Introduction
Rural Americans make up approximately 20% of the US population1 and experience more health disparities than their urban counterparts. Rural residents suffer higher all-cause mortality and are more likely to die of each of the 10 leading causes of death, including heart disease, cancer, accidents, chronic lower respiratory disease, stroke, Alzheimer’s disease, diabetes, kidney disease, influenza and pneumonia, and suicide2. While mortality rates for urban residents have been decreasing over the past 10 years, mortality rates among rural residents remain stagnant, resulting in a widening mortality disparity affecting rural residents2. Rural residents face barriers to healthcare access3, are more likely to be uninsured4, are more likely to live in poverty5, and are exposed to unique occupational and environmental toxicities6. These structural barriers, among others, contribute to higher rates of health-related unemployment, tobacco use, and physical inactivity7.
The ability to identify and address the mechanisms of these disparities is directly dependent on the quality of existing rurality measurements. Even within the US alone, there are multiple definitions and instruments used to determine rurality. These measures demonstrate a lack of agreement in classification of geographic areas as rural versus non-rural. Specific measures of US rurality include Rural–Urban Commuting Area (RUCA) codes, Metropolitan Statistical Areas, Rural–Urban Continuum codes, Urban Influence codes, County Designation, Core Based Statistical Areas and others8-12. Each measure variably defines rurality, relying on population density, commuting patterns, or proximity to key resources. In all cases, the measures are based on geographic characteristics, resulting in groupings of people that do not incorporate or accurately reflect the sociocultural differences in the populations captured by geographic classifications13. The most common measure of US rurality in health services research is the RUCA classification codes12. The US Department of Agriculture (USDA) developed the RUCA system for economic purposes14. RUCA codes are based on population density measures and population-level commuting patterns. The primary RUCA codes range from 1 to 10 and are defined as follows: (1) Metropolitan area core, (2) Metropolitan area high commuting, (3) Metropolitan area low commuting, (4) Micropolitan area core, (5) Micropolitan area high commuting, (6) Micropolitan area low commuting, (7) Small town core, (8) Small town high commuting, (9) Small town low commuting, and (10) Rural areas15. Conventionally primary RUCA codes 1–3 represent urban residences and 4–10 represent rural residences. Most uses of RUCA, including by the US Census and the US Health Resources and Services Administration, dichotomize areas into rural or urban16. Rural is defined as non-urban, or the lack of urbanicity as recognized by proximity to a populous urban core.
The lack of attention to individuals’ and groups’ sociocultural characteristics or identities limits the applicability of these measures to health services research aimed at improving health equity17. Categorizing residences as rural or urban based on commuting or relative proximity to a more populous ‘urban core’ may be appropriate for evaluating some mechanisms of disparities, such as connectivity to areas with healthcare services. Such dichotomization or definition of rurality based on the absence of urbanicity is inadequate for examining potential mechanisms related to health-related behaviors and socioeconomic effects on individuals and groups identifying as rural. For example, consider that a hospital closes in a small town. The hospital’s employees may now commute to a larger town an hour away for work, thereby changing the small town’s RUCA code to reflect this greater connectivity to the large town and decreasing the measured ‘rurality’ of the small town. However, the negative economic and health effects on the residents of the small town are not accurately represented by its new RUCA code. A rurality measure that reflects this multidimensional concept has been elusive due to the need to integrate cultural, demographic, economic, social, and equity factors17,18. A measure of rurality that considers individuals’ perceptions of their community identity while maintaining efficiency for large-scale research is needed to better conduct patient-centered rurality healthcare research. This is particularly true for research focused on behaviorally driven health topics, such as tobacco use, cardiovascular health, and vaccination uptake, or those related to occupational or environmental exposures. Implementation research also relies heavily on constructs such as acceptability, applicability, and relative priorities, necessitating rural measures that reflect social and cultural contexts. Using such patient-centered measures would facilitate the effective and efficient implementation of evidence-based treatments and programs. Additionally, patient-centered measures would better reflect individuals’ and groups’ experiences of potential discrimination based on their rurality, which has been underexplored in rural health but is critical to understanding and overcoming health inequities in other domains19.
