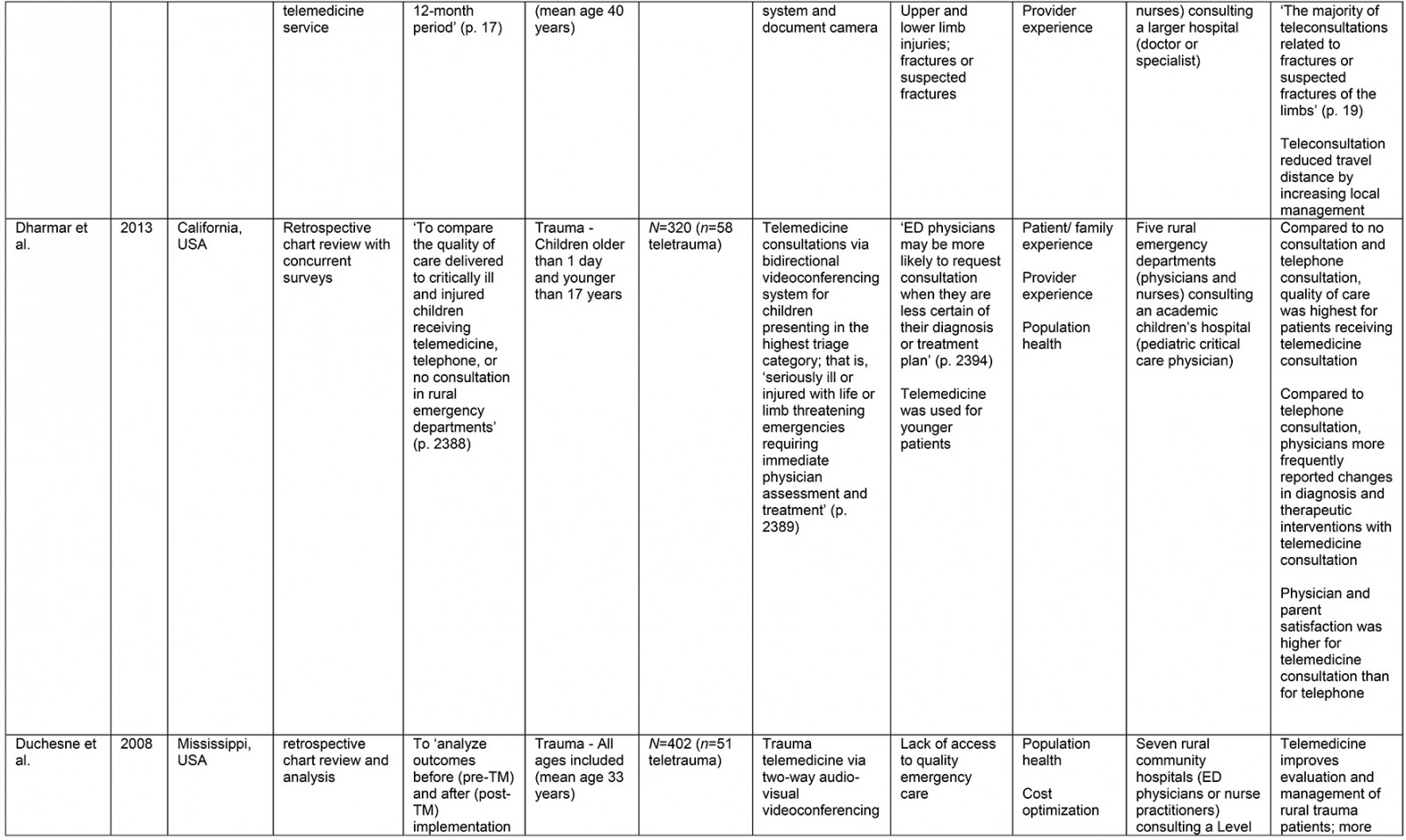
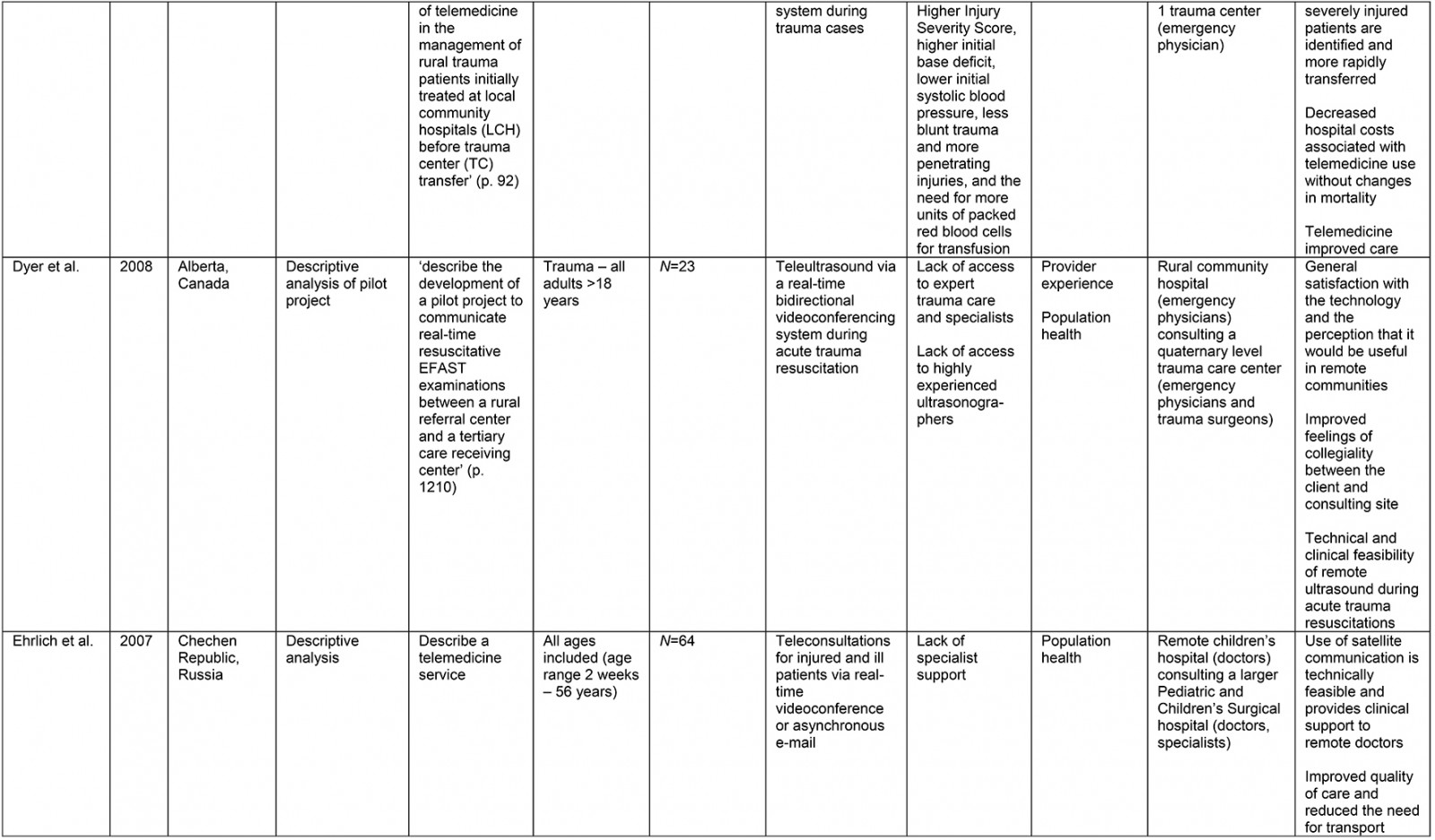
A data extraction framework was used to organize and ensure consistency of data collection (Supplementary table 2). Framework headings were created according to the research questions and to provide a descriptive overview of the current literature.
