Introduction
China has the heaviest burden of stroke in the world, and this burden has increased in the past 30 years. In 2013, a nationwide representative survey of stroke was conducted across 155 urban and rural centers in 31 provinces of China1. Age-standardized prevalence, morbidity and mortality of stroke were 1114.8/100 000, 246.8/100 000 and 114.8/100 000, respectively. Among all stroke patients, the prevalence and incidence of ischemic stroke were 69.6% and 77.8%, respectively1. The burden of stroke in rural areas is worse than that in urban areas. This is related to not only unhealthy diet and lifestyle habits in rural areas, but also rather poorer medical conditions compared to urban areas1.
The treatment of ischemic stroke is particularly time-sensitive. The key means of improving the prognosis of ischemic stroke is through IV thrombolysis and mechanical thrombectomy within the effective treatment time window2. These two approaches were considered as the definite treatment throughout this research. Whether the patient of acute ischemic stroke could access these two therapies effectively depended directly on the time from symptom onset to arrival at the qualified stroke center.
Rural doctors of China are relatively unskilled in terms of stroke management3. Also, regional hospitals lack necessary imaging equipment such as CT and the essential treatments available at primary hospitals3. This is further complicated by long-distance transfer to the only stroke center for regional areas. It is therefore very difficult for ischemic stroke patients living in rural areas to get definitive treatment within the therapeutic time window, unlike other more developed countries around the world3. This situation is even worse in remote island areas. Isolated by sea, and with lack of air transport and other efficient rescue transportation, patients in these regions have even more difficulty accessing timely and effective treatment. With a view to probing this issue, a careful investigation was retrospectively conducted on the management of ischemic stroke patients living in the area of remote islands in China.
This study is one of the very few studies that retrospectively address the issue of ischemic stroke management in a small archipelago in China4-10. The authors believe it is the first investigation concerning the delay of the definite treatment for ischemic stroke focused on the often-neglected population living in remote outer Chinese islands.
Methods
Geography and access to definitive treatment
The main island (MI, 502 km2) of Zhoushan City is the fourth largest Chinese island, located in the north-eastern offshore area of Zhejiang Province (29º 50′N, 122º 25′E). Zhoushan is an archipelago comprising 1390 islands, with 103 inhabited islands. Putuo District, in the eastern part, has the biggest permanent resident population, with 382 902 people according to the China’s 7th National Census in 2020. Compared to the census in 2010, the proportion of the population aged more than 60 years increased by 9.79%, and the proportion of the population aged more than 65 years increased by 6.56%. The administrative region of Putuo District includes the eastern part of Zhoushan Island (MI region) and 455 outer islands (OIs, Fig1). Putuo District has only one primary stroke center: at the Putuo Hospital of Zhejiang Province, operating under Sir Run Run Shaw Hospital Zhejiang University School of Medicine. It is in the eastern area of MI, a 15-minute drive from the passenger boat terminal. Since 1 December 2020, this center has been accredited as a treatment center for comprehensive diagnosis and definitive treatment of ischemic stroke including IV thrombolysis and mechanical thrombectomy2. The other OIs have only primary medical centers, unable to offer definitive treatment of ischemic stroke due to a lack of CT or MRI scanners and thrombolytic agents. More than 99% of MI residents have social insurance, covering 50–70% of the cost of peri-admission medical care and examinations.
Of the 455 OIs, there are 32 inhabited islands, with a total population of about 110 000. Sail durations from the six larger inhabited islands to MI are 45–20 minutes and operated through scheduled passenger boats only during the day. The other 26 inhabited OIs do not have direct scheduled boats to the MI. If required, emergency patients can be transferred from OIs to Putuo Hospital by a dedicated emergency ship, operated by a local government service since 2017. This option is expensive; a cheaper option for emergency patients is to pay for a private boat. For both options, urgent transportation requires prior medical arrangements for continuous medical care in the presence of a medical practitioner and a registered nurse. Conversely, patients living on MI can usually be urgently transported by car or ambulance to the Putuo stroke center.
All patients in the present study had been transferred to the emergency department, treated and hospitalized at the Putuo Hospital. Although the Putuo Hospital is in the center of Putuo District, several patients were transferred upon request to other central hospitals, despite these being further away. This study, therefore, was unable to gather all cases of ischemic stroke, but what was sampled constitutes the vast majority of ischemic stroke cases in Putuo District during the study period.
