Introduction
WHO recognizes ‘Health for All’ as one of three core priorities for universal health coverage1,2. Telemedicine is a tool that has the capability to accomplish the goal of health care for all: it increases access to health care for people in rural areas, where specialists are especially scarce.
A common model for telemedicine programs is the hub-and-spoke model, in which ‘hub’ tertiary hospitals provide access to resources for smaller ‘spoke’ hospitals3. Patients who present to the spoke hospitals consult with a specialist from the hub hospital on-demand and without traveling. In this way, hub hospitals can expand their reach and provide high-level care to communities that are not physically nearby. Many spoke hospitals are in rural areas that are medically underserved, so this model of telemedicine increases the accessibility of quality care in these areas. Although telemedicine has shown great potential to increase access to health care for patients in need, the question of the most effective technology remains.
Telemedicine robots, computers on wheels with cameras and proprietary software, are commonly used in teleneurology programs4,5, but this technology can be problematic because staff must be trained to use it, and it is often very expensive6,7. Therefore, some telemedicine programs have been turning to lower-cost technologies, such as tablets5,8-11.
The Department of Veterans Affairs (VA) emerged as a leader in telemedicine starting in 2003 with the launch of their national program, which eventually included many subprograms, including teleneurology11,12. Early on, the program utilized telemedicine robots, but issues with maneuvering, the need for staff training and high cost inhibited success13. Therefore, the VA program decided to abandon the use of robots, instead looking to tablets. The VA telestroke program, which started in 2017, now serves over 30 medical centers and thousands of stroke patients using tablets11,12. Because of the VA’s longstanding use of telemedicine, their program serves as an example to other hospitals looking to implement telemedicine programs effectively.
Methods
On 28 February 2014, Vanderbilt University Medical Center (VUMC), in Nashville, Tennessee, USA, launched its teleneurology network program, based on a hub-and-spoke model that was approved by the Vanderbilt Institutional Review Board. The goal of the teleneurology network is to elevate specialty care and its accessibility while allowing patients to stay close to their work, homes and families. When a neurology patient visits a community hospital, their community physician can request a consult with an on-call Vanderbilt neurologist14. Without this program, the patient would have to be transferred. To date, the network has reached 12 community-based hospitals across the states of Tennessee and Kentucky. This network includes five hospitals in counties with medically underserved areas, and four hospitals in counties that have medically underserved populations, according to the Tennessee Department of Health15.
This teleneurology network utilizes iPads, and consults are conducted over FaceTime. Staff in Information Technology at VUMC reported that this technology complied to the Health Insurance Portability and Accountability Act 1996 (HIPAA) when linked over password-protected internet connection. Images from local hospitals are viewed using Jenesis, a secure image-sharing application developed at VUMC. Satisfaction surveys have been administered to all community hospital physicians starting in May 2014 and patients starting in February 2018, and the results are collected and stored in REDCap, a web application developed at VUMC that securely stores data. The surveys were administered after the consultation was complete. If a physician requested multiple consults, surveys were administered after each one. Patient surveys were emailed to patients with known email addresses. The questions asked to physicians and patients in the surveys are shown in Tables 1 and 2, respectively.
Ethics approval
IRB #180277 ‘Teleneurology Quality Improvement Data Review’ does not meet the criteria for research as described in 45 CFR §46.102(d), and institutional review board approval was not required.
Results
Since the program’s commencement in 2014, a total of 14 241 teleneurology consults have occurred at 12 different community hospitals (Fig1). After their consults, 87% of patients continued to be cared for in their familiar community settings. The rest of the patients required transfer to a higher level of care (12% to VUMC, 1% to non-VUMC hospitals).
Patients with a wide variety of diagnoses have been able to use the teleneurology program (Fig2). The most common diagnosis for a patient using the telemedicine consults is stroke or suspected stroke (26.9% of consults), followed by seizure (11.2%), altered mental status (8.7%), headache or migraine (7.01%), weakness or hemiparesis (6.79%), follow-up (5.45%), and paresthesia or numbness (4.61%).
