Introduction
Technology in medicine has developed very rapidly, but traditional medicine continues to be practiced and sought. The contradiction between the development of modern medical technology and the existence of traditional medicine is not only happening locally in certain regions/countries but has become an international concern. Many countries have recognized the use of traditional and complementary medicine for health and disease prevention, and some have national policies1-3. In several countries, such as China, India, Malaysia, Korea and Japan, an integration model with conventional medicine has been established4-8. WHO has published guidelines for developing excellent and safe traditional medicine9,10.
In Indonesia, traditional medicine is well known and practiced from generation to generation. The Indonesian Basic Health Survey results in 2013 and 2018 indicated an increase in THS use at the household level from 30.1% to 31.4%11,12. The Regulation of the Minister of Health of the Republic of Indonesia in 2018, number 15, stated that THS includes treatment and care that is carried out based on experience and skills passed from generation to generation, has been trusted over a long period of time and follows established principles13. According to the regulation, THS includes (1) certain ingredients, both packaged and homemade, using substances derived from plants, animals or minerals, and preparation of extracts (galenic) or a mixture of ingredients; (2) a manual treatment technique based on manipulation and movement of one or several body parts, such as massage, reflexology and acupressure; (3) a treatment technique that aims to utilize the mind’s ability to improve body functions, such as hypnotherapy; and (4) a treatment technique using energy fields from both outside and within the body itself, such as internal energy and prana13.
Although still minimal, the THS has been integrated into hospital services. This exists in several hospitals on Java Island. The users of these services have a wide age range (20–50 years) and reside not far from the hospitals. Despite being disappointed that THS is not covered by the National Health Insurance, users continue to access this service14.
Culture and history in the community, affordability, and regulations regarding traditional medicine practitioners affect the level of public trust and sustainability of support for implementing various conventional healthcare programs. Government support for implementing traditional health services through regulations also affects the success of implementation15,16.
In theory, there are several variables related to THS utilization. Among them are gender, marital status, and medical expenses17-21. Other related factors reported in previous studies related to THS utilization are socioeconomic or wealth status22-24, age and education level19-21,25,26, occupation type20,27, and religion28-30.
THS utilization is mainly on Java Island, which has many urban areas with better facilities and infrastructure than eastern Indonesia. In North Maluku, West Papua, Central Sulawesi, South Sulawesi, Nusa Tenggara Timur, and Papua, the community performs traditional medicine independently, without the help of traditional healers and traditional health workers or therapists. This may have an impact on limited modern health facilities31-33.
Currently, there is a gap – in some cases extreme – between health service utilization in urban and rural areas in Indonesia, and rural areas often lag behind urban areas. In urban areas, people tend to have better access because there are private health service providers that participate34,35. The presence of THS is expected by the government to fill the lack of modern health facilities available in rural areas.
The proportion of people with low socioeconomic status (SES) in urban and rural areas is also unequal. In 2020 there was an increase in the percentage of those with low SES in urban and rural areas; in March 2020, the low SES population in urban areas was 7.4%, while in rural areas it was 12.8%. This figure increased in September 2020: to 7.9% and 13.2% in urban and rural areas, respectively36. The present study aims to analyze the relationship of SES with THS utilization in rural Indonesia by looking at the increase in these percentages.
Methods
Data source
The study employed secondary data from the 2018 Indonesian Basic Health Survey. The Ministry of Health of the Republic of Indonesia surveyed a national cross-sectional survey. Interviews using Household Instruments and Individual Instruments were used to compile data from May to July 2018.
The 2018 Indonesian Basic Health Survey population consists of all Indonesian households. The survey's sample frame is based on the 2018 National Socio-Economic Survey, which was conducted in March 2018. In addition, the 2018 Socio-Economic Survey visited a target sample of 300 000 residences from 30 000 census blocks (run by the Central Statistics Agency)37.
The survey was conducted using the probability proportional to size (PPS) approach, which involves two stages of systematic linear sampling. Stage 1 is implicit stratification based on all census blocks' welfare strata as determined by the 2010 Population Census. PPS chose the sample survey as the sampling frame for picking census blocks from a master frame of 720 000 census blocks from the 2010 Population Census, of which 180 000 (25%) were selected. The survey employed the PPS method to determine multiple census blocks in each urban/rural strata per regency/city to build a Census Block Sample List. A total of 30 000 census blocks were chosen. In stage 2 the survey selected 10 households in each census block with the highest implicit stratification of education completed by the head of household using systematic sampling to preserve the representation of the diversity value of household characteristics. As part of the 2018 Indonesian Basic Health Survey, all selected household members were questioned37.
