Introduction
In Australia, the geographical maldistribution of the medical workforce has prompted the creation of more opportunities for medical students to train rurally, with evidence consistently demonstrating its association with being more likely to practise in rural and underserved areas after qualification1-3. This includes placements in smaller rural communities being associated with future practice in similar rural settings4-6. With increased opportunities for medical students to complete some or all of their training rurally, a significant volume of research has been generated that seeks to explore whether rural- and metropolitan-trained medical students are equally competent upon graduation. It is now well recognised that medical students who train rurally receive an educational experience the same or of higher quality than their metropolitan peers, as demonstrated by program evaluations7, examinations8,9, and clinical performance10. Rural medical education, particularly during clinical years, provides students with more hands-on exposure to patients11,12, one-on-one access to preceptors11, and greater continuity of patient care13 than what they would normally encounter during metropolitan clinical training.
Delivering high-quality medical education in rural areas is of critical importance for producing skilled graduates who may be more inclined to later practise rurally. However, less attention in the literature has been given to understanding how rural clinical training may additionally impact wider groups of stakeholders such as patients, host organisations and rural communities where students undertake their training, despite engagement from these stakeholders being equally important to the success of rural training opportunities. Although this has not been widely investigated, preliminary research has reported that rural clinical training is an equally valuable experience for supervisors/preceptors14 and is well received by patients15. As such, there is scope to better explore the positive impact that medical students can have on rural practices (systems) and rural communities (health outcomes/management) while training in these areas.
To address this evidence deficiency, we present a study describing how a series of consecutive student placements in a single practice of a small rural community have driven a series of clinical audits and interventions that continuously fed into the next placement, resulting in improved management of chronic disease. This evidence is important in demonstrating the impact that rural clinical training can have on health care, while maintaining a high-quality student experience, and for identifying the program elements contributing to its success so that similar strategies can be more widely adopted.
Methods
Data for this case study were obtained from student reports relating to a rural medicine rotation at a single Australian medical school. As part of the medical program, all domestic students in their first clinical training year, irrespective of whether they are completing rural or metropolitan clinical training, are required to complete a 6-week placement in a smaller rural or remote area that is centred around ‘rural generalist’ practice models (henceforth termed rural and remote medicine (RRM)16). As a requirement of the RRM rotation, students develop and complete a research project during the placement, in consultation with staff at the hosting medical centre. The outcomes of each project are then evaluated by the student in the form of a written research report, which forms the assessable component of the unit. For the present study, finalised student reports were provided to the research team by the practice principal at the medical centre (placement site) with no contact between the students and research team.
With the RRM rotation limited to only 6 weeks across six blocks each year, student projects are generally restricted to simple quality improvement (QI) activities such as descriptive studies, chart audits, simple surveys and other mini-interventions. Most commonly, each student chooses and designs their project with minimal awareness of projects in previous blocks at that location. Within this case study we report on the QI activities undertaken at a single rural medical centre over a 15-month period. During this time, the medical centre hosted eight students from the medical school who completed a project relating to management of the same chronic disease. As a result, this medical centre was chosen as the focus of the report as it allows us to demonstrate how the aggregate of these projects made a meaningful impact on chronic disease management locally, despite the brevity of each individual placement and associated QI activities.
Based on guidance from the medical centre, eight interrelated student projects investigated chronic kidney disease (CKD). CKD was chosen given the higher disease burden in rural compared to metropolitan areas17. In addition, people with CKD in rural areas are more likely to delay treatment due to the distance and associated expenses to travel to metropolitan centres to access care that cannot be provided locally (eg dialysis, nephrologist)18,19. CKD was identified as a priority because it is typically more difficult to detect than other chronic diseases. In this regard, CKD patients may be asymptomatic until around 90% of kidney function is lost19, meaning that the disease has often progressed before patients seek medical attention. Taken together, the difficulties in detecting and treating CKD in a rural context generate a heavy reliance on general-practice-led models for early detection and prevention, managing disease progression in its early stages, and co-managing patients more advanced in their disease progression19. As such, improved detection, treatment and management of CKD at the primary care level was a high priority for the medical centre.
