Introduction
Attracting and retaining healthcare workers in remote and rural areas is still a challenge in the world1,2. The recruitment and retention issue is critical, especially in providing health services to achieve WHO’s Sustainable Development Goals (SDGs)3. The world road map to meet the need for competent and qualified healthcare workers in 2030 also considers the strategy for recruiting and retaining healthcare workers4,5. Developed and developing countries, including Indonesia, experience the problem of attracting and retaining healthcare workers6,7.
Indonesia adheres to a health system with a target of universal health coverage. The Central Government has established the Sistem Jaminan Sosial Nasional–Kartu Indonesia Sehat (SJSN–KIS, National Social Security System–Healthy Indonesia Card), with the Badan Penyelenggara Jaminan Sosial Kesehatan (BPJS, Social Security Agency of Health) as the institution that manages the implementation of health insurance and services for the community8. To support this, it is necessary to have an equal distribution of health workers, including the distribution of specialist doctors in hospitals9. Until recently, Indonesia has been one of the countries experiencing a shortage of healthcare worker resources, especially specialist doctors10. Global health workforce labor data in 20175 indicates that the proportion of specialist doctors available in public hospitals is more than 80%11. However, there is a relatively large disparity between provinces in Indonesia, where many specialist doctors stay in big cities such as Daerah Khusus Ibukota Jakarta, Daerah Istimewa Yogyakarta, and Bali11. The total number of medical specialists in Indonesia is approximately 38 782, mostly in Java–Bali Island. According to data from the Indonesian Ministry of Health in 202011, Jakarta, Jawa Barat, and Jawa Timur accounted for 18 040 medical specialists. Factors affecting retention of medical specialists are related to age, gender, marital status, infrastructure, and opportunity for dual practice12-14.
Through the regulation of the Ministry of Health in 2020 concerning licencing and hospital classification, the number and qualifications of human resources (including specialist doctors) are adjusted according to workload, needs, and capabilities of hospital services15. This is in line with Ministry of Health Regulation 69 of 2016 concerning Implementation of Mandatory Work for Specialist Doctors in Fulfilling Specialist Service Needs in Indonesia, which was later replaced by the Ministry of Health Regulation 36 of 2019 concerning the Implementing Regulation of the Presidential Regulation 31 of 2019, which states that requests to fulfill the need for specialist doctors through the Mandatory Specialist Doctors Work program (later the Pendayagunaan Dokter Spesialis (PGDS, Specialist Doctors Utilization program)) were submitted by hospitals and local governments after seeing the results of workload analysis or plans for hospital human resource needs16.
The PGDS is one of the breakthrough government efforts to distribute specialist doctors to all corners of Indonesia, especially for public hospitals in disadvantaged areas, borders and islands17. For the PGDS, the placement of specialist doctors is not mandatory for new graduate specialists18-20.
PGDS participants are students who have passed the professional education program for specialist doctors, and students who have passed the adaptation program, at universities that have received educational funding assistance from the Central Government. PGDS participants comprise graduates of five basic specialist doctors: obstetrics and gynecology specialists, pediatricians, internal medicine specialists, surgeons, and anesthesiologists, and for the addition of types of specialization other than those mentioned will be determined by the Minister of Health. They will be placed in hospitals owned by local governments and the Central Government (priority in remote, border, and island areas), and regional and provincial referral hospitals17.
The placement period for specialist doctors in the PGDS is 1 year. However, doctors can reapply to be placed back in the area with the same program. Figure 1 outlines the placement of specialist doctors in the PGDS.
One of the main concerns in the PGDS is the effort to maintain the retention of specialist doctors on duty at their assigned places. Retention is an organized effort to establish an environment that motivates employees to remain in their jobs by implementing appropriate policies and interventions designed to attract and recruit healthcare workers who have recently graduated, left work, worked in another profession, or retired21.
Good retention of healthcare workers in an area is needed to build trust between healthcare workers and clients6,22. In addition, staff productivity will increase so that health programs can run effectively and efficiently23,24. The lack of healthcare workers in an area will certainly affect the health services provided in that area13,25. It is believed that the recruitment of new healthcare workers often requires a large amount of money and takes a long time22. The exit of healthcare workers from a health service organization will impact health services, the organization as a whole, and the organizational components26. These impacts are clearly seen, especially in rural and remote areas where the number of healthcare workers is insufficient and the distribution is not even27,28.
The implementation of this PGDS involves various stakeholders, including local governments. The general mechanism for submission of plans by specialist doctors in hospitals to the central government through the PGDS shown in Figure 217.
Knowing the factors that affect the retention of specialist doctors in a placement area is very important for stakeholders in making decisions and establishing policies related to the distribution and utilization of specialist doctors.
