Introduction
Background
There is a global shortage of health professionals in rural areas, impacting all fields and specialties1. The population of Australia is relatively small but widely dispersed, with rural and remote populations experiencing poorer access to health care than those in metropolitan areas2. At present Australian healthcare accessibility is dependent upon locality, with health professionals per capita higher in major cities than in rural areas3. Outer regional, remote and very remote areas have severe shortages of allied health, dental and medical specialists, with ratios of nursing and midwifery staff to population also lower in remote and very remote areas4. Although technology plays an ongoing role in healthcare distribution, recruiting and retaining health professionals in rural communities is necessary to ensure equitable provision of health services across the country.
In medicine, outreach programs are operated to bring healthcare services and information directly to communities that need them. Rural health career outreach programs operate under the same principle and offer rural students the opportunity to experience and learn about health careers without leaving their communities. Given the limited availability of health services in rural and remote areas, and the cost of travelling to larger population centres, these programs provide learning experiences that would be otherwise inaccessible to many rural and remote students. Exposing students to health career promotional activities can increase interest in health careers5,6 and potentially increase enrolments in healthcare programs7, with the aim of eventually alleviating workforce shortages and potentially enhancing population health outcomes. Rural outreach programs are therefore a vital piece of the puzzle when it comes to establishing universal health coverage to ensure people have access to the ‘health services they need, when and where they need them, without financial hardship’8. Structured contact between schools and health professionals is crucial in nurturing rural students considering health careers9, particularly while secondary school students are considering career and education options10. Outreach programs heighten students’ consideration of health careers by providing role models that counter incorrect assumptions about health professional gender, class11 and locality12. Furthermore, tertiary health students with rural backgrounds are more likely to work in rural areas9,13-15, thereby contributing to sustainable rural health workforce.
Rural health career outreach programs can highlight diverse health professions, clarify how these professions contribute to the healthcare system, make practitioners visible and highlight enrolment pathways. Programs can take place over several days, such as the 4-day Australian Health Careers in the Bush workshops16. The majority of past participants (>90%) reported that the program had a major impact on their course and career selections, with many (83%) subsequently enrolling in health-related courses, highlighting the potential of experiential career programs to drive healthcare courses enrolments17. However, the resources required to run multi-day events are significant, making single-day models more feasible for rural and remote communities.
Short career outreach programs generally occur within a single day and can include activities such as didactic sessions, informal talks, simulations, hands-on activities, recorded procedures and facility tours. Studies assessing programs with a multidisciplinary career focus are uncommon in published literature. One such program, the Canadian Healthcare Travelling Roadshow, operated in rural locations and engaged students in highly interactive sessions18. Following participation in this program, students reported an increased consideration of health careers. A systematic review of outreach programs targeting rural and under-represented secondary school students – and focusing on medical rather than health careers – found only three short programs19. Two were in Canadian contexts: one focused on medical careers only20 and the other on medical and health careers21. The third study was Australian and focused on health careers22. The Canadian studies reported a 13% increase in the number of students considering health careers20 and that 92% were more interested in health careers21 following their participation in outreach programs. The Australian study qualitatively assessed their program using past and recent participants, and stakeholders from the school education system, health services and university sector22. The authors found the program reinforced career goals, motivation and interests, and highlighted the importance of visible career pipelines in returning students to work in their communities. Furthermore, early engagement with students helped develop confidence and capacity to engage in career decision-making22.
Aspire2Health: a novel rural career outreach program
The Aspire2Health program originated in response to a request by parents of regional secondary school students in Queensland, Australia (Modified Monash Model (MMM) Category 2) for information and guidance on health careers from Rural Medical Education Australia. The program grew organically from informal discussions to facilitated sessions where regional students could meet and discuss career pathways with local clinicians. Successes with regional students led to program expansion, with many organisations contributing staff, equipment and funding. Subsequently, the program expanded into rural and remote towns (MMM 3–7).
The overarching aim of Aspire2Health is to increase the size and sustainability of the rural health workforce by growing rural students’ interest in and awareness of health careers. Aspire2Health operates on the principles of student accessibility and healthcare system equality:
- Aspire2Health events must be run in rural and remote locations to ensure they are accessible to rural and remote students.
- Aspire2Health represents the healthcare system without privileging the contributions of any profession.
These principles are combined with activities that portray a broad variety of healthcare professions and professionals, from a range of perspectives. Students watch professionals demonstrate their contributions to health care in a scripted emergency scenario, explore authentic healthcare settings during ambulance and hospital tours, engage in small-group discussions with healthcare professionals and, finally, engage in hands-on clinical skills. The involvement of local health professionals further emphasises that health careers are valued and accessible in students’ rural and remote communities. Aspire2Health is the only Australian health career outreach program for secondary school students operating in several rural and remote communities. The Aspire2Health program is ongoing and is a first step in investigating whether rural and remote secondary school students’ interest in health careers can be piqued via outreach programs, leading to increased health course enrolments, and potentially contributing to future health workforce sustainability.
Study aims
Published literature consistently finds that, following short rural health career outreach programs, students report greater interest in pursuing health careers. These articles do not, however, address our understanding of how students respond to activities within these programs. Our knowledge of how to optimise student interest is thus lacking. This is particularly important in the face of external circumstances such as pandemics and economic stresses, which can affect the resources available to operate health career outreach programs, especially those in rural locations.