Summary of the projects
Each CKD project was developed in a similar manner, whereby students consulted with the supervising clinician and other staff at the medical centre (doctors (n=4), nurses (n=3) and administrators (n=1)) to identify a gap in clinical knowledge, patient awareness or clinical practice. Students then worked with staff at the medical centre to develop the project proposal, implement the QI activity and evaluate the outcomes. For each project, the proposal was refined as necessary and approved by the supervising clinician before any further work was undertaken. A critical component of this consultation and project refinement was medical centre staff briefing the students on past research projects on the same topic, including outcomes and limitations. As such, each student was somewhat aware of the finer details of projects preceding them, with guidance from the medical centre staff supporting each project’s refinement. Each of the projects is briefly summarised in Table 1, detailing the gaps leading to development of the project, intervention/evaluations completed and the associated outcomes.
Table 1: Summary of student chronic kidney disease projects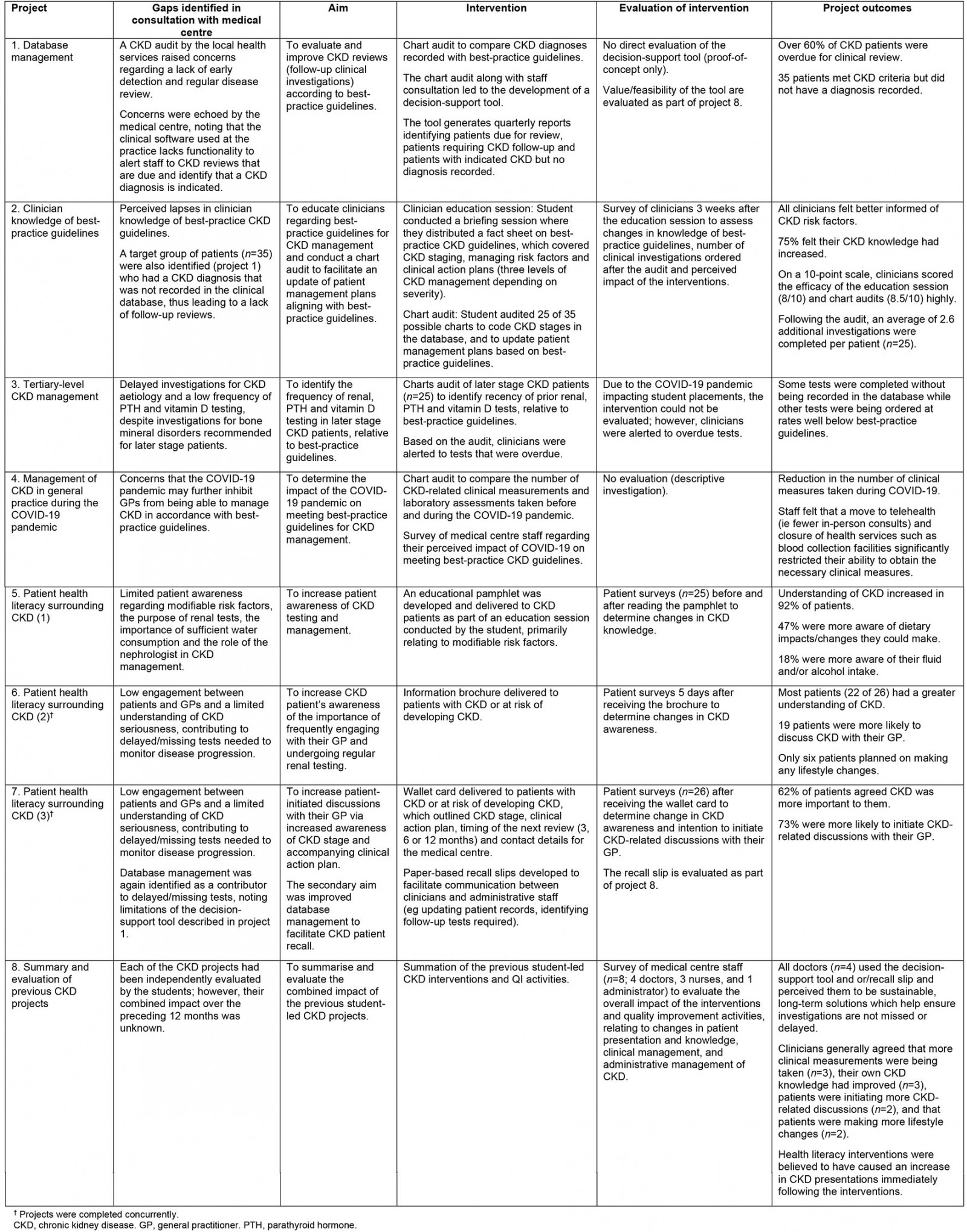
Ethics approval
Each of the student projects was undertaken without ethics approval as they were completed as part of each student’s medical training. Retrospective ethics approval to use the student project reports for this research was granted by the University of Queensland Human Research Ethics Committee (project number 2021/HE001085).
