Introduction
The sudden advent of the COVID-19 pandemic in early 2020, and New Zealand’s ‘go hard and go early’ lockdown, led to mental and economic stress for many people. A survey conducted during that period found increased risks of anxiety, psychological distress and low wellbeing1. There was also evidence of resilience, with increased family connections, pride in the ability to cope, and a heightened sense of community for many New Zealanders1. A study of wellbeing during the lockdown found that many New Zealanders reported benefits in terms of coping well, maintaining their health, and using the time for reflection and self-development2. Other evidence of resilience includes increased time with family and a quieter, less polluted environment1.
Lockdown was particularly hard on those with pre-existing mental health issues, who demonstrated about twice as much psychological distress, anxiety and poor wellbeing compared with the general population3. Loss of work from the pandemic has also been shown to be associated with mental health problems4. A New Zealand study conducted during the April–May 2020 lockdown found that healthcare and other essential workers had increased risk of anxiety compared with non-essential workers5. Healthcare workers were self-identified, with no details on the nature of the care they delivered.
Frontline general practices were particularly hard hit by the sudden lockdown. They had to minimise their face-to-face consultations, and triage patients with COVID-19 symptoms or at higher risk, into a ‘red’ stream. The red stream patient cohort were kept separated from non-respiratory patients and managed by a dedicated ‘red stream’ practice team wearing personal protective equipment. Government funding was slow. As patient numbers plummeted, it was reported that general practitioners (GPs) were losing their jobs or working for free6. Practices had to quickly implement alternative forms of consultations. Guidance given to general practices by the Royal New Zealand College of General Practitioners during the COVID-19 pandemic was that they should switch to telehealth consultations and provide fewer face-to-face consultations. The proportion of face-to-face consultations expected of practices varied according to the alert level.
While increased strain is likely to occur in general practice due to the pandemic, it is unknown whether the levels of strain would differ according to rurality. The aim of this study is to assess the strain on practices experienced from the effects of the COVID-19 pandemic, and to ascertain whether this differed between urban and rural locations.
Methods
The overall project is a four-country collaboration (New Zealand, Australia, USA, Canada) involving repeated cross-sectional ‘quick’ surveys of primary care practices in each country (Appendix A). The methods have been described in previous work outlining primary care practices’ concerns around the New Zealand border7. While each country used very similar surveys – especially Australia and New Zealand, which developed theirs in parallel, contextual differences meant that there was some variation in the questions and the frequency of surveys. The survey series from each of the countries was standalone.
In New Zealand the results were rapidly analysed and fed back to the sector, policymakers and the media. The New Zealand branch of the project included dissemination of survey links through professional primary care organisations as well as snowball recruitment. The organisations involved in dissemination of the links included the Royal New Zealand College of General Practitioners (RNZCGP), Royal New Zealand College of Urgent Care, General Practice New Zealand, the Rural General Practice Network, the Practice Managers and Administrators Association of New Zealand as well as several other groups such as primary care organisations and private medical Facebook groups. Participants were also invited to pass the survey links on to colleagues (snowball sampling), hence a denominator was unknown and a response rate was not possible to calculate. The core questions in each survey were based on the US core questions and had Likert scale responses or binary responses. Demographic details were collected from each participant, including profession, type of practice (such as general practice, urgent care) and whether the participant was working in a rural or urban setting, Rurality was self-identified by the participant and not defined in the survey system.
The degree of lockdown (termed ‘alert level’, with alert level 4 indicating the most severe lockdown), varied over the course of the study period (Fig1). The surveys were sent initially on a fortnightly basis starting shortly after New Zealand had exited from alert level 4 but, due to the elimination strategy pursued by New Zealand at that time and the reduction in COVID-19 cases, surveys were later sent at monthly or at longer intervals to avoid participant fatigue. As the survey links were disseminated through a range of mechanisms, the survey response rate is unknown. Participants accessed the participant information sheet at the start of the survey, and completion of the survey implied consent.
Five core questions were asked of participants and these included enquiring about the strain experienced by the practice, what capacity the practice had to test patients for COVID-19, the types of stressors being experienced by practices, the forms of consultations occurring (eg telehealth, face-to-face consultations) and the number of patients with respiratory illnesses or suspected COVID-19 presenting to practices. The allowed response options are described in Table 1.
The survey responses were collated by the Larry Green Center in the USA and password-protected files shared with the New Zealand team. Simple descriptive analysis of the data was carried out in Stata/IC v15.1 (StataCorp; http://www.stata.com). Two-sample, two-tailed, t-tests were calculated, comparing rural and urban means of the Likert responses and χ2 calculations for binary responses. There was some variation in the wording of the responses or the number of Likert responses for questions in some surveys. In these cases the affected questions were removed from the analysis in order to maintain comparability.
Table 1: Description of allowed responses to questions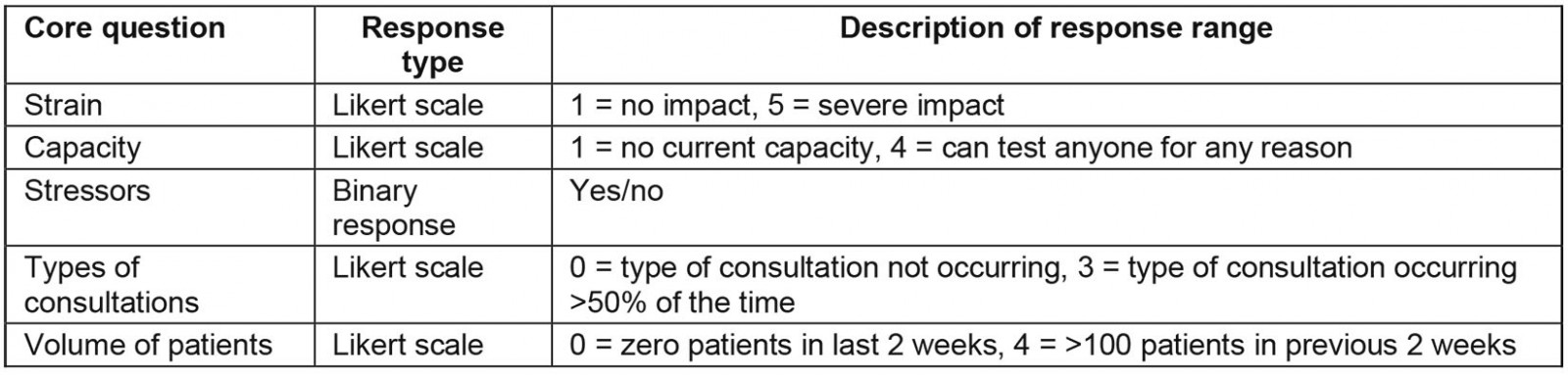
Ethics approval
Approval was granted by the University of Auckland Human Participants Ethics Committee on 11 May 2020 for 3 years (ref. 024659).