Aspire2Health collected student feedback on overall program impact, interest ratings for each activity, and qualitative data describing students’ program experiences and suggestions for program improvement. Aspire2Health events operated pre-COVID (2019) and peri-COVID (2020–21), with the latter years impacted by COVID health restrictions and reduced healthcare system capacity. This generated a unique natural experiment, with pre-COVID participants experiencing no restrictions on Aspire2Health events while peri-COVID participants were exposed to ‘negative’ changes such as social distancing and mask-wearing, shortened activity times, and reduced ambulance and hospital tour availability. The aims of this study were to determine the:
- suitability of the Aspire2Health program and its elements
- short-term impact of the Aspire2Health program on students’ interest in health careers
- impact of COVID restrictions on delivery of the Aspire2Health program and its elements, and if these changes affected program experience and outcomes.
Methods
Participants
The Aspire2Health program ran in regional centres, rural towns and remote communities in the Toowoomba, Darling Downs and South-West regions of Queensland, Australia. Students in years 9 and 10 (aged 13–16 years) at selected government and non-government schools in these regions were invited to participate in Aspire2Health events. Consent to attend was provided by the parents of students who chose to attend. Feedback data for this study were collected with consent from participants during Aspire2Health events for the purpose of program review and development.
Program overview
The Aspire2Health program is 6 hours in duration and includes an observed clinical scenario, ambulance and hospital tours, discussions with health professionals, and hands-on clinical skills stations (Fig1). In 2020–21 the impact of COVID in the regions in which Aspire2Health operated was limited, with sporadic, short lockdowns and low COVID case numbers. In 2020 and 2021 COVID restrictions required Aspire2Health to adopt social distancing, mask-wearing and cleaning between group rotations, alongside external limitations such as declining ambulance and hospital tour availability (Table 1). The activities included in Aspire2Health are described in detail below.
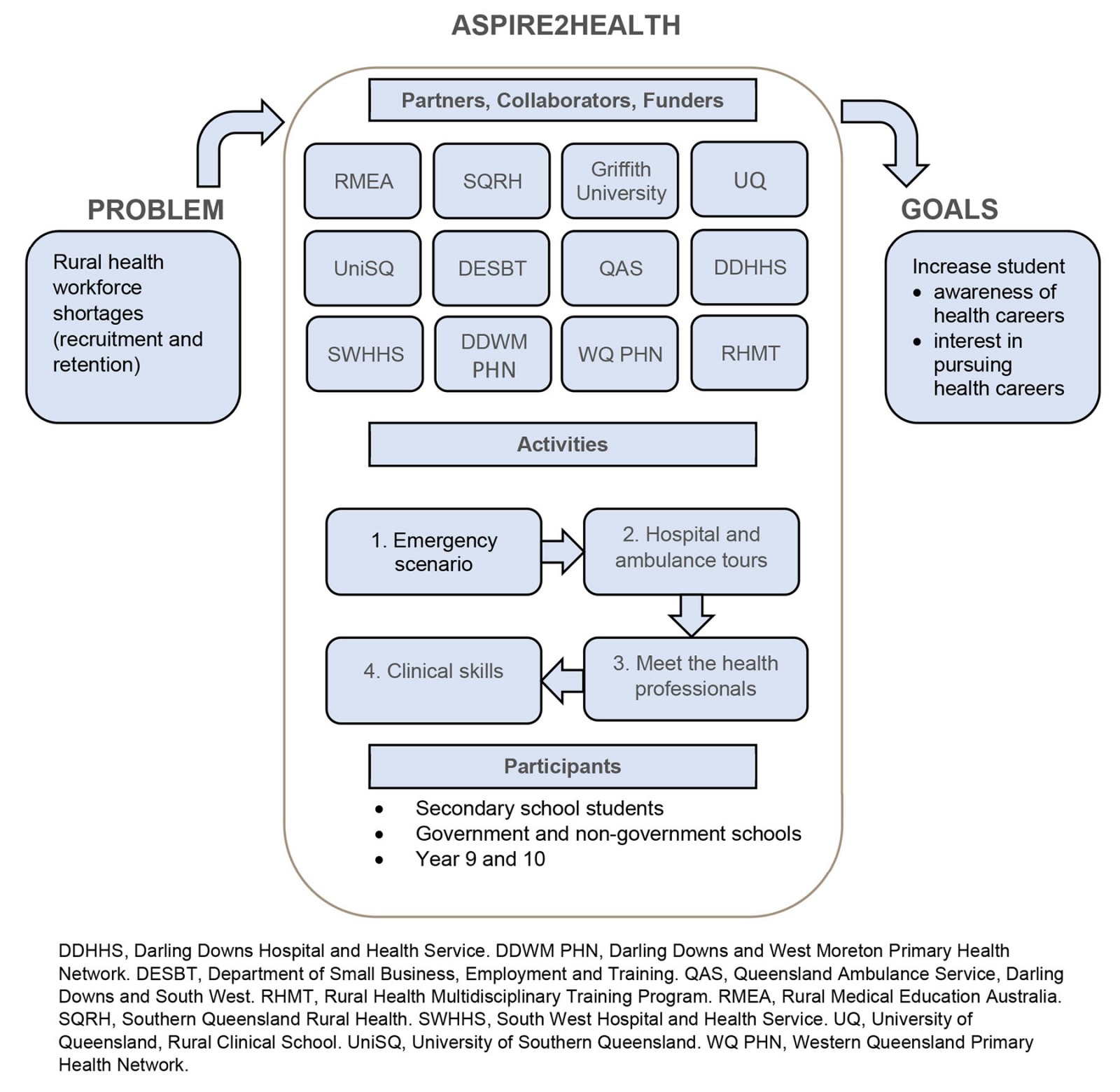 Figure 1: Conceptual diagram of components and purpose of the Aspire2Health program.