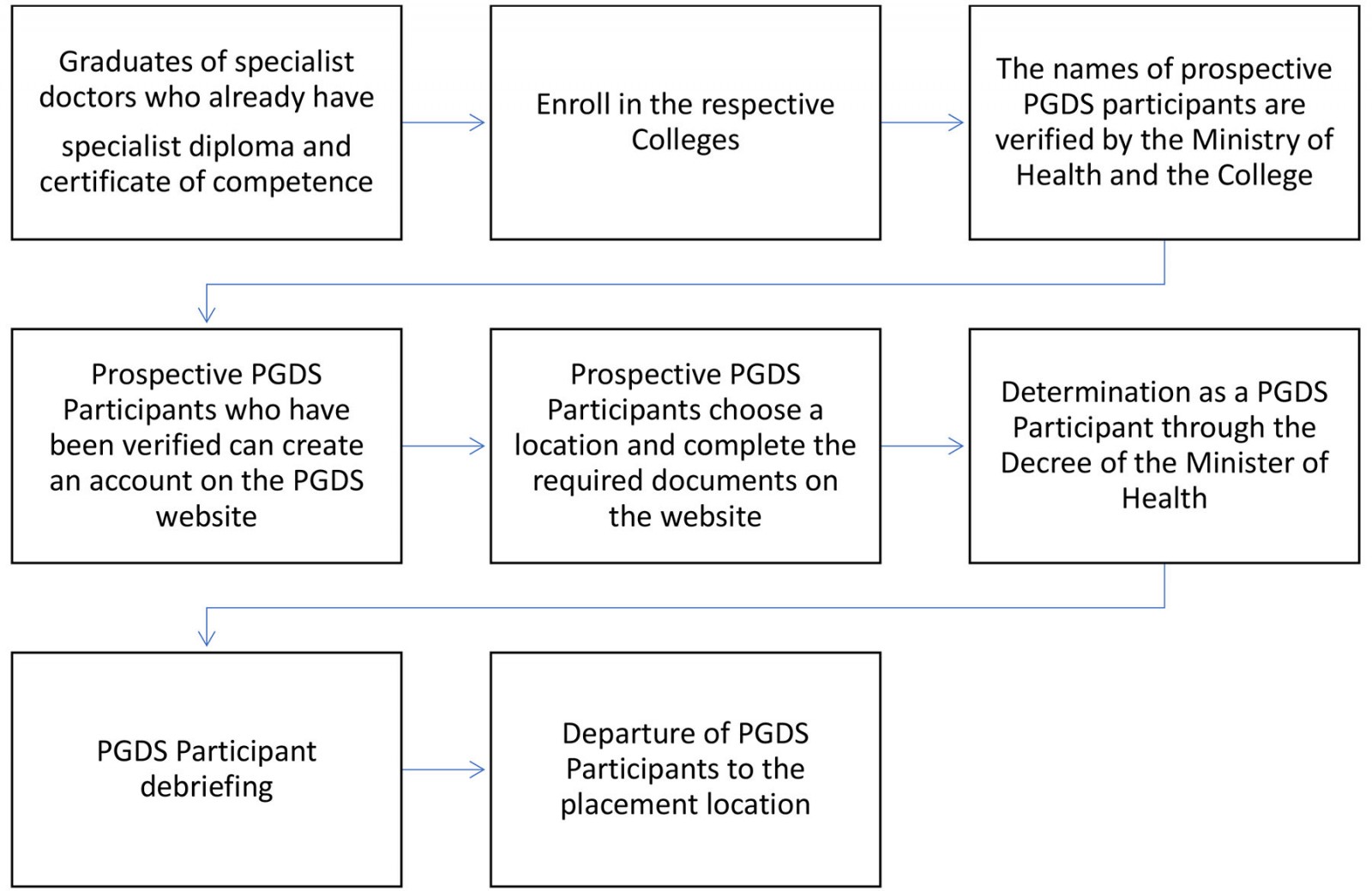 Figure 1: Outline of the Specialist Doctors Utilization program.
Figure 1: Outline of the Specialist Doctors Utilization program.