Results
The number of responses, profession of respondents, rural or urban classification of practices for each survey is shown in Table 2. The mean number of respondents per survey was 137.8, with a range of 62–231. Response numbers declined over time and time between surveys increased; eventually, surveys were stopped. Twenty-six percent (314) responses were from rural practices and 1202 responses from urban practices. The number of GPs, nurses and practice managers may not equal the total number of participants due to participants potentially coding themselves as belonging to two different professional groups (eg nurse and practice manager).
Although the majority of practices reported a moderate degree of strain throughout the survey period, there was a suggestion that rural practices reported less strain than urban practices (Fig2).
Rural practices appeared to report more flexibility in their capacity to test patients, with a consistently higher mean testing capacity across surveys (Fig3), although no statistical significant differences were noted. There was no difference between rural and urban practices with the number of symptomatic patients seen. However, rural practices appeared to refer fewer patients to testing centres and hospitals for testing and treatment (Fig4), while maintaining similar volumes of patients that they tested themselves or monitored at home.
Rural practices appeared to have fewer GPs absent from work because of illness or quarantine (Fig5). This was consistent for nurses and receptionists, with differences seen between rural and urban nurses, and rural and urban receptionists. Rural practices also experienced smaller reductions in decreases in patient volumes (Fig6), although for the latter this did not reach a level of statistical significance. No differences were seen in access to personal protective equipment nor limitations in chronic care management.