Figure 1: Conceptual diagram of components and purpose of the Aspire2Health program.
Table 1: Aspire2Health activity program and the impact of COVID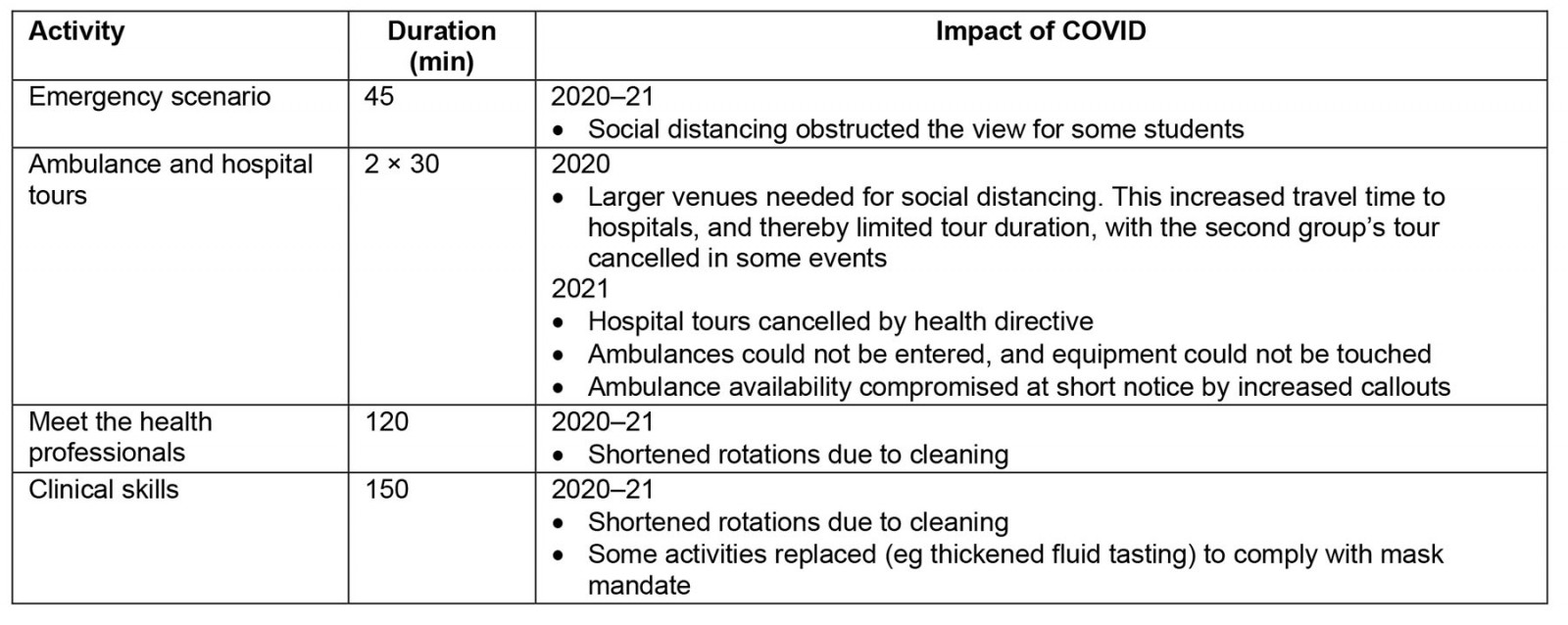
Aspire2Health Program
Emergency scenario (Aims: Display a rural context and the interprofessional nature of rural health practice): The emergency scenario opens each Aspire2Health event. The fictional scenario begins with a rural individual experiencing a quadbike or horse-riding accident in a paddock. Paramedics arrive and stabilise the patient before transferring them to hospital, where medical and nursing students (as doctors and nurses) continue treatment. The scenario culminates in spontaneous cardiac arrest and CPR. Following the scenario, facilitators emphasise that some patients begin their journey like this, and then continue their journey with allied health professionals and community-based practitioners.
Ambulance and hospital tours (Aim: Experience clinical settings, observe and/or handle specialised equipment): In two groups, students tour their local hospital and an ambulance. Hospital tours expose students to several hospital environments (primarily emergency, maternity and operating theatres), avoiding contact with patients for privacy reasons. Where possible, students are provided the opportunity to use hospital equipment and tools (eg hoists). Ambulance tours are more tactile experiences, with students entering the ambulance and activating the lights, sirens and horn. Medical equipment is shown, and their uses explained, with students permitted to handle many items. Medicines are displayed, and their uses and contraindications are explored.