All patients with ischemic stroke who attended the Putuo stroke center through the emergency department from 1 January to 31 December 2021 were considered as part of the study population. To identify OI residence of patients, addresses at time of symptom onset were confirmed by telephone based on the contact information; those immigrating to MI were reallocated so that they were part of the MI group.
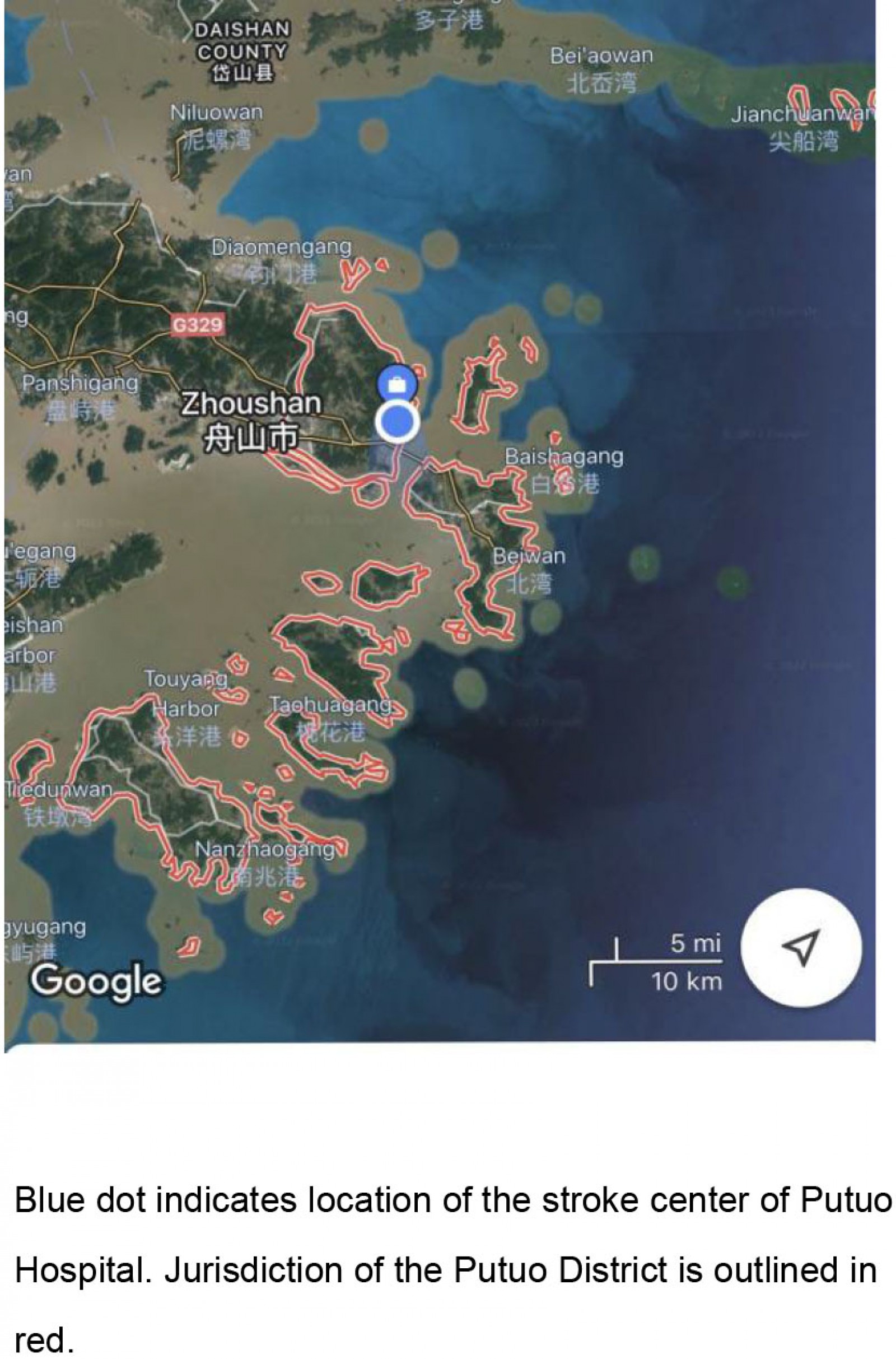 Figure 1: Putuo District, Zhoushan City, Zhejiang Province, China.
Figure 1: Putuo District, Zhoushan City, Zhejiang Province, China.