Regarding forms of telehealth consultations, rural practices reported less use of video consultations or telephone consultations and more face-to-face consultations (Table 3). There were no differences in reimbursement of telehealth consultations or use of other forms of telehealth such as portals.
Table 2: Demographic data for respondents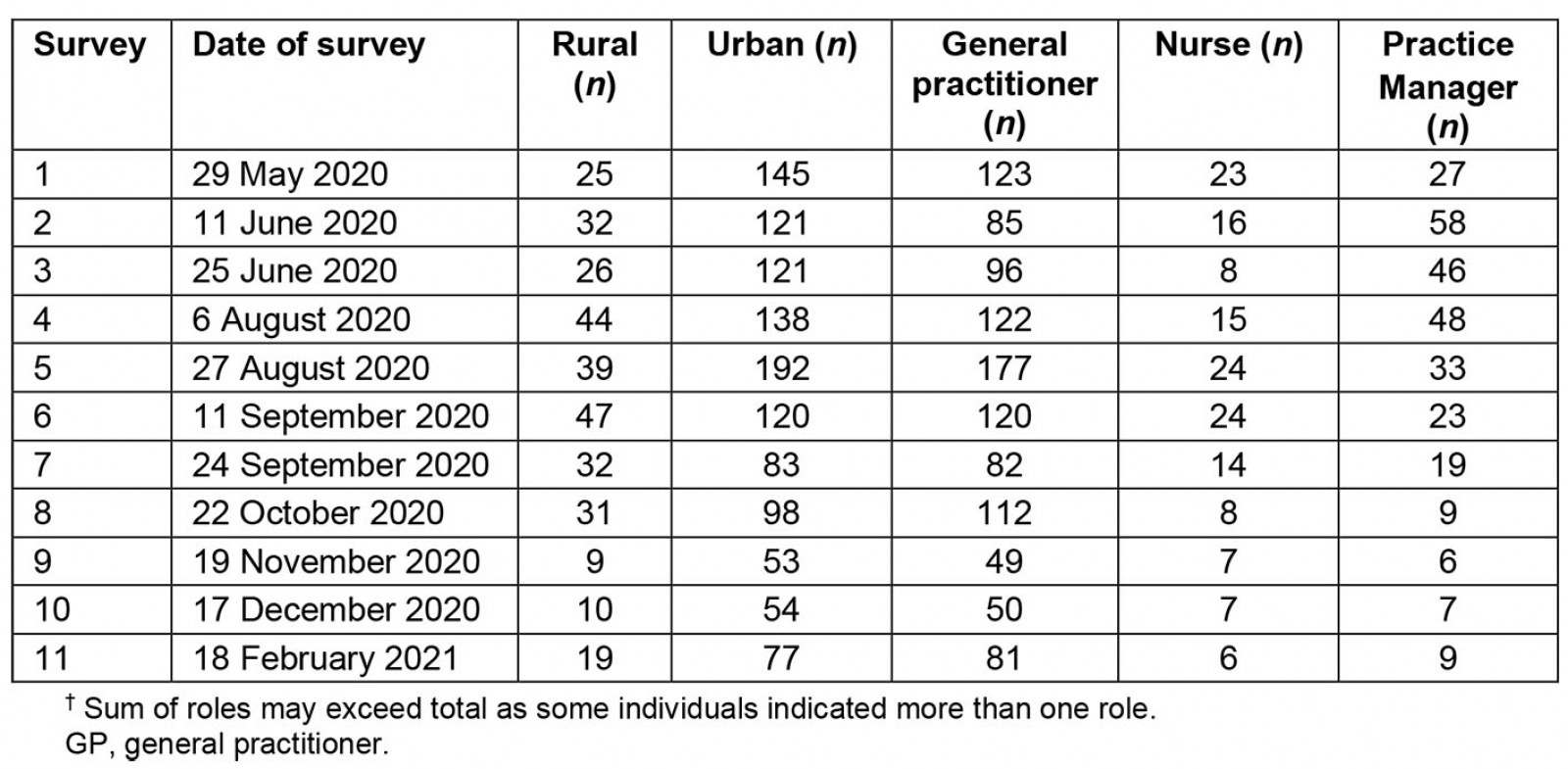
Table 3: Use of video, telephone and face-to-face consultations in New Zealand medical practice respondents, May 2020– February 2021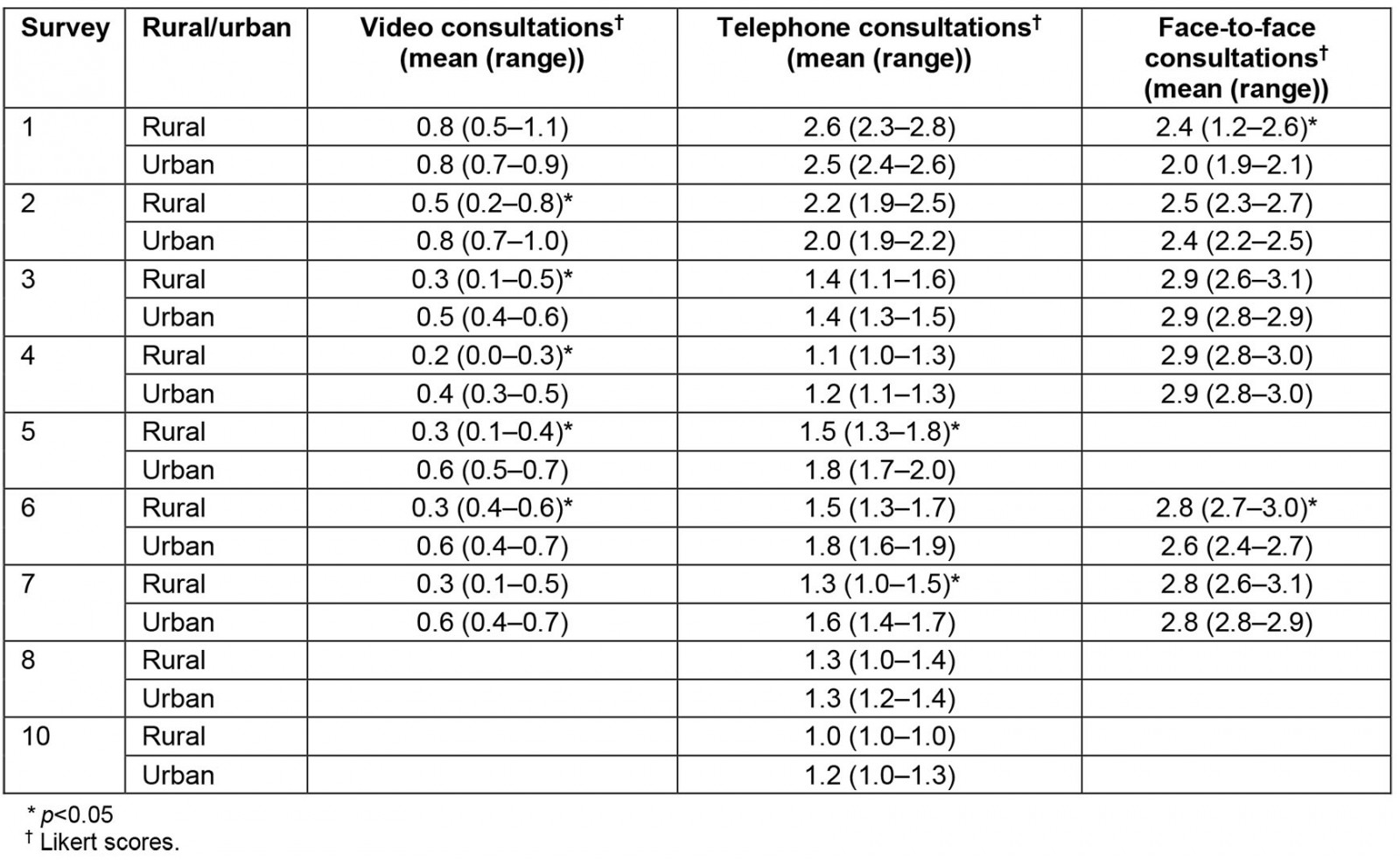
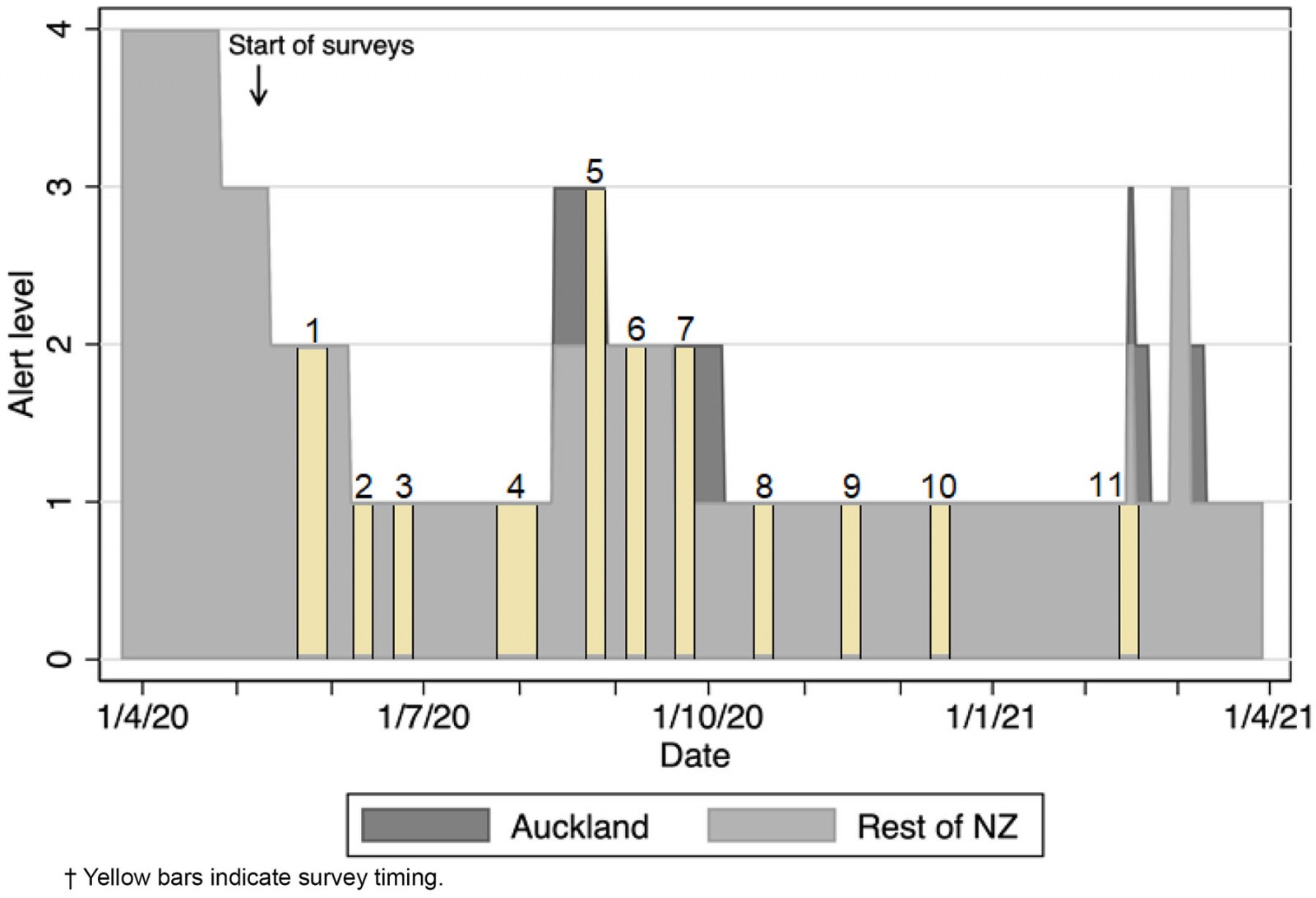 Figure 1: Alert levels for Auckland and rest of New Zealand, April 2020 – April 2021.†
Figure 1: Alert levels for Auckland and rest of New Zealand, April 2020 – April 2021.†
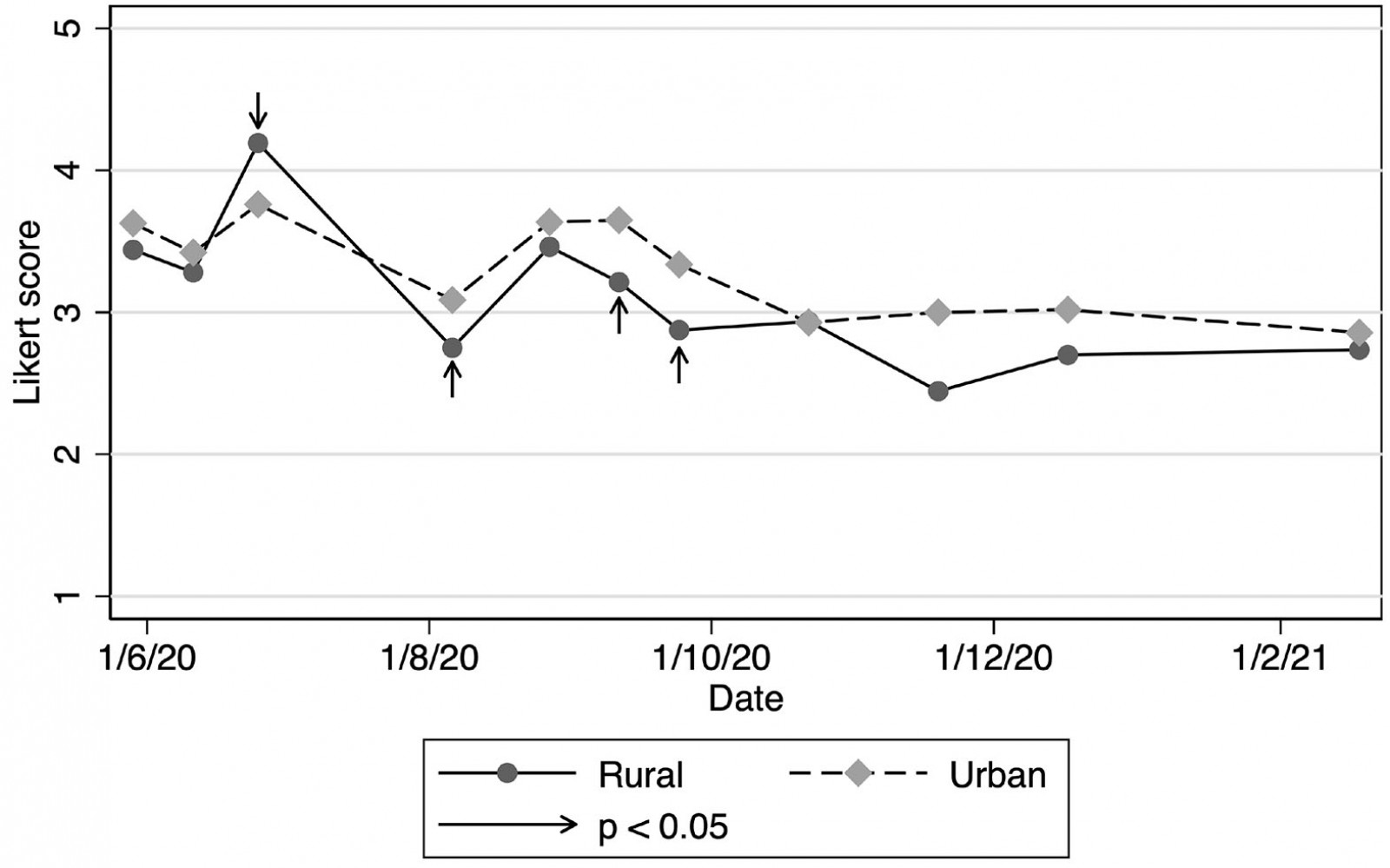 Figure 2: Strain in New Zealand medical practices (mean Likert scores), June 2020 – February 2021.
