Context
Acute rheumatic fever (ARF) and its irreversible sequela of permanent, incurable heart damage known as rheumatic heart disease (RHD) are diseases of poverty. Poor environmental infrastructure including sanitation, overcrowding due to inadequate housing and inadequate access to culturally safe primary health care contribute to high rates of ARF in Australia’s Aboriginal and Torres Strait Islander peoples1. In Australia, ARF has been eradicated in affluent population groups, who have and continue to benefit from the country’s white, settler-colonial British history. Despite Australia’s adoption of the United Nations Declaration on the Rights of Indigenous Peoples, Australia’s Aboriginal and Torres Strait Islander peoples are pointedly excluded from positions of power and lack meaningful control over their own circumstances and life choices2.
In November 2020, this journal published the experiences of eight authors who introduced off-label oral sedation with a centrally acting alpha agonist medicine (clonidine) to the management of three Aboriginal children3. Having had prior episodes of ARF, each of these three children had been prescribed long-term intramuscular (IM) penicillin for secondary prophylaxis (SP) to prevent future ARF recurrences. While this sedation was performed with parental permission, the clinical case report raises four critical issues that we consider in response.
Issue
What is the evidence for secondary prophylaxis?
As evidence-based decision-makers are aware, systematic reviews to synthesise the entire extant evidence are gold standard inputs to the process of decision making. The most well known clearing house for systematic reviews conducted to the highest standard is the Cochrane Library. A systematic review of all rigorous evidence underpinning the use of antibiotics in SP in preventing recurrent ARF as primary outcome was originally conceptualised by Manyemba and Mayosi in 2000 and subsequently published in 20024. Regular updates in 2005, 2007 and 2009 obtained no new evidence4. In 2013, those authors advised Cochrane Centre that the review would no longer be updated. We ourselves have found no more recent randomised clinical trials comparing SP regimens to prevent recurrent ARF for patients with initial ARF. The authors of the original systematic review found three trials comparing either oral or IM penicillin with placebo; four trials comparing oral with IM penicillin but no placebo group; one trial comparing three-weekly IM with four-weekly IM penicillin without placebo group and one trial comparing two-weekly IM with four-weekly IM penicillin also without placebo group. No study was ‘properly randomised’4. Those authors also noted that the methodological quality of research articles was so poor that a conventional meta-analysis was not possible. Table 1 shows the denominators in each trial’s prescribed group, the number and proportion experiencing the primary outcome of one or more episodes of recurrent ARF, ranked from least to worst recurrent ARF results. Both the best and worst trial results were demonstrated in groups receiving IM penicillin (Table 1). Specifically, the highest rate of ARF recurrence, at 24%, was demonstrated in a group receiving four-weekly IM penicillin4.
While those authors surmised that ‘Taking tablets is easier but might not work as well as injections’4, they nonetheless presciently offered four recommendations:
- In view of the poor quality of the available evidence, well-designed randomised controlled trials comparing the effectiveness of penicillin injections with oral phenoxymethylpenicillin are required.
- There is still a need for well-designed multi-centre randomised controlled trials to compare 2-weekly, 3-weekly and 4-weekly penicillin injections.
- Regarding the safety of intramuscular penicillin, there is need to set up surveillance and adverse drug reactions monitoring systems.
- Patients with rheumatic fever and their families should be involved in discussions to set research priorities that answer questions relevant to their needs4.
Regrettably, these recommendations went unheeded. Medical opinion settled emphatically on IM penicillin, perceiving the IM route as ‘… the cornerstone of the long-term management of patients with ARF’5-7. Indeed, oral regimens are not to be recommended ‘except in exceptional circumstances’8. Australia’s peak health data intelligence agency, the influential Australian Institute of Health and Welfare, is among many to reproduce, as recently as 2021, the position that SP with IM penicillin is ‘… the only RHD control strategy shown to reduce recurrences, delay progression, and be cost effective at community and individual levels’9.