Screening
Through the inpatient and emergency medical records of the stroke center of Putuo Hospital, the medical records of patients (risk factors, symptoms and signs, National Institutes of Health Stroke Scale (NIHSS), brain CT and MRI, definitive treatment methods (IV thrombolysis and mechanical thrombectomy), total inpatient cost, prognosis) were reviewed and collected. Inclusion criteria were:
- the ischemic stroke must have been the first-ever for that patient and occurred during the time of the investigation (1 January 2021 – 31 December 2021)
- the patient must have been living in Putuo District at that time
- the ischemic stroke must have been diagnosed within 28 days after the beginning of the stroke, and verified. Diagnosis of stroke must have been made by the clinician attending to the individual case, based on clinical criteria and neuroimaging.
Exclusion criteria were as follows:
- Patients relapsed.
- Patients developed acute ischemic stroke after hospitalization due to any other illnesses.
All available data, documents and the diagnosis of stroke were reviewed by two neurologists from the Putuo Hospital stroke center.
Diagnostic criteria
According to the WHO standard, stroke is defined as ‘the rapid development of clinical symptoms of focal (or holistic) dysfunction of brain function, lasting more than 24 hours or leading to death'11. There should be no obvious causes except for vascular sources, i.e. head imaging in the first week of stroke onset should exclude of neurological abnormalities caused by trauma, metabolic disorders, tumors or central nervous system infections.
Presence of pre-stroke risk factors was established on the basis of the following criteria:
- hypertension, defined as a medical history of hypertension or use of antihypertensive medication
- diabetes mellitus, defined as a medical history of diabetes mellitus or use of antidiabetic medication
- atrial fibrillation, defined as a medical history of atrial fibrillation
- coronary artery disease, defined as a medical history of coronary artery disease
- arteriosclerosis, defined as a medical history of arteriosclerosis or confirmed by arterial imaging during hospitalization
- valvular heart disease, defined as a medical history of valvular heart disease or confirmed by valve imaging during hospitalization
- hyperlipemia, defined as a medical history of hyperlipemia or confirmed by lipid screening during hospitalization.
Statistics
SPSS v20.0 (IBM; http://www.spss.com) was utilized for analysis of the data. A two-sided value of p<0.05 was taken as the significant difference. All data other than categorical and ordinal variables were tested for normal distribution. If qualifying as a normal distribution, the data were tested using a t-test. If not, the Mann–Whitney U-test was used, including categorical and ordinal variables. When analyzing pre-stroke factors and definitive treatment, χ2 was used.
Ethics approval
This study was conducted between 1 January and 31 December 2021, following approval by the Ethical Committee of SRRSH Hospital, Zhejiang University School of Medicine, Hangzhou, China. Informed consent was not required as this was a retrospective study according to the exemption of informed consent approved by the ethical committee.
Results
A total of 340 cases were retrieved across the study duration. Of these, 326 fulfilled the inclusion criteria (Table 1). All data other than categorical and ordinal variables were not normally distributed (see Supplementary table 1). Of those selected, 178 males (59.3%) and 122 females (40.7%) lived on MI, with a total mean age and standard deviation (SD) of 70.3±13.2 years (range: 28–93 years). The remaining 15 males (57.7%) and 11 females (42.3%) resided on OIs, with a total mean age±SD of 76.6±12.2 years (range: 39–90 years). Among the population selected, no significant difference in gender and age were noted between the two regions. The most prevalent risk factors in ischemic stroke cases were hypertension (72.1%), arteriosclerosis (68.1%), atrial fibrillation (31.6%) and diabetes mellitus (28.5%) (Table 2). The least prevalent risk factors were hyperlipemia (1.2%), valvular heart disease (4.0%) and coronary artery disease (13.8%). The prevalence of arteriosclerosis was significantly higher among the MI group than in the OI group, but the prevalence of hyperlipemia was significantly greater in the OI group (although this might be inaccurate because of the paucity of the samples). However, there was no significant difference in the prevalences of hypertension, atrial fibrillation, diabetes mellitus, valvular heart disease and coronary artery disease between the two regions. All the results of risk factors were roughly consistent with those of previous studies1,4. This study did not include and analyze the risk factors of smoking and alcohol intake. Being a retrospective study, some bias might be present regarding the smoking and alcohol intake history. These data were obtained via the medical records, without objective evidence.