Figure 2: Strain in New Zealand medical practices (mean Likert scores), June 2020 – February 2021.
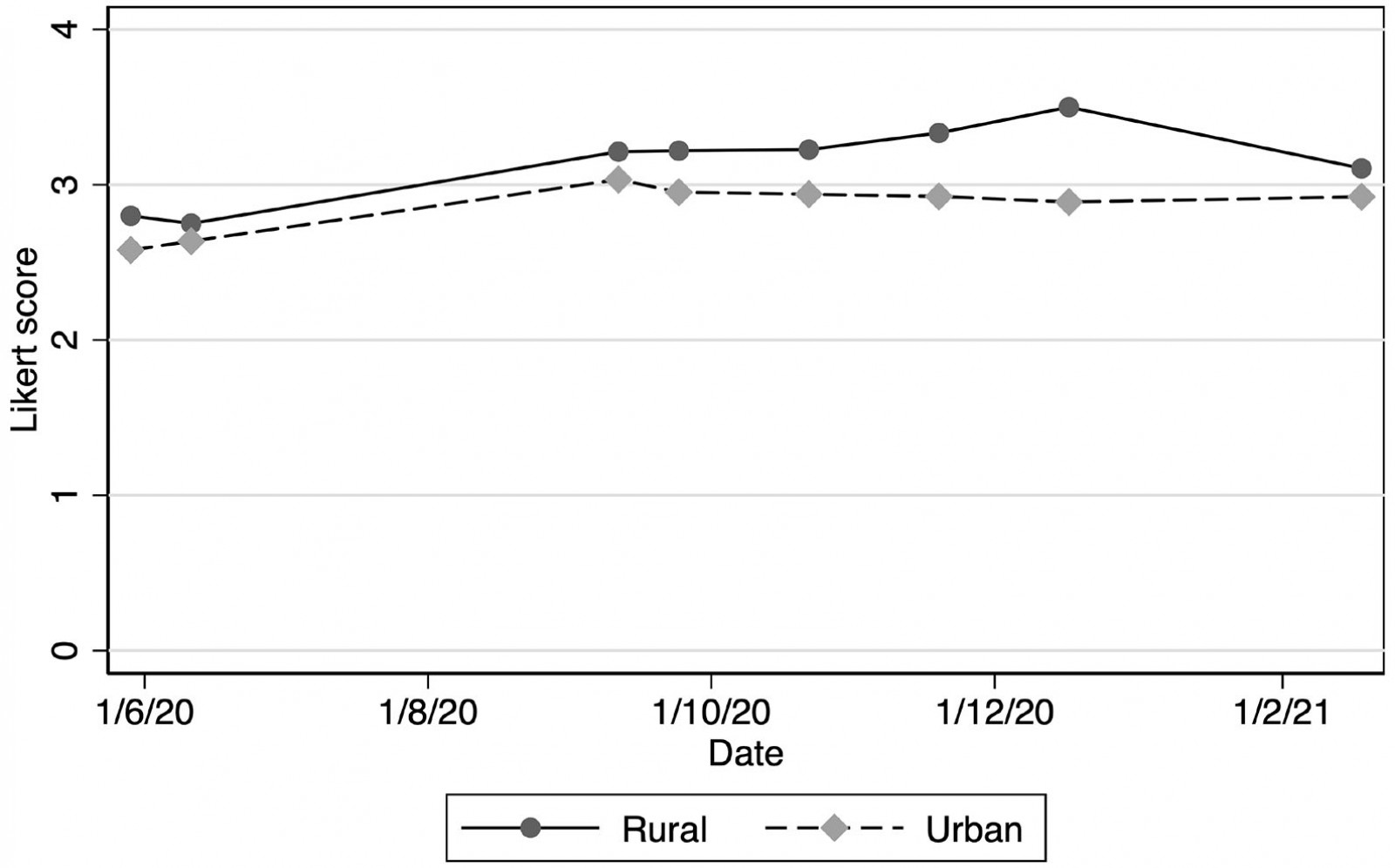 Figure 3: Capacity of New Zealand medical practices to test for COVID-19 (mean Likert scores), June 2020 – February 2021.
Figure 3: Capacity of New Zealand medical practices to test for COVID-19 (mean Likert scores), June 2020 – February 2021.