This claim of cost-effectiveness was not the only sentiment to take hold. Noting that ‘Some health services prefer to administer BPG [benzathine penicillin G] on the same day every month, rather than every 4 weeks’, the second edition of Australia’s national ARF guidelines produced in 2012 stated that a calendar month regimen was ‘… an acceptable alternative’ to a 28-day IM penicillin SP regimen to promote adherence10. Yet nationwide contemporaneous clinic data showing that only 27% of those prescribed IM SP on 28-day regimens received more than 80% of their required prescribed SP was identical to that of those on monthly regimens (also 27%)11. This second edition of Australia’s national guidelines had also failed to acknowledge that repeated IM injections with a viscous fluid every 28 days could be painful12. In their clinical case report, Mitchell and colleagues3 directed readers to the revised third edition, which states, ‘Sedation may be necessary when distress remains significant despite using other measures to manage pain, fear and distress’13. This third edition also cautions that clonidine (the sedative used in oral form in the case studies) has adverse effects including hypotension and atrioventricular block13. Clonidine may be contraindicated in those with RHD13.
Table 1: Ranked outcomes from nine trials included in a systematic review of randomised clinical trials comparing SP regimens to prevent recurrent ARF for patients with initial ARF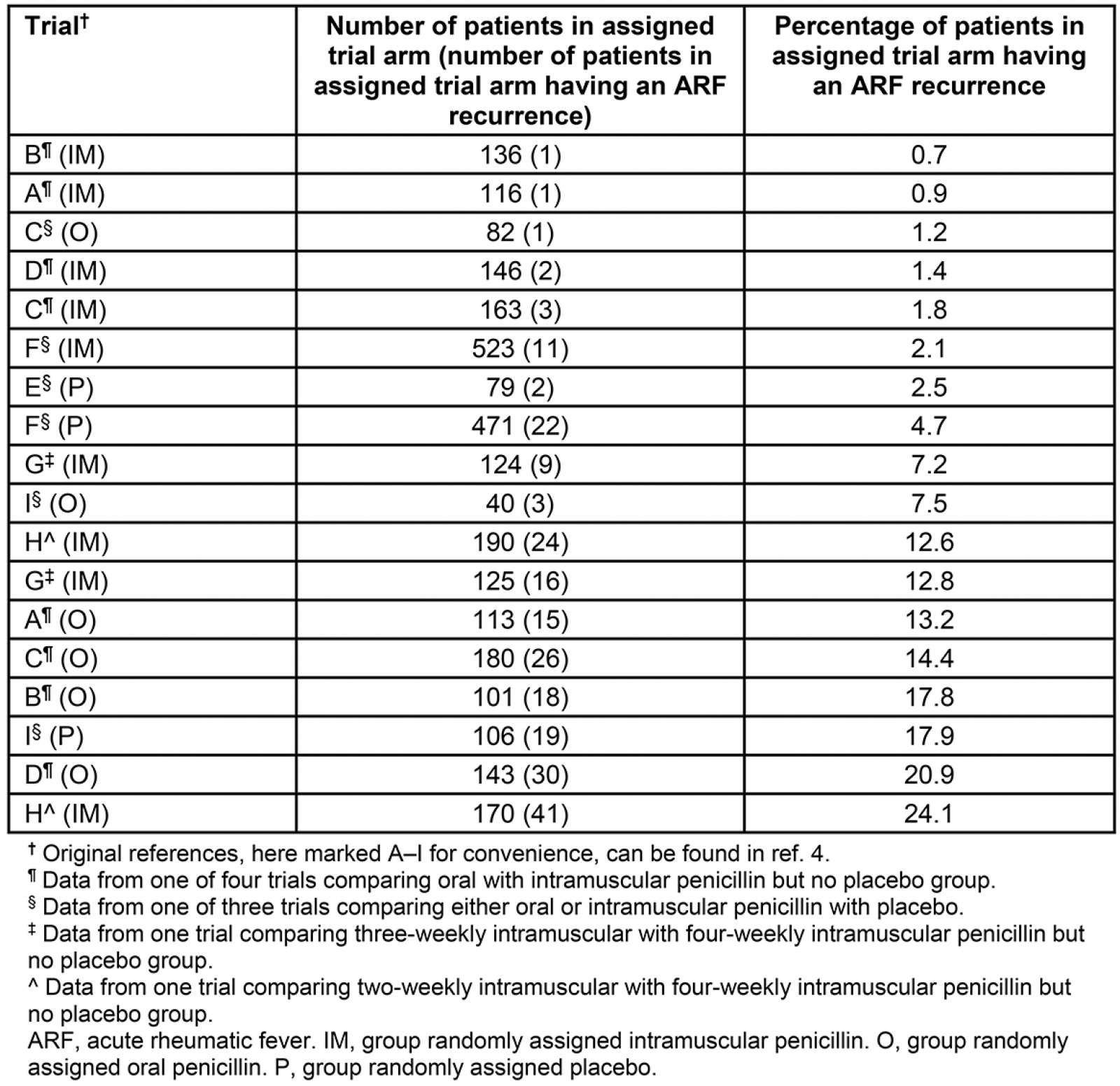
What happens on the ground?
