Introduction
Rural areas worldwide face a continued shortage of suitably trained workforce to deliver healthcare services, with inequity in the distribution of health workers between cities and rural locations presenting policymakers with an ongoing challenge1,2. Papua New Guinea (PNG) is described as a developing nation with a growing population of over seven million3. PNG is made up of 22 provinces, 89 districts and 349 local-level governments4. Urban areas in PNG are the provincial capitals and the main capital city, Port Moresby. According to the 2011 census, the rural areas of PNG are home to 87.5% of the population5. Conversely, only 12.5% of the population live in urban areas, with 4.5% of those living in Port Moresby5.
The delivery of health care in PNG is impacted by shortages of healthcare professionals, including the allied health professions, which presents as a continuous stressor on the delivery of proper healthcare services throughout the country. The allied health professions in PNG are very much in their infancy in terms of having a workforce of university-qualified practitioners. The density of dentists and allied health professionals such as pharmacists is also very low when compared to regional figures (0.049 per 1000 population)6. Anecdotally it is recognised that a similar trend and critical shortage of radiography workforce exists.
Attracting and retaining healthcare professionals, including radiographers, in rural practice is known to be problematic in PNG7,8. These issues are slowly being addressed with the recently introduced National Development Plan (2010–2030), in which the PNG Government has set goals aimed at achieving an efficient health system that can deliver a health service to the entire country at internationally acceptable standards3,9. Despite these aspirations, health workers continue to avoid rural areas, with some areas having no radiographer workforce10. Poor transport, declining healthcare infrastructure and a lack of medical imaging equipment have been reported as key barriers to rural practice6,11. Like the radiography workforce, reports on medical imaging equipment are scarce. Anecdotal reports estimate that there are one or two radiography (X-ray) and ultrasound units available in the provincial hospitals, staffed by three to four radiographers. While the rural health centres and community aid posts typically have only one assistant radiographer with a single general X-ray unit, they may not have any diagnostic imaging equipment available. A recent report on specialised diagnostic imaging equipment in the public and private health sectors by Grundy et al documented three CT scanners and three mammography units. There were no data reported on ultrasound or general X-ray equipment6.
The PNG education system enrols students of various backgrounds. Talented students complete high school and foundation training in the city to have the opportunity to attend tertiary education. However, tertiary education rates are low, with only an estimated 2% of the population enrolled in higher education5. Of these, Health Science graduates, including the Bachelor of Medical Imaging Science (BMIS) graduates, constituted 8% of the total higher education graduates for 2010–201312. The BMIS was first offered at the University of Papua New Guinea (UPNG) in 2005, with the UPNG continuing to be the only education provider in PNG offering this degree program6.
Students complete a 1-year Science Foundation Year (SFY) program, then complete another 3 years of study in general radiography and advanced medical imaging technologies. There are currently no data reporting demographics of student entry into the BMIS from the SFY, or employment thereafter. Since the inception of the BMIS program in 2005, there have been approximately 300 graduates, with an annual quota of approximately 20 students enrolled in the program. Anecdotally, current enrolments are far less than that required to adequately serve the imaging needs of both the urban and rural areas in PNG.
The small number of graduates has limited impact on increasing the radiography workforce and the provision of imaging services. Rural workforce issues are further exacerbated by graduates’ unwillingness to seek employment in rural areas, creating a geographical bias to the country’s shortage of radiation workers. The consequences of the maldistribution of a health workforce include restricted service, decreased accessibility and, as a result, poorer population health outcomes13.
Immersion of students in community-based training and rural practice has been cited in the literature as an important predictor for postgraduate rural practice10. The literature reports that community-trained healthcare graduates give greater consideration to working in rural areas than those who have not experienced similar training14-16. How these issues impact employment decisions of student radiographers in PNG remains to be explored. The dearth of literature concerning PNG and rural radiography practice warrants investigation.
The purpose of this study was to assess factors that influence PNG undergraduate radiography students’ consideration of rural practice and to document the valued opinions of the students. It is proposed that this study will provide, for the first time, valuable data for both the UPNG and PNG health policymakers and to further inform the literature on the critical shortage of radiographers in PNG.