Participants
The analysis unit of the study was Indonesians aged 15 years and over. The inclusion criteria were those aged 15 years and over and those who lived in rural areas of Indonesia. The exclusion criteria excluded those with mental disorders, who could not answer questions clearly, or who were unwilling to participate. The study defined 357 556 participants as a weighted sample based on the sampling approach.
Outcome variable
Adults' usage of THS in the previous year, whether visiting a traditional care facility/healthcare facility or bringing in traditional healers or traditional health workers, was employed as the outcome variable in the study37.
Exposure variable
The 2018 Indonesian Basic Health Survey graded households based on the number and type of consumer goods they own, for example a television, a bicycle or an automobile, as well as dwelling characteristics such as availability of drinking water, bathroom facilities, and type of flooring materials. The survey used principal component analysis to calculate these scores. The survey calculated national wealth quintiles by assigning a score to each usual (‘de jure’) household member, ranking each person in the household population based on their score, and then dividing the distribution into five equal categories, each containing 20% of the population38,39. The SES categories were ‘lowest’, ‘lower’, ‘middle’, ‘higher’ and ‘highest’.
Control variables
Control variables for the study comprised five participant characteristics: age, gender, marital status, education level, and occupation type.
The study computed a respondent's age using their most recent birthday. Two age groups were used, based on productivity: 15–64 years and 65 years and over. Gender comprised two categories in the survey: male and female. The study also separated respondents into three marital status categories: never married, married/living with a partner, and divorced/widowed.
The study defined a respondent's education by acknowledging their most recent diploma. The research looked at three levels of education: primary education or less, secondary education, and higher education. The five occupation categories were unemployed, civil servant/army/police, private sector, entrepreneur, and farmer/fisherman/labor/others.
Setting
The authors conducted the study in a rural area setting in Indonesia. Rural area classification refers to the Indonesian Central Statistics Agency, and the study setting represents the national level.
Data analysis
The authors first created a bivariate comparison using the χ2 test. A collinearity test was also employed to ensure no strong link existed between the independent variables in the final regression model. The author used a binary logistic regression at the end of the study to look at the multivariate relationship between all independent factors and THS. Throughout the statistical analysis portion of the project, the authors used the Statistical Package for the Social Sciences v26 (IBM; https://www.spss.com).
Ethics approval
The 2018 Indonesian Basic Health Survey obtained ethics approval from the National Ethics Committee of the National Institute of Health Research and Development (LB.02.01/2/KE.024/2018). The survey deleted all respondents' identities from the dataset. The survey obtained written informed consent from all the participants and guardians during the survey. The author received permission to use data for this study from http://www.litbang.kemkes.go.id/layanan-permintaan-data-riset. The authors conducted all methods following relevant guidelines and regulations.
Results
The analysis found that the THS utilization average in rural Indonesia in 2018 was 33.6%. A complete distribution of THS utilization based on participant characteristics can be seen in Table 1. Based on THS utilization, the second-highest SES group had the highest proportion of THS use compared to all SES groups. Those in the 15–64 years age group were more numerous across all SES levels based on age group except for the lower and lowest SES groups, for which the 65 years and over age group had the highest numbers of respondents. Based on gender, women and men in the lowest SES group constituted a slightly higher proportion of respondents than do other SES groups.
According to marital status, people in the lowest SES level were most numerous in all marital classes compared to other SES groups. Those in the lowest SES level were most numerous compared to other SES levels in the ‘primary education and under’ category, and those in the highest SES level were most numerous, compared to other SES levels, in the higher education group. Based on occupation, and compared to other SES levels, those in the lowest SES level were most numerous in the ‘unemployed’ and ‘farmers/fishermen/laborers/others’ categories; the highest SES group was most numerous in the ‘civil servant/army/police’ group.
The collinearity test suggests that the independent variables have no meaningful association. Furthermore, the tolerance value for all variables is more significant than 0.10, and the variance inflation factor value for all factors is less than 10.00. According to the study, the regression model exhibited no signs of multicollinearity, implying that the test's decision-making base is solid.
