The COVID-19 pandemic has devastated communities around the world, and within Australia there was particular concern about the impact on Aboriginal and Torres Strait Islander communities given the disproportionate impacts of previous pandemics on Indigenous peoples1. Despite these concerns, Aboriginal and Torres Strait Islander people have had decreased rates of infection, morbidity and mortality than the general population through thorough health planning, strong leadership and the principles of self-determination within certain communities2,3. Aboriginal Community Controlled Health Organisations (ACCHOs) have taken on leading roles with health communication to the respective communities they serve to best promulgate the relevant information about COVID-19 in a culturally safe and appropriate manner4.
The COVID-19 pandemic has forced federal and state governments to change guidelines and legislation to combat an evolving health crisis. Within our ACCHO in Bendigo, Victoria, it was determined that the best manner in which to inform our local Aboriginal and Torres Strait Islander community was by ACCHO’s Aboriginal health practitioners providing education about immunisations and also administering the immunisations when they were available, a process known as ‘clinical yarning’5. Currently, Aboriginal health practitioners are not mentioned within the Drugs, Poisons and Controlled Substances Act 1981 (Vic), thereby rendering them unable to administer scheduled medications, immunisations and injections. This is despite Aboriginal health practitioners undergoing specialised training in immunisations and medication administration and formal Ahpra recognition. Interestingly, the scope and practice of Aboriginal health practitioners is largely dependent upon the state in which the practice is located.
In February 2021, a Public Health Emergency Order was issued under Section 22D under the Act to allow Aboriginal health practitioners to administer COVID-19 immunisations in Victoria.
The Bendigo & District Aboriginal Co-operative (BDAC) made the decision that for the COVID-19 vaccination program to be impactful it would need to be led, managed and administered by our Aboriginal health practitioners to ensure community confidence and increase the vaccination rate among the local Aboriginal and Torres Strait Islander community. BDAC has 918 active patients deemed eligible for a COVID-19 vaccine and, of that eligible cohort of patients, 662 identify as Aboriginal and/or Torres Strait Islander.
BDAC has vaccinated a total of 594 patients over a 6-month period, amounting to 59.2% of active eligible patients aged 15 years and over, with 465 of those patients identifying as Aboriginal or Torres Strait Islander or 70.2% of the eligible Indigenous population. A total of 327 patients have received two doses of their COVID-19 vaccine, equating to 49.4% of eligible Aboriginal and Torres Strait Islander people now fully immunised. In comparison, Victoria recorded 48 479 (44.8%) first doses and 32 165 (29.7%) second doses of a total eligible population (Aboriginal and Torres Strait Islander people aged 15 years and over) of 108 329. Looking at other Australian states, Queensland has administered 75 397 vaccine doses to Aboriginal and Torres Strait Islander people aged 15 years and older, with 47 080 (26.8%) first doses administered and 28 317 (16.1%) second doses administered to an eligible population of 175 834. Western Australia has administered 14 854 first doses (20.6%) and 8053 (11.1%) second doses to an eligible Aboriginal and Torres Strait Islander population (aged over 15 years) of 72 403 people6 (Fig1).
These figures compare with overall COVID-19 vaccination rates (at the same timepoint) in Victoria of 62.5% of the eligible population (>15 years) having had a first dose and 38.8% having had a second dose of vaccine. In Queensland, 54.3% of the eligible population (>15 years) had received a first dose and 35.8% had received their second dose, and in Western Australia 54.8% and 35.7% had completed their first and second doses of COVID-19 vaccine, respectively7. These data show that BDAC’s vaccination rates are higher than the Victorian average for COVID-19 vaccination despite overall trends showing that, in general, Aboriginal and Torres Strait Islander people have lower vaccination rates than the general population.
Often Aboriginal and Torres Strait islander people feel more comfortable within an ACCHO and engage with the organisations more frequently for their healthcare and other supports and interventions. ACCHOs allow for Aboriginal and Torres Strait Islander people to feel safe culturally, and confident that the quality of care they receive is of a high standard, with specialised healthcare approaches being implemented and designed around their demographic. Aboriginal health care focuses not only on the individual but their family and their community. Aboriginal health practitioners play an instrumental role in this approach to health care, tackle the stigma around Aboriginal and Torres Strait Islander people and challenge mainstream approaches. Having these specialised and trained Aboriginal health practitioners allows Aboriginal and Torres Strait Islander people to access appropriate and holistic health care and social supports without judgement and without systematic racial stigma.
The recent COVID-19 pandemic has shown how effective ACCHOs have been in managing a deadly pandemic amongst a vulnerable population group. The Aboriginal and Torres Strait Islander community knows how best to administer specialised health care, health promotion and health interventions to its members, and this is a key plank to self-determination. Often there is a lack of appreciation of the intricacy and complexity of the care being delivered within ACCHOs. The data here has shown how effective Aboriginal health practitioners can be in disseminating complicated information to patients and increasing vaccination rates among the population that they serve. The high uptake rates of COVID-19 vaccine at BDAC have only been made possible by the leadership taken by the Aboriginal health practitioners. It would be beneficial going forward to continue to see Aboriginal health practitioners able to administer medications, immunisations and injections to community in a culturally appropriate and safe manner in Victoria. This will contribute to a rise in immunisation rates and for the Aboriginal and Torres Strait Islander community to have regular and consistent dosing of their other medications, which again could improve morbidity and mortality within the community and further aid in the goals of closing the gap in Aboriginal life expectancy. These results also highlight the importance of involving First Nations people worldwide in the development, implementation and evaluation of health interventions involving them, and how effective these interventions can prove to be.