Methods
Students enrolled in the BMIS program at the UPNG were invited to complete a survey investigating motivators for rural radiography practice. There were 57 invited participants of which 17 were second-year, 23 were third-year and 17 were fourth-year students, representing 100% of the undergraduate BMIS student cohort. The survey included questions on sociodemographic variables including gender, age, education, rural background and previous employment; and four-point Likert-type scale questions (1 being ‘strongly disagree’, 2 ‘disagree’, 3 ‘agree’ and 4 being ‘strongly agree’) exploring motivation for rural practice, opinions on the promotion of radiography through rural practice, the influence of birthplace and incentives to practice.
Combined focus-group-type interviews were completed, comprising convenience samples of six students each from the second, third and fourth years of study who were available at the time of the study. The focus groups were conducted by one of the authors (RP), who recorded and later transcribed each session verbatim. There were four questions exploring students’ opinions on factors that may inspire students to consider rural practice, exploring promotion of rural radiography through rural practice, community-based training internships, the benefits of rural practice and influence of training at the UPNG on future rural practice. Triangulation of data was enabled by the use of focus groups in addition to the survey and reduced intrinsic biases that may have arisen from using the questionnaire only10,17.
Survey data were coded based on response type and analysed using SPSS v27 (IBM Corp; http:// https://www.ibm.com/products/spss-statistics). Descriptive analysis was completed for all variables, with comparisons between groups analysed by χ2; p<0.05 was deemed statistically significant. Focus group transcripts were analysed by thematic analysis. Qualitative data were analysed collaboratively by the first and second authors because the investigator of qualitative research becomes a key instrument in data analysis10. Analysis involved the manual development and revision of codes to establish themes and subthemes of similar meaning, with checking for consistency. Relationships between key themes that emerged from the qualitative aspect of this research were identified. The key themes summarised the meaning of the data, which addressed the aim of the study10.
Ethics approval
Ethics approval was granted through the UPNG School of Medicine and Health Science Research and Ethics Committee (SMHS REC); approval number 0719.
Results
Survey results
There were 57 respondents to the survey; however, three surveys were incomplete and not included for analysis. There was no statistically significant difference in age between males and females (p=0.35).
Consistent with the distribution of the population of PNG, students from urban areas constituted only 7.5% (n=4) of respondents (Table 1). Most respondents were schooled remotely from their hometowns in the Central Province 29.6% (n=16), with the next most common places of schooling being Morobe and East New Britain provinces (both 11.1% (n=6); Table 1).
All students had completed year 12 education and two had completed postgraduate studies. Prior to the first year of undergraduate study, the majority of students had completed their education at SFY UPNG 63.0% (n=34).
All respondents agreed that the majority of their lives had not been spent in a rural area, despite them identifying as being from the rural provinces (79.6%, n=43). There was strong interest in practising radiography in a rural area, with 51.9% (n=28) strongly agreeing and 37.0% (n=20) agreeing (Table 2). The majority agreed (50.0%, n=27) and strongly agreed (40.7%, n=22) that the profession would be promoted where radiographers were seen to be working in rural settings (Table 2).
The results of the survey report show majority agreement that being born in a rural area was a potential stimulus for graduates to work rurally, with 42.6% (n=23) agreeing and 29.6% (n=16) strongly agreeing (Table 2). However, this sentiment was not the same for salaries. There were 33.4% (n=18) of respondents who did not consider an attractive salary a motivator to engage in rural practice (Table 2).
A perception of professional independence associated with working in rural areas was reported to be a motivator to engage in rural employment, with 46.3% (n=25) agreeing and 31.5% (n=17) strongly agreeing (Table 2).
Similarly, rural social life was considered a motivating factor by a small majority of respondents, with 57.4% (n=31) agreeing and 20.4% (n=11) strongly agreeing (Table 2). The better equipping of rural facilities was also reported as something that would motivate rural practice: 29.7% (n=16) agreed and 63.0% (n=34) strongly agreed (Table 2).
The majority of respondents reported that rural training opportunities would also act as a motivator for future rural practice, with 96.3% (n=52) agreeing (Table 2). Further community-based training was also viewed as a motivator, with 46.3% (n=25) who strongly agreed and 50% (n=27) who agreed (Table 2).
Across all responses, only those regarding community-based training evidenced a gender bias, with this type of training being a stronger incentive for females than for males (p=0.02). There was a statistically significant difference between students who did their SFY at the UPNG and students seeing an 'equipped rural centre' as an incentive to practice rurally (p<0.001).