The community physicians surveyed were widely satisfied with the VUMC teleneurology service (Table 1). The response rate of physicians was 13%, and the total number of responses was 269. Notably, 96% of physicians were either very satisfied or somewhat satisfied with the service overall. The results of patients surveyed also reflected widespread satisfaction (Table 2). The response rate was 21%, and the number of patients surveyed was 381. Importantly out of the patients that had direct communication with the remote physician, very few had difficulty seeing or hearing their provider, and 97% felt they were treated with courtesy and respect during the service.
Table 1: Physician survey results for teleneurology service, Vanderbilt University Medical Center (n=269) 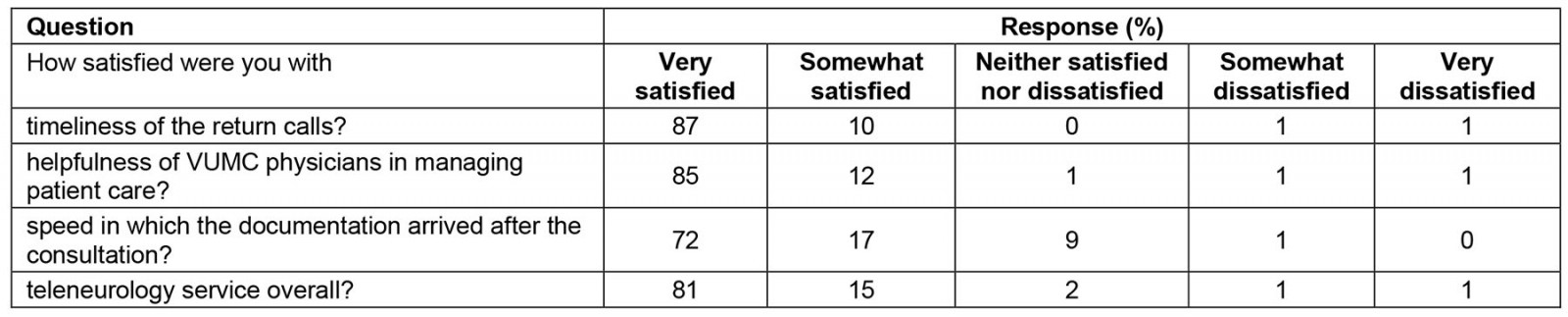
Table 2: Patient survey results for teleneurology service, Vanderbilt University Medical Center (n=381)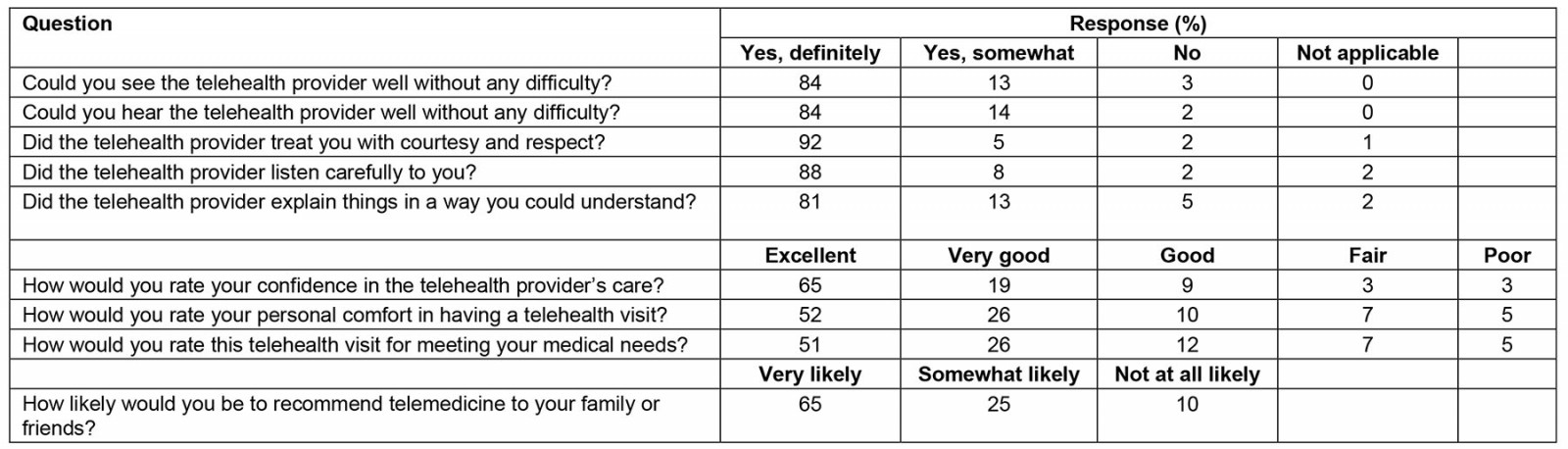
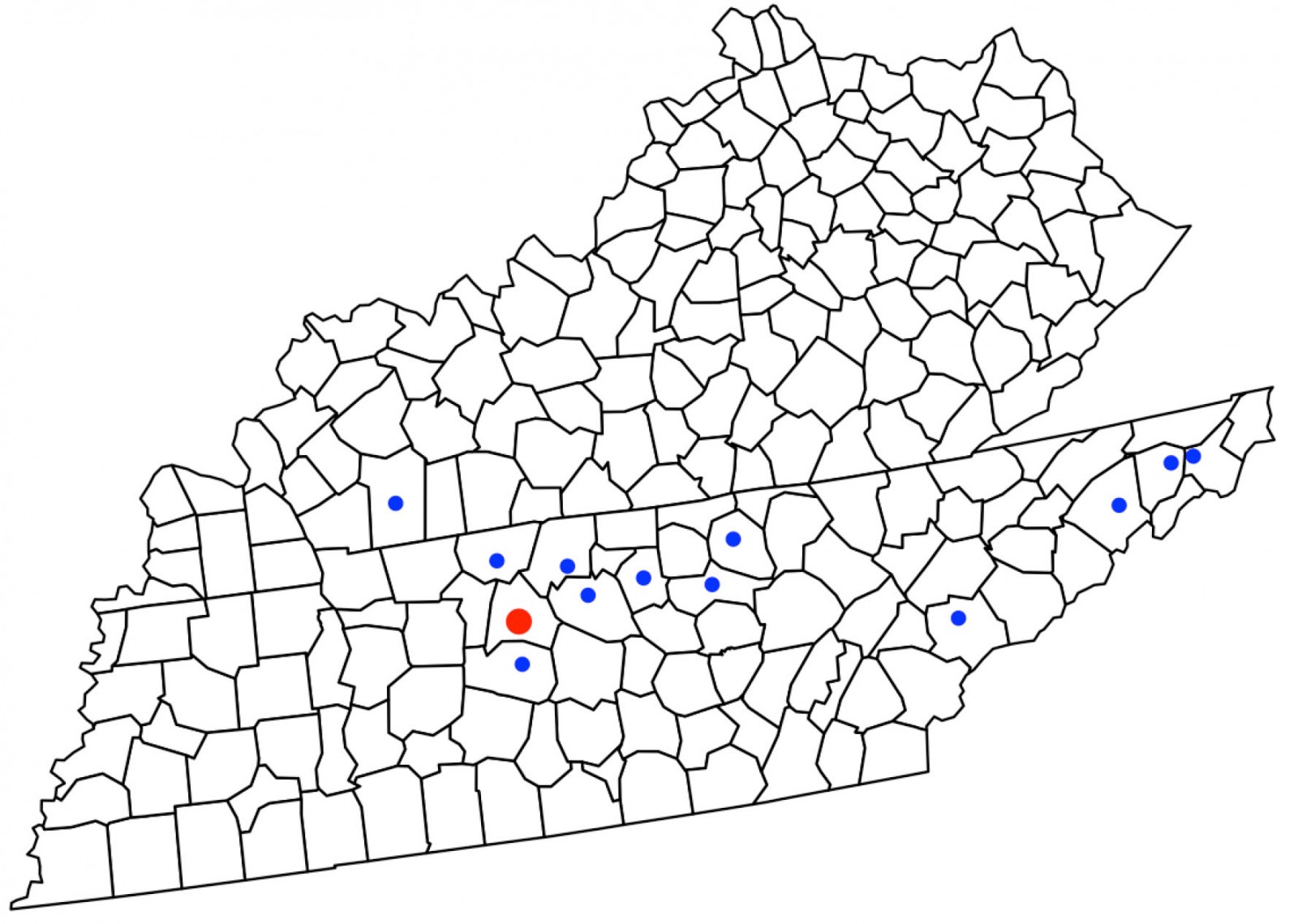 Figure 1: Locations of hospitals that have participated in the Vanderbilt University Medical Center (VUMC) teleneurology network. The red dot represents VUMC, and the blue dots represent community hospitals. Not all community hospitals represented are currently in the network.