Previous research has demonstrated only fair correlation between RUCA codes and individuals’ perceptions of their rurality or urbanicity among New Hampshire and Vermont residents20. However, this study was limited by the sample used, as New Hampshire and Vermont residents are probably not representative of the general US population. Additionally, after the study’s publication, the USDA announced that a programming error within the dataset used (ie RUCA-ZIP 3.10) had resulted in the misclassification of residents21,22. These findings raise concerns about the generalizability and data validity of the previous study. Therefore, we aimed to examine the concordance between people’s self-identification of rurality and their ZIP code-derived RUCA of rurality among a nationally representative sample, and determine patient-centered RUCA-based classifications of rurality and urbanicity.
Methods
We recruited US residents from CloudResearch’s Prime Panels, which is a platform that aggregates several online research panels to enable large-scale data collection with quality sample of respondents that are representative of the US population. Participants eligible for the survey were adults aged more than 18 years, US residents, and active members of the Prime Panels. We oversampled from areas defined as rural by conventional RUCA classifications (RUCA 4–10) based on national statistics that approximately 15–20% of US residents reside in areas defined by RUCA as rural16. All participants enrolled and completed the survey in January 2020.
Using commercially available Qualtrics software (Provo; www.qualtrics.com), we developed and administered a cross-sectional survey asking participants to report the rurality of their residence (ie ‘Do you live in a rural area?’ with the following available responses, ‘yes’, ‘no’, and ‘I do not know’), the rationale for their selection choosing one or more categorial options plus a free text option, ZIP code, and sociodemographic information. The survey was presented only in English and designed to be understandable