Table 1: Province of origin and place of schooling of respondents (n=54)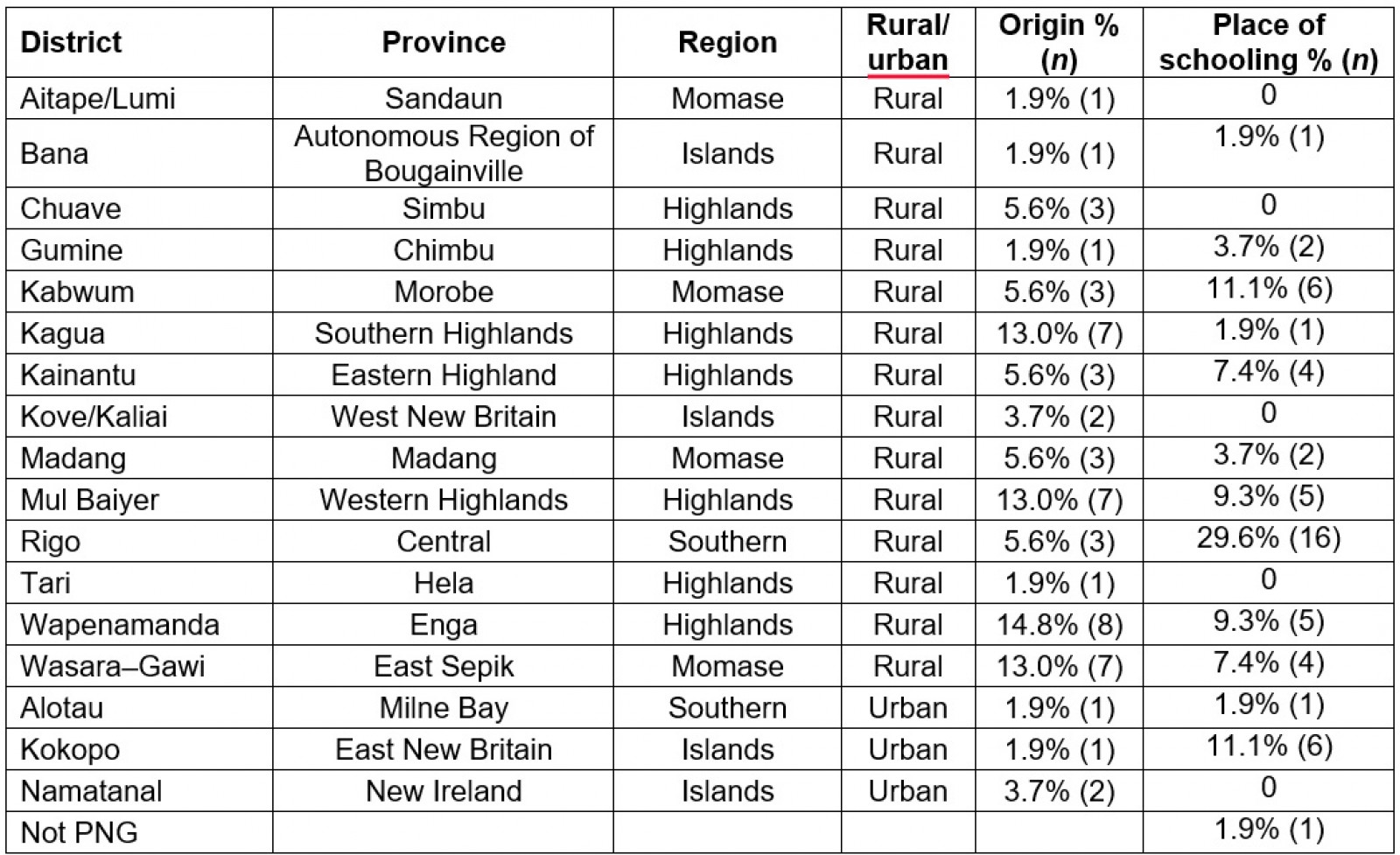
Table 2: Responses to questions relating to rural practice intent and motivation (n=54)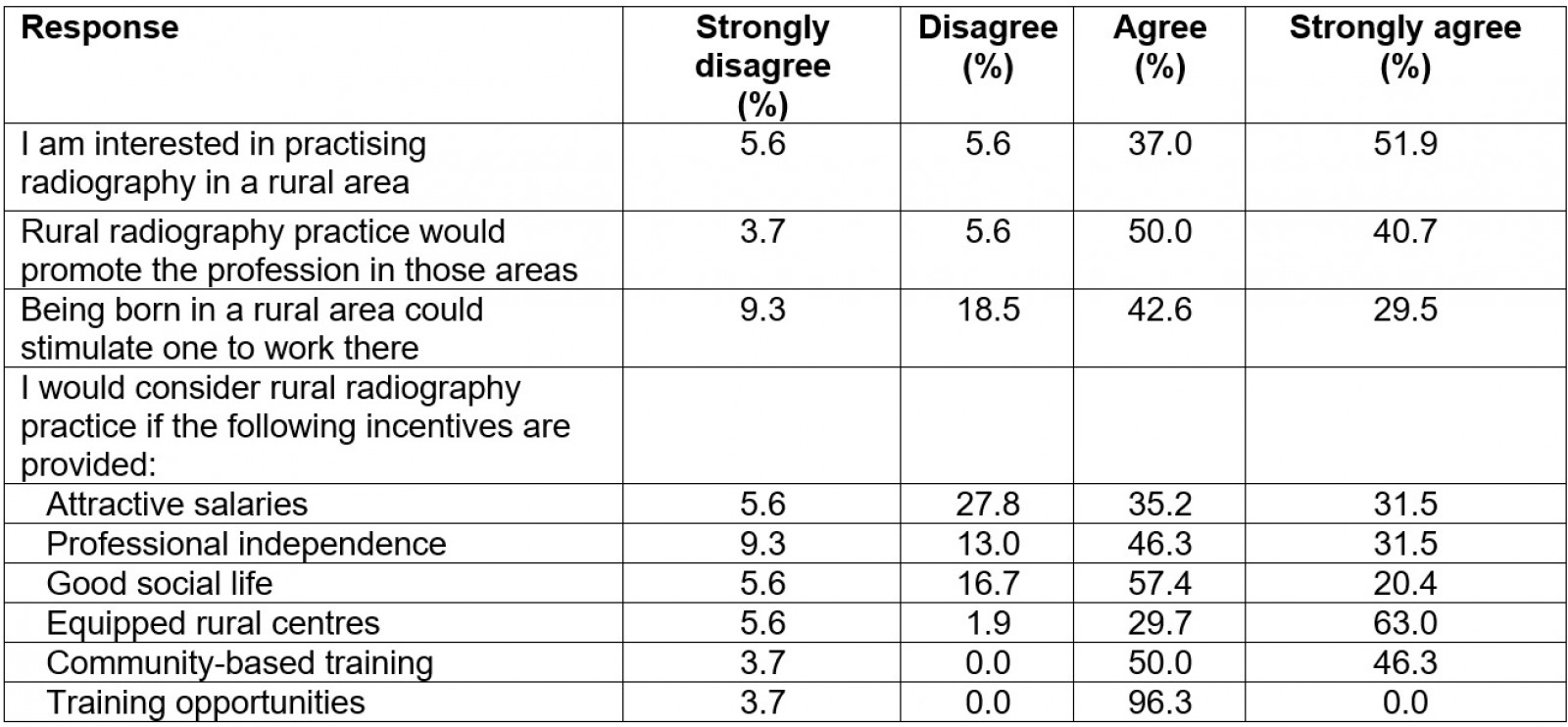
Focus group results
The focus groups raised four key themes among participants (denoted P in quoted text):
- promotion of rural radiography practice as being both the responsibility of UPNG and the individual student
… We need to have some rural placements available that students can have a feel of what rural radiography is and that is one good way of actually promoting rural radiography … (P6)
- requirement for the curriculum to align with the needs of rural practice non-digital, film/screen imaging
… what we are doing at PMGH is digital and we don't actually know or actually perform or practice conventionals [non-digital film screen imaging], how we going to process the image, especially film in the darkrooms … (P5)
… what we're learning keeps on restricting us from going back home because everyone thinks they can't really fit into the community back home because what they're learning is restricted into the city ... So yes, if we had like a training or something would definitely put us in the right position to serve our own people and would want to go back and … serve the rural communities. (P6)
- positive benefits of rural community-based training
… I think competency is one of the biggest advantage(s). You'll find that people working in rural areas are much more competent because sometimes they have to do stuff where normally they wouldn't do in urban areas … (P12)
… It helps us broaden our understanding on radiographic techniques and skills in darkroom and conventional radiography … (P17)
- impact of the lack of contemporary imaging equipment at UPNG on rural practice and several subthemes (Table 3).