Figure 1: Locations of hospitals that have participated in the Vanderbilt University Medical Center (VUMC) teleneurology network. The red dot represents VUMC, and the blue dots represent community hospitals. Not all community hospitals represented are currently in the network.
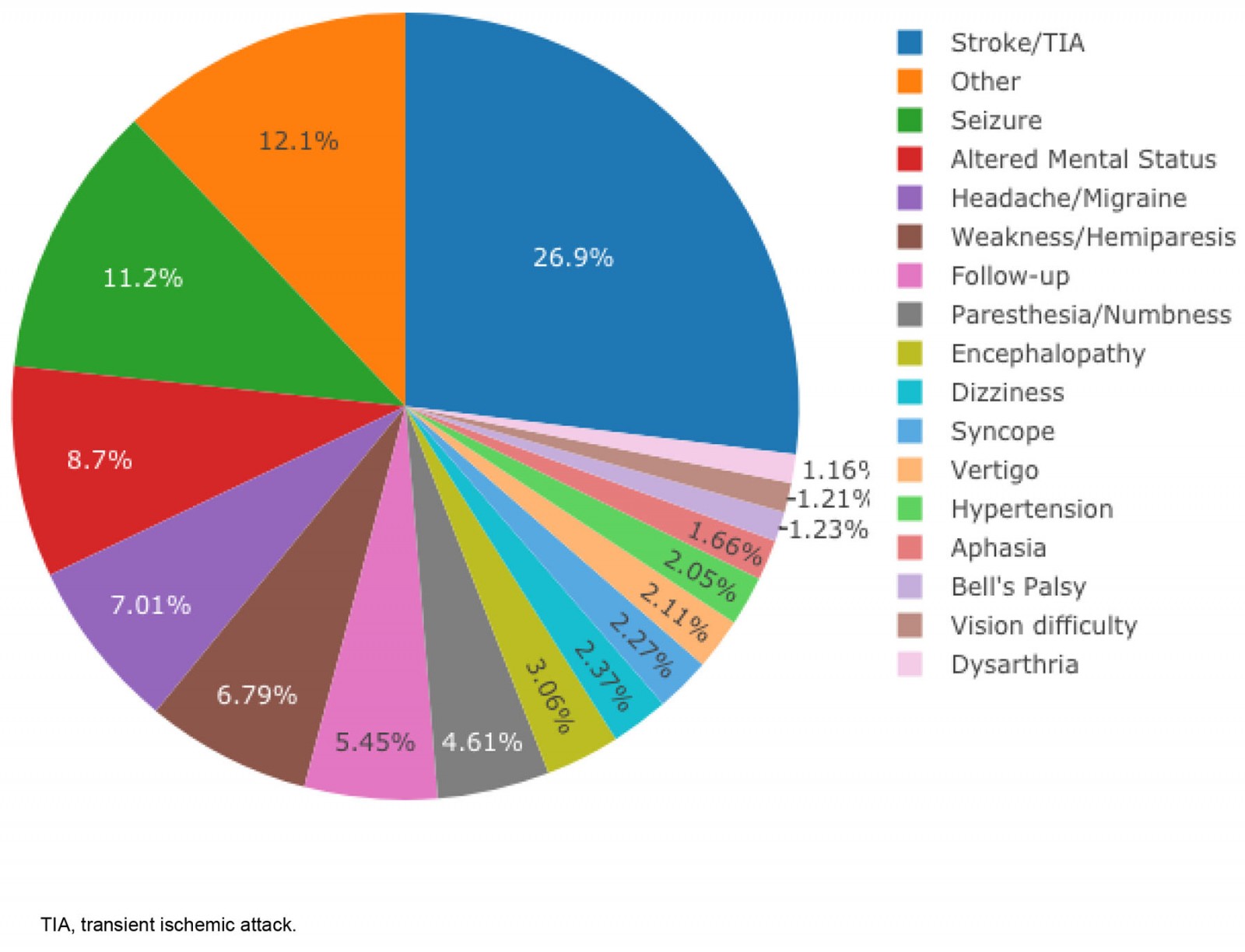 Figure 2: Proportion of patients with various diagnoses who received a teleneurology consult. Stroke patients most commonly use the teleneurology service, but the service has been helpful for a wide variety of other diagnoses.