by the general population based on a Flesch–Kincaid Grade Level23 of 7.3 that reflects seventh and eighth grade level of education in the US. All participants had to provide online informed consent prior to participation and received nominal compensation for successful completion of the survey. We estimated 10 minutes on average for survey completion. We reported frequency distributions of participant demographics.
We recruited 1135 participants, of which we excluded 302 for failing attention checks, two for living outside of the US, and 57 who failed to provide their perception of their rural or urban residence (Fig1). We derived the RUCA code area based on the participants’ provided ZIP code. We determined the concordance between their self-identified rurality and their ZIP code-derived RUCA classification of rurality by calculating an overall Cohen’s kappa (κ) statistic and percent agreement across four RUCA categories (RUCA 1, RUCA 2–3, RUCA 4, RUCA 5–10). We used the USDA’s 2010 RUCA codes, ZIP Code Database, updated in August 202015. In this study, p-values less than 0.05 were considered statistically significant. All analyses were conducted using R v4.2.0 (R Foundation; https://www.r-project.org).
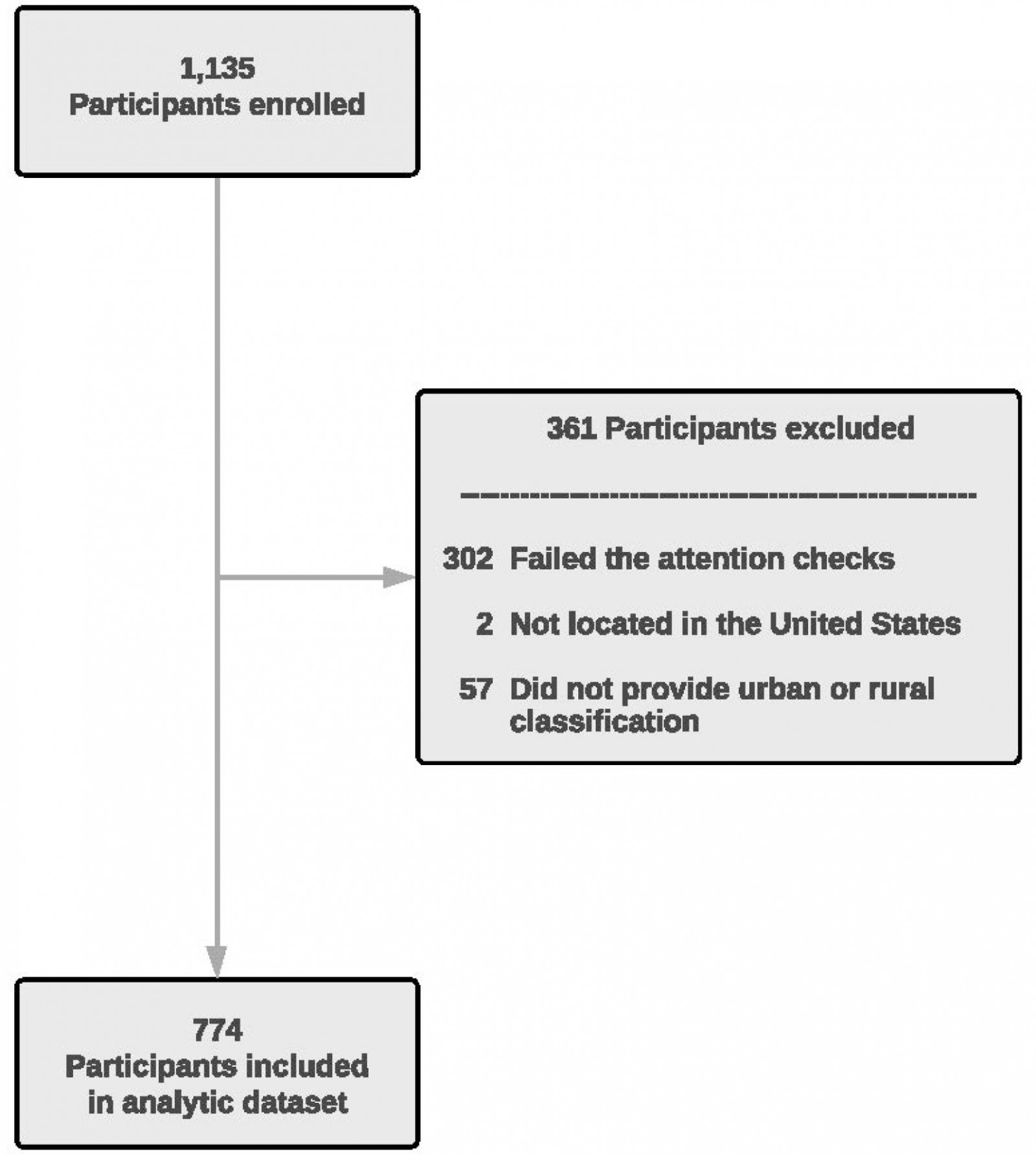 Figure 1: Flow diagram depicting the inclusion of participants in the analytic dataset.
Figure 1: Flow diagram depicting the inclusion of participants in the analytic dataset.
Ethics approval
The University of Pennsylvania Institutional Review Board approved all study procedures and found that the study was exempt from ongoing review (proposal 834506).
Results
We included 774 of 1135 participants, resulting in a successful survey completion rate of 68.2%. The average completion time was 11.9 minutes, and the average age was 46.1 years with a standard deviation of 16.3 years. In addition, 60.6% identified as women, 81.1% as White or Caucasian, 8.4% as Black or African American, 7.1% as multiracial, and 6.7% as Hispanic or Latino. The full demographics of participants is reported in Table 1.