Table 3: Focus group themes and subthemes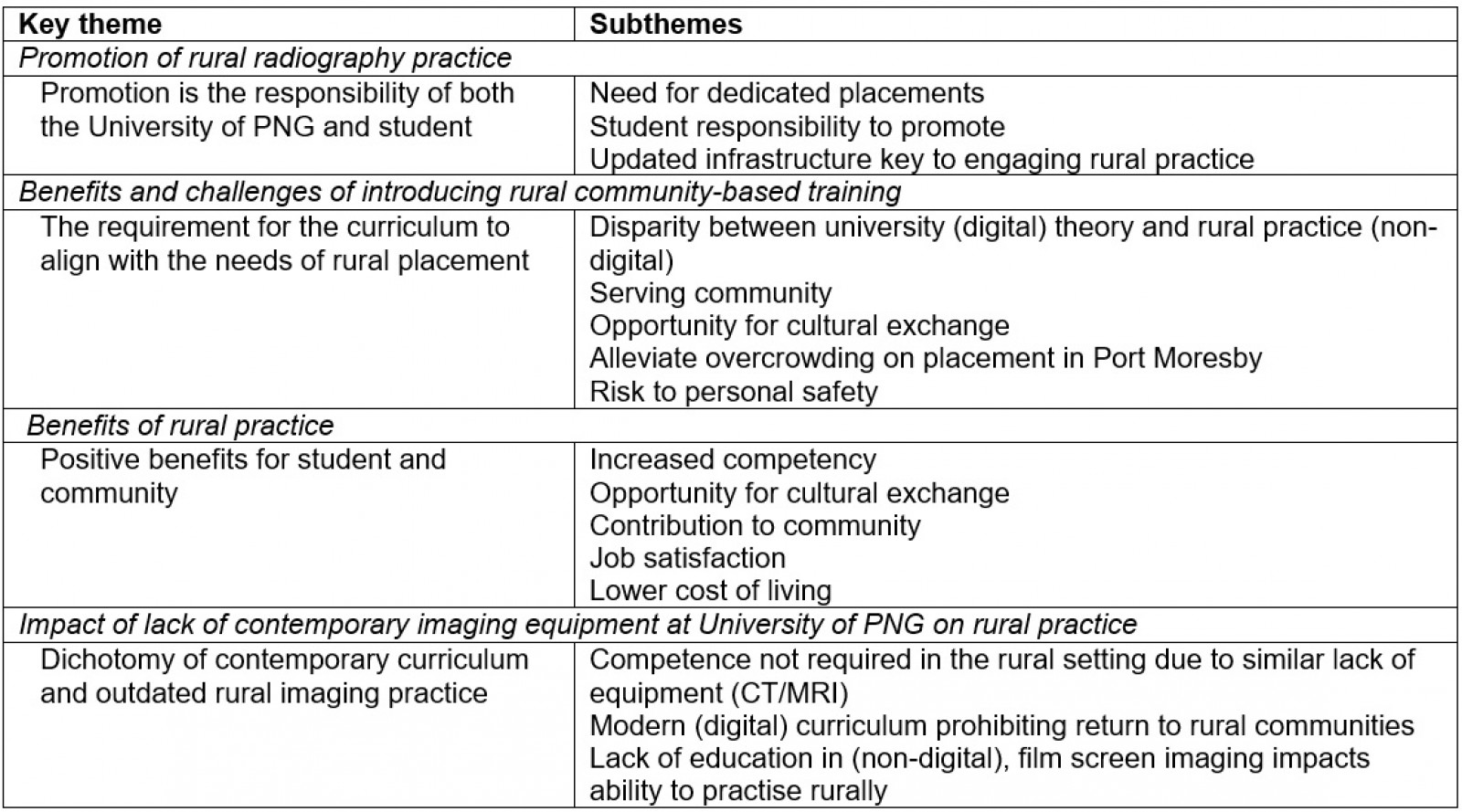
Discussion
This study explored undergraduate radiography students’ perceptions of rural practice through a survey and focus groups. Findings support a complex relationship between contemporary education, ill-equipped rural facilities, community and perceived benefits of rural practice. Students from urban areas constituted only 7.5% (n=4) of respondents (Table 1). This demographic finding is not surprising and is consistent with the distribution of the population of PNG5.
