Introduction
In Canada, the province of Ontario’s current healthcare delivery model is transforming towards patient-centered health care1. This conceptualization values health promotion, chronic care management and a patient-centered approach that considers the social determinants of health2. There are many drivers of this transformation of healthcare delivery including the aging population of Ontario requiring increased healthcare services1. This highlights a need for improved home and community care3.
Northern Ontario is a vast land mass of more than 800 000km2, where 40% of the population live in rural communities that are culturally diverse, with many Indigenous and rural Francophone communities that are located hundreds of kilometres away from tertiary health care centres3 and physicians4. In recent years, paramedics in Ontario have become more involved in providing patient-centered health care in patients’ homes and clinics. Funded by the Ontario Ministry of Health and Long-Term Care, a province-wide community paramedicine (CP) pilot program was launched in 20155. The goal was to provide improved patient care in home and community contexts and to reduce the high rates of unnecessary emergency department visits and hospital admissions5.
CP is an evolving, community-based healthcare model where paramedics function outside their usual emergency response and transport roles5. In Canada, the emergency response dispatch system is activated when patients, caregivers or bystanders call emergency services. This new CP role's original purpose was to reduce the number of unnecessary emergency calls, emergency department visits and improve patient health promotion by increasing proactivity in addressing patients’ health needs in their homes and communities5.
One of the primary strategies employed in the Ontario model of CP is to identify frequent emergency medical services (EMS) users through dispatch data; paramedics can then identify and proactively arrange to consult or meet with those who frequently call 9116. CP consists of several essential consultations that are delivered to patients. Consultations are usually provided by ad hoc home visits and/or at wellness clinics in the community. An ad hoc home visit is a service in which paramedics visit patients in their homes and monitor their health status, provide assessments for activities of daily living, record client vital signs and provide medical referrals that may be required5. Wellness clinics are usually held in a public setting (eg a social housing complex for seniors, community centre or a booth at local events) where paramedics invite local residents, usually seniors, to participate and provide health education, blood pressure readings and medication reconciliation6. Rural and northern CP programs are unique compared to larger urban CP programs in southern Ontario because urban programs usually have dedicated community paramedics or paramedics who devote their entire shift to performing CP duties. However, in rural CP programs in northern Ontario, it is more common for paramedics to practice both conventional paramedicine and CP during the same shift.
Some research has studied the patient perspectives of Ontario CP programs5-9; however, there is a paucity of literature related to paramedic perspectives of CP. To understand the outcomes and impacts of a community-based health program, it is essential to understand the program from all parties' perspectives. This would enhance comprehensive recommendations to the CP program if it is to be sustainable and positively received in the future by both patients and paramedics10. Important constructs to consider are paramedic training and education that may be necessary for CP7,11,12 and the paramedic–patient professional relationship6,13.
The patient–paramedic professional relationship may be strengthened in a CP context compared with an emergency response context6,13. The conventional model of paramedicine usually involves treating patients in ambulance vehicles, outside of ambulances at the scene of the incidents and transporting them to a hospital to be cared for by medical staff; paramedics then leave without knowing about the outcomes related to the patient’s illness or injury. Often the duration of the paramedic–patient interaction in an emergency context can be measured in minutes. In Australia, paramedics with expanded roles have indicated an increased sense of community belonging from the longer interaction and relationship development when treating patients several times in their homes13.
A Cochrane systematic review identified 11 studies related to CP programs14. Ten of the 11 studies indicated that CP was positively received by patients. A CP-type program in which paramedics in Australia had an expanded scope of practice was viewed as generally positive by paramedics and improved work-related experiences of paramedics15; similar results were found in the UK16. Though there have been previous evaluation activities regarding CP, there is a need for further research related to CP in Canada from paramedics. The theoretical Framework for Program Evaluation in Public Health, developed by the US Centers for Disease Control and Prevention, outlines effective methods for health program evaluation. To ensure adequate program evaluation and program implementation, it is important to collect evidence from those who are stakeholders in the program and those who either benefit from or deliver the health programs, such as paramedics directly involved in practicing CP17.
The purpose of this article was to evaluate several pilot CP programs in northern Ontario from the perspectives of paramedics, to gain program recommendations related to both rural and urban settings across northern Ontario.