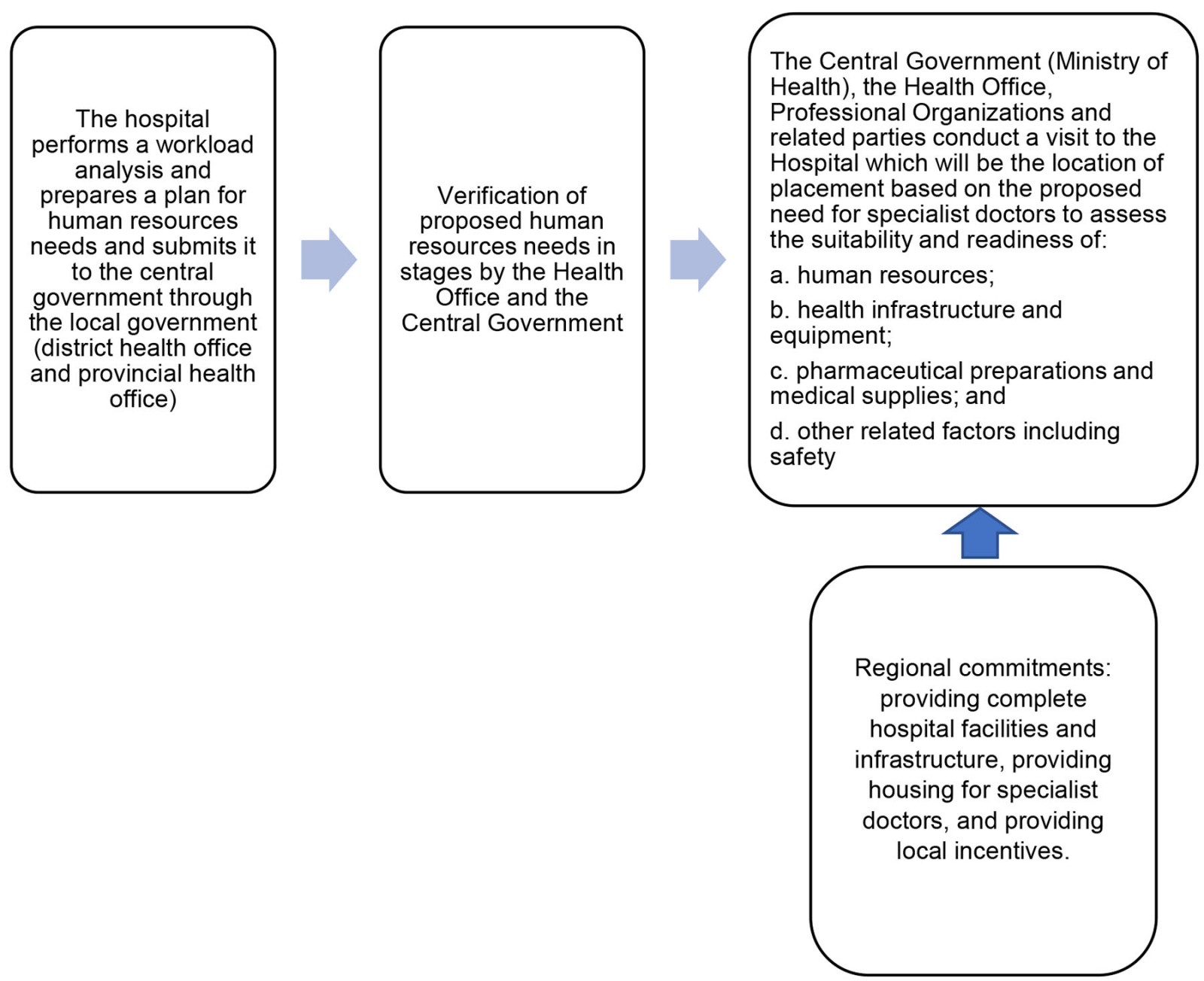 Figure 2: Stakeholders of the Specialist Doctors Utilization program.
Figure 2: Stakeholders of the Specialist Doctors Utilization program.
Methods
Study design
This study had a qualitative descriptive approach using realist evaluation design, which can capture evaluative conclusions for a program in more detail through the configuration of context, mechanism, and outcome (C–M–O). The context is population characteristics, types of organizations, and human resources to culture. The mechanism is the process that arises from specific program interactions. The outcome is the changes that occur due to the interaction between context and mechanism. So, in the C–M–O configuration, the realist evaluation can explain in depth what programs are not optimal, and the social groups, conditions, and process patterns. Therefore, realist evaluation can capture evaluative conclusions on a program in more detail29.
The research locations are in eight provinces representing seven regions of Indonesia: South Sumatra, West Java, Bali, East Nusa Tenggara, Central Kalimantan, Southeast Sulawesi, North Maluku, and West Papua. Respondents were specialist doctors participating in the PGDS, professional organizations, eight provincial health offices, and eight selected district/city health offices over Indonesia.
Data collection and analysis
After obtaining ethics approval, the team conducted a trial of the instrument. The instrument trial was conducted in the Thousand Islands (Kepulauan Seribu), Jakarta for specialist doctors participating in the PGDS and professional organization branches, and other stakeholders. Several interviews were conducted online because the research took place during the COVID-19 pandemic. Direct interviews were carried out in compliance with health protocols by maintaining distance and wearing masks. The test results are the basis for improving the instrument for data collection in the field.
The research was conducted from February to December 2021, and data collection was carried out for approximately 2 months. Eight teams gathered the data for this research. Each team was responsible for data collection and analysis in one province. Before data collection, the team first contacted the relevant provincial health office and the district/city health office for permits and identified the person in charge of the program at the health office and hospitals regarding the PGDS. The hospitals where PGDS participants are placed were chosen as data collection sites. The research team contacted the five basic specialist medical professional organizations at the central level to complete the data. They provided specialist doctors’ names and contact numbers from the regional representative professional organizations who could be interviewed.