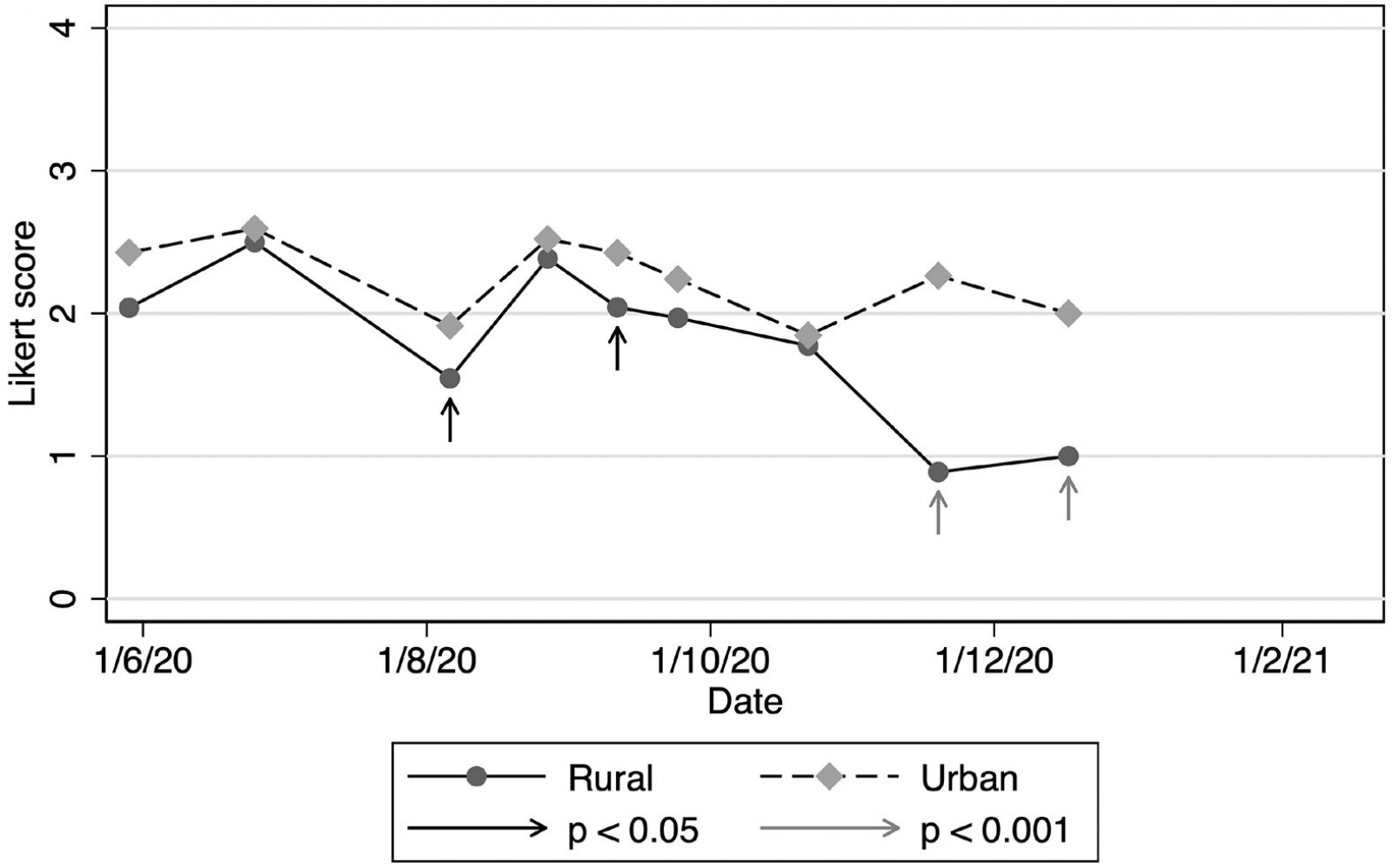 Figure 4: Patients referred for testing or treatment (mean Likert scores), New Zealand, June 2020 – February 2021.
Figure 4: Patients referred for testing or treatment (mean Likert scores), New Zealand, June 2020 – February 2021.
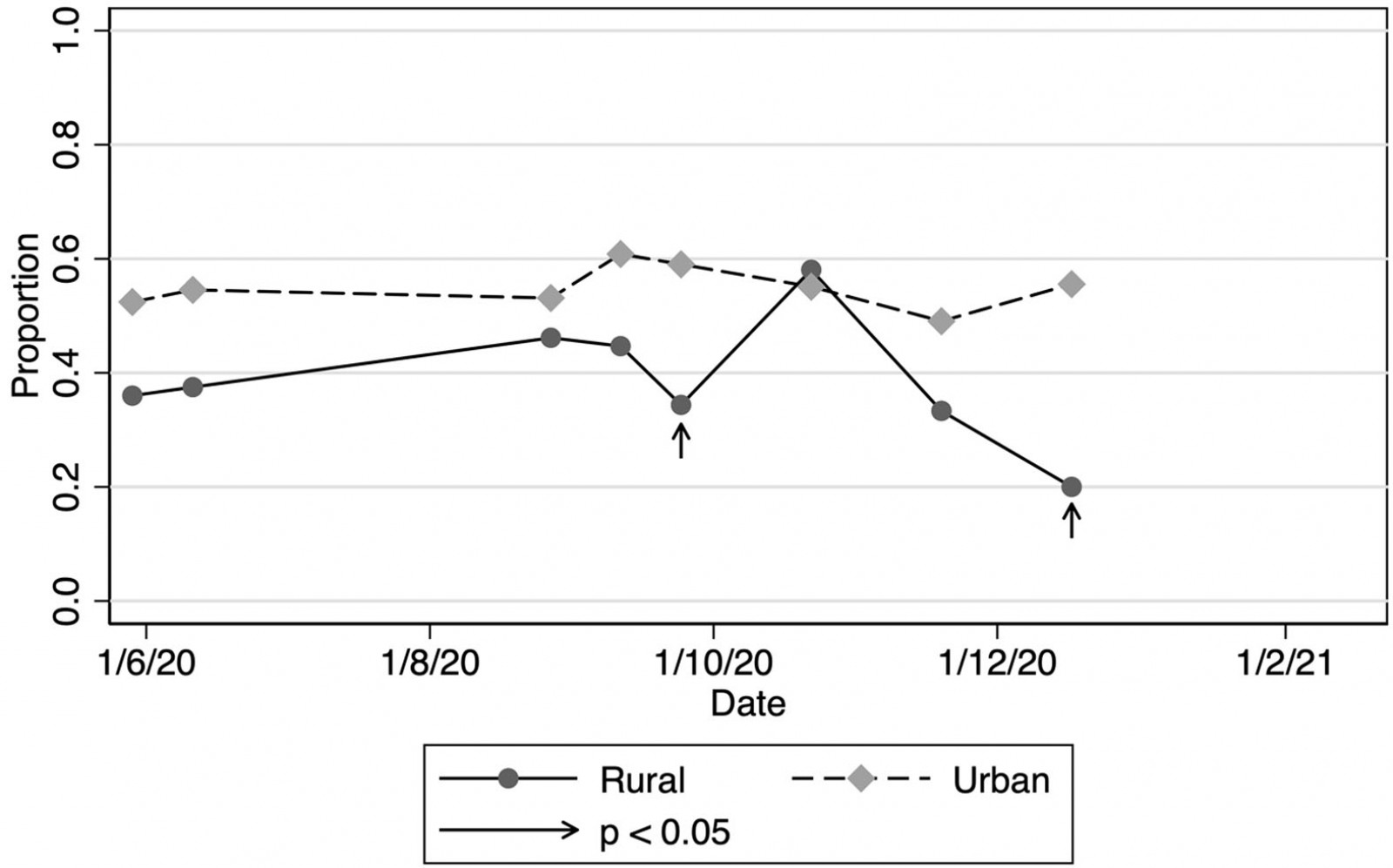 Figure 5: Practices in which general practitioners absent due to illness or quarantine, New Zealand, June 2020 – February 2021.
Figure 5: Practices in which general practitioners absent due to illness or quarantine, New Zealand, June 2020 – February 2021.
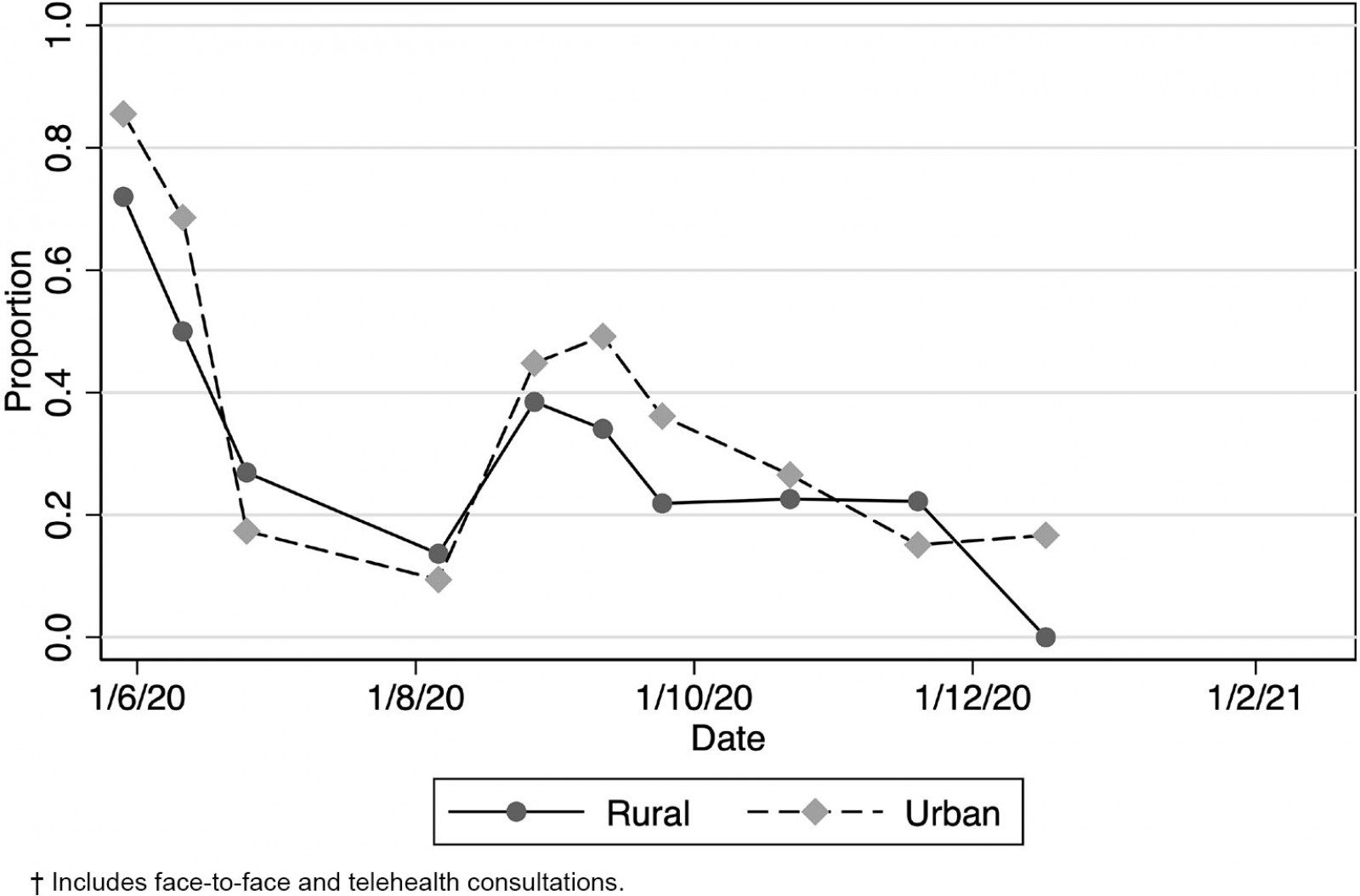 Figure 6: Practices experiencing a decrease in patient volumes, New Zealand, June 2020 – February 2021.†
Figure 6: Practices experiencing a decrease in patient volumes, New Zealand, June 2020 – February 2021.†
Discussion
The Quick-COVID surveys were designed to be pragmatic and rapid ways to inform public policy on the impact of COVID-19 on primary care. The surveys were never intended to be representative of all practices or particularly rigorous in design, due to the rapid turnover of the surveys, and caution should therefore be applied to analysis of the data. There was an initial urgency, with the need to acquire personal protective equipment, start COVID-19 testing, ‘red stream’ practices and introduce telehealth. After elimination of community spread had been achieved, practices probably had less pressing need to ensure their concerns were heard, with growing survey fatigue – hence response numbers reduced. However, the authors posit that the surveys do provide an indication of trends and general themes, and reflect underlying concerns in primary care. The most pronounced general theme apparent in the data is that rural practices had slightly different responses to the COVID-19 pandemic compared to urban practices. Some possible explanations include rural practices having less staff absent due to illness or the need to quarantine, or experiencing less financial pressures due to downturn in patient volumes and secondary loss of income from patient fees. Rural locums are hard to access and there will seldom be available colleagues to provide cover. Alternative explanations include a rural model of care that lends itself to greater coping strategies or a workforce that is self-selected to operate in an environment of constrained resources and higher acuity. This might have been reflected in the self-assessment by rural practices that they had more capacity to test patients for COVID-19 or an ability to pivot more towards utilising an acute model of care to triage and manage patients presenting with respiratory symptoms compared to urban practices.