Of 774 participants, 456 (59.0%) lived within RUCA codes 1–3, and 318 (41.1%) lived within RUCA areas 4–10, conventionally categorized as urban and rural, respectively (Table 2). Additionally, 394 (50.9%) participants self-identified as urban, while 380 (49.1%) self-identified as rural (Fig2). The overall Cohen’s kappa statistic indicated moderate agreement between perceived rurality and rural RUCA categorization (κ=0.48, 95%CI=0.42–0.54). Agreement was 77.8% among people living within densely populated RUCA-defined urban areas (RUCA 1; n=405), 63.4% among people living within moderately populated rural areas (RUCA 4; n=134), and highest among people living in sparsely populated RUCA-defined rural areas regarding less of commuting patterns (89.1%, RUCA 5–10; n=184) (Table 2). However, agreement was only 19.6% among people living within proximity of and commuting to RUCA-defined urban areas (RUCA 2–3; n=51). Based on our results, we reclassified RUCA 2–3 designations as rural. Agreement for individuals living in RUCA 2–3 increased to 80.4% and resulted in an increase in overall concordance (κ=0.56; 95%CI=0.50–0.62), using the revised RUCA classification (Fig2).
Among the 51 participants residing in RUCA codes 2–3, 41 (80.4%) their rural self-identification was discordant with conventional urban classification for RUCA 2–3. Among 40 of these 41 respondents, the most frequently reported reasons for this discordance were their perceptions of the population density, their