Results
Summary of project outcomes
As shown in the summaries in Table 1, each project was guided by a gap in knowledge or patient care identified by the medical centre and took into account other student CKD projects completed prior or simultaneously. Of the eight CKD projects, two focused on database management. The first database management project comprised a clinical audit and development of a decision-support tool. With the audit revealing overdue clinical investigations and a lack of CKD diagnoses recorded, the tool served as a way of detecting missing/overdue tests and diagnoses to allow patient management plans to be updated, given that this functionality was not embedded within the clinical management software at the medical centre. While this was effective, it was noted that data were not always entered into the clinical management software consistently and therefore were not being captured in the reports generated via the decision-support tool. As such, the paper recall slip was developed as a complementary measure, which helped clinicians to communicate CKD-related actions taken during the visit and to identify updates that needed to be made to patient data or tests that needed to be ordered.
Three projects investigated clinician knowledge and implementation of best-practice guidelines for CKD management. With strategies in place to better support clinicians from an administrative perspective, it was deemed important to ensure clinicians were properly informed of best-practice guidelines for CKD management. By reminders to clinicians of the importance of various CKD-related investigations this knowledge was able to be applied more effectively, with support from the database management tools. These projects focused on staging and clinical action plans, tertiary CKD management and testing, and effects of the COVID-19 pandemic on CKD management. Within each project, a chart audit revealed a mismatch between clinical practice and best-practice guidelines. Although only one of these projects included an intervention/evaluation, it was found that, by re-educating clinicians on best practice, they became more aware of CKD management, leading to a tangible increase in the number of investigations ordered per patient.
Three projects involved educating patients on various aspects of their CKD management. Although the first four projects addressed CKD management in terms of clinician knowledge and practices within the medical centre, CKD patients themselves are often unaware of their condition and its seriousness. As such, to comprehensively improve CKD management within the medical centre, it was important to address patient awareness to ensure they remained actively involved in managing their condition. These projects targeted increased knowledge of the importance of frequent renal testing, stages of CKD progression and accompanying clinical action plans, and modifiable risk factors. Immediately following the interventions, positive effects were evident for CKD awareness and patients intending to initiate more CKD-related discussions with their GP.
Following the first seven projects targeting various aspects of CKD management, the final project served as an overall evaluation to determine perceptions of medical centre staff on the aggregate impact of the preceding projects. The final evaluation confirmed data in the student reports that the projects had a meaningful impact on CKD management at the medical centre and within the rural community through its patients. Moreover, this impact was strengthened via consecutive projects completed on the same topic. By addressing the problem from varied perspectives, change occurred in relation to staff awareness, patient awareness and clinical practices at the medical centre.
Discussion
This case study describes a novel model of medical education whereby students completed simple research projects across a 6-week rural medicine rotation, with multiple projects completed in the same practice and mostly one at a time, relating to the same chronic condition. The project outcomes demonstrate that all were able to generate new knowledge, awareness or practices within patients and staff of the medical centre, which as an aggregate created a meaningful impact on CKD management in a rural primary care setting. All medical and administrative staff at the medical centre agreed that, in some form, the student placements were valuable to the practice. Therefore, our study demonstrates that, if designed effectively, medical student placements in a rural area can positively impact both the medical centre and the health care of patients.