Meet the health professional (Aims: Convey the experience of working in a health career, career options within professions, and diverse pathways into professions): Small groups of students rotate between health professionals (eg paramedics, nurses, physiotherapists) where typical work activities are discussed and professionals share their career motivations, professional development opportunities and career progression options for their professions. Students are prompted on their key areas and professions of interest, and professionals demonstrate how many health professions contribute to the treatment and rehabilitation of patients. For example, a neurological issue may be referred by a general practitioner; a neurosurgical procedure performed by surgeons, anaesthetists, and nurses; and recovery facilitated by physiotherapists and occupational therapists. Diverse pathways into professions are emphasised, as are school and life choices that facilitate health career pathways. Sessions close with examples of diverse pathways into tertiary healthcare courses.
Clinical skills (Aim: Utilise skill development to demonstrate that health careers are attainable):
Students rotate through stations participating in hands-on activities facilitated by nurses, paramedics, medical students and allied health professionals. Permanent stations include CPR, suturing and plastering. The fourth station provides two or three activities specific to allied health (eg physiotherapy, speech pathology), nursing and midwifery. The professions represented depend upon the availability of professionals to run the session. The stations sought to convert the interest in health careers generated during the emergency scenario, hospital and ambulance tours and ‘meet the health professionals’ activities into motivation to pursue a healthcare career. By teaching achievable skills learned in university and performed by clinicians, we aimed to reduce the perceived difficulty of tertiary study and allow students to visualise themselves as successful clinicians.
Materials and data analysis
Feedback was collected at the end of each event using a five-point Likert scale to assess overall program impact (three items), interest in each activity (five items) and open-ended feedback items regarding what was most enjoyable and what could be improved (two items; Table 2). All Likert scales were reported as ‘strongly agree’ to ‘strongly disagree’, except for the item ‘Overall, how would you rate the event?’, which was scored from 1 (‘poor’) to 5 (‘excellent’). In 2019, data were collected by printed surveys, then de-identified and transcribed into Microsoft Excel. In 2020–21, data were collected electronically using Microsoft Forms, with students accessing the survey on their personal devices using a quick-response (QR) code. Blank and irrelevant responses were excluded from analysis.