The Quadruple Aim framework15 was used to help categorize articles according to evaluation aim. Aims include provider experience, patient experience, population health, and cost optimization. Use of the Quadruple Aim framework for this literature review permits identification of aspects of the healthcare system being examined and highlights gaps in teletrauma evaluation research.
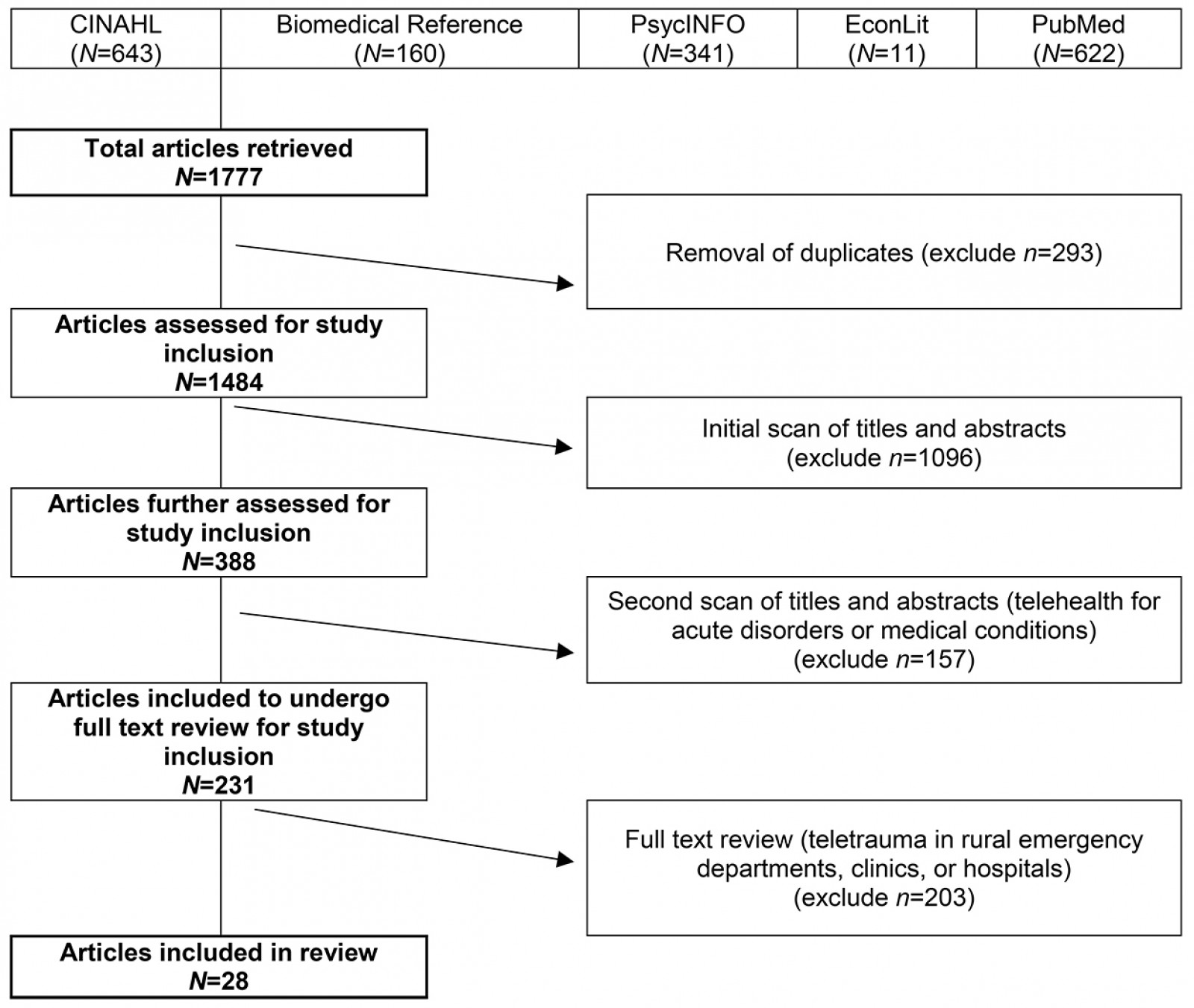 Figure 1: Article selection flowchart.
Figure 1: Article selection flowchart.
Supplementary table 1: Search strategy by database using keywords and subject headings
Results
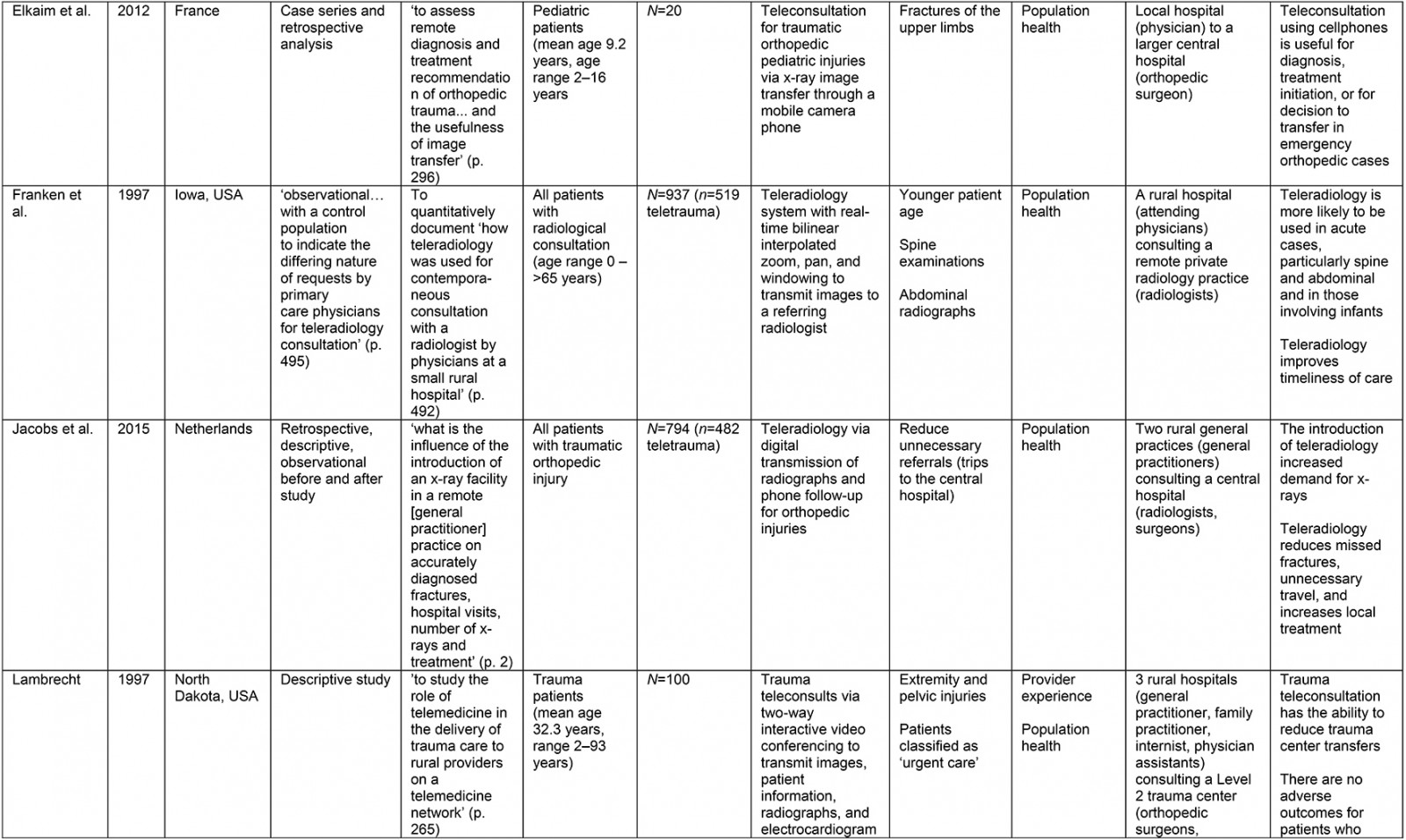
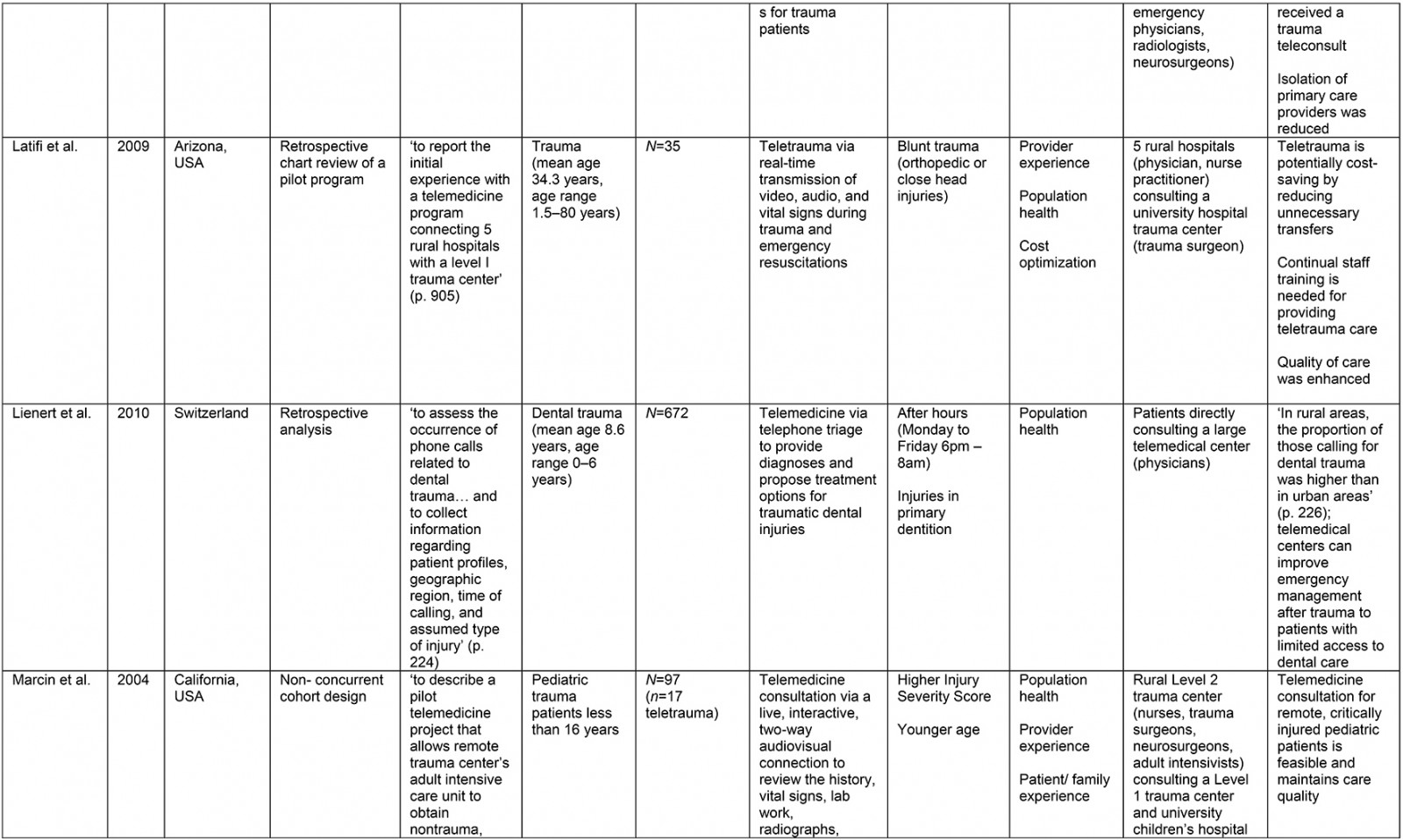
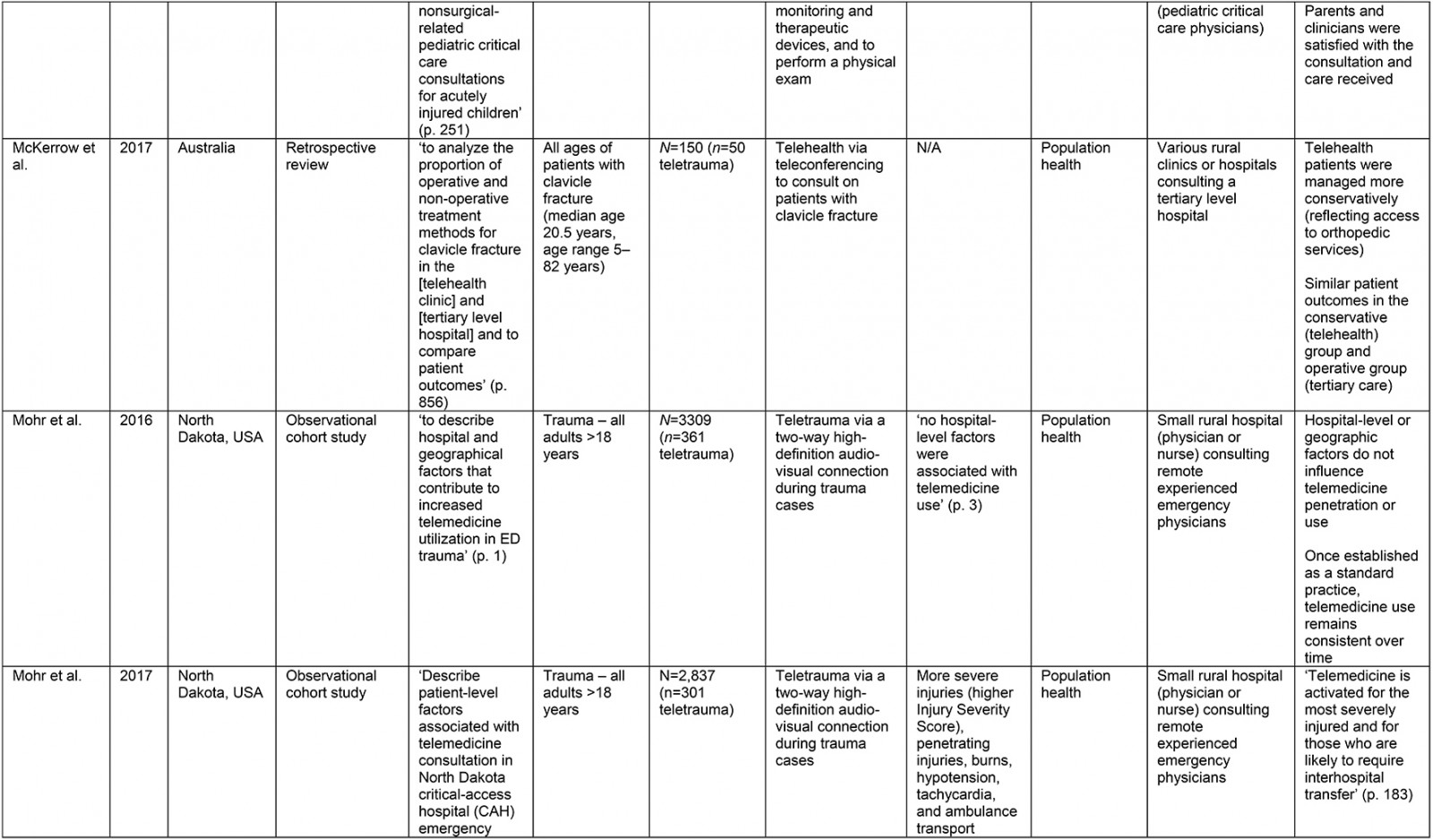
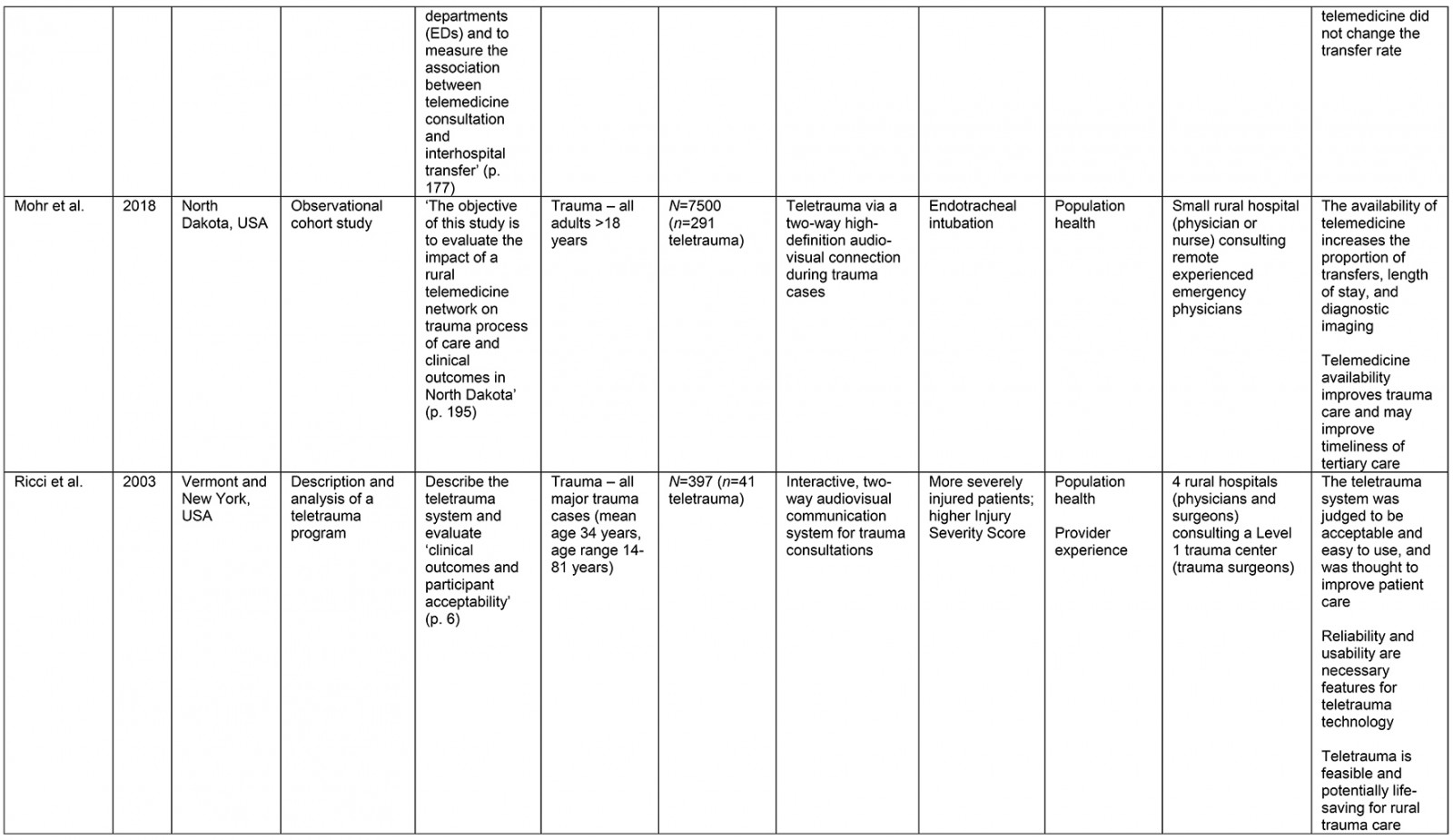
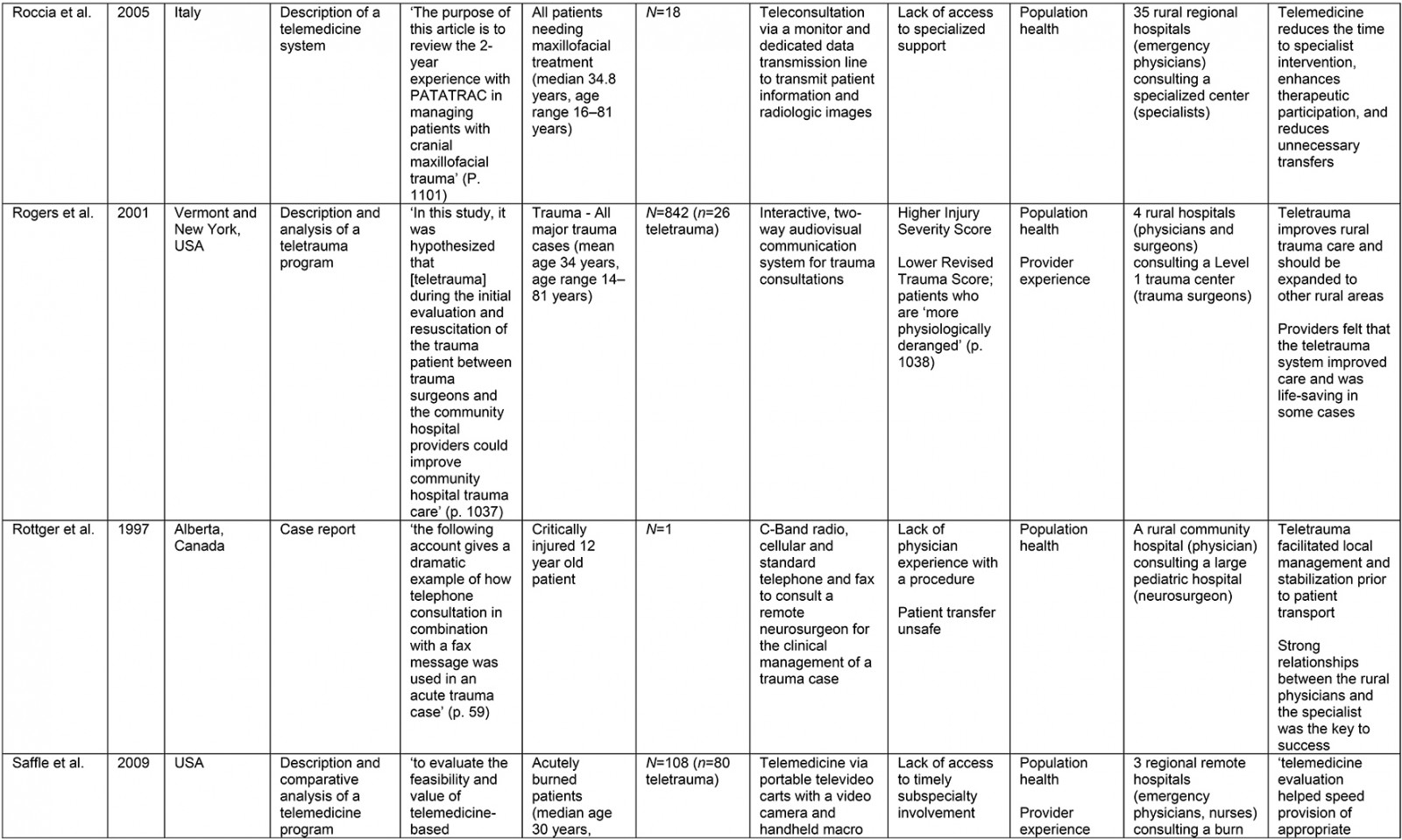
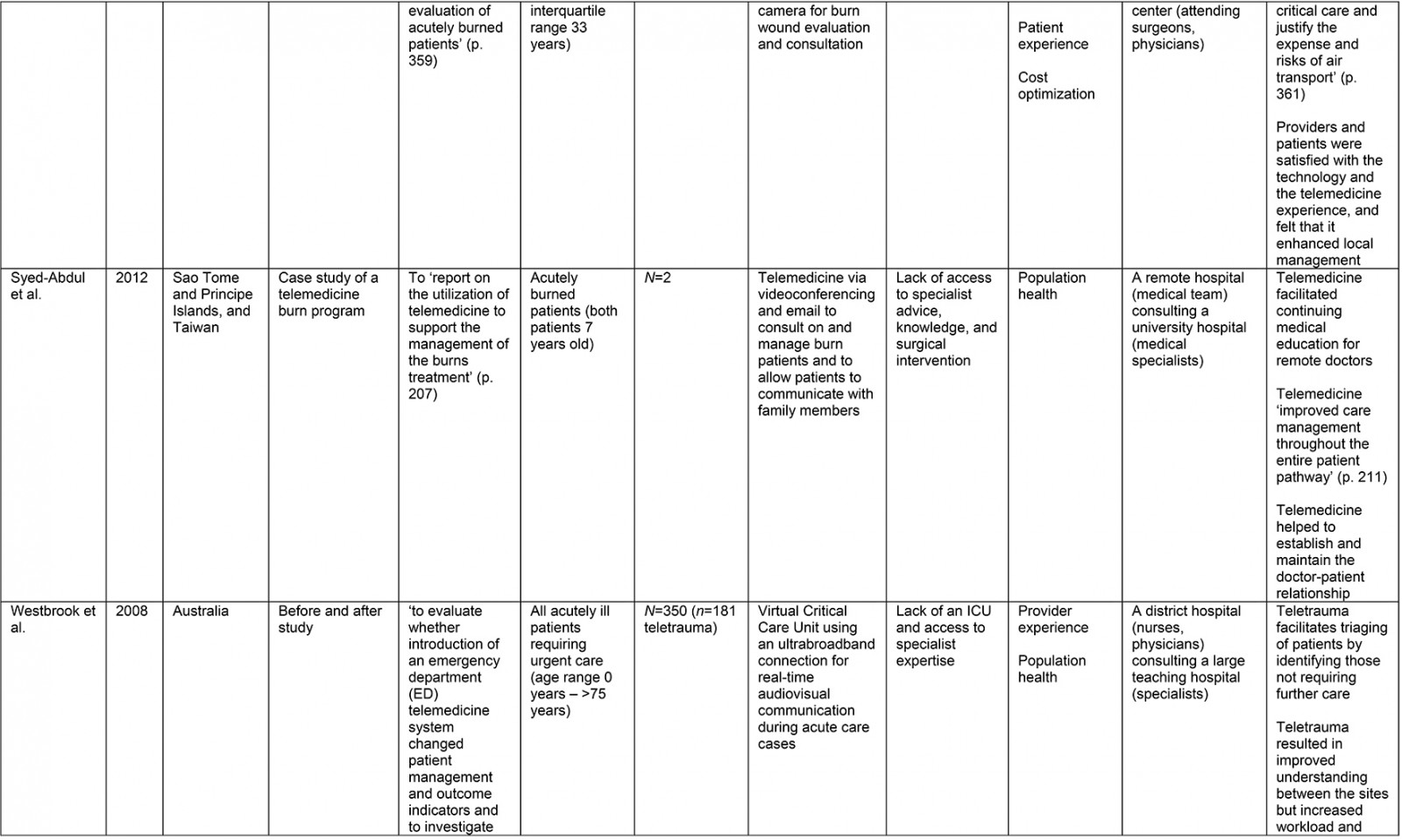
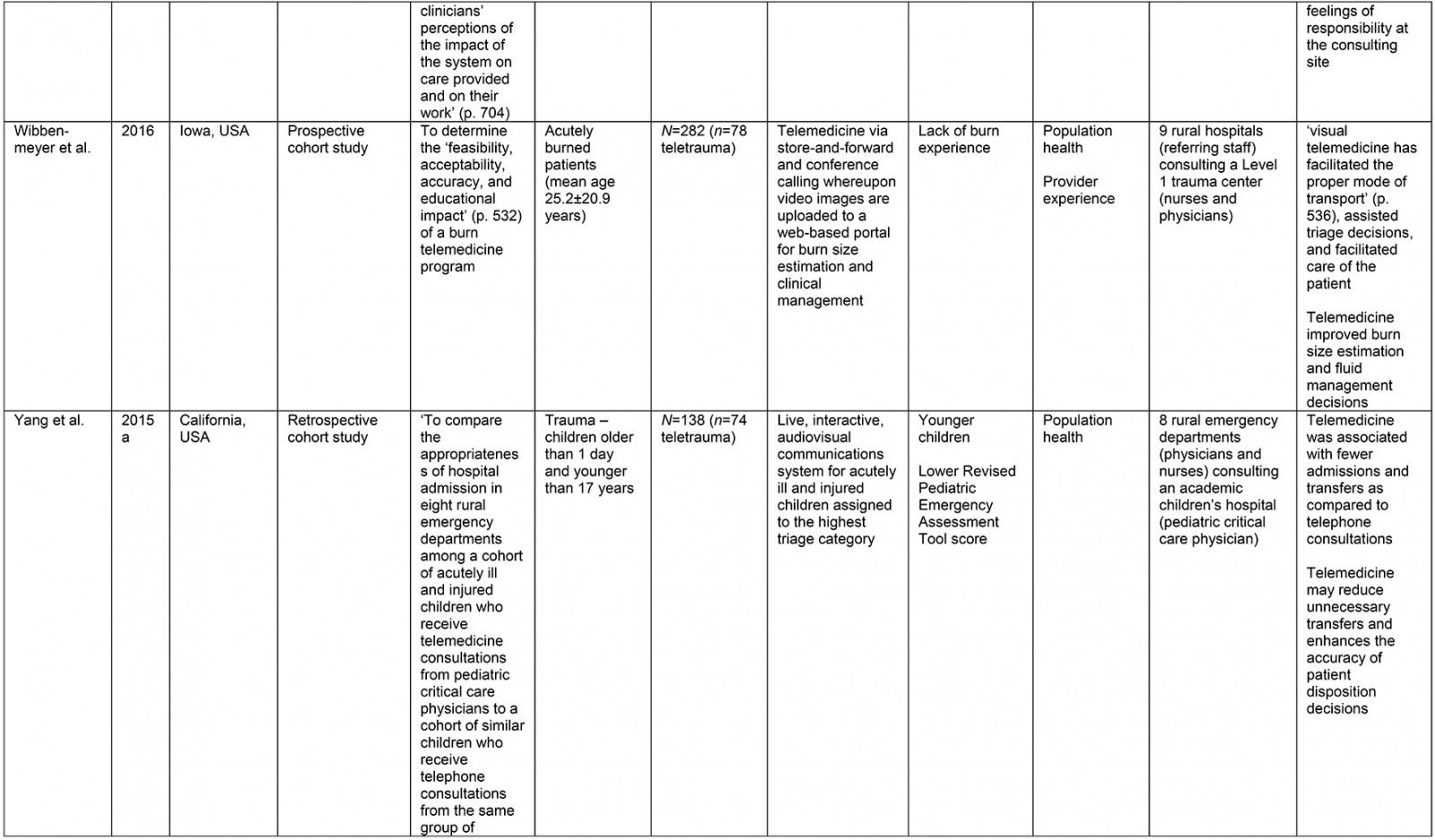
From the original 1777 articles identified in the initial search, 28 articles met the eligibility criteria and were included in the analysis (Supplementary table 2). Of the studies identified, 16 focused on patient populations that were classified as trauma cases. The remaining 12 articles examined cases meeting the definition of traumatic injury (acute injuries requiring immediate medical management) and were thus included, but did not specifically classify patients as being trauma patients. Subheadings were