Methods
This study consisted of surveying paramedics in eight districts located in northern Ontario, Canada. Data were collected by an online questionnaire including closed- and open-ended questions. A sequential explanatory research design was employed, the primary source of data was quantitative, and the supplemental data from the open-ended responses provided further explanation and aided interpretation of the quantitative data18 through thematic analysis19.
The process of questionnaire development involved generating CP-specific questions, which were modified in consultation with managers/supervisors. The questionnaire was pilot tested with paramedics to ensure questionnaire functionality, comprehension and relevance using cognitive interviewing principles20. This study focused on evaluating responses to the questions related to CP, and there was a subset of questions for paramedics with experience practicing CP about their experience with specific aspects of CP services that they may have been involved in (wellness clinics, home visits, referrals and remote patient monitoring). The closed-ended questions consisted of Likert-type response options: ‘strongly disagree’, ‘disagree’, ‘agree’, ‘strongly agree’ and ‘do not know’. The purposes of the CP questions were to gain a wide variety of paramedic perspectives regarding several aspects of CP services, to gain insight into positive components and areas for program improvement.
The final questionnaire instrument and informed consent process was prepared for online distribution using REDCap21.
Questionnaire administration
The online questionnaire was distributed to eight paramedic services by an invitation email that was sent to the manager/supervisor or CP lead in each district across northern Ontario. The email, containing a link to the online questionnaire and informed consent process, was then distributed to all paramedics. Paramedic services were designated as northern if they were located in the Northeast and Northwest health regions known as Local Health Integration Networks (LHINs). ‘Rural’ was defined as communities with less than 30 000 people3.
The EMS providers were instructed to distribute the email invitation to participate in the online questionnaire to only frontline primary care and advanced care paramedics; paramedic managers/supervisors were excluded. The eight participating EMS providers were located throughout various jurisdictions in northern Ontario. For this study, these services are described collectively as those of EMS providers. The majority of these EMS providers provide pre-hospital care to rural areas throughout northern Ontario, although paramedics employed with these services also provide pre-hospital care in several larger, urban centers.
Six of the eight EMS providers involved in this study are relatively unique in that CP was practiced with on-duty paramedics who practiced CP duties in addition to their conventional emergency response duties, and two urban centres utilized paramedics fully devoted to practicing only CP. The number of paramedics working in these districts, at the time of the questionnaire administration, was estimated to be 879. This population included primary care paramedics (PCPs) and advanced care paramedics (ACPs) working full-time and part-time. At the time of questionnaire distribution, the percentage of the 879 paramedics working in the EMS districts who were male was estimated to be 67.7% (n=595), and the percentage of paramedics who worked as full-time paramedics was estimated to be 60.9% (n=535).
Data analysis
All data collected using REDCap21 was downloaded, cleaned and error-checked before analysis. Questionnaires that contained completed CP-related questions regarding wellness clinics, home visits, program successes and areas for improvement were used for the analysis. The overall approach to the data analyses was Creswell’s Explanatory Sequential Design Method18, which focuses primarily on analyzing quantitative data with the open-ended data used to support and assist in the interpretation of the quantitative data.
The quantitative data were analyzed using the Statistical Package for the Social Sciences v20 (IBM; http://www.spss.com). The demographic data (sex, age, certification level, years employed, employment status, LHIN geographical area and work location) and CP program-specific data were summarized using descriptive statistics. Statistically significant differences in demographics of those who participated in CP compared to those who did not were examined using χ2 analyses and Fisher’s exact tests. Due to the substantive differences between urban and rural CP programs, a χ2 analysis was used to explore the differences in paramedics’ perspectives in these two different contexts.
The open-ended data for CP-related questions were analyzed using Clarke and Braun’s thematic analysis technique to uncover themes emerging from the text19. As described by Clarke and Braun, the thematic analysis process included familiarization of the data in which several reading phases were conducted to understand the more in-depth meaning of the text19. The next phases included generating initial codes, and these codes were then used to develop specific themes related to the overall CP program. These data analysis results were organized using descriptive statistics and themes related to overall CP, wellness clinics and home visits.
Ethics approval
Ethics approval was obtained from the Laurentian University Research Ethics Board on 28 October 2016 (REB 6009514).