The self-assessments of strain highlighted that rural practices generally reported lower levels of strain. Strain and burnout in general practice are complex concepts, with a multitude of causes including sociodemographic factors, workload and system-level factors. Recent New Zealand workforce surveys of GPs have demonstrated that the rural workforce is older, has more males, more international medical graduates and is more heavily reliant on short-term employees than are urban counterparts8. While anecdotal evidence might suggest that a number of these factors such as age and workforce pressures might predispose to more burnout in rural practices, this is not supported by the literature. For example, the RNZCGP workforce survey suggested that rural GPs were less likely to experience burnout compared to urban GPs8. This is a finding similar to that of a recent secondary analysis of the Commonwealth Fund survey in which rural GPs internationally were found to have lower levels of job stress. Other key factors relating to job stress in the Commonwealth Fund survey were age (GPs aged 45–54 years had lower stress levels, possibly reflecting a self-selection bias) and being female (female GPs had a lower possibility of offering same-day appointments, shorter consultations and less case management9). While there are sociodemographic differences between rural GPs and urban GPs that may account for some of the differences in stress and burnout, it is likely that rurality is an independent protective factor and that models of care influence stress levels9.
While this study was not designed to analyse the protective factors of rural general practice, the data suggest that there are differences in the model of rural general practice. The key finding was that rural general practices consistently rated themselves as having more capacity to undertake COVID-19 testing compared to urban general practice. This increased capacity existed despite both types of practices reporting similar volumes of patients presenting with respiratory symptoms and despite rural practices likely to be busier, with less decrease in patient volumes. The RNZCGP workforce survey highlighted that rural practices were less likely to not accept new patients compared to urban or semi-rural practices. This may be because many rural practices are the only health provider in a town, and so there is more of an obligation to provide services.
Another reason for the differences in capacity might be the smaller numbers of staff who had to isolate. Reasons for isolating might be the development of respiratory symptoms in staff or their families. The prevalence of COVID-19 in the primary care workforce in New Zealand was small during 2020 and would not account for any substantial differences in isolation. One possibility for the differences in staff isolating might reflect gender differences in rural and urban practices, with the burden of isolating for family reasons falling more unfairly on female GPs.
