Introduction
Hospital-acquired (nosocomial) influenza is a concern for many health organisations and policymakers around the world, as it presents a threat to both healthcare service provision and inpatient outcomes1. The risk is heightened for hospitalised patients, who are often older with existing comorbidities, making them more vulnerable to infection2.
Influenza is highly infectious, thus effective management of inpatients with this illness in order to minimise nosocomial infections is crucial. Isolating respiratory infectious patients within the inpatient hospital setting should be a key priority given the current COVID-19 crisis, as both viruses are transmitted by contact, droplets and fomites3.
Australian rural and remote health services have fewer resources, as well as chronic workforce shortages4. The demand for health services is highlighted in rural areas due to an increasing ageing population with chronic and complex chronic disease, and it is exacerbated by limited health services organisations and remoteness4. This scenario adds burden to hospital resources during influenza season and can result in a somewhat reactionary bed management system, as bed transfers are used as one of the primary strategies to manage hospital bed block5.
Reactionary bed management results in placement of infectious patients into any ward initially where there is a bed available, which then requires relocation of other patients5. This is especially an issue in rural and remote hospitals where there may be limited or non-existent specialty beds or wards specifically for respiratory illnesses. Placement of infected patients amongst non-infectious patients increases the risk of nosocomial spread.
All of these bed transfers have a significant impact on the workloads of both nurses and cleaning staff. Initial suboptimal patient bed placement exacerbates the demands placed on an already chronically understaffed rural clinical workforce5,6.
This article presents findings on bed management practices for influenza patients admitted to a rural referral hospital.
Methods
This quantitative retrospective descriptive case study examined the relationship of nosocomial influenza infections and organisational bed management. A review of clinical cases, nursing and cleaning staff workloads was conducted during the influenza seasons for 2016 to 2019.
Setting
The study setting was a rural referral hospital in New South Wales, Australia with 282 beds, providing acute care services to a population base of 77 029, with 25.5% aged 60 years or greater7. The hospital consists of an intensive care unit, four acute care wards (coronary care unit, one medical ward, two surgical wards) and one subacute rehabilitation ward. An escalation unit, comprising 26 beds, is only operational when the hospital is nearing bed block.
Participants
Participants were adult inpatients with a diagnosis of either community-acquired influenza (on admission or within 48 hours of admission) or nosocomial influenza (defined as a positive swab after 3 days in hospital)8. Patients diagnosed with influenza were considered to be infectious for a period of 7 days according to district guidelines. Inpatients aged less than 18 years were excluded as they were placed in the children’s ward and not moved throughout the hospital during their admission.
Data collection
Retrospective data were collected over four peak influenza seasons (July to September each year) for the years 2016–2019. Two clinical databases were used to track influenza cases and bed movements of patients throughout the hospital.
In addition, retrospective data was collected from existing cleaning logbooks, which provide a record of the cleaning time of infectious rooms, known as terminal cleans, after patient transfers or discharges.
Informal observations were made by nurse educators to record the length of time required by staff for a regular bed transfer. The informal observational review was performed to quantify the time reported by the nurse educators with the time noted in published studies by Blay9.
Statistical analysis
Data were analysed using descriptive statistics. Differences of categorical data were tested using Pearson’s χ2 test or Fisher’s exact test. Differences of continuous variables were detected using the Mann–Whitney U-test after the normality test. A p-value of less than 0.05 is considered to be statistically significant and all p-values are two-tailed.
Ethics approval
The project was reviewed by the local human research ethics committee and was classified as negligible risk research activity (AU202005-09).
Results
Patient characteristics
A total of 229 patients had a diagnosis of either type A or type B influenza during the study period. Of those, 86.9% of patients had community-acquired influenza and 13.1% were nosocomial cases.