Table 2 displays the binary logistic regression of THS utilization in rural Indonesia in 2018. Those at the lower SES level are 1.111 times more likely to utilize THS based on SES than those at the lowest SES level (adjusted odds ratio (AOR) 1.111; 95% confidence interval (CI) 1.085–1.137). The middle SES group is 1.113 times more likely than the lowest SES group to utilize THS (AOR 1.113; 95%CI 1.086–1.140). Meanwhile, those in the higher SES group are 1.166 times more likely than those at the lowest SES level to use THS in rural Indonesia (AOR 1.166; 95%CI 1.139–1.194). The highest SES group is 1.166 times more likely than the lowest to use THS in rural Indonesia (AOR 1.166; 95%CI 1.134–1.200). The result indicates all SES groups are more likely, compared to the lowest SES group, to utilize the THS in rural Indonesia.
The study found four control variables related to THS utilization: age group, marital status, education level, and occupation type. Based on age group, those aged 65 years and over are 1.054 times more likely than those aged 15–64 years to utilize THS (AOR 1.054; 95%CI 1.023–1.086). Being married or living with a partner is 1.695 times more likely than never having been in a union to use the THS (AOR 1.695; 95%CI 1.657–1.735). Those who are divorced or widowed are 1.746 times more likely to utilize the THS than those who have never been in a union (AOR 1.746; 95%CI 1.683–1.811). Regarding education level, those with secondary education are 1.030 times more likely than those with primary education or less to