In terms of educational background, most respondents (51.8%) were schooled remotely from their hometowns in the Central Province, with the next most common places of schooling being Morobe and East New Britain Province. These findings are in contrast to a study by Tomdia et al, who reported that only 36% of the student cohort undertaking the Bachelor in Medicine Bachelor in Surgery (MBBS) program and entering from the SFY had attended primary school in village or government/mission stations11.
All students in the current study had completed year 12 prior to the first year of undergraduate study. A majority (63.0%, n=34) of students had completed UPNG SFY, 22.2% (n=12) had completed Pacific Adventist University (PAU) SFY, and 11.1% (n=6) had completed UPNG Open College (Table 1). These findings are consistent with a similar study at the SMHS reporting a majority (61%) cohort of students who completed the 4-year MBBS program had gained direct entry from UPNG SFY, more than half (53%) completed PAU SFY, and 41% completed UPNG Open College11. Although a majority of the students complete the UPNG SFY program before entry into the SMHS’s BMIS and MBBS programs, the difference in findings between both studies could be attributed to the 3-year and 4-year completion rates between students of both programs respectively, entering by different routes – which the current study did not investigate.
The majority of respondents 79.6% (n=43) in the current study agreed that the majority of their lives had not been spent in a rural area despite identifying as being from rural provinces (20.4%, n=11). It was also noted that there was verbal disagreement among respondents during the focus groups concerning the definition of a rural community. Individual respondents’ understanding and perceptions of what constitutes a rural community, and being schooled in other provinces and cultural norms have been put forward as rationales for the issue.
In the current study, there was interest (88.9%, n=48) in practising radiography in a rural area, and the majority (90.7%, n=49) agreed that the profession would be promoted where radiographers were seen to be working in rural settings. These findings are expected as the majority (53.8%, n=29) of the respondents in this study had rural backgrounds. These findings also support other studies across countries including Australia, the US and Canada13,15,16,18 that have identified that an individual’s rural background influences a health worker’s intent to work in rural communities. Other reports note that the formative years of some rural healthcare workers were not spent in rural areas, emphasising the importance of encouraging those from both urban and rural backgrounds into rural practice10,19.
Postgraduate rural practice has been reported as being strongly influenced by being from a rural location16,20,21. The results of the survey similarly report that being born in a rural area was agreed by the majority (72.2%, n=39) to be a potential stimulus for graduates to work rurally; however, this sentiment was not the same for salaries. There were 33.4% (n=18) of respondents who did not consider an attractive salary a motivator to engage in rural practice. To encourage rural practice, countries worldwide have implemented initiatives to specifically mitigate the low wages inherent in public sector employment10. In PNG, initiatives include the Domestic Market Allowance, intended to offset public service salaries, which are considerably lower than those of the domestic labour market10. These findings suggest that worker satisfaction to practise in rural areas could be linked to secondary factors such as safe working and living conditions, and supervisory and community support22.
In the current study there was a perception that working in rural areas afforded professional independence as well as offering a different social life. Respondents also indicated that better equipping of rural facilities would act as a motivator for future rural practice. These factors, while external to the undergraduate program, were similar in importance to respondents seeking rural training opportunities and community-based training embedded in the BMIS to enable exploration of rural radiography practice. Immersion of students in community-based training and rural practice has been cited in the literature as an important predictor for postgraduate rural practice10. Across all responses in the current study, only those regarding community-based training evidenced a gender bias, with this type of training being a stronger incentive for females than for males (p=0.02). There was no explanation for this finding. The above findings concur with a similar study in Uganda, which reported that rural training opportunities and social amenities such as recreation facilities and entertainment would motivate radiographers to engage in rural practice10. Both PNG and Uganda are developing countries with limited resources, and great challenges exist for policymakers in both countries to capitalise on these motivators.
There were statistically significant differences between students who did their SFY at the UPNG and seeing an ‘equipped rural centre’ as an incentive to practise rurally (p<0.001). This response may reflect the lack of medical imaging equipment for training students in the BMIS program. It should be noted that the BMIS program is supported by a single medical imaging laboratory at the SMHS, with limited teaching resources and no radiography equipment for hands-on training of students prior to entering the clinical environment.