The collected data comprised individual factors for specialist doctors, regional commitments and community aspects that affect the retention of specialist doctors. Retention here is considered as PGDS participants completing 1 year according to the period of placement in the PGDS, or extending their placement period in the area so that there is an occupancy of specialist doctors every year. There is no retention if the specialist doctor does not complete the 1-year placement period.
Although PGDS participants can choose their placement locations, they may feel uncomfortable due to factors such as completeness of hospital infrastructure, provision of incentives, and community acceptance. Interrater bias was minimized by retaining and sharing details of coding, categories, and names of interviewers. Any disagreements between teams were discussed and resolved during the discussion.
There were 58 respondents in this study, from provincial health offices (8), district/city health offices (8), hospitals (8), university faculties of medicine (3), professional organizations (21), as well as PGDS participants (10). Data were collected through in-depth interviews using a structured questionnaire tested previously. Interviews were conducted with the person in charge of the PGDS at the provincial and district/city health offices, the head or person in charge of the PGDS at the hospitals, doctors participating in the PGDS, the chair or representatives of specialist medical professional organizations in each region as well as selected medical faculties representing the provinces where the data were collected. The professional organizations of specialist doctors interviewed were the Association of Obstetrics and Gynecology Specialists (POGI), Indonesian Association of Internal Medicine Specialists (PAPDI), Indonesian Association of Pediatricians (IDAI), Indonesian Association of Surgeons (PABI), and Association of Anesthesiologists and Intensive Therapists (PERDATIN).
All interviews were audio-recorded, transcribed, and manually entered in the matrix. The results from each province were then compiled and analyzed with the C–M–O analytical configuration.
Ethics approval
This research received ethics approval from the Health Research Ethics Commission of the Health Research and Development Agency (KEPK-BPPK) of the Ministry of Health (LB.02.01/2/KE.029/2021).
Results
Characteristics of respondents
As shown in Table 1, more than half (60.3%) of respondents of this study were male, and 37.9% of respondents had an age of 50 years or more. The 10 interviewed PGDS specialist doctors comprised anesthesiologists (4), pediatricians (2), internal medicine specialists (2), and surgery specialists (2).
From the results of this study, all respondents participating in the PGDS in the eight locations completed their placement period for 1 year. The availability of PGDS participants from secondary data for 2017–2020 in eight locations is shown in Table 2.
Table 2 shows that all provinces were continuously filled with PGDS participants from year to year, except for Bali. From the secondary data, Bali had PGDS participants in 2017 and 2019, but not 2018.
The in-depth interviews (Table 3) identified several contexts related to the retention of specialist doctors in placement areas. These are grouped into the context of individual considerations and the context of regional commitments. The context of individual considerations consists of geographic as well as demographic and socioeconomic factors. The context of regional commitments consists of the availability of regional incentives, provision of infrastructure for PGDS participants, fulfillment of hospital infrastructure, and opportunities for the career development of PGDS participants. In the context of geographical factors that specialists consider, a location in which a specialist has previously worked or trained is more favorable. Examples are an area that has been an internship site, the area of origin of the doctor and his family, or a well-known tourist area such as Badung in Bali province, and Wakatobi in Southeast Sulawesi province. Geographical factors also consider the placement area’s access to the provincial capital or the individual’s area of origin. Included in the demographic and socioeconomic context are the number of residents compared to the number of hospitals, security of the placement area (not conflicted or vulnerable areas), public facilities, or supporting social facilities such as the existence of good and adequate schools, and places to buy basic supplies. It also includes a society that is open to immigrants and the ability of the community to pay for medical treatment outside of BPJS, and for sembako (nine basic, essential commodities, such as rice and eggs).
The context of regional commitment is the amount of incentive from the regions, including reliable payment; fulfillment of regional infrastructure facilities for specialist doctors such as decent houses and vehicles; fulfillment of infrastructure facilities in hospitals, especially those related to medical equipment needed by the specialist doctor to provide health services; as well as career development for specialist doctors in the future, such as opportunities to participate in training/capacity development.