use the THS (AOR 1.030; 95%CI 1.009–1.053). Those with higher education are 0.938 times less likely than those with primary education or less to use the THS (AOR 0.938; 95% CI 0.896–0.981). Moreover, someone with an occupation is more likely than someone who is unemployed to utilize the THS in rural Indonesia.
Table 1: Descriptive statistics of participants' characteristics by socioeconomic status (n=357 556)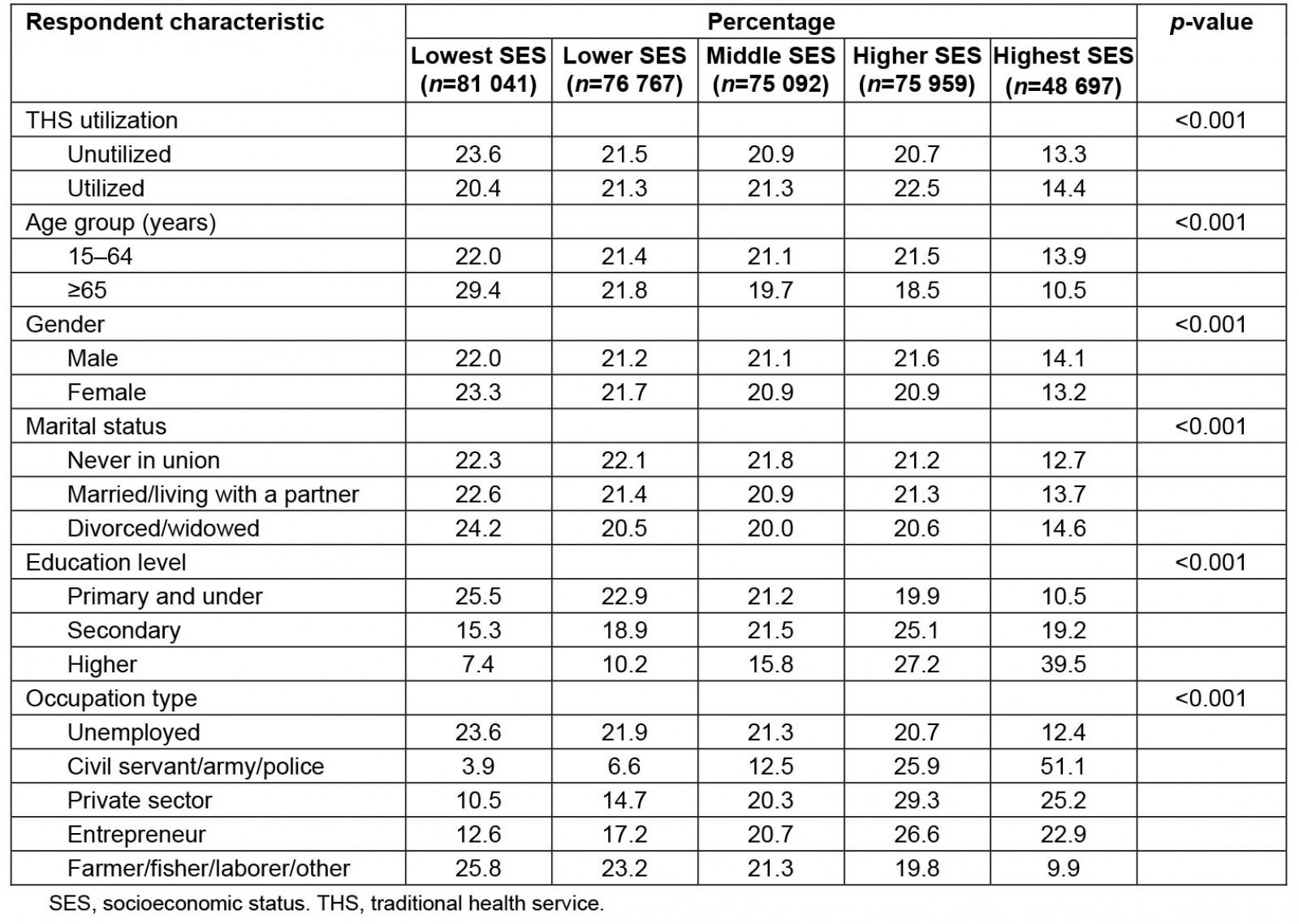
Table 2: Results of binary logistic regression of traditional health services in rural Indonesia, 2018 (n=357 556)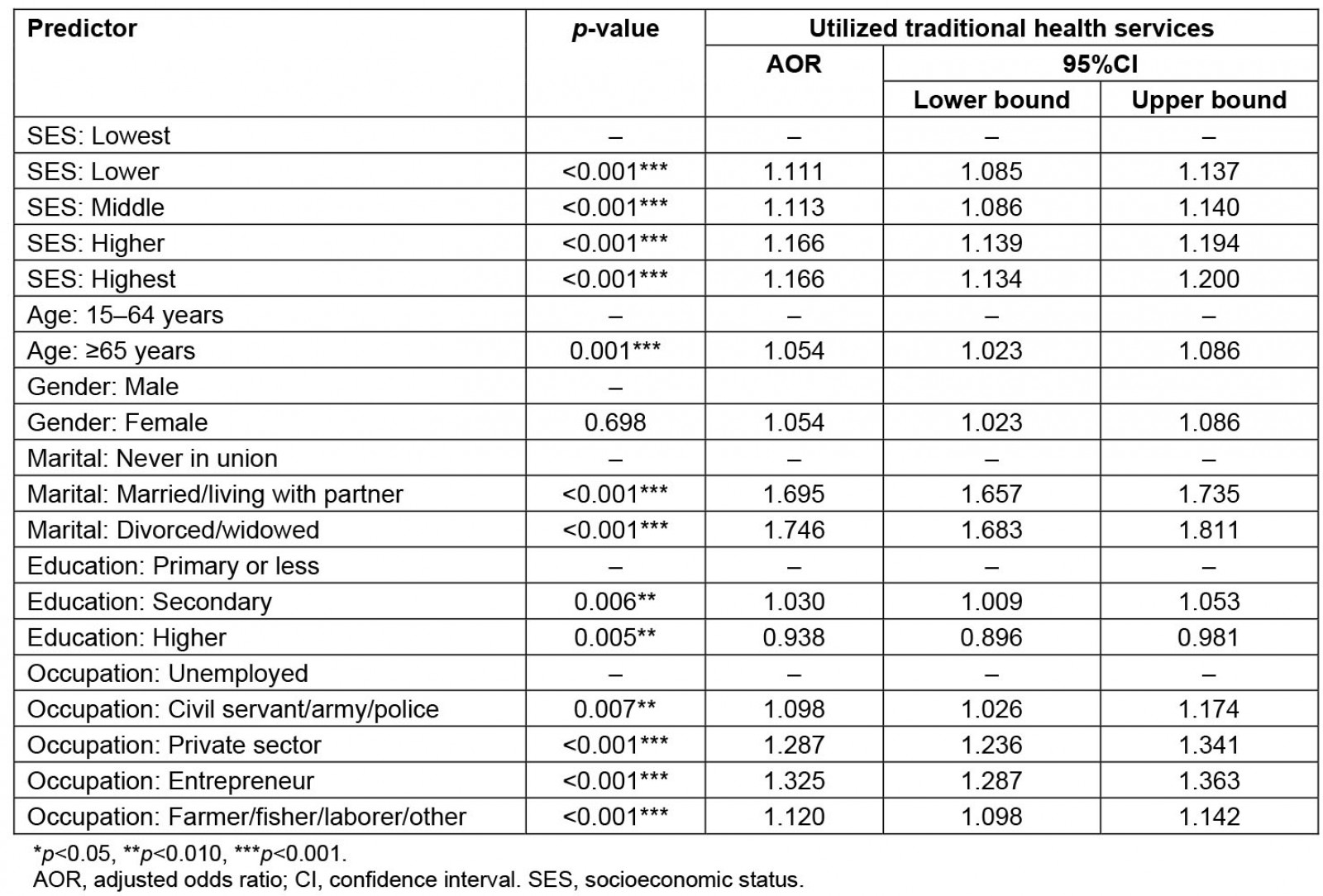
Discussion
The study results show that all SES levels are more likely, compared to the lowest SES level, to utilize the THS in rural Indonesia. This situation relates to the availability of costs to those with low SES, who must prioritise their money elsewhere. However, THS is considered cheap, easy, and effective in reducing healthcare costs, especially for those who are poor27,40. The ability to buy services is a factor that has a significant relationship with the behaviour of choosing traditional medicine41. Previous research has stated that the affordable price of therapy is one of the considerations and reasons for patients choosing traditional treatment. There are also economic factors related to alternative medicine42. A study shows that income per capita affects the tendency to visit traditional and modern healthcare facilities. Individuals are more likely to pay for health services if the per-capita expenditure is high43.