Codes were developed from the qualitative data by the lead author to ensure congruity and comprehensiveness. This data was semantically analysed to generate initial themes; minimal interpretation was necessary due to the short length of responses23. All authors individually reviewed the full qualitative dataset, with final codes and themes agreed upon by consensus. No differences in themes were observed between years, hence themes are drawn from the full data set.
Statistical analyses were performed using SPSS for Windows v28 (IBM; https://www.ibm.com/au-en/products/spss-statistics). Statistical significance for all omnibus tests was set at p<0.05, two-tailed. Planned comparisons between pre- and peri-COVID cohorts (2019 v 2020–21) on the three items measuring overall program impact and the five items measuring level of interest in activities were each determined using Mann–Whitney U-tests. Effect sizes were measuring using η2, where 0.01 to <0.06 is considered a small effect, 0.06 to <0.14 a medium effect and >0.14 a large effect. Comparisons between item responses within each year was performed using the Friedman test followed by posthoc pairwise comparisons using Wilcoxon signed-rank tests with sequential Bonferroni adjustments. Effects sizes were assessed by Kendall’s W, where 0.1 to <0.03 is considered a small effect, 0.3 to <0.5 a moderate effect and >0.5 a large effect.
Table 2: Feedback survey structure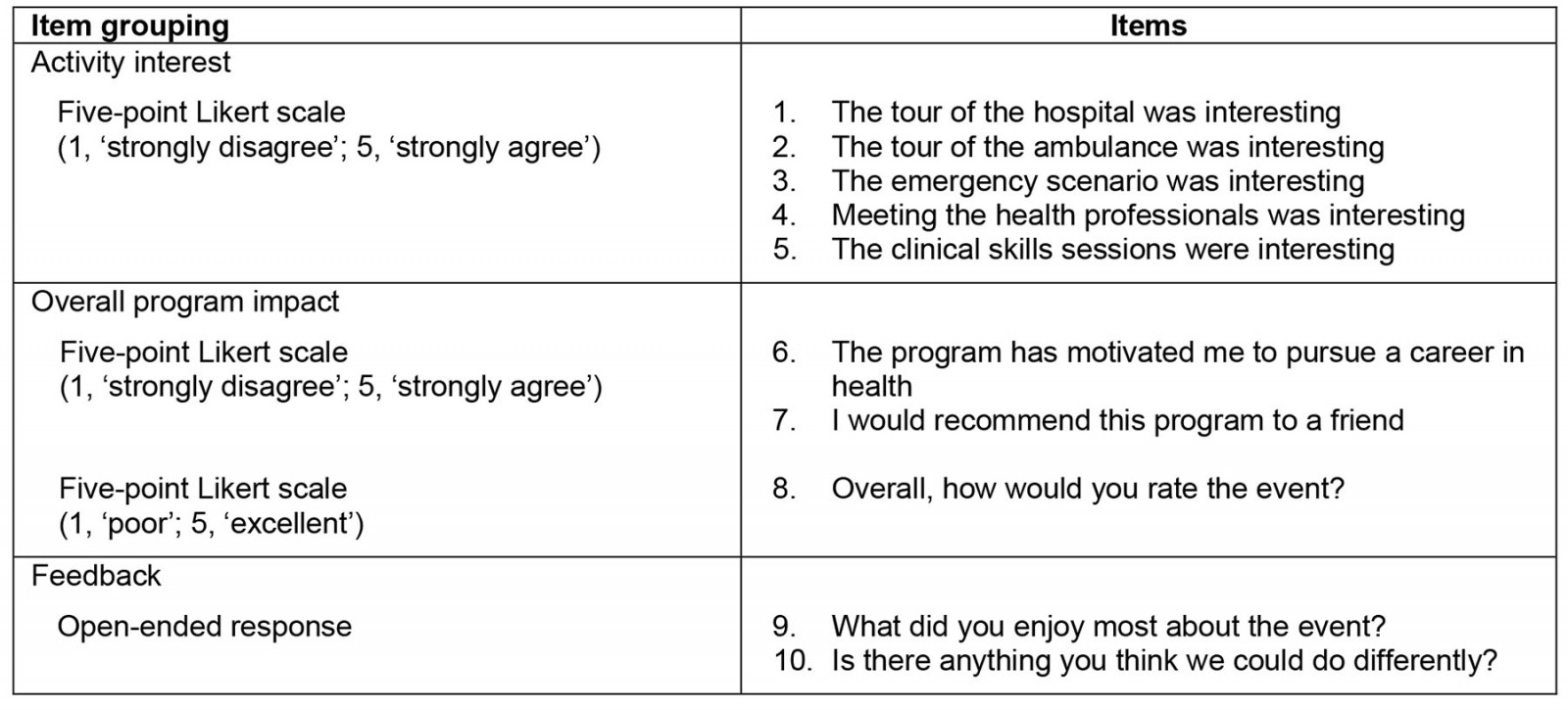
Ethics approval
An ethics exemption was granted by the Griffith University Human Research and Ethics Committee (HREC 2022/616) to utilise the data for research purposes.
Results
Data overview
A total of 495 students (162, 119 and 214 in 2019–21, respectively) participated in Aspire2Health events from rural and regional secondary schools (30, 21 and 55 in 2019–21, respectively). A substantial number of these students submitted feedback data after pre-COVID events (n=125, 77% response rate; 2019) and peri-COVID events (n=248, 74% response rate; 2020–21). Events were held in a regional centre, rural towns and a very remote community (Table 3).
Table 3: Distribution of Aspire2Health events by location rurality in 2019–202124,25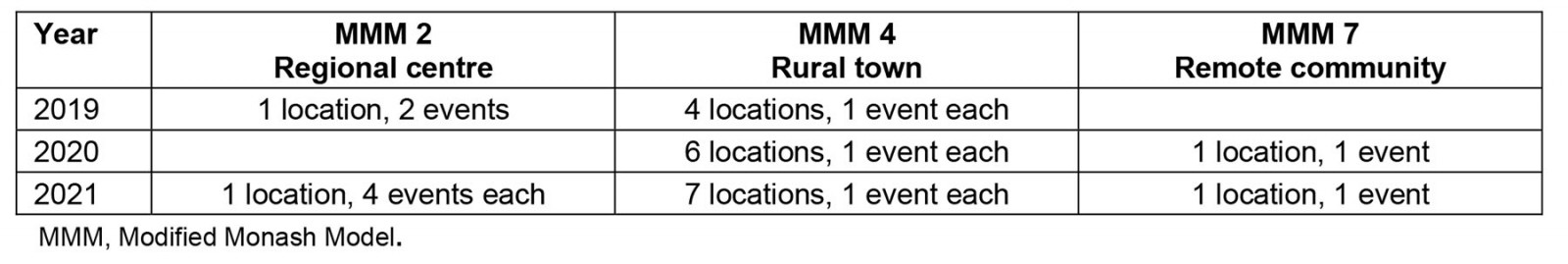
Overall program impact
Items evaluating overall program impact were rated highly (Fig2). Student responses to ‘The program has motivated me to pursue a career in health’ were similar pre- and peri-COVID (mean (M)=4.7 v M=4.5; p=0.114, η2=0.01) with 91% (pre-) and 92% (peri-) of students agreeing or strongly agreeing with this item. A similar pattern was observed with the item ‘I would recommend this program to a friend’ pre- and peri-COVID (pre-COVID M=4.8 v peri-COVID M=4.7; p=0.098, η2=0.01): 98% (pre-) and 99% (peri-) of students agreed or strongly agreed with the item. Compared to pre-COVID, overall rating of the event decreased slightly peri-COVID (M=4.8 v M=4.7; p=0.04, η2=0.01), although student satisfaction remained high, with 98% (pre-COVID) and 99% (peri-COVID) of students rating the event as 4 or 5 (‘very good’ or ‘excellent’). Overall, these results indicate that student satisfaction with Aspire2Health events peri-COVID was minimally affected by changes in program delivery, and by reduced ambulance and hospital availability.