In relation to peri-admission management, only the time lag from onset of the stroke to arrival at the emergency department of Putuo Hospital was found to be significantly different between the two regions (MI group: mean time and SD of 14.7±25.5 hours; OI group: 41.7±44.4 hours; p<0.001) (Table 3). Patients living on OIs had significant delays in reaching the stroke center of the Putuo Hospital as compared to those on MI. Because of the significant postponement, the rate of ischemic stroke patients of the OI group receiving definitive treatment was significantly lower than in the MI group. The odds ratio for IV thrombolysis was 0.131 (OI group to MI group, range: 0.017–0.987, p=0.021). By comparison, the OR of definitive treatment including IV thrombolysis and mechanical thrombectomy is 0.122 (OI group to MI group, range: 0.016–0.917, p=0.016) (Table 4). NIHSS at discharge and inpatient expense showed significant difference. Parameters of NIHSS at admission, alteration of NIHSS, duration of inpatient stay and prognosis showed no significant differences (Table 3).
Table 1: Gender and age profile for main island and outer islet residents admitted to Putuo Hospital with ischemic stroke, 1 January – 31 December 2021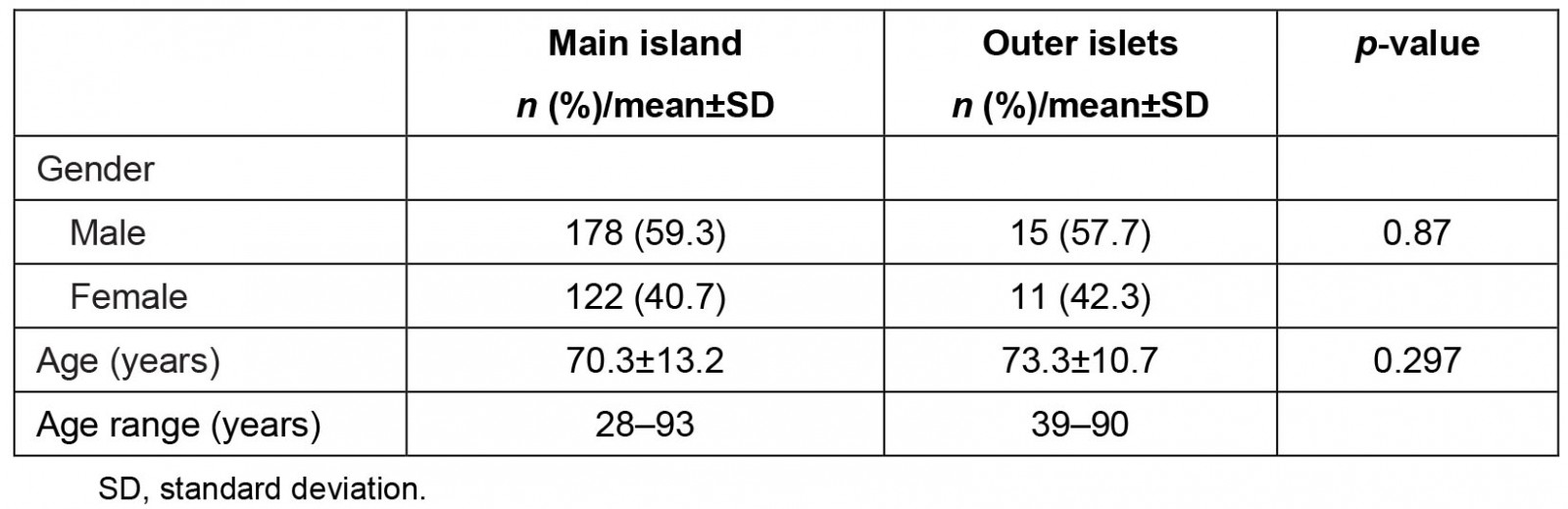
Table 2: Prevalence of some risk factors for main island and outer islet residents admitted to Putuo Hospital with ischemic stroke, 1 January – 31 December 2021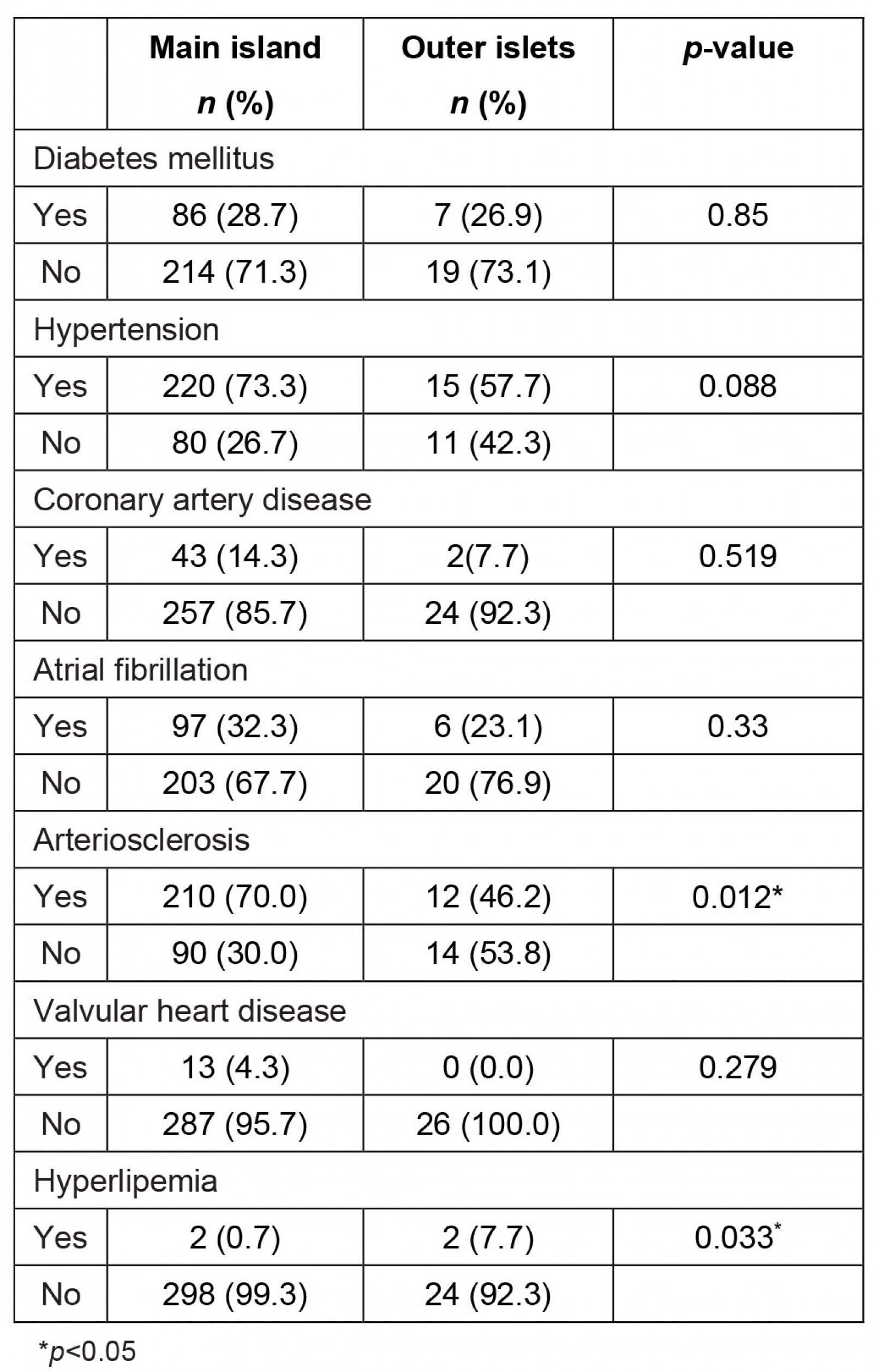
Table 3: Peri-admission management parameters for main island and outer islet residents admitted to Putuo Hospital with ischemic stroke, 1 January – 31 December 2021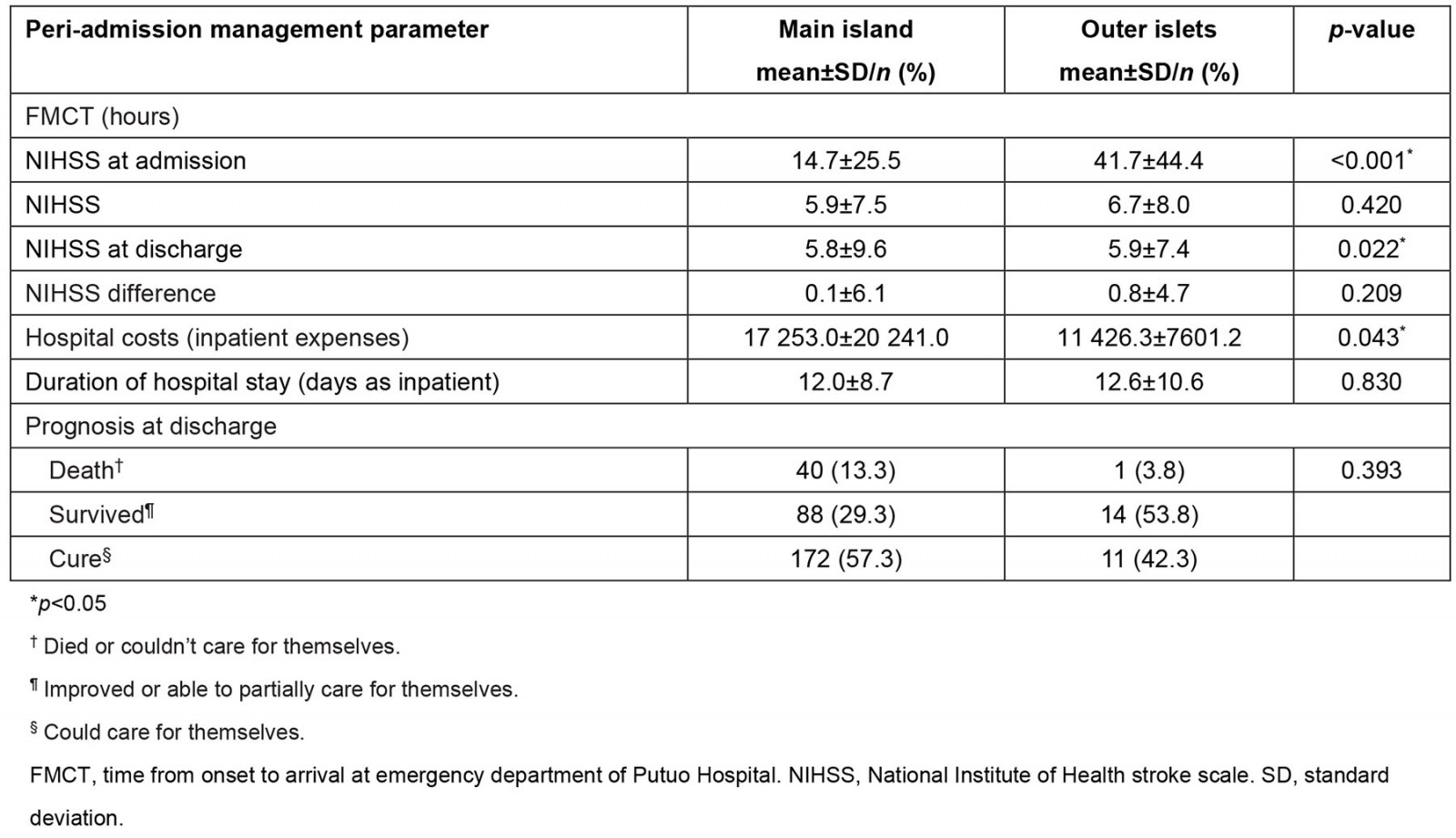
Table 4: Odds ratios for IV thrombolysis only and definitive treatment for main island and outer islet residents admitted to Putuo Hospital with ischemic stroke, 1 January – 31 December 2021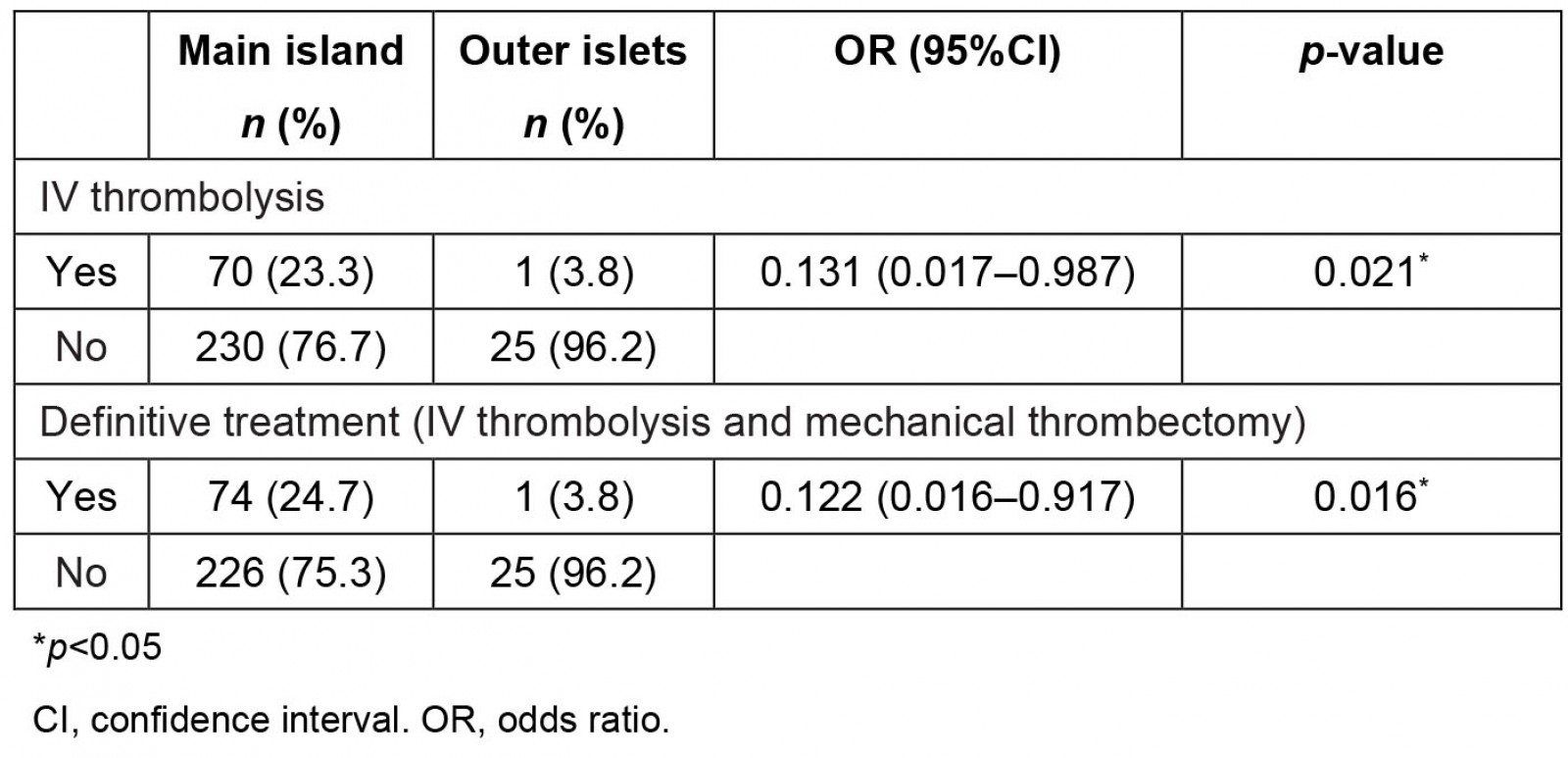