The present study found that those aged 65 years and over are more likely than those aged 15–64 years to utilize THS in rural Indonesia. The study shows that older people are more likely to choose traditional medicine than younger people41,43. A previous study reported that the probability of selecting traditional medicine for young people is 74.5%, while for older people it is 91.31%. The researcher explained that the situation might be related to complaints of pain being more common in the older age group, with complaints that are not well known treated with modern medicine41. This opinion is consistent with a study on households in rural areas, where households mostly carry out traditional care with the head of the family for more than one generation44. Older people may prefer traditional medicine because it's easy or practical. In addition, conventional medicine is more in demand by older people because of the belief that chemicals obtained from medical treatment can harm health, considering that antibodies or the body's ability to withstand external attacks decline in elderly individuals. In addition, traditional medicine is inherited from ancestors, has been carried out for a long time and becomes a habit43.
The study results indicates that marital status is related to THS utilization in rural areas in Indonesia. The results are aligned with previous research45. However, this result differs somewhat from a previous study, which stated that marital status did not have a significant relationship with the use of traditional medicine41.
Based on education level, the present study has a relationship with THS utilization in rural areas in Indonesia. Someone with secondary education has a slightly higher probability of using THS than those in other education categories. Conversely, someone with higher education is less likely to use THS than someone with primary education. Education is a collection of experiences to understand something that is not understood before. In general, people with a higher level of education are more likely to use health services. This is because the higher a person’s level of education, the better they receive and understand new information, especially health information, and increasing changes in attitudes and behavior46,47.
Of the families who had literacy education as adults, 75% did not use health facilities44. However, a previous study found no relationship of education to an individual's probability of choosing traditional medicine43. This result is similar to that of previous research, which states that education does not have a significant relationship with the use of conventional medicine41.
Furthermore, the study result shows that occupation type is related to THS utilization in Indonesia's rural areas. Civil servants, army personnel, and police officers have health insurance, and they can choose health treatment at modern facilities that accept insurance. Also, National Health Insurance does not cover THS. Farmers and fishers earn little money and cannot afford to take time away from work or spend much money, including for health treatment27. Therefore, traditional medicine is an option because it could minimize the cost of healthcare access27,40.
Traditional medicine services are necessary for Indonesians with various SES levels and knowledge. Hence, traditional medicine needs to be more recognized by the government, and its position needs to be aligned with modern medicine in the national health insurance system. It is essential to promote in-depth cultural research to prevent marginalization and stigma around traditional medicine. Providing there are community benefits, supervision and development of traditional medicine need to be carried out. Because of their long history in the community, among other reasons, complementary and alternative therapies should continue to be used.
Strengths and limitations
This study analyzed a large number of data to represent information in rural areas. However, the study looked at secondary data; therefore, the factors examined were limited. Other factors that have been linked to THS utilization in previous studies, such as trip duration, travel costs to facilities, religion, concepts of illness, and types of medical condition, could not be analyzed here30,48,49.
Conclusion
The study concluded that SES status relates to THS utilization in rural Indonesia, and all SES levels are more likely than the lowest level to utilize THS in rural Indonesia. The results indicate that although THS is widely acceptable, those at the lowest SES level are the group who rarely access THS.
Acknowledgements
The authors would like to thank the National Institute of Health Research and Development, which agreed to analyze this article's 2018 Indonesian Basic Health Survey data.
References
You might also be interested in:
2020 - Organophosphate exposure and the chronic effects on farmers: a narrative review