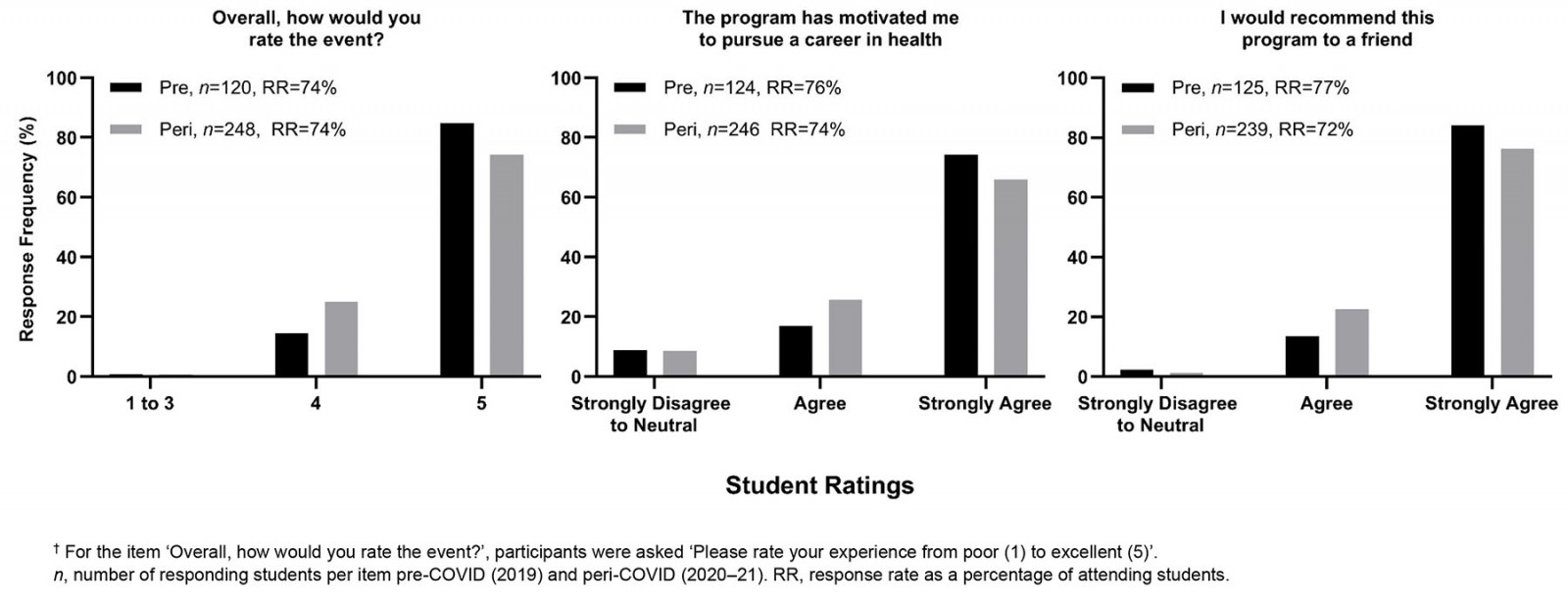 Figure 2: Distribution of responses to items evaluating overall Aspire2Health program impact.†
Figure 2: Distribution of responses to items evaluating overall Aspire2Health program impact.†
Activity interest
Two of five learning activities had an interest-rating decline by students during COVID, compared with before COVID (Table 4). Interest in hospital tours decreased from 4.4 pre-COVID to 3.8 peri-COVID (p=0.002, η2=0.083), prior to the cancellation of hospital tours in 2020. There was a statistically significant decrease in interest in clinical skills (pre-COVID 4.9 v peri-COVID 4.7; p=0.001); however, this change is unlikely to be of any practical significance to Aspire2Heath given its effect size (η2=0.034). Student interest in ambulance tours, meeting the health professionals, and the emergency scenario, remained the same pre- and peri-COVID.
The Friedman test indicated within-year differences in student interest in activities during both the pre-COVID period (χ2=47.31, p<0.001, W=0.19) and peri-COVID period (χ2=51.19, p<0.001, W=0.22). Posthoc comparisons showed that student interest in clinical skills sessions pre-COVID was rated as higher than for the other four activities. Additionally, meeting health professionals and the emergency scenario were rated as more interesting than the ambulance and hospital tours. Peri-COVID hospital tour interest data includes participants from 2020 only (as tours were cancelled in 2021), although it is clear from the 2020 data that hospital visits were regarded as less interesting than other components. Posthoc comparisons of peri-COVID data identified clinical skills sessions and meeting the health professionals as the most interesting learning activities, compared with the emergency scenarios and ambulance tours. Additionally, the emergency scenario was regarded as more interesting than the ambulance and hospital tours. On the whole, these results point to the activities related to clinical skills, meeting the health professionals and the emergency scenario being consistently more interesting to students than both ambulance and hospital tours.