The mechanism that emerges from the context (context of individual considerations and the context of regional commitment) is that the specialist doctor decides to choose the area and then feels at home both professionally and socially. This is evident in the following interview comment:
What makes me feel at home is that the place is safe, there are no traffic jams, the work environment is good, so my relationship with the specialist and nurses, is good … so it is very comfortable and not a burden. Yes, I feel at home because I get two incentives in total, and it is big too. I also get some services from patients, it is not appropriate, but it is okay. I think of it as dedication. So that is enough, what makes you grateful are those two incentives, so it is pretty good to make you feel at home. I just thought about how my friend, who only gets a salary from medical services, cannot get local incentives. Yes, I just thought that luckily I got two here, sir …' (participant 6a)
The placement of specialist doctors in the PGDS is only for a year, but doctors can revisit them after their assignment period ends. If the area is considered suitable, the specialist will select the area to be the placement area:
PGDS is good for distributing specialist doctors to regions because specialist doctors must be willing to be placed in areas that the Center has determined. PGDS, specialist doctors chooses [their] own hospital, and many factors determine the choice of the specialist, for example, regional incentives, housing, cars, and others. (participant 8)
For specialist doctors participating in the PGDS, selecting placement locations considers incentives and other things, especially family factors. This is supported by the following respondent statements:
So I see that the consideration is not merely an incentive, sir. His family is already here, and his wife is already a doctor there, so it is not just an incentive, sir. That is why he feels at home there. Yes, there are other factors, sir, especially your family, if the incentive is number two. (participant 6)
A work environment that can develop the professional abilities of specialist doctors is also one of the mechanisms of this research. Retention also occurs because specialist doctors feel financially secure because of monthly financial guarantees from both central and regional incentives. This can be seen in the following interview comment:
In my opinion, it comes down to financial matters, yes, ma’am, for the income may be greater in the city it is greater than here, we are small in comparison, ma’am. (participant 2)