Promotion of rural radiography practice
The promotion of rural radiography practice was seen to be a responsibility of the UPNG in offering placements during the undergraduate year. This response reflects the lack of placements for BMIS students to practise rurally as commented by a student in the present study (P6):
… We need to have some rural placements available that students can have a feel of what rural radiography is and that is one good way of actually promoting rural radiography …
The impact of dedicated clinical placement on a student’s intention to engage in future rural practice has been identified as significant in other countries23. This influence has also been demonstrated to have both short- and long-term impacts in other allied health professions and medicine23. Similar to student (P6), there was a general need noted for the individual student to reach out to the community to explain the profession and the technology to the population:
… [an] individual like myself, I’m a leader to my own community … in this way you could influence our own young people too. And also our own family members or community members … (P16)
Provision of equipment and supporting infrastructure such as power was strongly noted as needed to promote rural radiography practice, as commented by another student:
One of the ways to improve rural radiography would be to install basic x-ray machines. I grew up in rural area, so I know that much of the rural hospitals, they lack basic x-ray machines ... So that could be one way to promote it [the profession]. (P12)
Introduction of rural community-based training
Motivation to work rurally was tempered by feelings of lack of theoretical education in non-digital film screen radiography; however, the desire for rural employment was high (88.9%, n=48). The current focus at the UPNG and placement sites on digital imaging was seen as a limitation to working or training rurally. Similar comments were echoed by some students on the need for introducing rural community-based training to overcome this bias.
An internship was viewed to be a positive opportunity to build competency in non-digital, film screen or conventional (as opposed to digital) radiography to enable rural placement, build on knowledge and help communities. These results suggest that rural community-based training including a curriculum in non-digital, film screen radiography could influence student radiographers to practise in rural areas. A rural placement was also seen as a way to showcase the different cultures of PNG and the rural environment, as echoed by one student:
… Some of us we come from the rural [communities] to university and we know the situation out there but others who are in the cities they don’t really know that. So in promoting rural radiography we should send students out there … (P7)
In contrast to this response, another student noted an associated personal risk, despite being supportive of a rural placement:
I think there’s a very big gap out there, there’s nobody working out there because they fear tribal fights and they want to be here in the city … When it comes to residency, the idea of keeping us all here [at the urban hospital], I don’t think it’s good … there are too many of us crowding here … It’s about time now we do our residency in rural places. (P2)
Indeed, there is a known high level of violent crime in PNG, including tribal disputes, with gender-based violence (including sorcery-related violence) prevalent24. A recent parliamentary committee inquiry into gender-based violence in PNG reported 70 recommendations to the PNG Government for action to improve this problem25.
These responses suggest that a collaborative effort between all stakeholders, including UPNG and the PNG National Department of Health, to address the gap in offering placements for students to practise rurally may serve to motivate student radiographers to practise in rural areas post-graduation6. Elsewhere, rural placement has been evidenced to promote future rural practice, with positive placement experiences being shown to directly impact intent to practise rurally18,26. Rural placements associated with transformative personal and professional growth are important rural workforce strategies26. In line with the PNG Government’s National Health Plan 2011–2020 policy that outlines the ‘back-to-basics’ approach with the goal of ‘Strengthened primary health care for all and improved service delivery for the rural majority and urban disadvantaged’6 (p. 156), training interventions such as for a rural radiography training program is an urgent need6. Although such a program could address the chronic shortage of rural radiography workforce, the limited resources available in PNG may not be able to sustain a rural placement that translates to graduate rural employment.
Benefits of rural practice
Many positive benefits were foreseen from practising in a rural setting. Most of the students noted that increased competency from having to use conventional non-digital film/screen image acquisition technology, including manual exposures and expanding professional practice, was a key benefit:
… we would gain experience in knowing how to be able to use those conventionals [non-digital film/screen acquisition] and because it wouldn’t be everything readily available like in the city, it would make us be innovative … be more careful with the exposures and everything … it would make you more competent to a DR [digital] user in the city. (P3)
The responses align with a recent medium-term evaluation of the PNG National Health Plan and significant equipment upgrades across the country, with 70% of hospital equipment (such as X-ray machines) being updated (digitised) or replaced6. This evaluation further confirmed that equipment upgrades have primarily occurred at provincial hospitals. However, this evaluation does not include data on rural health centres and community aid posts that continue to miss out on critical life-saving imaging equipment, or the shortage of radiography workforce. One of the solutions to sustain the rural radiography workforce in line with the 2010–2030 development plan is to implement a rural radiography training program as soon as possible. This solution could be achieved through developing curriculum for a certificate in rural radiography in collaboration with relevant stakeholders, including the UPNG Open College, to coordinate a distance and flexible learning program, and by seeking approval from the National Department of Health and the provincial health authorities to secure funding and budget support.