Table 4: Student interest in learning activities†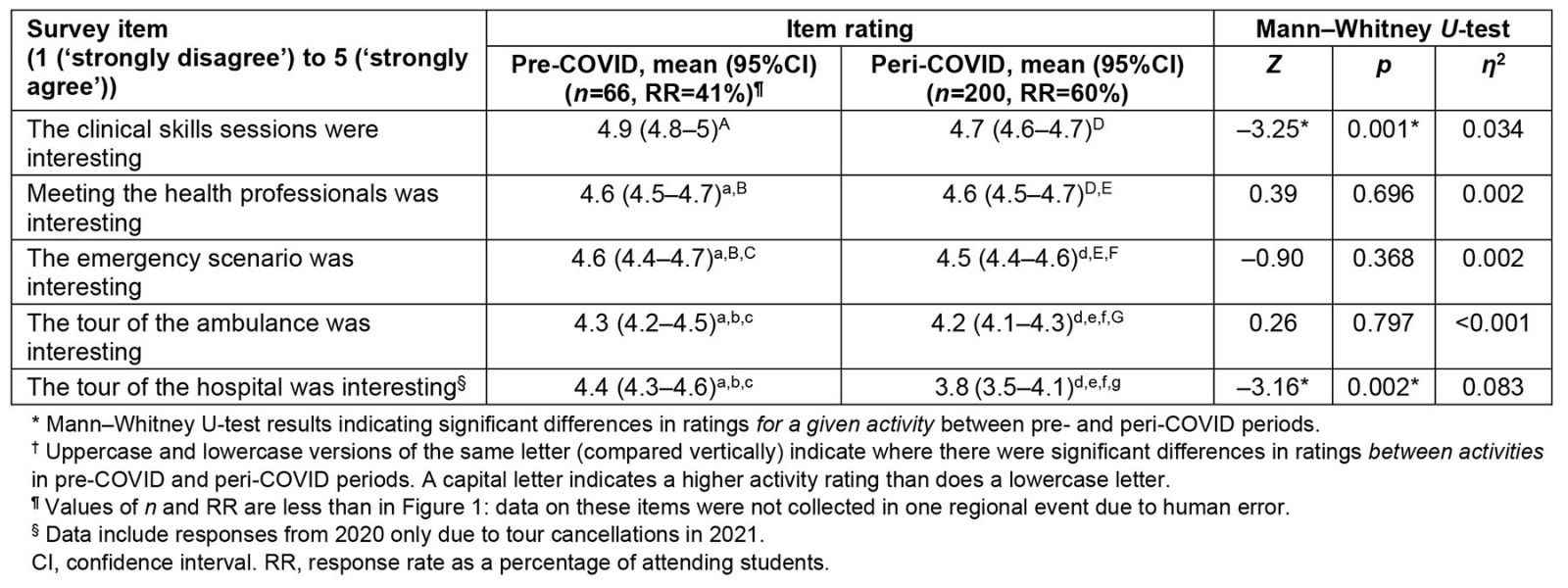
Qualitative feedback
Analysis of qualitative data generated four interpretive themes. No differences in themes were observed between years, hence themes are drawn from the full data set.
Almost all respondents provided a response to the question ‘What did you enjoy most?’ (n=365, 98%). Of these, ‘clinical skills’ (n=203, 55%) was the most common response. The most cited skill was suturing (n=57, 15%; eg ‘The practical stuff. My favourite part was sewing the pig foot together’), followed by CPR (n=28, 8%) and plastering (n=29, 8%). Most remaining comments described general enjoyment of the clinical skills activity (n=25, 7%; eg ‘The event I enjoyed the most would of [sic] been the clinical skills session’). The interactive hands-on (n=29, 8%) and practical (n=32, 9%) focus of the sessions was highlighted by students. One student made the following comment:
The hands-on stations at the end of the day. I really enjoyed trying everything and having a go at them all.
‘Interacting with professionals’ (n=146, 39%) includes comments describing students’ enjoyment talking to (n=52, 14%) or meeting (n=23, 6%) health professionals (eg ‘Talking to the different health professionals!! They are all so lovely’). Interactions with university students were also positively regarded (n=18, 5%; eg ‘Talking to the students at uni, they had really good advice [on] the different activities in the afternoon’). Some felt they better understood what specific health professionals do (n=46, 12%; eg ‘Going around to each healthcare professional’s station and gaining a better understanding of the practical work they do’) and were interested in their experiences (n=9, 2%; eg ‘I enjoyed talking to the professionals and hearing about their experiences’).
When asked ‘Is there anything you think we could do differently?’ over half of the respondents provided an answer (n=271, 55%); ‘no changes required’ (n=158, 58%) was the most common response. Within this theme most responses (n=94, 25%) indicated that students had no suggestion to contribute (eg ‘Nothing that I can think of’). The remainder of comments had no suggestions while also providing positive feedback on the Aspire2Health program (n=64, 17%; eg ‘N/A. Everything was great! Thank you!!’).
‘Variety and duration’ (n=40, 11%) reflected students desiring more time, content, professionals, and engagement. Increased time for activities was requested in general (n=18, 5%; eg ‘Maybe have the event go for longer like 2 days so you take more away from it’), for clinical skills (n=10, 3%) and for meeting the health professionals (n=8, 2%). One student commented:
After the round robin with each health professional, possibly catching up with any more questions again would be lovely and informative.
Some students (n=4, 1%), on the other hand, suggested less time for meeting the professionals (eg ‘Maybe make the session with the health professionals a bit shorter’). Others recommended more clinical skills sessions (n=12, 3%), more hospital tours (n=4, 1%) and more options in general (n=2, 1%). Other suggestions included interactive emergency scenarios (n=4, 1%) (eg ‘Involve students in the emergency scene inside the hospital’). Some wanted more professions represented (n=16, 4%), with most of these comments (n=13, 3%) specifying additional professions, as exemplified by this comment from a student:
The program could have included other health professions such as dentistry, pharmacy or optometry.
Discussion
This study reviewed Aspire2Health program feedback data pre-COVID (2019) and peri-COVID (2020–21) to explore the suitability of the program and its elements, its short-term impacts on student interest in health careers, and the impact of COVID on program experience and outcomes. Our findings show that Aspire2Health continued to motivate students to pursue health careers despite the disruptive impact of the pandemic. Further, activities with hands-on engagement or opportunities to interact with health professionals were of greater interest to students than hospital and ambulance tours. The results of this study may suggest that:
- despite health crises, rural health career outreach programs could continue to motivate students to pursue health careers
- rural health career outreach programs should prioritise hands-on activities and/or those involving interactions with health professionals to maximise student interest.