I have asked several times. In my opinion, the amount of incentive received [Rp. 35,000,000 (~A$3500)] withholding tax is very small ... because compared to other regencies that have just opened, they are much larger. Because yes … we like it or not, we have to admit that incentives are the attraction of each region … if they don’t want to increase incentives, people will think about it, here it is given like this … for example in X and Y can be given twice as much as here, and people will definitely choose to go there … especially when there is only 1 hospital here. (participant 8)
The outcome of the context–mechanism configuration from the results of this study is divided into three levels: the individual level, the organizational level, and the community level. Individual-level outcomes are in the form of commitments from specialist doctors who are placed to work according to a predetermined time, which is for 1 year. In other words, doctors will not be absent from their assignments or leave their workplaces early. The organizational-level outcome is in the form of professional development for specialist doctors. In addition, patients’ needs for treatment by specialist doctors can be served without having to refer to a hospital in the provincial capital. Community-level outcomes in the form of health service targets in the regions can be achieved. When this happens, the regions can absorb National Health Insurance funds more optimally to increase regional income.
Table 1: Frequency distribution of respondents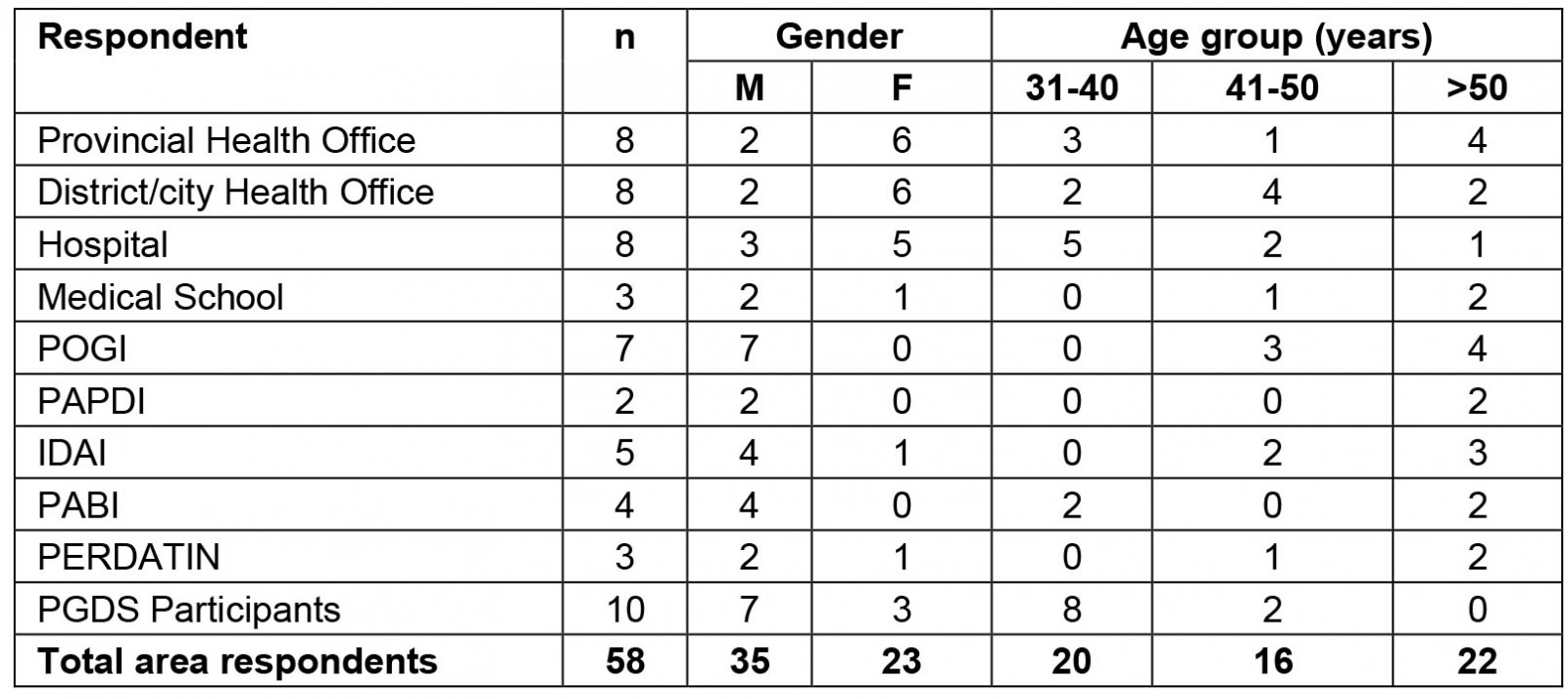
Table 2: Availability of participants in the Specialist Doctors Utilization program at eight research sites, 2017–2020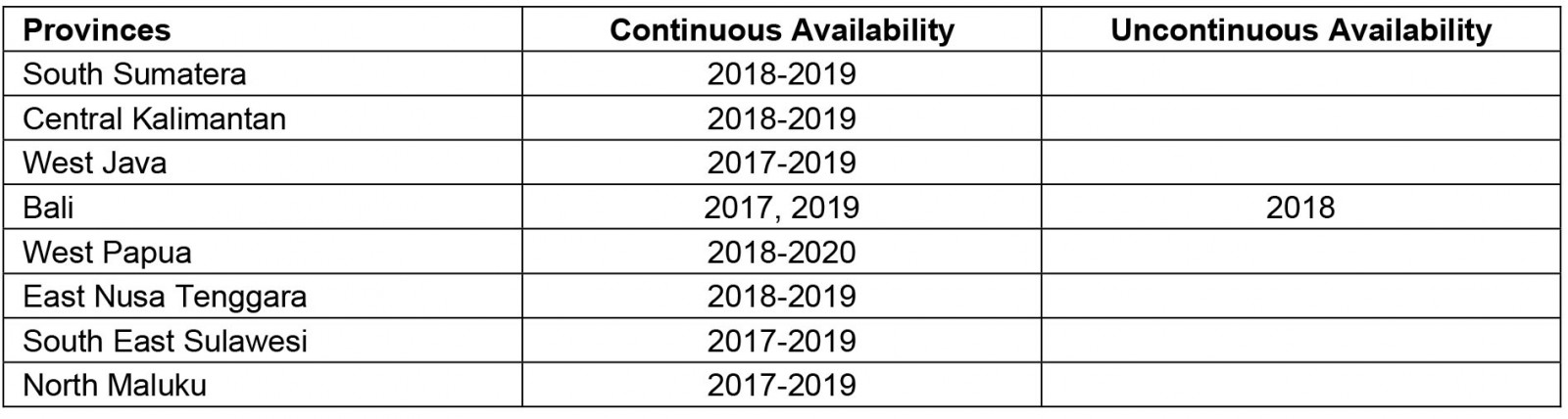
Table 3: Summary of realist evaluation of specialist doctors’ retention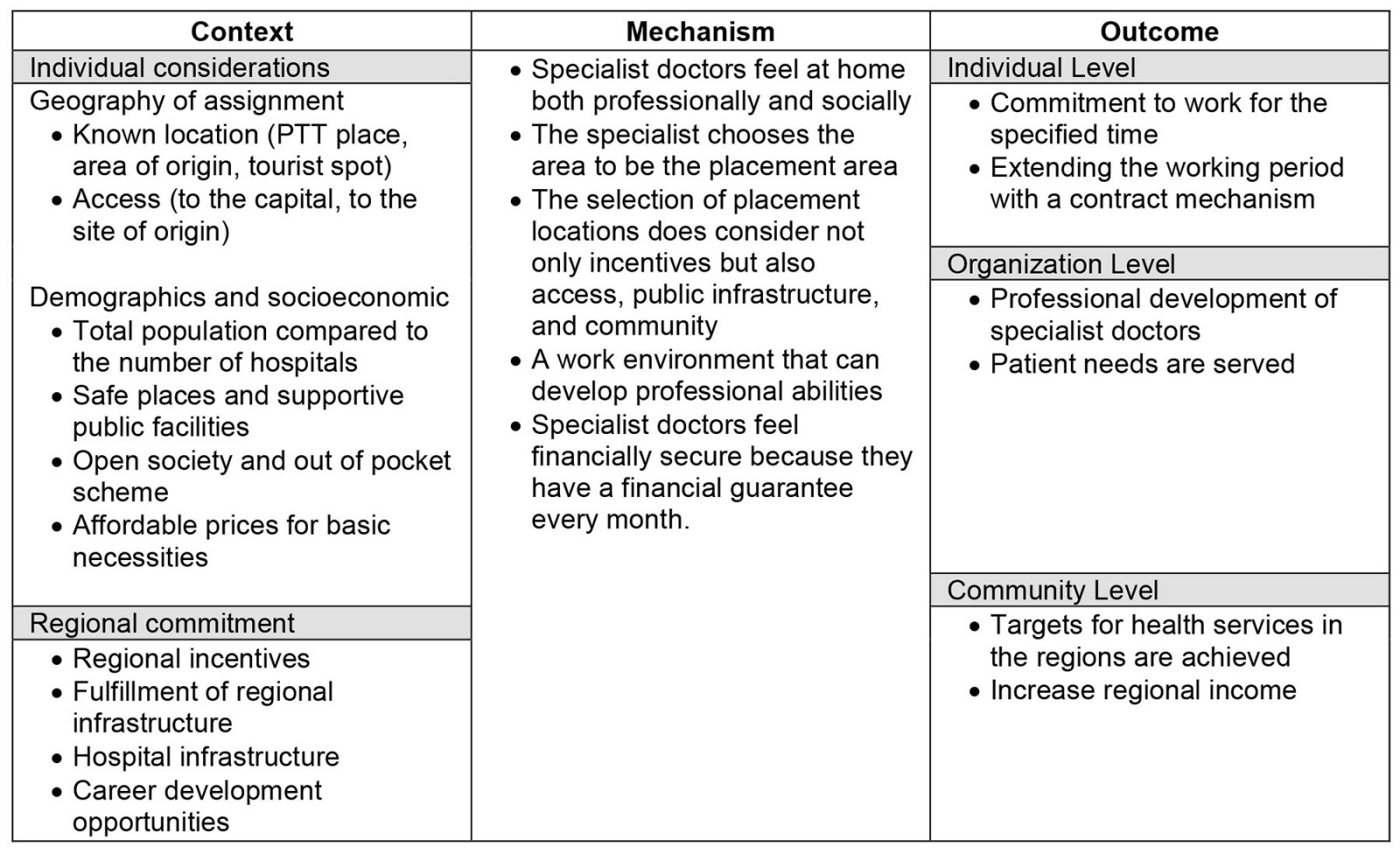
Discussion
Efforts to equalize distribution of healthcare worker resources, especially specialist doctors, through the PGDS still require some improvement, especially those related to the retention of specialists. Improvement efforts will consider the reasons for the retention of specialist doctors in placement areas, which from the results of the C–M–O configuration can be described as follows.
Context of individual consideration
Specialist doctors consider geographical, demographic, and socioeconomic factors, whether or not they feel at home at the placement location. In the context of geographical factors, the location of the assignment that has been previously identified and the ease of access to the provincial capital or the area of origin are considered. Demographic and socioeconomic factors are population size, security, and adequate public or social facilities. There is also the public’s openness to migrants, the community’s ability to pay for their treatment outside of BPJS, and for sembako (nine basic food commodities).