Results
Quantitative findings
Out of the 879 paramedics who were eligible to participate, 185 (21.0%) completed CP-related questions on the questionnaire and were included for the analysis. The average length of time paramedics practiced CP was 6 months to 1 year at the time of questionnaire administration. There were 75 (40.5%) participants who self-identified as having experience with CP for an EMS provider with a formally established CP program (Table 1). Paramedics with CP experience were classified as having CP exposure and may not have necessarily practiced CP full-time. With the exception of the two urban centres services, the EMS providers’ combined expectation was that all paramedics were to be trained to practice CP as it was to be included in their job duties along with responding to emergency-911 calls.
The χ2 analysis indicated that significant differences between paramedics who participated in a CP program and those who did not was related to certification (χ2 (1, n=185)=8.79, p=0.012) and work location (χ2 (1, n=185)=19.66, p<0.001) (Table 1). Of the 75 paramedics with CP experience, 60.0% (n=45) participated in wellness clinics, and 72.0% (n=54) participated in home visits (Table 2).
The Fisher’s exact test findings in Table 2 summarise perspectives from only the paramedics practicing CP (n=75) related to the type of service in which they were involved (ie wellness clinics v home visits), satisfaction with CP, practice preference (CP v conventional duty) and length of time participating in CP. When asked which paramedic duties they would prefer to practice, 66.7% (n=50) of the 75 paramedics who practiced CP indicated they would prefer a combination of regular EMS duties and CP, with 27.8% (n=21) indicating EMS only, and 5.6% (n=4) preferring to practice only CP (Table 2). Compared to their rural counterparts, northern urban paramedics appeared to be more positively receptive to CP. The results showed a higher percentage of urban paramedics indicating the desire to either practice CP duties only (15.4% urban (n=2) v 3.4% rural (n=2)) or a combination of regular EMS duties and CP duties (76.9% urban (n=10) v 64.4% rural (n=40)) (Table 1). Regarding CP service type, rural paramedics were most likely to provide home visits as a CP service (p=0.038). No other statistically significant differences were detected between urban and rural CPs.
Table 1: Characteristics of paramedic respondents in northern Ontario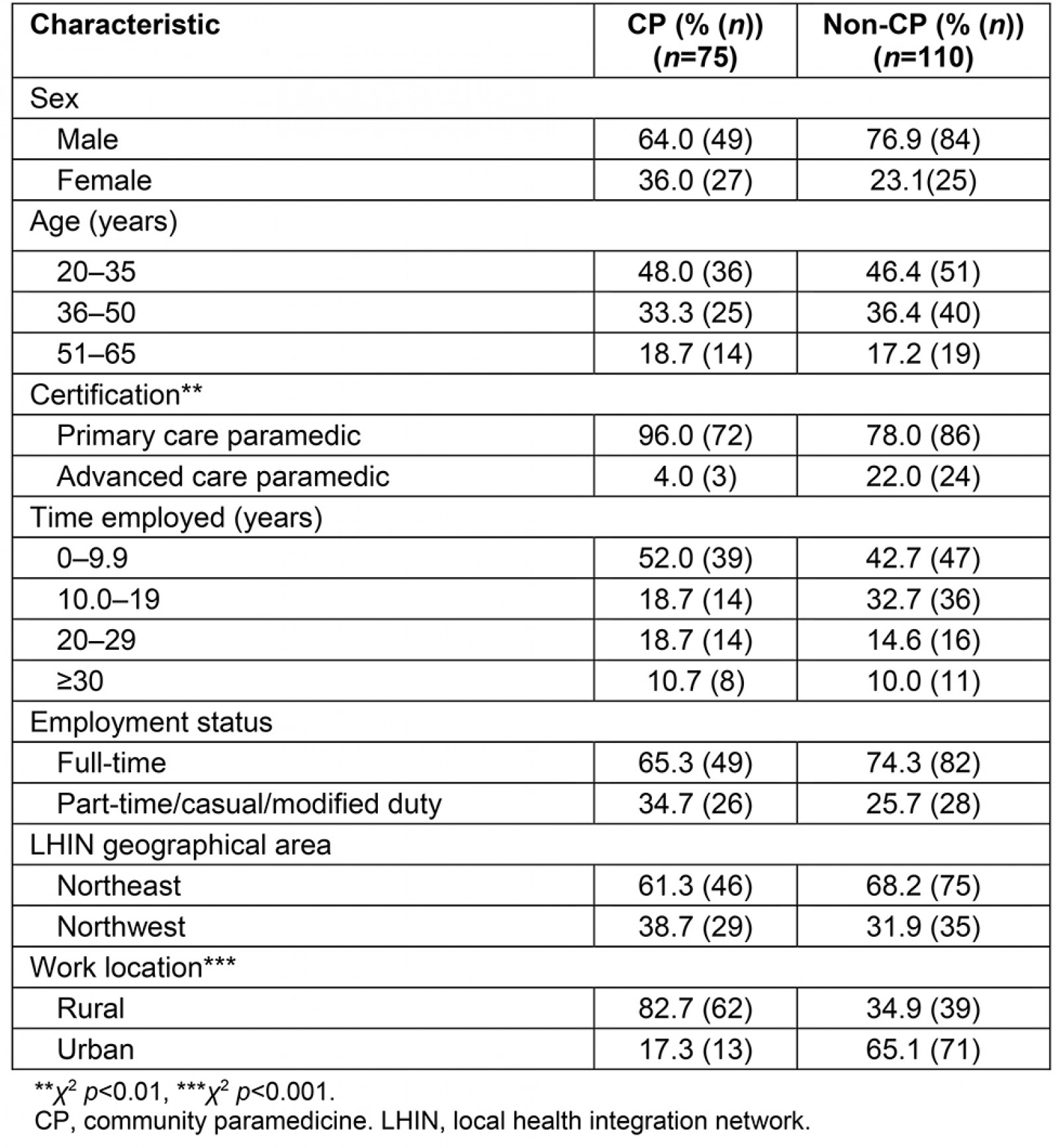
Table 2: Service type, satisfaction, and preferences of urban and rural paramedics practicing community paramedicine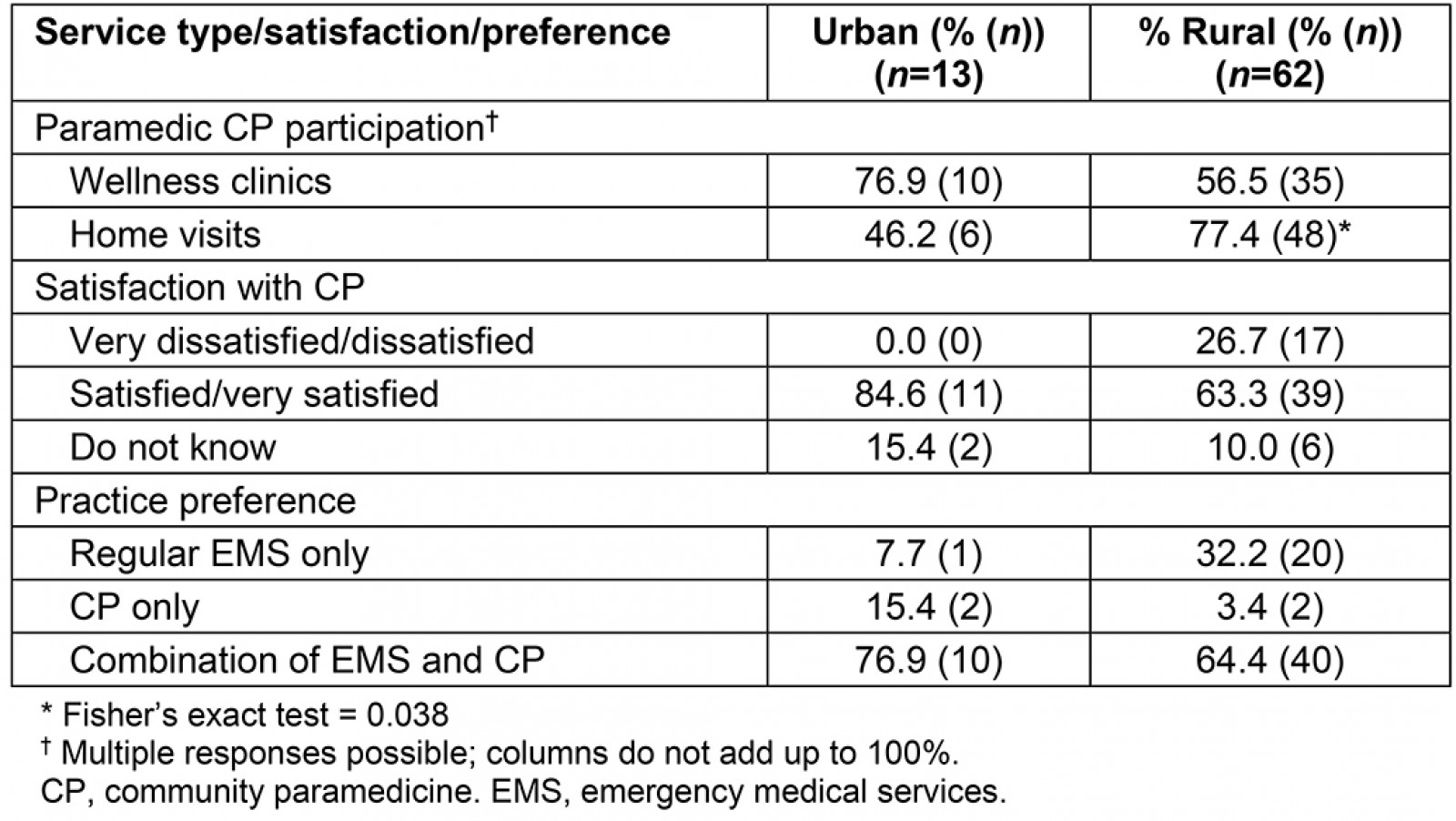
Overall impressions of CP: Two-thirds of paramedics (67.1%, n=50) were satisfied or very satisfied with the overall impacts and outcomes of the program, while 21.9% (n=17) were dissatisfied, and 11.0% (n=8) were not sure. Most paramedics with CP experience also stated that more