selected to best address the various aspects of the research question and to highlight commonalities or inconsistencies uncovered in the review. Examples are what constitutes a teletrauma service in terms of technology, or what is meant by ‘rurality’, ‘acceptability’, and ‘feasibility’, as this terminology is commonly used but often not explicated. A comprehensive service evaluation framework provided a guide for understanding the effects of teletrauma across all dimensions of the healthcare system.
Study characteristics
A large proportion of articles were published within the past 10 years (n=12) although teletrauma research has appeared as early as 199710,16,17. Three studies utilized observational cohort study designs11,18,19, six were classified as descriptive analyses12,16,20-23, three were identified as comparative or before-and-after studies13,24,25, while the most frequently used design was a retrospective analysis (n=11). Studies were conducted in 11 different countries, the most common being the USA (n=15) and Canada (n=3).
Of the 28 studies, 61% (n=17) included a non-teletrauma comparison group in analysis (ie trauma with no telehealth component, or phone consultation only). The largest teletrauma sample sizes examined was 1322 telehealth consultations regarding an injury26. The study with the smallest teletrauma sample size was a case report of a traumatically injured child (n=1) who received remote clinical management prior to transfer17. Articles with a study population that included patients of all ages constituted 61% (n=17) of the total, followed by pediatric patients under the age of 18 years (n=7) and adults over 18 years (n=4).
The communication network for teletrauma programs varied in size: one article studied telehealth consultations for acute injuries from 14 community hospitals consulting a larger hospital26; another examined a telehealth service between nine rural hospitals consulting a Level 1 trauma center to evaluate and manage burns patients27. The largest network included maxillofacial trauma cases from 35 rural hospitals consulting a specialized center12. Typically, articles described teletrauma services between a single rural community hospital or emergency department and a center with a higher level of care (n=13).
Terminology in the literature
The term ‘teletrauma’ is associated with the use of telehealth technologies for trauma care and management. Few articles28,29 used the term ‘teletrauma’ to describe a telehealth system designed for use during trauma care. Instead, several studies labelled their telehealth service based on the specific technology used. These included tele-ultrasound20, teleradiology21, and telesonography22. Although the functions of the individual systems are similar, the services were labelled