Discussion
Despite China’s rapid economic development in the past 30 years, there are large regional differences, and large disparities in the level of medical care relating to economic conditions. In this study, a single island district in eastern China, with more than 30 small inhabited islands under its jurisdiction, was selected as the study population. This selection is quite representative despite the size of the sample, and is consistent with the results of previous studies. This is the first time a study is able to bring forward a realistic presentation of the management of ischemic stroke in an archipelago area in China. It therefore represents the current circumstances of emergency care for all acute illnesses in the island areas of China. It is also noted how, similarly, even in developed countries such as Australia, there is a general lack of medical care in outer marine regions12. This is also true regarding emergency medicine care12.
For the population living in the outer islands of Putuo District, Zhoushan, acute conditions requiring urgent treatment may be delayed, with the results of the comparison of acute ischemic stroke patients being a typical example. Patients from both OIs and MI had delay in reaching the stroke center; however, those who had warning symptoms of stroke on OIs had to wait longer and pay more to cover urgent transportation.
Throughout 2021, only 1 out of 26 patients from the OIs reached the MI stroke center within the therapeutic time window for IV thrombolysis and managed to receive treatment. None of the ischemic stroke patients were treated with mechanical thrombectomy, although some patients chose not to have mechanical thrombectomy due to the higher cost.