paramedics should practice CP, with 76.7% (n=65) agreeing with this statement. Paramedics who practiced CP (Table 3) were asked to indicate their opinions about CP through their agreement with several statements about program-specific aspects. The questionnaire item that resulted in the strongest agreement from paramedics was about the patients’ receptiveness and appreciation (97.3% (n=71) agree/strongly agree). Other CP-related items are summarized in Table 3.
Table 3: Paramedic perceptions of community paramedicine program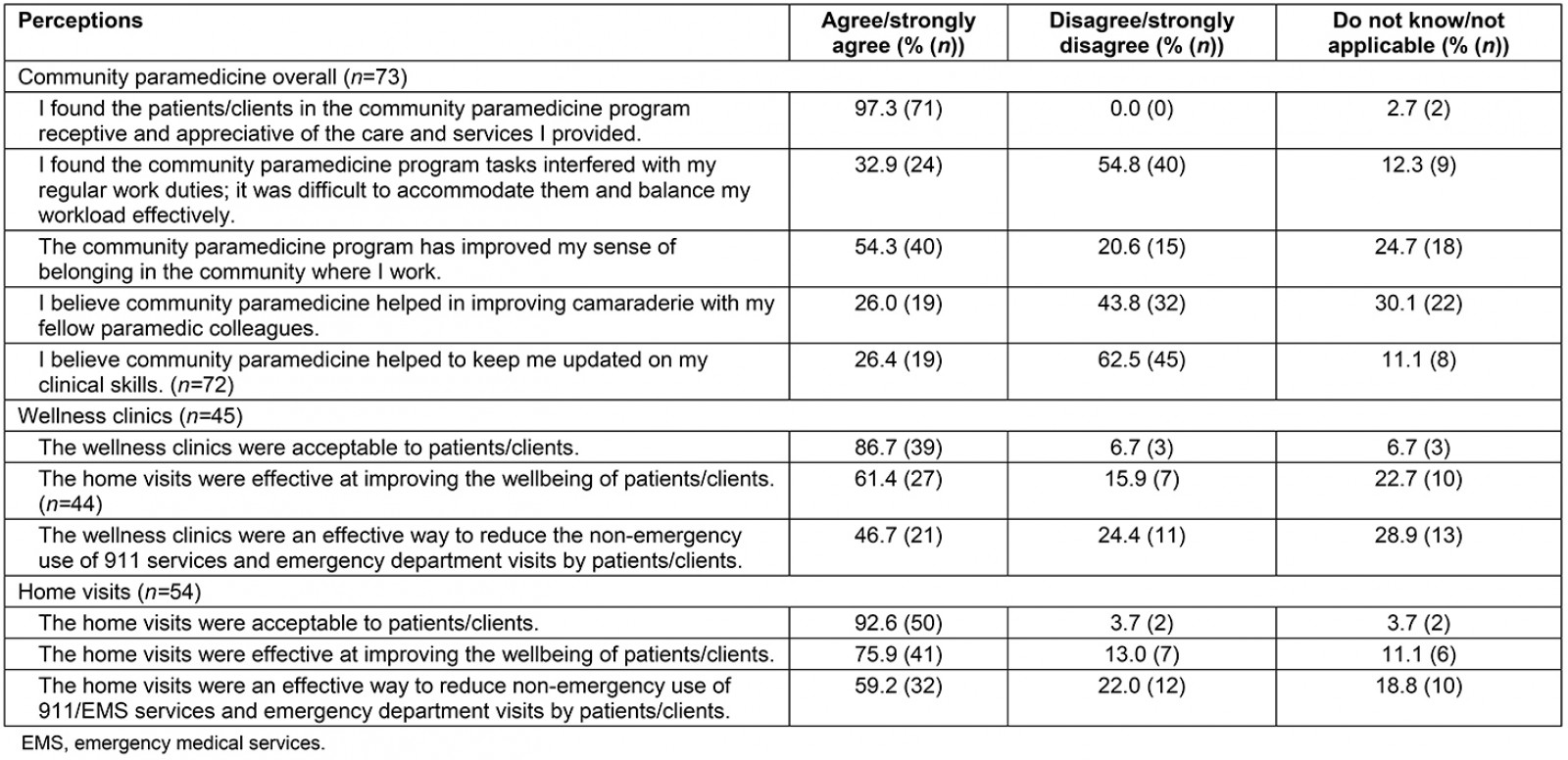
Qualitative findings
The open-ended responses when paramedics were asked ‘What did you like about the CP program?’ generated two themes: developing professional relationships and promoting patient health. When paramedics were asked ‘What could be done to improve CP programs?’, three themes emerged from the data: lack of CP-related training, fear of service interruptions (related to wellness clinics) and need for improved patient data tracking (related to home visits).
Developing professional relationships: Paramedics indicated that CP provided the opportunity for them to develop professional relationships with patients. The additional time spent with patients during a CP interaction seemed to be an important factor that enabled paramedics to develop relationships and follow up with patients. These two supportive comments were given by paramedics when asked ‘What did you like about the CP program?’:
Having the ability to develop a friendly relationship with patients and other people in the community. Being sociable with the residents of the seniors’ homes. (ID 110)
Get out into public easier to sit and chat and get detailed assessment when we are not trying to beat the clock. Working in non emergency setting allows for more connection and follow up with patients. (ID 165)
Promoting patient health: Another common theme that arose from the open-ended data was the opportunity for paramedics to improve a patient’s health status through CP. This was viewed as both health education and emergency prevention:
The aspect of giving individuals the opportunity to take their health into their own hands. Being able to open doors to them on how to take care of themselves. A lot of older residents want to get better but simply do not know how and this provides them with the resources to help themselves. (ID 067)
Gets more involved with regulars and frequent callers with conditions that can be looked at prior to 911 calls. Then referred as needed for an appointment with a doctor before hand before that next 911 call is placed. (ID 098)
Lack of CP-related training: Although CP was generally well received by paramedics, there were also issues and challenges. To gain further insight into these challenges and issues, paramedics were asked what they felt could be improved. The main theme was that paramedics perceived a lack of CP-related training.