A key component of this case study is the brevity of the placements completed by each student, meaning that the volume of work that can be completed during each project is restricted. For this reason, it is likely that the projects in isolation may have had minimal impact on patient care or practices/processes within the medical centre. However, by encouraging students to complete related projects across consecutive placements and address a complex problem from different perspectives, the outcomes became more notable.
The impacts of the projects as an aggregate are further strengthened by continuous consultation and feedback from the medical centre as each placement began. Commencing students met with staff at the medical centre to discuss potential projects that may have been appropriate to complete during the placement. Considerations discussed when choosing a project related to the needs of the medical centre, interests of the student, feasibility and resourcing. In this instance, students were also briefed on other student CKD projects completed or in progress so that they could understand the nature of the problem and work with the medical centre to consider how the problem had already been addressed and what gaps remained. These discussions can be particularly beneficial to the students by helping them to understand the context that leads to difficulties in treating patients in a rural setting. These discussions are also important in ensuring that projects address the needs of the medical centre, rather than simply meeting the minimum placement requirements for the student.
Although it has been demonstrated that the projects have strong value for the medical centre, only short-term impacts have been assessed. Therefore, in further understanding the benefits of these projects, it would be useful to revisit the various interventions at later time-points to evaluate longer term impacts. When medical centre staff were asked to reflect on the impact of the projects, it was perceived that patient awareness (relating to three of the eight projects) appeared to dissipate after the interventions, making it particularly relevant to evaluate the long-term outcomes of the health literacy interventions and consider strategies for increasing their long-term impact. For example, health literacy interventions all involved providing patients with simple educational material, with patient education shown to be a key strategy in improving CKD outcomes20. One strategy to improve patients’ health literacy longer term could be to administer this educational material at regular intervals, serving as consistent reminders to patients. Information contained in the educational material came from established guidelines (Kidney Health Australia recommendations), which are freely available and easily accessed online. Therefore, confirming the currency/relevance of the information and regularly redistributing the material could be an ongoing strategy that could be implemented without medical students present. The outcomes of other interventions such as the decision-support tool and paper recall slip are more likely to have longstanding impacts given they have already been embedded within clinical practice at the medical centre. This assumption is further supported by survey data of medical centre staff (project 8 in Table 1) showing they all agreed that the database management strategies were viable, long-term solutions and is evident in the routine use of these tools at the medical centre more than 12 months after the student placements. Nevertheless, each intervention deals with CKD management from a different perspective and thus all are valuable to the aggregate effect.
Although this case study sought to demonstrate the impact of rural clinical placements through a single healthcare-related outcome, the value of these placements from a student perspective cannot be underestimated. Research experience during medical training leads to improved academic performance21, helps to guide specialty selection21 and improves critical thinking skills22 Additionally, research is widely considered a core skill that all medical graduates should possess23. By having students contribute to projects of a more longitudinal nature, their research skills are likely to become better developed as a result. In doing so, students also gain a better understanding of the context of rural medicine and become more familiar with the logistical and practical restrictions that clinicians and administrative staff face in meeting best-practice recommendations in rural and remote areas. Furthermore, prior research experience is generally favoured when junior doctors in Australia apply to specialty training programs and, as such, placements such as those described contribute significantly to the professional development of the students. Nonetheless, it may be useful to further explore the value of this placement model from a student perspective to better understand the overall benefits and consider how similar programs might be developed and implemented more broadly.
Conclusion
This case study has demonstrated that short-term rural clinical placements for medical students have the potential to greatly improve clinical practice in rural and remote communities. By having consecutive students contribute longitudinally to improved management of the same chronic condition, they were able to address the problem from different perspectives, leading to improved administrative processes, clinical practices, and patient awareness and accountability. As a result, other medical education programs might consider adopting a similar approach.