Regarding geography, demography, and socioeconomic factors, the results of research conducted by the the Indonesian Institute noted three major issues that are still a problem in the healthcare sector in Indonesia. One of these is the problem of infrastructure that is not evenly distributed and is inadequate. This can be seen in 9599 public health centers and 2184 hospitals in Indonesia, which are still centered in big cities. So there are still many people who cannot access health services because there are no healthcare facilities. Another reason is because some geographical locations are difficult to reach12,30.
In relation to demographic and socioeconomic factors, according to the National Development Planning Agency 202231, many healthcare workers, especially doctors, prefer to work in urban areas with many attractive private healthcare service facilities (pull factors). Specialist doctors are reluctant to work in hospitals in disadvantaged areas, borders, and islands due to limited health service facilities32.
Context of regional commitments
Based on the results of this study, regional commitments that affect the retention of specialist doctors are the availability of regional incentives, provision of facilities for specialist doctors, fulfillment of hospital infrastructure, and opportunities for specialist doctor career development. As stated in Ministry of Health Regulation 36 of 2019, during their placements period PGDS participants receive allowances from the Central Government. They also receive incentives from the relevant regional government, sourced from the regional revenue and expenditure budget according to the ability of the region. The inadequacy of both financial and non-financial incentives for specialist doctors is one of the causes of maldistribution of specialist doctors32. According to a study by Sigmananda in 2014, salary or incentives are one of the factors that can affect a person’s job satisfaction and the decision to keep working in a place or not33. Research conducted at H. Hassan Barry Kandangan Hospital showed that incentives are the dominant factor in doctor job satisfaction33. Ormel et al (2019) analyzed how incentives are related to the motivation of healthcare workers resources. His study showed that low motivation is influenced by a gap in expectations caused by low incentives, timely payment of incentives, and unequal incentives among healthcare worker resources34.