Table 1: Overview of patient characteristics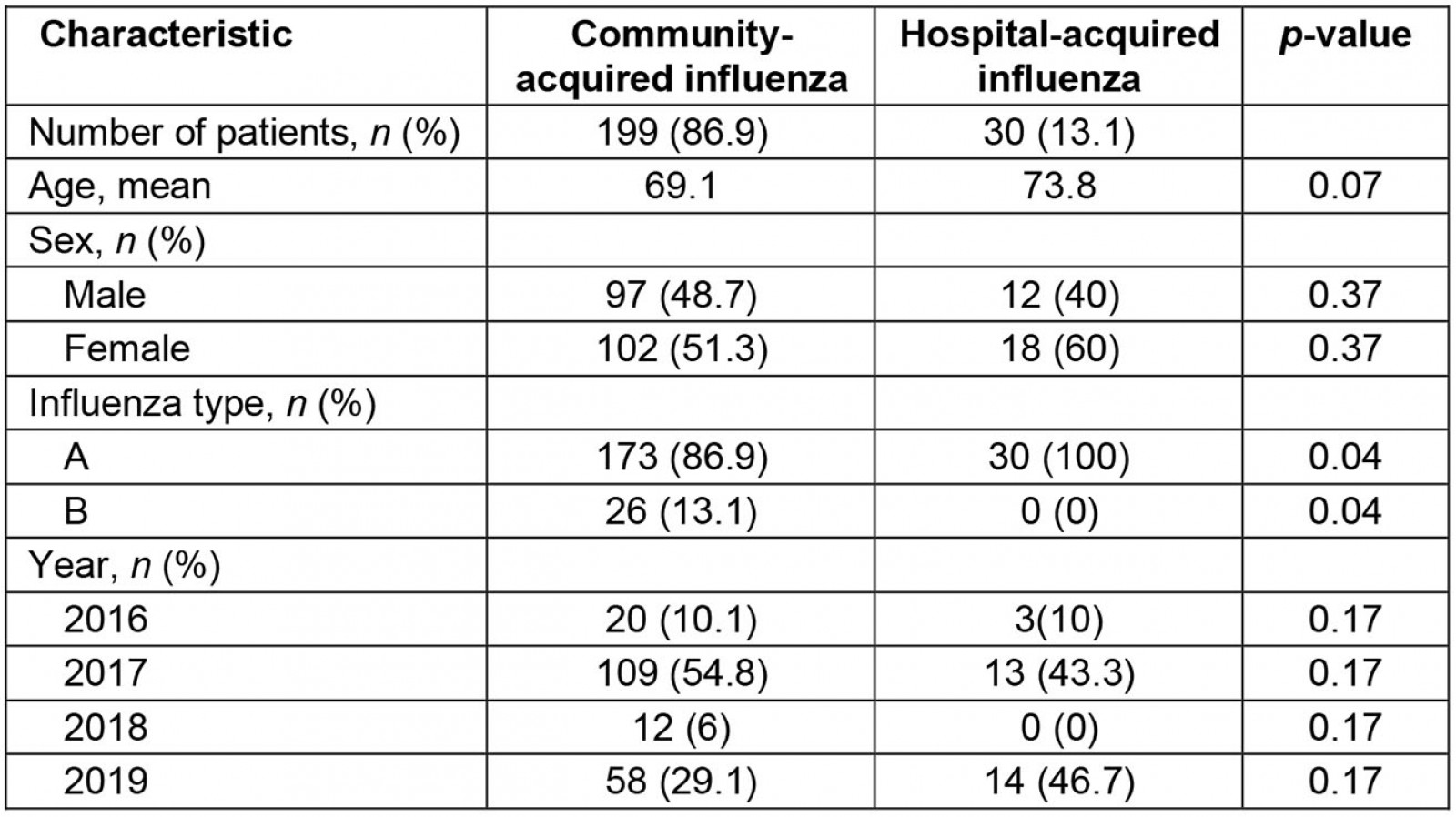
Bed transfers
As shown in Table 2, of the 199 patients admitted with community-acquired influenza, more than 40% (n=85) were subsequently transferred elsewhere from their admission bed during the infectious period. The initial admission of patients from the emergency department bed to a ward bed was not counted as a transfer.