based on their diagnostic or technological focus. Despite the lack of a formal definition, all telehealth technologies used at any point during the management of traumatic injury may be generalized as ‘teletrauma’, regardless of a focus on a particular aspect of care (eg sonography, basic consultation, or airway management). In summary, there was a lack of consistency in terminology related to teletrauma, and this may preclude knowledge synthesis in this field. The use of the prefix ‘tele-’ and attaching the clinical function of the service challenges the identification and evaluation of teletrauma literature more broadly.
The definition of ‘rural’ varied between articles. Some articles stated that the client site was rural or remote but did not elaborate on how this was defined20,23,27,30,31. Others used officially recognized rural zones, whether provided by a government body or healthcare organization, to classify sites as rural11,18,32,33. However, several articles expanded on the meaning of ‘rural’ by describing the remote facility characteristics and surrounding geography in relation to a larger center. Thus, rurality was described in distinct ways across the literature.
Several aspects of rurality were identified, including geographic separation9,26, lack of appropriate resources21,22, temporal barriers to care12,13,25, or some combination of these. It may be of use for future studies to define rurality in terms of these characteristics in addition to the accessibility of surrounding higher level services. This will aid in understanding the local context of health service delivery and how telehealth operates within that context, facilitating more accurate service evaluation.
Essential system components
Despite the varied language used, the essential components required for telehealth emergency services in rural areas were consistent throughout the literature. For trauma care, this typically included a real-time, bidirectional audio-visual videoconferencing system with a dedicated network line9,22,28,29. It was common for teletrauma systems to have mounted cameras with remote control capabilities9,29,33-35; however, most articles described the system only as having cameras with pan/tilt/zoom functions. Although different technologies and techniques have been used to establish a teletrauma system, more than half of the articles (n=15) used some form of video-conferencing. This has included a two-way audio-visual connection11,18,19,36, audio-visual communication system25,29,33-35, transmission of audio, visual, and vital signs28, and the explicit mention of a video-conference system9,16,20,22,23,26,32,37. For teletrauma systems deployed in rural areas, there were similarities in the types of technology used and the technological capabilities.