In developed countries, such as Japan13 and the UK, emergency helicopters are used to proactively transport patients in a timely manner, but it is difficult for residents of less developed countries and rural areas in underdeveloped countries to afford helicopter transportation. Even though the local government has operated an emergency boat transportation policy since 2017, only 6 out of 26 patients in 2021 were transferred by emergency transport boats. Patients should pay a third of the whole transportation cost according to the Chinese emergency transportation policy of 2017, and the cost ranges between 500 and 1500 Chinese yuan. (The average wage was 57,727 Chinese yuan in 2020, according to the Chinese National Bureau of Statistics.) The remaining 18 emergency cases observed opted for regular daytime scheduled passenger boats, which considerably postponed the FMCT to reach the indication of definitive treatment of acute ischemic stroke. Emergency medicine in island regions has been characterized by regional centrality and local hollowing out of primary care, which is conspicuous in relation to emergency care14.
Factors delaying definite treatment are pre-hospital factors (those occurring before a patient’s arrival at stroke center) and in-hospital ones. The pre-hospital ones are the most responsible for delay to timely definitive treatment, which consists of patient-related factors and system-related delays.
According to the results of China’s 7th National Census, the proportion of people aged 60 years and above in Putuo District increased by 9.79% compared to 2010. Most young people would like to move into the MI for the more and better job opportunities. This contributes to the larger proportion of the aging population in Putuo OIs.
The older age groups in China’s rural and remote island regions generally have a lower level of health literacy and are more likely to live alone. This can result in delayed recognition of stroke symptoms, and has been confirmed as a major cause of pre-hospital delay15-20.
Regarding system%u2011related factors, education and training of local medical staff in stroke recognition has been shown to reduce pre-hospital treatment delays21. There is a regional imbalance in China's health care, and although the Chinese government has gradually established and strengthened community health service centers, the high cost of transfer of patients to high-level medical centers makes it difficult for primary care to play its full role. This phenomenon is even more obvious when observing OIs, where there is a shortage of primary health care workers. Inadequate training also impacts care, especially in the management of emergencies and critical illnesses. This is very similar to the situation across various island areas around the world with different levels of economic development12,22-24.
Comparison of rural/regional areas with metropolitan areas has proved consistent with available evidence that distance from a stroke center increases onset-to-needle time25,26. Longer distances led to increased delay and decreased chance of definitive treatment for acute ischemic stroke patients in remote OIs. This group must await boats for transportation and are sometimes locked down due to typhoons from the Pacific Ocean or other conditions.
Therefore, solutions must be designed and carried out in the future. Improving the quality of acute care in remote and rural areas requires the guidance of high-level medical resources, especially for time-dependent diseases such as acute ischemic stroke, so tele-mentoring at the pre-hospital level has been highly attractive as a promising solution, with the potential to rapidly optimize acute care at a limited cost27-29. However, there is a significant economic cost challenge to remote emergency care, which requires government coordination, and studies demonstrate that remotely directed emergency care can reduce overall healthcare costs27,30. The use of augmented reality technology for remote real-time guidance allows primary care physicians on OIs to be guided by experienced, high-level medical providers to handle emergency patients according to standards more efficiently and effectively28,31.
An OI physician training program that focuses on emergency medicine training would enable OI primary care physicians to be able to recognize and provide basic but standard management of various emergencies and critical illnesses32,33, which can also be simulated through augmented reality technology34,35. Regular health education dissemination for people in OIs should focus on when and from whom to seek emergency assistance30,35,36, and how to seek support from government departments and higher level hospitals19. It should be promoted that the larger islets with populations over 5000 need a CT machine to exclude hemorrhagic stroke and to have pharmaceutical preparation for IV thrombolysis3. The CT scan could distinguish more acute diseases.
Limitations
This study was retrospective research with selection bias and information bias. The case search was performed through the only stroke center of the district, but it was impossible to identify all the ischemic stroke cases who did not seek medical attention, especially those who experienced and/or died from ischemic stroke who were limited by poverty or loneliness. There may have been recall bias in relation to symptom onset address clarification through making telephone calls to the relatives of the victims.
The other limitation of this study concerning the data collected was the inaccurate residential address of many of the patients. As well as the results of ischemic stroke patients, it was found that, of the whole population including 77 patients suffering from various emergency care demands originally registered on OIs, 40 patients had already moved to MI (Supplementary table I). This data was confirmed via telephone calls to all patients.
Conclusion
Through the Putuo study, it was clarified that the diagnosis and definitive treatment (IV thrombolysis or mechanical thrombectomy) of acute ischemic stroke patients from OIs was significantly postponed when comparing with those from MI. Therefore, new effective and efficient solutions such as high-efficiency and convenient telemedicine through augmented reality are urgently needed.
References
You might also be interested in:
2019 - Social and community networks influence dietary attitudes in regional New South Wales, Australia