Of 30 patients who contracted influenza in hospital, 70% (n=21) were transferred from one bed to another during their infectious period.
Of the patients who did get transferred during the infectious period, some were transferred more than once (Fig1).
Table 3 shows different types of transfers during the patient’s infectious period. It was noted that 85 patients with community-acquired influenza were associated with 142 bed transfers. This included 50% of patients being transferred to another ward (interward) and the other half being transferred within the same ward (intraward).
Table 2: Patients transferred with community- and hospital-acquired influenza at a rural hospital, New South Wales, July–September 2016–2019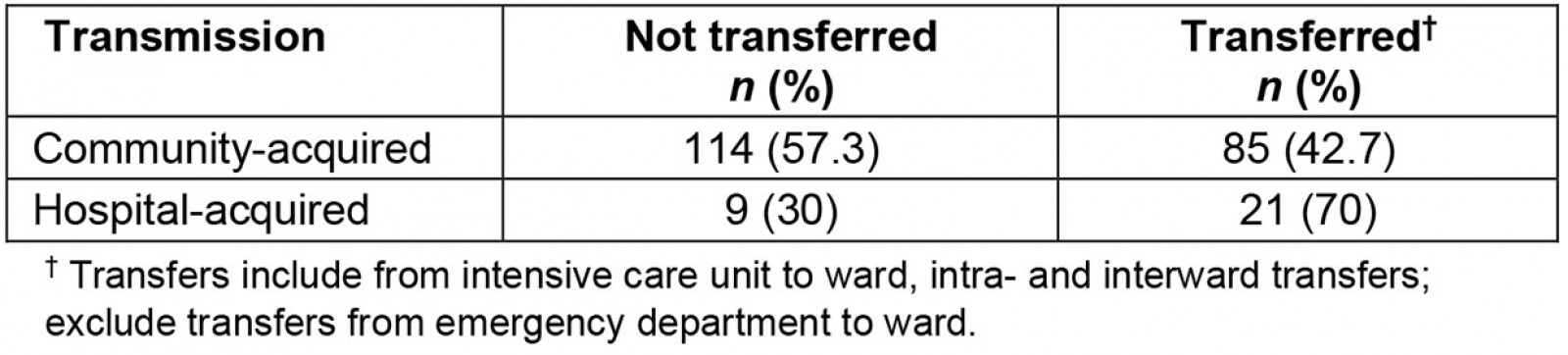
Table 3: Intra- and interward transfers during patients’ infectious period at a rural hospital, New South Wales, July–September 2016–2019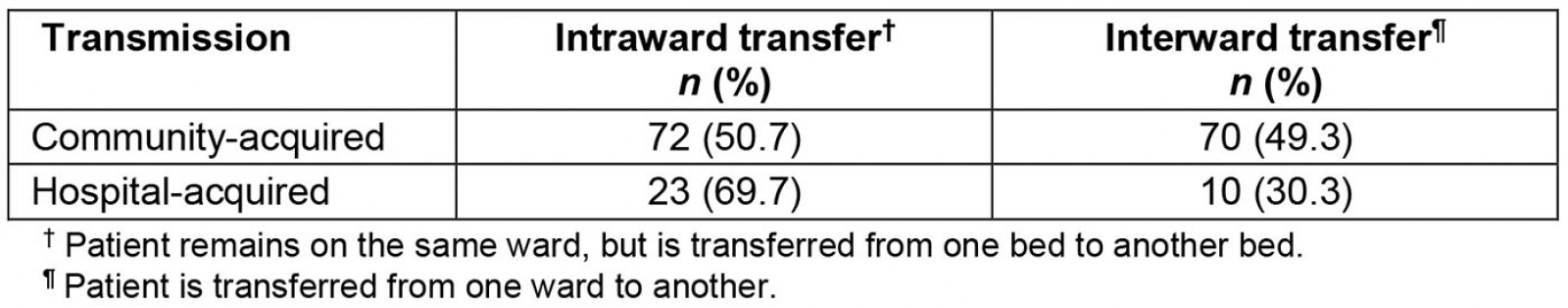
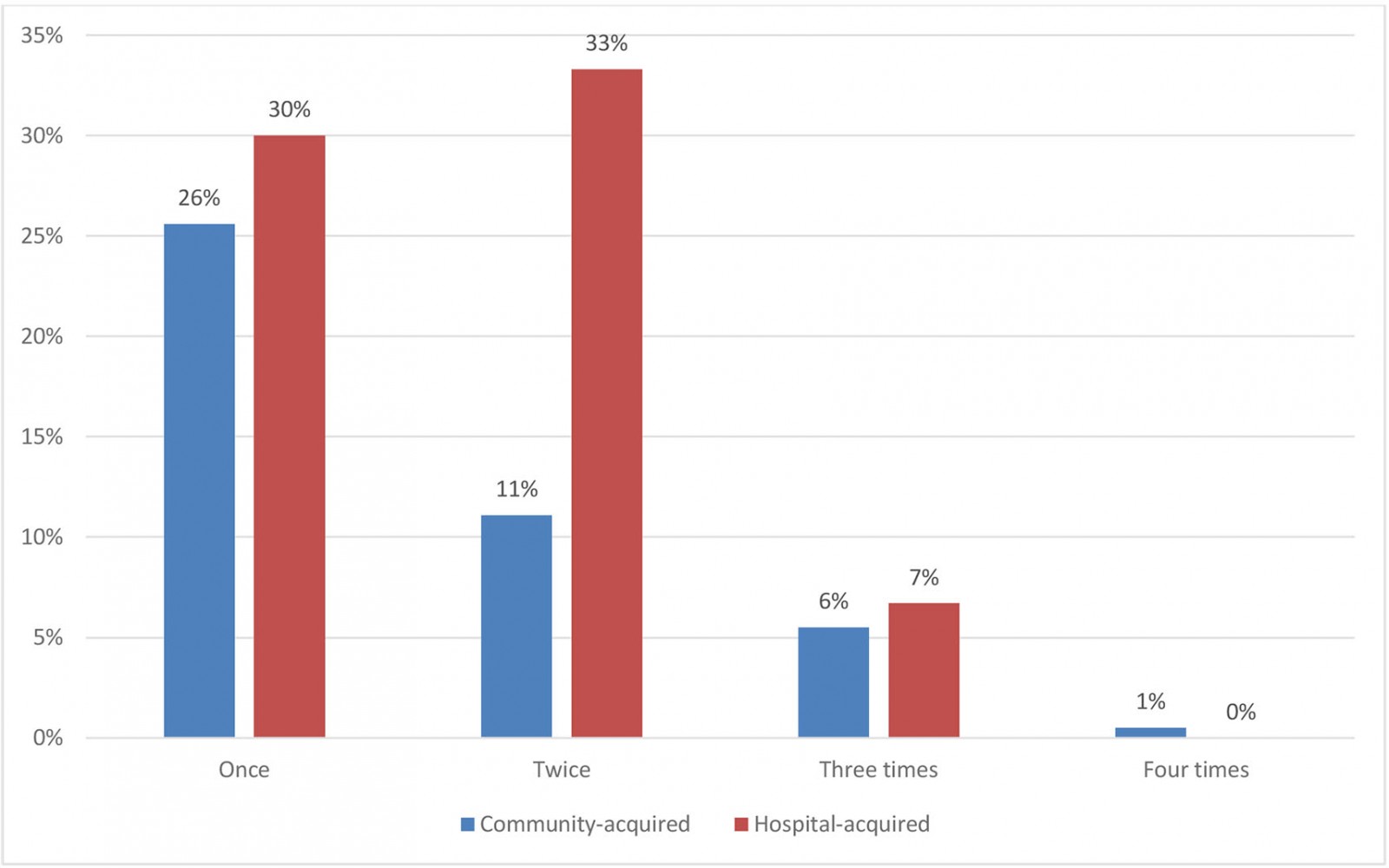 Figure 1: Transfers per patient with influenza (during infectious period) at a rural hospital, New South Wales, July–September 2016–2019.