Several paramedics voiced their frustration with the lack of training they received before they began practicing CP, and this was seen as detrimental to the program. Most paramedics received little to no training and indicated they would view CP as being more beneficial if additional training were to be offered:
The skills required to participate in a CP program are simple however different from what paramedics are now used to. I believe it's important to brush up on interpersonal skills when dealing with patients in a CP program. (ID 012)
I feel that the training could be more. I feel that the 1 to 2 hour training is not adequate to help it reach its fullest potential. I feel that there should be more training with paramedics being able to expand scope of practice for medication. (ID 053)
Education surrounding chronic disease management should be completed prior to any home visits or wellness clinic participation. Patients constantly seek advice on their chronic conditions and we do not have the training needed to educate them. (ID 143)
Wellness clinics: Paramedic responses related to their involvement in wellness clinics (n=45) were generally positive (Table 4). In particular, 86.7% (n=39) of respondents agreed that wellness clinics were acceptable to patients, while 61.4% (n=28) agreed that wellness clinics improved the wellbeing of patients. With respect to whether wellness clinics reduced the number of unnecessary EMS calls, 46.7% (n=21) of paramedics indicated that they agreed, while 24.4% (n=11) disagreed, and the remaining 28.9% (n=13) did not know.
Fear of service interruptions: Although involvement in wellness clinics was generally well received, many paramedics were concerned at the possibility of having to leave wellness clinic patients in order to respond to an emergency call. The risk of possibly having to abandon wellness clinics was perceived as a service interruption that impeded the success of the wellness clinics:
I find when we do wellness clinics we are still on shift and a few times we got a call while all these people were waiting for us and I find that completely disrespectful. (ID 012)
Should not be done by on line crews. The risk of being called away by 911 and leaving the wellness clinic abandoned is too strong. Should be completed by dedicated crew or light duty medic who is not responsible for 911 calls. (ID 219)
The fear of service interruption was perceived as lack of organization and detrimental to the quality of the CP program. Paramedics indicated the need for an improved system for managing wellness clinics that would mitigate having to leave to respond to an emergency call.
Home visits: The responses related to home visits (n=54) were generally positive (Table 4). The vast majority of paramedics indicated that they believed the home visits were acceptable to the patients (92.6% agreed, n=50), and that paramedics agreed they improved patient wellbeing (75.9% agreed, n=41). However, similar to the paramedic responses regarding wellness clinics, fewer paramedics agreed that the home visits assisted in reducing the number of unnecessary EMS calls, with 59.2% (n=32) agreeing, 22.0% (n=12) disagreeing, and 18.8% (n=10) indicating they did not know.
Need for improved electronic patient data tracking: Although paramedic perspectives related to their involvement in home visits were generally positive, the paramedics’ responses to open-ended questions indicated there was a need for better documentation and patient reporting for home visits. Paramedics indicated they would appreciate better electronic patient tracking as it would ease the burden of paperwork and data compilation after the call. An electronic patient data collection system would also provide information to enhance the delivery of services:
Better documentation standards, including the use of an electronic, retrievable form to track patient status (eg to discuss trends with patient during visit) [...] it's not an emergency, but it's still an ambulance call. It should be treated and documented as such. Consider these visits 'medical appointments' instead of just a vital-signs checkup. (ID 030)
Better tracking through same system as emergency calls. Patients consent to us accessing their history through EPCR [Electronic Patient Care Reporting] to create more seamless system. Expand regions served by CP and expand capabilities of CP. (ID 183)
These two paramedics expressed their frustration with a lack of adequate patient documentation and tracking when reflecting back on their home visits with CP-enrolled patients.
Discussion
It is evident from the questionnaire results that the majority of paramedics were positive when describing CP program overall. Many of the paramedics in this study worked in rural areas, where they balanced conventional paramedicine tasks, responding to emergencies with the newly assigned CP-related tasks. CP was officially launched throughout several districts across the province in April 2015, and the level of CP experience varied across the workforce; yet it was generally low, with sparse training. However, there were issues with CP that may have contributed to work-related dissatisfaction of paramedics. CP is in its infancy in Ontario, and limited available funding poses challenges for decision-makers and stakeholders to improve CP program training and management systems5. A fear of service interruption at wellness clinics and more efficient patient tracking software were issues that paramedics indicated will need improvements in the future.
The results indicated that PCPs were more likely to practice CP compared to ACPs, and that rural paramedics were more likely to practice CP than urban paramedics. However, the vast majority of PCPs who practiced CP came from rural programs, and EMS providers in rural northern Ontario typically have lower call volumes that allow more time for paramedics to practice CP compared to their urban counterparts; this is likely to be the reason for the low number of ACP responses.
Another potential limitation is the possibility of response bias related to paramedics’ preconceived attitudes towards CP. A number of paramedics did not fully complete the questionnaire, which could have presented a bias in the findings.