Figure 2: Proportion of patients with various diagnoses who received a teleneurology consult. Stroke patients most commonly use the teleneurology service, but the service has been helpful for a wide variety of other diagnoses.
Discussion
The data collected for 6 years of teleneurology consults at VUMC show that using tablet technology for teleneurology is highly effective, in the opinions of both patients and physicians. Furthermore, the use of tablet technology is intuitive because of the presence of tablets outside of the context of teleneurology; it is likely that users have pre-existing knowledge about how to operate a tablet. It takes very little staff training to initiate or answer a call for a video visit, which further decreases the barrier to care.
Tablet technology is exceptionally low cost, especially when compared to other types of telemedicine robots. The concern of HIPAA compliance is mitigated by the use of encrypted password-protected networks, software and applications. Lastly, as shown by the near-perfect report of patients able to see and hear the physicians without difficulty, the iPads used at VUMC and community hospitals are extremely reliable. The positive outcomes of this program communicate that implementing a telemedicine program does not necessitate buying expensive equipment that increases burden, which is especially significant for smaller community hospitals. In rural settings, specifically in underserved areas or areas that have underserved populations, increasing accessibility to specialty care through telemedicine improves health outcomes without the added burden of travel or the cost of hospital transfer for patients.
These results should be interpreted with limitations in mind. The participating hospitals, physicians and patients in this study are limited to a small section of the USA. This study was not randomized or controlled, so its results cannot be applied to a broader population, and confounding variables cannot be ruled out. Additionally, the percentages of physicians and patients completing the satisfaction survey were low, signaling the possibility of a sampling bias; it is possible that the participants who felt compelled to respond had an experience to report that the service was better or worse than the true average experience. Only patients with email addresses on file were asked to complete the satisfaction survey; this introduces the possibility that the average patient surveyed had a greater sense of technological fluency than the true average patient. All aforementioned possibilities could have introduced bias and influenced the outcomes.
Conclusion
The findings at VUMC show the potential of tablet technology to increase financial accessibility of telemedicine programs for hospitals nationwide. Third-party platforms utilizing telemedicine robots are cumbersome and expensive; on the other hand, tablets allow the growth of telemedicine to be nearly boundless. Adapting to the COVID-19 pandemic necessitates the use of technology that can be implemented quickly and on a large scale. By adopting telemedicine programs, hospitals can greatly improve access to quality specialized care for patients with geographic or clinical barriers.
Funding statement
This research was not funded by outside sources; it is a review of data from a Quality Improvement project.
Conflict of interest statement
Kelly Harper, Claire Hanson, Bryan Eoff, and Dr. Derek Ribeau have no competing financial interests. Vanderbilt University receives income from grants or contracts Allergan, Ipsen, Impax, Medtronic, Merz, Pharma Two B and Voyager for research or educational programs led by Dr David Charles. Dr Charles receives income from USWorldMeds and the Alliance for Patient Access for consulting services.
References
You might also be interested in:
2009 - The impact of recession on the health of rural citizens in British Columbia, Canada