Pre- and peri-COVID students indicated the clinical skills, ‘meet the health professionals’ and emergency scenario were more interesting than the ambulance and hospital tours. Qualitative data support this result as well, with many students positively commenting on clinical skills or interactions with professionals, but few mentioning ambulance and hospital tours. The authors recognise that the COVID pandemic may have increased student interest in health careers. Self-selection of students does not enable us to determine if this was the case, or if differences in outcomes occurred because of different sample characteristics arising from such contextual changes. Student’s higher ratings of these activities – and requests for more activities, more time to meet the health professionals and a more interactive emergency scenario – may suggest that active engagement is key when designing rural health career outreach programs. This is valuable for program design, as prioritising ‘simpler’ activities that provide active engagement, such as clinical skills and meeting the health professionals, can generate high student interest while reducing reliance upon external organisations, equipment and facilities, accessibility to which can be limited by pandemics and other health emergencies.
Despite the influences of the pandemic on the program, its median impact measures ratings remained high (peri-COVID, M=4.5–4.7). No differences were observed pre- versus peri-COVID in students reporting the program had motivated them to pursue a career in health or recommending Aspire2Health to a friend. Aspire2Health operated only in Queensland during the pandemic, so some caution is required when generalising these outcomes in conditions with differing restrictions. Other health outreach programs have shown similar findings to Aspire2Health, albeit with smaller sample sizes (n=22–45), such as increased interest and consideration of health careers18,21,22, and high levels of program satisfaction18,20,22. A negative effect on Aspire2Health student ratings of ‘Overall, how would you rate the event?’ was detected; however, given its small effect size (η2=0.034) it is of little practical significance. Longitudinal studies would be required to determine the impact of Aspire2Health on converting latent interest in health care to motivation to pursue a health career; however, the high ratings of Aspire2Health for ‘Overall, how would you rate the event?’ and ‘The program has motivated me to pursue a career in health’ may indicate some success. More students participating in Aspire2Health were willing to recommend the program to a friend compared to past results from another medical school outreach program20. The robust scores of these three survey items suggest that Aspire2Health can run successfully in difficult circumstances, such as a pandemic, and continue to generate interest in health careers among rural secondary school students.
Data on the longer term impacts of rural health career outreach programs on career intentions and decisions are rarely reported19. This study is similarly limited and cannot comment on the long-term impacts of the Aspire2Health program. Future studies should assess rural health career outreach programs’ longitudinal impacts on students’ career choices and implement pre–post survey designs at each event to improve data quality. Studies assessing these impacts should also consider whether they are affected by student gender, identification as Aboriginal or Torres Strait Islanders and degree of rurality (eg regional, rural, remote). Post-COVID Aspire2Health program evaluations now collect this information, addressing this potential limitation for future investigations. Additionally, students’ pre- and post-event knowledge of pathways into tertiary health courses could be assessed to ensure that students possess an improved level of knowledge about the next steps required to convert interest in health careers to successful enrolment in health courses. The Aspire2Health program is ongoing, with the present iteration of the program already incorporating changes based upon the findings of this study. The Aspire2Health program no longer offers ambulance and hospital tours, with resources instead redirected to hands-on experiences and interactions with professionals. Other changes to the program include adding career advice sessions, expanding to other rural towns, developing resources for parents and school guidance officers, and increasing inter-event consistency. Future research using this program is currently underway to investigate the medium- and long-term impacts of the program on student intentions to pursue health careers.
Conclusion
Rural health career outreach programs offer rural students the chance to be actively involved in learning about health careers and provide experiential learning opportunities that would otherwise be difficult to access in their communities. Our findings suggest that rural health career outreach programs should focus on providing opportunities for active engagement via hands-on activities and ample interactions with health professionals. Rural health career outreach programs such as Aspire2Health could be run effectively, even during challenging circumstances such as pandemics, and continue to drive student interest in pursuing health careers. Optimising rural health career outreach program design could be a valuable, and thus far underresearched, piece of the sustainable rural health workforce puzzle.
Acknowledgements
Aspire2Health would not be possible without the collaboration of many organisations. The authors would like to thank the following organisations for their operational support: Rural Medical Education Australia; Southern Queensland Rural Health; Griffith University; University of Queensland, Rural Clinical School; University of Southern Queensland; Queensland Government, Department of Small Business, Employment and Training; Queensland Ambulance Service, Darling Downs and South West; Darling Downs Hospital and Health Service; South West Hospital and Health Service. We would like to thank the following organisations for their financial support: Darling Downs and West Moreton Primary Health Network, Western Queensland Primary Health Network and the Rural Health Multidisciplinary Training Program. The authors acknowledge Sherrilyn Walters, Jamie Quinn and Dr Adam Hulme for their assistance in revising the manuscript.
Funding
Funding for this research was provided by the Rural Health Multidisciplinary Training (RHMT) program grant of the Australian Government.
Conflicts of interest
Paul Purea and Nicola Cotter are involved in organising and facilitating the Aspire2Health program.