Figure 1: Transfers per patient with influenza (during infectious period) at a rural hospital, New South Wales, July–September 2016–2019.
Staff hours related to bed transfers
The large number of transfers required significant amounts of clinical hours from nursing and cleaning staff to facilitate the transfer and to perform terminal cleans, respectively. Informal observation found that it took an average of 46 minutes of nursing time to facilitate one patient transfer. This is comparable to the literature, which shows that each transfer requires an average of 57.5 minutes to complete9. The audit of the cleaning logbook indicated that each terminal clean took an average of 38 minutes. This equates to 84 minutes of combined staff time being required for each inpatient transfer, with a total of 245 staff hours to facilitate all 175 transfers (which only included patients with influenza) over peak influenza seasons in the past 4 years.
Discussion
Findings from this study provide an overview of inpatient characteristics with influenza, the bed transfers experienced by these patients, and the impact on the staff workloads in a rural hospital. The report of 13.1% nosocomial transmission in this study is almost twice that of the 5.6% (96 of 1722 patients) reported in Godoy et al’s study10.
This high rate of nosocomial infection may be linked to a high incidence of bed transfers at the study hospital as suggested in the literature9,10 and is corroborated by the number of bed transfers occurring, especially during 2017 and 2019 influenza seasons.
Ideally, community-acquired influenza patients should occupy a maximum of one bed during their stay. Optimal management of nosocomial influenza inpatients should include the occupancy of a maximum of two bed locations during their stay: the first bed assigned on admission (presumably having been diagnosed with a non-influenza-like illness), and the second after they have been moved in light of their influenza diagnosis, and only if required. Unlike tertiary and metropolitan centres, where patients are often admitted to a specialty ward and kept there for the duration of their admission, this is not possible in rural and remote centres due to reduced numbers of specialty beds available and high rates of non-infectious chronic disease4,11.
With the limited specialty bed numbers within the hospital, there is a need for bed management practices that aim to reduce influenza transmission and bed transfers within the hospital. This is critical, especially during the active phase of infection for patients admitted with community-acquired influenza, as a reduction of these transfers will decrease the risk of nosocomial infections.
Findings from this study provide valuable insight into the rural hospital bed management practices (transfers in particular) for inpatients with influenza and the consequences associated with these transfers. This information will inform future development of an optimal bed management plan for surges of influenza and other highly infectious respiratory illnesses outside of metropolitan centres.
Limitations
There were some limitations to this study. One is the small sample size, secondary to the limited duration, of July to September for the previous 4 years. These 3 months each year usually showed significant overlap, with increased periods of bed block due to the higher number of patient admissions during the winter months in Australia.
Conclusion
This study highlights the need for a formalised bed management plan that limits the number of bed transfers for infectious influenza inpatients in rural locations. There are a large number of inter- and intrahospital transfers of community-acquired influenza inpatients occurring during the infectious phase of the disease, and after diagnosis. These transfers are associated with increased risk of nosocomial influenza infection, with each transfer adding an increased burden to the workload of both nursing and cleaning staff and reducing the time nurses are able to spend to provide care for their patients.
Recommendations
It would be beneficial for rural and remote facilities to develop and implement an organisational bed management strategy that aims to reduce the number of intrafacility bed transfers of patients who have confirmed influenza, especially during the 7-day infectious period. A strategy that incorporates a designated respiratory ward (if possible) or expansion of hospital-in-the-home services would assist in decreasing intraward and facility transfers, reduce burdens on workloads and limit further exposures of healthcare staff.