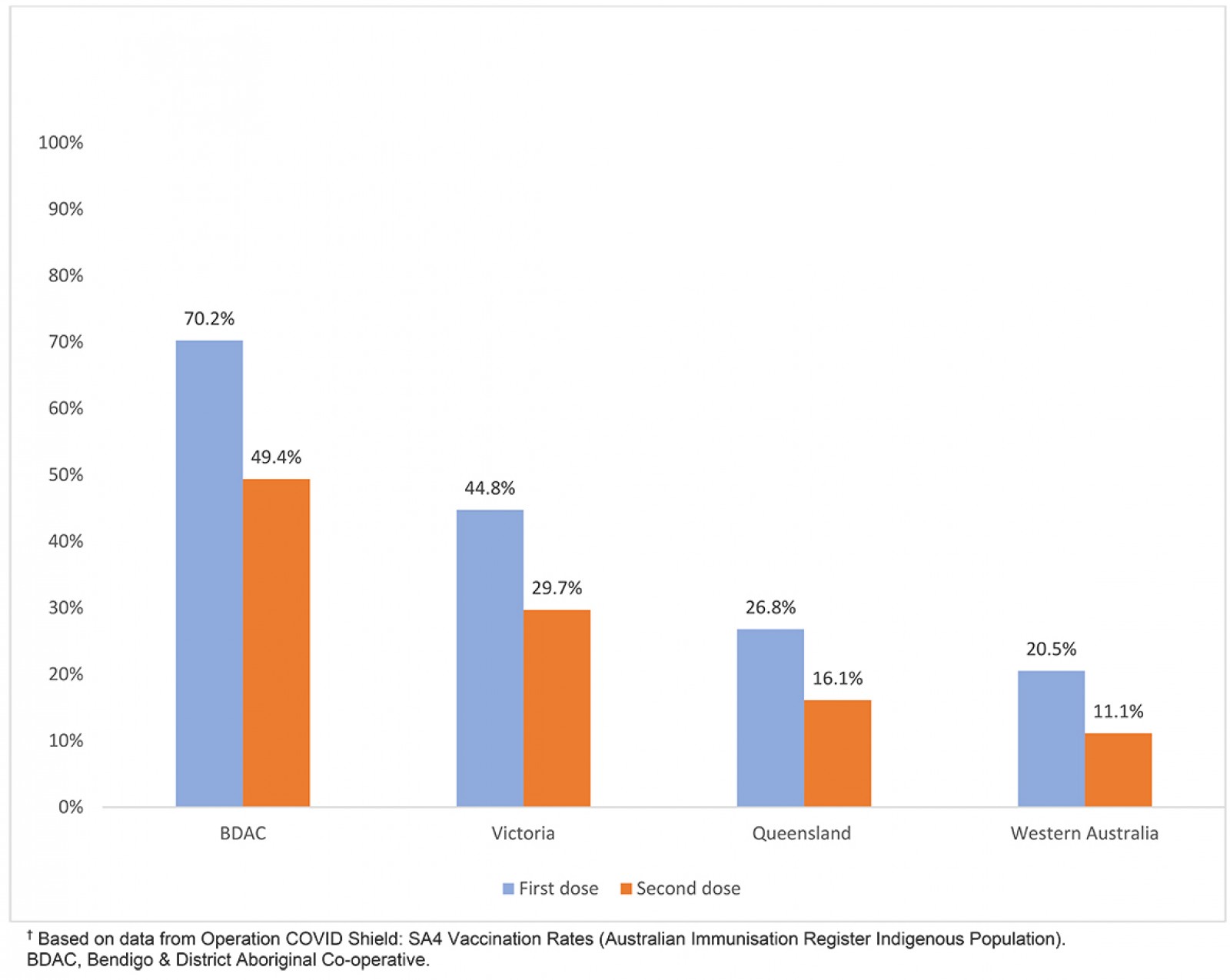 Figure 1: COVID-19 vaccination rates for Aboriginal and Torres Strait Islander people at Bendigo & District Aboriginal Co-operative and in Victoria, Queensland and Western Australia, 8 September 20216.
Figure 1: COVID-19 vaccination rates for Aboriginal and Torres Strait Islander people at Bendigo & District Aboriginal Co-operative and in Victoria, Queensland and Western Australia, 8 September 20216.
Acknowledgements
We thank our patients at Bendigo & District Aboriginal Co-operative who continue to seek care from us during COVID-19.
References
You might also be interested in:
2012 - Remote supervision of health professionals in areas of workforce need: time to extend the model?