Since 2009, the Australian Government has spent $54 million on an unwritten rheumatic fever strategy including significant allocations to establish RHD registers with mandatory centralised reporting and monitoring of SP provision in four state and territory jurisdictions in which ARF is endemic among Aboriginal and Torres Strait Islander peoples. Governance for these RHD registers is unclear and, as government bodies, the policies are rarely controlled or overseen by Aboriginal and Torres Strait Islander peoples. In turn, data from these RHD registers as submitted and analysed by the Australian Institute for Health and Welfare persistently demonstrate that SP provision on the ground is suboptimal9,14. Across the country, 33% of those Aboriginal and Torres Strait Islander peoples with ARF or RHD receive less than half their prescribed annual SP regimen9. This percentage has barely budged since the inception of centralised RHD registers, widely touted as the investment necessary to improve SP performance9,14,15.
In 2019 (the most recent year for which data are available), more than 1300 Aboriginal and Torres Strait Islander peoples received less than 50% of their prescribed IM SP doses9. About 25% of notifications to Australian RHD registers are for recurrent episodes. National Continuous quality improvement programs and localised cluster randomised trials have not lifted SP performance16-18. Anecdotal feedback to us from parents and guardians of children with ARF in the remote Kimberley region of north-western Australia is instructive. Rotation of injection sites for long-term IM regimens is critical. Life cycle transition from childhood to adolescence is turbulent and challenging for optimal SP regimen provision. We hear constantly that family engagement using up-to-date resources led in their development by Aboriginal and Torres Strait Islander peoples including videos, and direct personal support based on sustained relationships, must be improved.
Who ‘problematises’ acute rheumatic fever and the delivery of prescribed secondary prophylaxis?
Studying problematisation reveals what is taken for granted, what is assumed and who is winning the political and polemical battles ranging from abstract concepts to material resource allocation19. Deep reflection through the study of problematisation also alerts researchers to their ‘unavoidable participation’ in deeper hegemonic dynamics of structural disadvantage19.
Despite more than 40 years of academic publications about ARF and RHD, the number of studies led by Aboriginal and Torres Strait Islander peoples as evidenced by first authorship in publications is minuscule. By contrast, large mainstream institutions shape the academic questions deemed important to be answered and the expertise necessary to design and conduct research. Their biomedical interests are advantaged in the process. Fifty-nine clinicians interviewed as part of a cluster randomised trial that was unsuccessful in changing SP regimen provision revealed not only the distress caused to patients by IM injections but also their own distress in administering these injections20. These clinicians revealed good knowledge of pain reduction measures yet, paradoxically, offered them inconsistently. The study’s authors identified that repeated, painful procedures in children necessitate well-planned and child-focused primary health care. While concluding initiation of long-term SP regimens of IM injections every 28 days was ‘a special event requiring expert input’, little specific advice for practice was communicated20.