It is estimated that there are more than 1000 different cultural groups, and 800 spoken languages are known in PNG11. Hence the students saw engaging in rural practice as an opportunity to exchange culture:
… PNG is so diverse, we’re made up of diverse cultures so working in rural … one of the benefits, you’ll learn different cultures of different provinces. (P7)
Some students viewed that being able to experience rural life and positively contributing to the rural community both through imaging and engaging the community was a positive benefit of rural practice:
… The greatest benefit you could get is to actually help people out there. Like we don’t get to do that a lot here … so like when you go out there like you can see it yourself that you’re making that difference in people’s lives. (P10)
There was also a view that rural practice would benefit job satisfaction, as described by some students:
… the satisfaction that you’ve provided the services for those people who couldn’t afford to come to the urban area for taking radiographic examination. (P13)
… personally for me is the satisfaction that I have given something back to my own people in my country … (P17)
Other students viewed that the positive benefits of rural practice aligned with a cheaper cost of living:
… I think you would save a lot if you work in the rural areas … rural people highly regard health workers … people will provide food and that’s one of the biggest advantage of working in rural areas. (P12)
The generosity of rural communities in providing free produce to respected healthcare workers has been previously reported and was seen as important support for the healthcare workers and an influence to practise rurally27. The average salary for a radiographer in PNG is reported to be 6970 kina per month28. With the reported household net income required for adequate rural living reported as PGK 159329, the average wage for a radiographer combined with potential for free food supports cheaper living costs for rural radiographers. People who are already based in rural areas, such as assistant radiographers who are trained on the job, could benefit from a rural radiographer program. There is a need to invest in education through the UPNG Open College and at service level through the provincial health authorities. Distance learning with these authorities is the most practical approach to implementing a rural radiographer training program if change is to occur.
Impact of lack of imaging equipment
A lack of imaging equipment at the UPNG, including MRI, CT and ultrasound, is known to impact the learning experience of the BMIS students. Most students, however, did not feel that the limited access to advanced imaging technology influenced their consideration of a rural experience:
… truth is we know that in rural setting there is no advanced imaging. So lack of advanced imaging for me it will not restrict me in any way I know. (P6)
These responses confirm the evidence that the technology is simply not available rurally, as reported by the WHO4. However, others felt it impacted their professional confidence:
I think the fact that there is an obvious lack of these equipment, undeniably it gives us a sense of fear as students … So I’m thinking if I go to a rural setting, am I ready to carry out the exams under non-supervision … so personally I think if I want to graduate I wouldn’t straight away go to a rural setting. Maybe get experience for a while and then I’ll go there. (P3)
… only knowing in one particular area [digital image acquisition] … it’s an incomplete MIT [qualified radiographer]. (P16)
The difference in technology between rural and urban facilities and the BMIS focus on digital technology has inadvertently created a situation whereby students are essentially ill-equipped to service the very communities they wish to serve. Until the technological lag is fully addressed, the desire to provide contemporary medical imaging education needs to be tempered by the actual needs of the nation. It may well be that by addressing this key issue graduates may feel more comfortable seeking employment in rural communities.
Conclusion
PNG is a developing nation with an inherent lack of health infrastructure and limited resources. A willingness of students to engage in rural practice was tempered by an underlying feeling of ill-preparedness due to the dichotomy of the rural and urban imaging landscapes concerning image acquisition (non-digital versus digital). Undergraduate training on digital equipment does not fully equip graduates for working with non-digital film screen imaging in the rural setting. Conversely, having advanced imaging modality competency such as MRI or CT is of limited value to rural practice and the vast majority of the PNG population if there is no such equipment available in rural communities.
The BMIS students in the present study were given the opportunity to critically discuss their perceptions on the promotion of rural radiography practice. From the focus group discussions, students supported the concept of introducing rural community-based training. It was interesting to note that, while being challenged by the impact of the lack of imaging equipment in rural facilities, most students appreciated the benefits of practising in rural areas.
Being from a rural location and experiencing a rural placement, including experiencing new cultures and a desire to give back and support rural communities, were evidenced as strong drivers for both student placement and graduate rural practice. Moving forward, a balance is needed between all factors to support and encourage graduates to move from urban facilities and seek careers in rural practice. A more detailed study of the medical radiation science professionals of PNG, including longitudinal studies of those practising rurally, is needed to validate this study.