Differences in capacity might hint at different adaptive models, as referral rates for assessing respiratory patients and COVID-19 symptoms, in the surveys, were lower in rural practices. This likely reflects the distance from hospitals and District Health Board testing centres. This difference might suggest the existence of a particular rural model of healthcare delivery and that this model reduces pressure on secondary services. While there is extensive work highlighting differences in rural models of care in Australia10,11, less is known of a New Zealand model of rural general practice. Some quantitative work has shown little difference between urban and rural practices in the types of health professionals employed, the advanced procedures carried out or the nursing duties performed12. However, other work has highlighted specific characteristics that are felt to define a New Zealand rural model13. These characteristics include reduced access to medical and diagnostic services, increased clinical acumen, extended practice and strong multidisciplinary focus.
Conclusion
The Quick-COVID surveys have highlighted differences in strain experienced by rural general practice and urban general practice. Consistent with the literature, these surveys show that rural general practices appear to experience less strain. Also consistent with the literature is that rural general practice has the capacity to manage conditions in a different way to urban general practices. These differences might be accounted for by differences in personal characteristics of rural GPs or in differences in the model of rural general practice. The New Zealand rural primary care context is different to the rural context in similar health systems in other countries. Having a deeper understanding of New Zealand rural models of care is critical in developing an evidence base to support and strengthen rural general practice.
While this study does not propose to unpack differences between urban and rural practices, it does provide an important counter narrative to a deficit-based way of viewing the state of rural general practice in New Zealand. While workforce issues are a critical consideration, there are significant strengths and resilience in New Zealand rural general practice, and these strengths need to be more clearly articulated.
Acknowledgements
The project was funded through a Ministry of Business, Innovation and Enterprise grant, Grant number CIAF-1380 PROP-71234-CIAF-UOA.
References
You might also be interested in:
2015 - People living in remote communities can have best-practice diabetes care