Findings in this study indicated that most paramedics who responded to the questionnaire (67.1%, n=50) who practiced CP were satisfied. This reflects previous research, which found that paramedic participation in extended roles led to increased job satisfaction because of more time spent with patients6,13. Conventionally, paramedics treat and operate in an emergency setting where there is often little opportunity to follow up with patients after they are assessed, treated and then transported to the hospital. CP allows paramedics to follow up on their patients, develop a professional relationship and oversee their recovery5.
Paramedics from this study indicated the need for additional training and/or education to assist them in practicing CP, and this is consistent with a recent CP study from Australia22. In most of the paramedic services participating in CP in the present study, paramedics received very little training to acquire the additional knowledge and competencies that may be required in CP (eg social determinants of health, mental health and additional medication information), and most CP-related training only occurred for a few hours.
Lack of training was also an important factor in CPs working in rural communities in Renfrew County, Ontario9. Specifically, researchers from that study found education in the areas of health promotion and prevention was lacking and needed to be enhanced to create opportunities for paramedics to engage in additional education that would further their clinical skills and expertise, particularly in areas such as health promotion and disease prevention9.
Currently in Ontario, paramedicine is highly regulated; however, there is no self-regulated college and the CP role and practices are not outlined in the Ambulance Act, the Basic Life Support Patient Care Standards or the Advanced Life Support Patient Care Standards2. The JDCF Framework, as described by Karasek (1979), demonstrates how increased decision latitude in an individual’s job duties is more desirable for their wellbeing23. If paramedicine was a self-regulated profession in Ontario, it could provide an increased sense of job control/decision latitude for paramedics24. Developing a job identity is still an issue that paramedics encounter; however, CP developments may contribute to the development of a paramedic profession25. A more clearly defined provincial CP framework and practice guidelines may also alleviate some challenges with what is expected of paramedics who participate in CP, and this is also important for ensuring safety standards8.
This study has several limitations. CP was only initiated in some areas for a few months before the questionnaire dissemination, and in these areas paramedics were only able to respond with limited participation and experience with CP-related duties. There was also a low response rate for a few EMS providers, and only a few paramedics (n=13) who practiced CP in larger urban centres; this makes it difficult to form generalizations regarding urban paramedic opinions related to CP. Additionally, paramedics labeled as practicing CP were defined as having had exposure to practicing CP, and not necessarily having experience practicing CP full-time. Therefore, some of the paramedics may only have had very limited exposure and experience with CP.
The present study’s strength was that it included paramedics from eight EMS providers, providing a broad cross-sectional perspective of CP programs in northern Ontario from frontline paramedics’ perspectives. Sinha (2012) identified a significant need to invest in the development and sustainability of CP programs to alleviate issues related to access to primary care1, and this study provides data to support this assertion. This study’s findings provide formative information to managers/supervisors, and community health stakeholders related to CP, with particular emphasis on potential areas of improvement to assist in ongoing program implementation and evaluation. There may also be several policy implications that emerge from this study, particularly related to changes in Ontario’s paramedic scope of practice. For example, recently there was a policy change to increase paramedic decision-making to provide patients with alternative care rather than be simply limited to direct transport to hospitals26.
Conclusion
This study adds to the growing knowledge base related to CP programs in northern Ontario. The findings provide a unique perspective from frontline paramedics, and they will inform future CP program developments. Recently, there has been an increase in CP funding across Ontario. CP is still a new approach that has shown promise for improving patient health and wellbeing, and there may be positive effects for paramedics as well. Even though the paramedics in this study had limited exposure to CP, the findings of paramedics who did participate in CP suggested that the workforce is receptive and believe that more paramedics should be permitted to practice CP (76.7%, n=65). Paramedics indicated they enjoyed how CP allowed opportunities to build professional relationships with patients and better promote patient health. However, paramedics practicing CP indicated that there is room for improvement related to improved training, mitigating service interruptions and implementing patient tracking software.
This study provided evidence to support recommendations to support the development of CP programs further because the majority of paramedics indicated that they found CP to benefit patient health and wellbeing. More research needs to be conducted to determine best practices of CP programs in other jurisdictions.
This study’s findings provide paramedic management professionals with information regarding program successes and areas for improvement for CP programming in the future that were unique in a northern Ontario context.