During the COVID-19 pandemic, one form of appreciation from the Central Government for healthcare workers has been the provision of incentives. This effort is expected to provide moral encouragement to healthcare workers to work harder in serving patients exposed to the coronavirus and is a motivational tool that is expected to improve the performance of healthcare workers. The provision of these incentives has been regulated in the Decree of the Minister of Health (DMH) Number HK.01.07/MENKES/4239/2021 concerning the Provision of Incentives and Death Compensation for Healthcare Workers Handling COVID-19. The DMH is an update of DMH Number HK.01.07/Menkes/278/2020 concerning Provision of Incentives and Death Compensation for Healthcare Workers Handling Corona Virus Disease 2019 (COVID-19)35,36. The results of research conducted by Rositoh et al (2021) show a significant effect of COVID-19 incentives on the performance of healthcare workers in hospitals37. Research on financial incentives is mainly carried out in African countries by including other combinations of interventions such as incentives in various forms (eg salaries and allowances). This intervention is very effective if carried out for a short-term retention program. The success rate is low in the long term if non-financial interventions do not accompany it38.
Availability and completeness of facilities from the results of this study are factors that affect the retention of specialist doctors. Complete hospital facilities are certainly very supportive of specialist doctors in providing specialist health services. According to the study by Robbins and Langton (2003), equipment used to support work, if it is not in accordance with the demands of the assigned task, can be a source of work stress39. Furthermore, if the work stress is high, it can damage the person’s performance39. The completeness of these facilities affects the retention of specialist doctors in the placement area. According to Dieleman and Harnmeijer (2016), one of the interventions to increase retention at the facility level is improving work facilities40.
Career development for specialist doctors as a form of regional commitment also affects the retention of specialist doctors in placement areas. According to Dolea et al (2020), motivation and retention of healthcare workers to work in remote and disadvantaged areas is relatively high if there is personal and professional support, such as improving living conditions for healthcare workers and their families41,42. In addition, a clear career path in favor of healthcare workers is an added value for healthcare workers to practice and stay there14,43. This is consistent with the results of the present study that unclear career paths cause specialist doctors not to extend their tenure, and to choose to move to other areas.
According to Syahmar et al (2015), career opportunities can affect student interest in working in rural areas during their studies44. Career opportunities have been regulated in Law Number 36 of 2014 concerning Healthcare Workers, which discusses special promotion rights for healthcare workers who work in disadvantaged areas, borders, islands, and areas with significant health problems. The regulation should ensure that healthcare workers in disadvantaged areas, borders, islands, and areas with health problems receive special promotion rights such as the opportunity to be a government employee45. If the regulation is implemented properly, it should increase the interest of specialist doctors to work in less desirable areas.
Outcome: retention of specialist doctors
Regarding retention, the results of the C–M–O configuration from this study indicate why specialist doctors feel comfortable working in areas where regional commitments are fulfilled, namely the provision of appropriate and timely incentives, the fulfillment of infrastructure, and the opportunity to develop a career. This feeling of belonging is indicated by the commitment of specialist doctors to work until their assignment period ends, and some extend their working period with a regional contract mechanism.
Retention of healthcare workers is needed to build trust between healthcare workers and clients. Retention can also increase productivity so that healthcare programs can run effectively and efficiently42. This is consistent with the results of the present study, that the outcome of the retention of specialist doctors is the fulfillment of the community’s need for specialist health services, the achievement of health service targets in the regions, and optimal absorption of National Health Insurance funds so as to increase regional income.
Conclusion
The retention of specialist doctors participating in the PGDS increases when the context of regional commitments is fulfilled. Some important regional commitments are the provision of appropriate and reliable incentives, the fulfillment of infrastructure for program participants, the fulfillment of hospital facilities, and the opportunity to develop a career. Factors that will be able to attract specialist doctors to become PGDS participants are fulfillment of individual considerations, such as geographic, demographic, and socioeconomic factors.
From the results of research and discussion, the study authors suggest:
- local government should fulfill its commitment to making specialist doctors feel at home working in their assigned area until the assignment period is completed or to extend the assignment period by other mechanisms
- Central Government needs to monitor and evaluate the implementation of the PGDS regularly, including monitoring and evaluating the realization of regional commitments
- cross-ministerial policies (Ministry of Health, Ministry of Home Affairs, Ministry of Finance, Ministry of Education and Culture) are needed to optimize the PGDS.
Funding statement
The Head of the Health Research and Development Agency of the Ministry of Health of the Republic of Indonesia provided funds for implementing the Evaluation Research on the Specialist Doctors Utilization in Indonesia in 2021.
Acknowledgements
The author thanks the Head of the Center for Research and Development of Health Resources and Services, the Indonesian Ministry of Health Research and Development Agency, who has provided support in the publication of the results of this research.
References
You might also be interested in:
2020 - COVID-19 leads to physically severe experiences for the rural elderly in Japan, during Obon