The design, specific elements, and capabilities of the telehealth system were driven by the needs of the clinical situation in which it was employed, provided appropriate local infrastructure was in place to facilitate the technological requirements. The technological components supported assessment of the patient by several parties at a distance in real time without requiring staff at the client site to position cameras9,29; a virtual presence is established at the client site with minimal interference to onsite staff. The similarities in technological components for rural teletrauma identified across the literature support the future development of teletrauma systems designed to meet the needs of patients and providers. Further knowledge syntheses in this area may be used to contribute to the creation of technological guidelines for rural sites wishing to adopt teletrauma services. The differences in technological components identified in the literature highlight the variability of technology capable of enabling a teletrauma service, while the commonalities in technology can help to elucidate the specific requirements for teletrauma deployment given the clinical demands.
Service evaluation aim
Examination of service evaluation aim permits insight into how the healthcare system is being affected by teletrauma services and identifies gaps in research. The majority of the included articles were classified as having only examined one aspect of Bodenheimer and Sinsky’s Quadruple Aim15. The most frequently evaluated aim was population health (n=26). Population health evaluation, in the context of teletrauma, included analysis of the safe medical management of patients21, transfer rates9, and clinical outcomes for patients37. Provider and patient experience was typically evaluated using quality of care measures28,32 or satisfaction surveys16,20,22,26. Evaluation aims studied the least were patient experience13,32,36 and cost optimization9,13,28,35. Articles categorized under the cost optimization aim included those evaluating transfer costs for teletrauma patients13,28, assessment of total hospital charges9, and a formal economic analysis35. Teletrauma service evaluations covering three or more aims were less common13,28,32,36 and usually included an examination of patient and provider experience as well as population health. Articles with combined evaluation aims typically included written surveys distributed to patients or providers and either a cost assessment or examination of clinical outcomes; one identified changes in diagnosis or therapeutic management of patients32, whereas another evaluated patient transport costs13,28.
While articles covering several evaluation aims could be considered more comprehensive, each individual aim appeared to be less robustly studied compared to those articles focusing on only one aim. For example, Saffle et al distributed a Likert scale containing only four questions to patients and providers to assess their experience using teletrauma13. Ricci et al, on the other hand, used a more robust method to assess patient and provider experience which included interviews, in-person observations, and questionnaires29. This provided a more in-depth analysis of the teletrauma-user experience through examination of attitudes, perceptions, and behaviors of patients and providers. A similar finding was discovered for the cost optimization aim; many studies postulate that teletrauma was (or could be) cost-saving, whereas Yang et al provided more formal analysis of associated costs35. Although it is useful for research to include all aspects of the Quadruple Aim15 to fully understand the effects of a service across the entire health system, it may be advantageous to capitalize on the robustness of single- or double-aim studies by synthesizing knowledge from several articles. Knowledge synthesis in this area contributes to a more comprehensive understanding of how teletrauma affects health systems while relying on robust studies that focus on only one or two aims.
Using Bodenheimer and Sinsky’s Quadruple Aim framework15, it was identified that service evaluation aims across articles were unbalanced. Population health was studied most frequently, while patient experience and cost optimization were evaluated the least, highlighting areas across the health system where service evaluation may be lacking.
Acceptability
The user experience is frequently evaluated in studies examining teletrauma services13,16,20,22,25,29,32,34,38. Teletrauma users include a variety of individuals involved with the encounter, including healthcare professionals (nurses, doctors, specialists) from both the client site and consulting site, patients, and family members of the patient. Likewise, one article, examining the impact of teletrauma for critically injured children, evaluated parent as well as provider satisfaction using validated surveys32. The authors measured various aspects of acceptability, assessing quality of care, changes in care, and satisfaction for teletrauma or telephone consultations. Results were then combined with quantitative analysis of the teletrauma and telephone consultations, providing a methodologically rigorous examination of user experiences in the context of pediatric trauma care.
Studies involving patient (or family) and provider perceptions of teletrauma have produced positive results, although ‘acceptability’ is measured in different ways across articles identified; clinicians have judged the system to be easy to use29, collegiality between the client and consulting sites was improved20,22,25, and up to 92% of providers were satisfied or very satisfied with a teletrauma interaction20. Teletrauma services for rural environments are also reportedly life-saving17,29,34. In two cases, a rural clinician was guided through an unfamiliar emergency procedure by an expert consultant, saving the life of the patient: Rogers et al described a successful emergency cricothyroidotomy by a community hospital surgeon who had not performed the procedure in more than 20 years34; Rottger et al mentioned that a craniotomy, a procedure that normally would have been conducted by a neurosurgeon, was successfully performed by a rural physician not trained on the procedure17. In both cases, teletrauma adequately facilitated safe and appropriate management.
Thus, ‘acceptability’ of teletrauma services can be considered an umbrella term that includes satisfaction, usability, and perceived value. Of these concepts, satisfaction was frequently used to capture patient or provider perspectives of teletrauma systems (n=7), reflecting acceptability of the service. However, while satisfaction with teletrauma services was generally positive, the full scope of benefits can be difficult to measure28 and thus the concept of acceptability should not be limited only to satisfaction as a proxy measure.
Feasibility
Across the literature, teletrauma was noted as being feasible; five articles explicitly mention the service as being feasible22,23,27,29,36. However, the concept of feasibility was measured in distinct ways across the various studies. Some examples of teletrauma feasibility include effective and reliable clinical ultrasound exam performance22, reliable use of satellite communication to support remote doctors23, accurate burn size estimation27, decreased overall hospital costs9, and lesser costs for video-conferencing compared to telephone when considering transfer decisions33. Therefore, ‘feasibility’ can be further categorized into clinical feasibility (accurate diagnosis), economic feasibility (cost-saving), and technical feasibility (reliable technology). Clinical feasibility was most commonly described in terms of therapeutic management or quality of care received (n=17). For example, Dharmar et al32 reported more changes in diagnosis and therapeutic interventions for patients who had teletrauma as compared to those with telephone consultations, resulting in a higher quality of care for teletrauma patients (5.60 (95% confidence interval (CI) 5.42–5.79) v 5.20 (95%CI 5.07–5.34), p<0.05, as measured on a seven-point scale). Teletrauma also facilitates the rapid identification and transfer of more severely injured rural patients, improving care9. In both cases, the teletrauma systems were judged as being feasible. Across identified articles, the term ‘feasible’ was used to represent a variety of conceptual categories. It may be useful for future research to adopt a common definition of feasibility in the context of teletrauma to facilitate program evaluation and allow for more robust comparisons.
Factors associated with teletrauma use
Associated factors can be categorized as being either antecedent (identifiable prior to the telehealth event) or as outcomes (identifiable after the telehealth event). These can be further subdivided into clinical or organizational factors. This classification system supports a targeted approach to teletrauma utilization where the system is activated only for those patients who may benefit most, identified and selected based on certain clinical and organizational criteria. Whereas some articles examined factors antecedent to individual teletrauma encounters and may therefore be used to screen patients, other studies cited reasons for adopting the teletrauma service as a whole.
Antecedent factors: Antecedent clinical factors included injury or trauma severity scales9,19,29,33,34,36, limb injury location16,26,30, mechanism of injury9,19,28, and patient age10,32,33,35,36.