Elsewhere, a ‘decolonising approach’ to service provision has been recommended ‘… to improve shared decision making and alleviate power imbalances between clinicians and Aboriginal patients’21. This aspiration remains abstract unless non-Indigenous service providers and researchers relinquish their own preoccupations and, instead, return to reconceptualise the problematics inherent in the current narrowly cast evidence base and become more willing to share, discuss and submit to Indigenous epistemic priorities, methodologies and solutions, no matter how challenging22,23.
What do Aboriginal and Torres Strait Islander peoples deserve to know?
Anecdotally, there is insufficient education of families and knowledge sharing proportionate to the lifelong sequela of ARF and the rationale for so many years of SP. The quality of preparation and support for families and communities to learn about the natural history of ARF and the effectiveness of alternative approaches is unstudied. Colleagues in the front line of primary health care are unable to dedicate contact and conversation to engage and educate families. Without this foundation, SP regimens, especially when painful, make little sense. It is also unknown whether – and how – the Aboriginal and Torres Strait Islander families of children with ARF are apprised of the evidence comparing oral and IM administrative routes for penicillin before IM regimens are commenced. As shown in Table 1, we have equipoise and an obligation to co-design a decision aid to underpin shared understanding and decision-making based on extant evidence24. Family education that is generous, open, iterative, patient and culturally safe will answer the questions and concerns of Aboriginal and Torres Strait Islander families. This is no cheap fix. Health professionals will need upskilling and resources to support informed consent. Aboriginal Health Workers and Aboriginal Health Practitioners bring cultural expertise and content knowledge, deserving greater acknowledgement as integral members of the primary health care team in this complex task. Community support and education help destigmatise SP and reduce family isolation.
We surmise that non-Indigenous families would receive more information about options for SP, including the comparative evidence for daily oral penicillin. Yet we found no decision aid for Aboriginal and Torres Strait Islander families rooted in evidence that would pass international standards and support effective decision making25. There has been a cavernous vacuum in the development of culturally responsive, evidence-based decision aids for critical therapeutic choices26,27. There has been scant attention in the medical literature to Aboriginal and Torres Strait Islander perspectives with scholarship led by Aboriginal and Torres Strait Islander first authors. We recommend a significant shift in this regard by those with power and resources. If anxiety among clinicians to present both oral and IM penicillin as alternatives with quantified benefits and risks is too high to pursue such an initiative, then at the very least a decision aid for parents whose child has received less than 40% of prescribed IM SP in the past 12 months to revisit oral penicillin as an option has merit. Having 40% or less of prescribed IM SP is incontrovertibly all pain and no gain28. Elsewhere, oral penicillin is more readily sustained29. There are many hundreds of Aboriginal and Torres Strait Islander children in this situation. We strongly encourage shared evidence-based decision making comparing options and structuring discussions about values, benefits, harms and trade-offs. Resources co-designed through Aboriginal and Torres Strait Islander leadership should be developed accordingly and issued to frontline clinicians before escalating clinical management to drastic scenarios such as off-label oral sedation.
Lessons learned
In this complex policy and practice context, Mitchell and colleagues reported three cases to illustrate off-label use of a centrally acting alpha agonist sedative to implement SP regimens in remote settings. In response, our reflections identify how influential biomedical problematisation of SP provision continues to camouflage deeper, unassuaged political and relational disparities for Aboriginal and Torres Strait Islander peoples in daily health care. Issues pertinent to successful SP provision such as evidence-based informed consent, SP options and research priorities must be reframed and led by Aboriginal and Torres Strait Islander peoples. Later this year in Broome, two Aboriginal authors will facilitate a women’s gathering to listen to community-generated ideas for sharing evidence and further action.
Acknowledgements
We acknowledge all Aboriginal and Torres Strait Islander people and leaders past, present and emerging, and respect their continuing relationship to the land and waters. We also acknowledge that the benefits now enjoyed by some as a result of European colonisation of Australia have meant incalculable suffering for others. We thank Ms Stefanie Oliver, pharmacist and PhD scholar at the University of Notre Dame, for insightful comments on earlier drafts.