Several clinical factors were found to be significantly associated with use of a teletrauma service. Scales were frequently used to evaluate the severity of injuries in trauma patients, including the Injury Severity Score39 or Revised Trauma Score40. It has been found that severely injured patients were more likely to receive a teletrauma consultation. Duchesne et al, for example, compared a cohort of patients who did not have teletrauma (n=351) to a group of patients that received teletrauma (n=51) to evaluate outcomes for rural patients9. The authors found that teletrauma patients had an Injury Severity Score of 18, compared to 10 for those patients who did not receive teletrauma (p<0.001). The authors also mentioned that they were able to select more severely injured patients, resulting in more aggressive treatment early on in the care management process. Similarly, Mohr et al19 found that, as compared to patients with minor injuries, those with severe injuries were 70% more likely to receive a teletrauma consultation (unadjusted odds ratio (OR) 1.70, 95%CI 1.13–2.56). This finding is echoed by several other studies reporting on injury severity or physiological illness9,29,33,34,36. Specific symptoms and mechanisms of injury have also been examined. Mohr et al found that patients presenting with hypotension, penetrating injury, tachycardia, and burns were more likely to receive teletrauma19, while Duchesne et al identified hypotension, penetrating injury, higher initial base deficit, and the need for more blood transfusions as being associated with teletrauma use9. Younger patient age was also found to be significantly associated with teletrauma use in a number of studies10,32,33,35,36. Marcin et al reported a mean age of 5.5 years for teletrauma patients versus 13.3 years for non-teletrauma patients (p<0.01) 36. Similar results in an adult population were demonstrated by Mohr et al who found that, as compared to younger patients, adults aged 65 years and older were 4.7 times less likely to receive teletrauma (risk difference –4.7, 95%CI –8.6 to –0.8)11.
Antecedent organizational and hospital-level factors were also examined in 14 of the captured literature9,12,13,17,18,20-25,27,32,37. Antecedent organizational factors included access to specialist knowledge or services9,12,13,21-23,25,37, number of unnecessary transfers21,24, clinical experience of local health professionals17,20,27,32, and hospital-level factors included rurality, number of trauma cases, and distance to a facility with a higher level of care18.
Mohr et al18 found that geographic factors such as rurality and distance to a facility with a higher level of care did not significantly explain variability in teletrauma use. However, the authors mentioned that the rural facilities all had similar capabilities resulting in a lack of variation of usage after teletrauma was adopted. Access to specialist knowledge or services was a commonly cited reason to adopt and use teletrauma (n=7). Saffle et al13 identified that untimely subspecialist involvement was a challenge overcome through the deployment of a teletrauma system. Physician confidence with therapeutic management and clinical experience were also factors identified in the literature; a lack of physician experience or familiarity with certain clinical situations have been noted as justification to adopt a teletrauma system20,27. Similarly, physicians were more likely to initiate a teletrauma consultation if they were uncertain of the diagnosis or clinical management of a patient32.
Outcome factors: Clinical outcome factors associated with teletrauma use were frequently reported by studies (n=14), including mortality9, length of stay11,25, and perceived quality of care received23,28,32,36. Duchesne et al9 noted that despite teletrauma being used for more severely injured patients, mortality did not differ significantly (17 (4.8%) pre-teletrauma v 4 (7.8%) post-teletrauma, p>0.05). The availability of teletrauma was also associated with an increase in length of stay for transferred patients (12.6 minutes, 95%CI 0.6–24.6) and non-transferred patients (15.6 minutes, 95%CI 9.7–21.4).
Organizational outcome factors were also studied, and included transfer rate or status11,12,16,19,23-26,28,33,35 and cost9,13,28,35. Roccia et al, for example, noted a 50% reduction in the number of transfers to a specialist center as a result of teletrauma use12. Cost reduction was also often associated with reduced transfers; Latifi et al noted that 29% (n=17) of transfers were prevented, saving an estimated $104,852 in transfer costs28. Lower costs as a result of implementing teletrauma were consistently mentioned in the literature9,13,28,35.
Discussion
The 28 articles included in this review provide insight into how teletrauma functions within rural settings and the effects of teletrauma on population health, patients, providers, and the health care system. Positive outcomes of teletrauma supports were well recognized; numerous articles explicitly mentioned the utility of teletrauma for rural areas9,17,20,22,29,34,37. As well, several antecedent factors associated with teletrauma utilization were delineated. These factors were categorized as being either clinical (eg demographics, signs and symptoms, medical interventions) or organizational (eg staff clinical experience, hospital rurality). Classifying these factors aided in understanding how various aspects of the care system may be used to target patients for teletrauma consultation. Although several elements, such as lack of access to timely specialist involvement and lack of physician familiarity with or confidence during major trauma, can be used to identify and select sites that may benefit from teletrauma, other elements can be used to develop a selective strategy for individual teletrauma encounters. Mohr et al explicitly call for a targeted approach to teletrauma utilization11. Uncovering the factors significantly associated with teletrauma use may lead to more judicious use of teletrauma resources in rural areas by identifying and selecting those patients who may benefit most. In this regard, it may be of use to employ a combination of clinical and organizational factors to select sites and patients for targeted teletrauma utilization. Whereas rurality, distance to a higher level of care facility, or lack of trauma resources are strong indications for teletrauma service adoption, clinical factors are less clearly indicative of when a teletrauma service should be used and warrant further investigation.
Studies also reported on a variety of factors associated with use of a teletrauma system. Few articles examined signs and symptoms of patients, in addition to other clinical and demographic information9,19. Although specific physiological signs (base deficit, tachycardia) may be used to select patients for future teletrauma use, further study is needed before this information can be clinically useful. On the other hand, several articles reported on other patient-level factors, identifiable prior to a teletrauma encounter, that are generalizable to and useful for future trauma cases. It was consistently found that younger patient age10,11,19,32,33,35,36, penetrating injury9,19, and high severity of illness or injury9,29,34,36 were significantly associated with teletrauma use. These findings can be used to support the development of criteria to select patients for targeted teletrauma use, such as a screening tool that may flag patients based on physiological or demographic information. However, it is important to recognize the complexity of trauma care in rural areas and the role of the provider. Given the large variety of resources available in rural areas and the variability of provider experience and comfort with trauma care, the decision to use teletrauma must not be based on clinical factors alone. It is essential that the provider be taken into account when deciding how to target teletrauma services in rural geographies.
None of the included studies specifically explored the experiences of physicians using teletrauma, and other stakeholders engaged in the planning and delivery of healthcare services. Further research to delineate these perspectives is needed to inform a comprehensive understanding of teletrauma services within a rural setting. Most notably, it may be necessary to examine how different teletrauma technologies support or hinder rural trauma care and how interprofessional relationships influence teletrauma encounters. As such, a next step may be to examine the use of teletrauma from the perspective of services users. Combining this data with the aforementioned clinical and organizational factors may constitute a strong step forward towards sustainable, effective, and efficient teletrauma system deployment in rural areas.
Conclusion
Rural trauma patients face increased challenges to accessing timely and appropriate health care. Teletrauma may be one solution, facilitating access to health services and resources. This review identifies gaps in current teletrauma research and highlights areas for further clinical and health services research. By identifying factors associated with teletrauma utilization, teletrauma programs may be used more judiciously and effectively in rural areas while enhancing access to definitive trauma care in rural areas. Gaps in current knowledge were also identified, including rigorous evaluation of why physicians use teletrauma. To address this identified need, further research is needed with an emphasis on the experiences of teletrauma users.
References
Supplementary material is available on the live site https://www.rrh.org.au/journal/article/6354/#supplementary
You might also be interested in:
2018 - Scope of Practice of Family Medicine Graduates Who Completed Rural vs Urban Program