proximity to the nearest neighbor, their proximity to the city or metropolitan area, the number of homes in their area, and their drive distance to work (Fig3).
Table 1: Participant demographics by conventional RUCA classification of urban and rural designations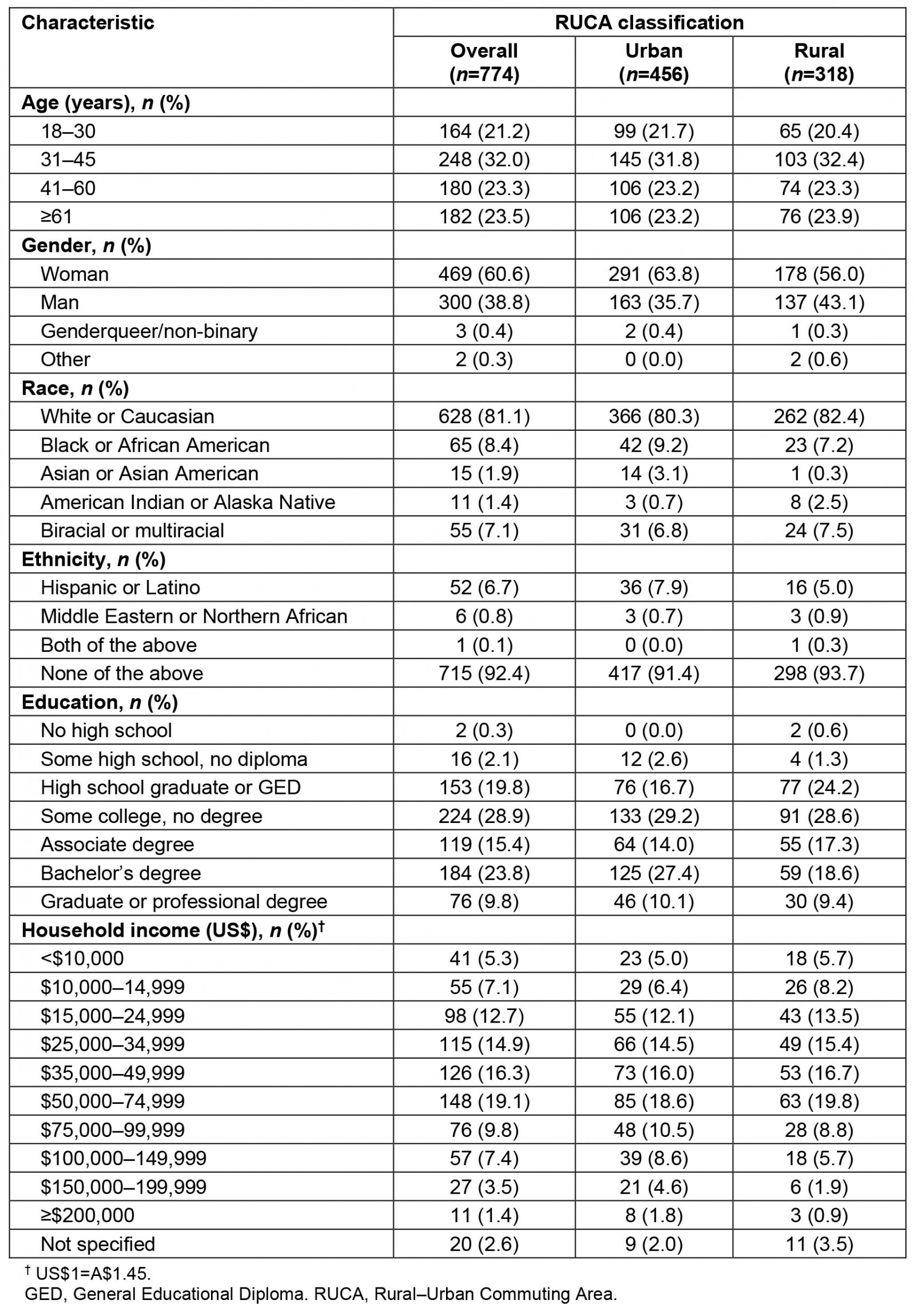
Table 2: Percent agreement between self-identification as urban or rural with conventional RUCA classification by RUCA code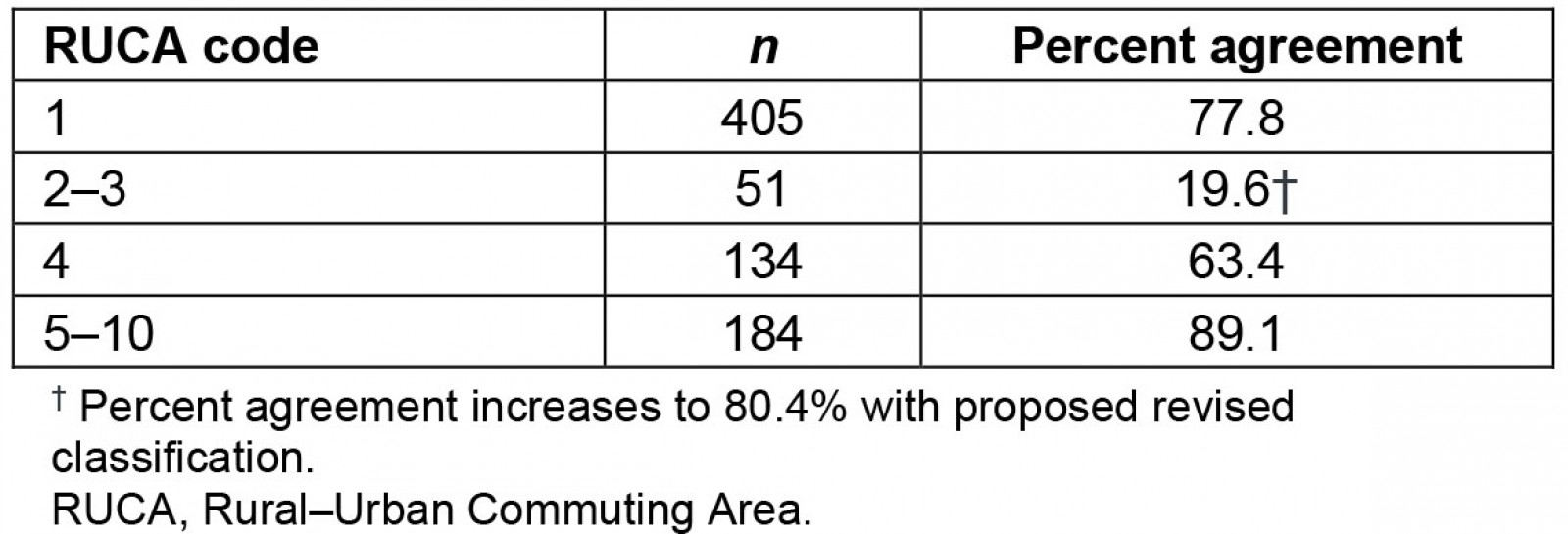
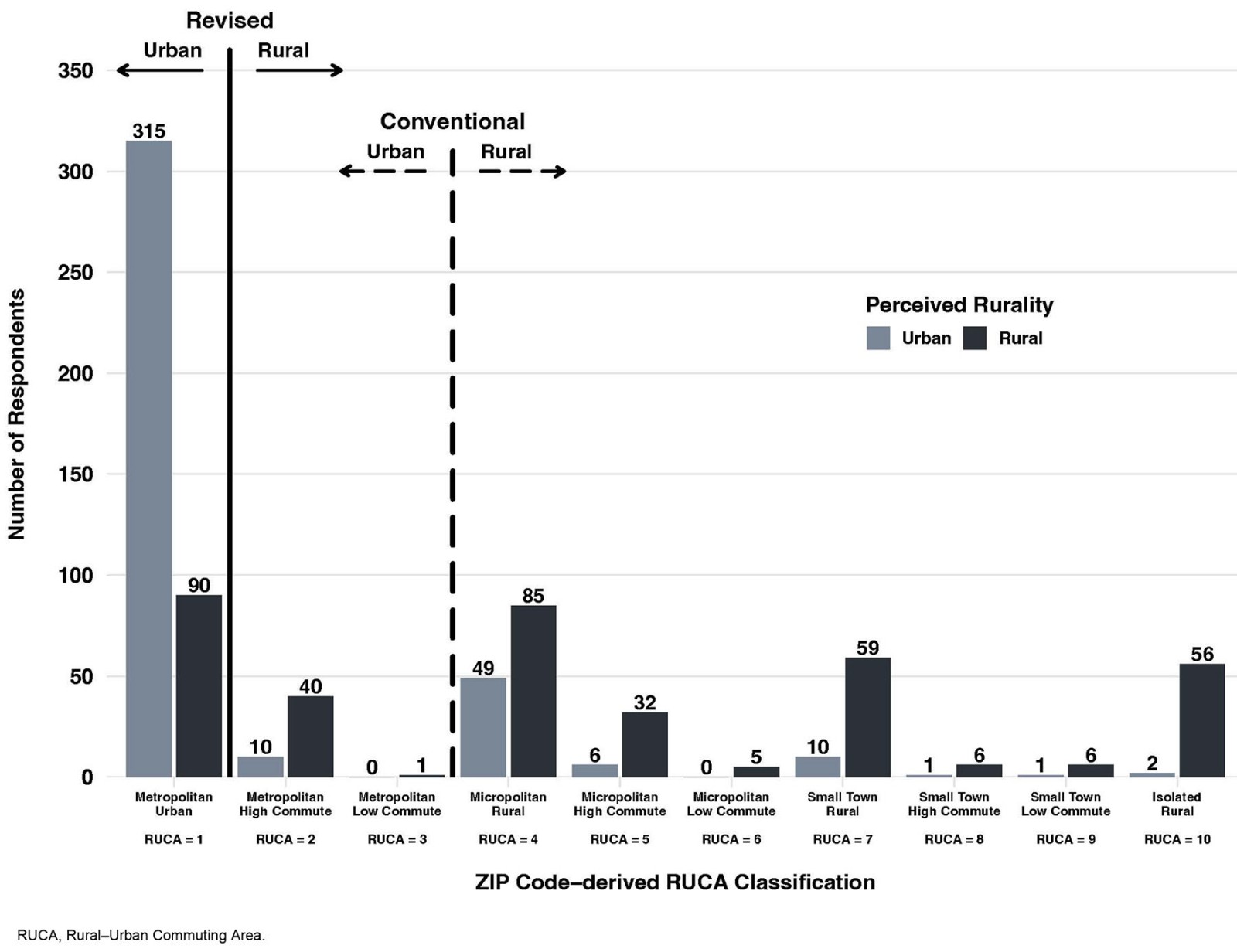 Figure 2: Participants’ self-identification as urban or rural by RUCA classification and proposed revised classification.
Figure 2: Participants’ self-identification as urban or rural by RUCA classification and proposed revised classification.
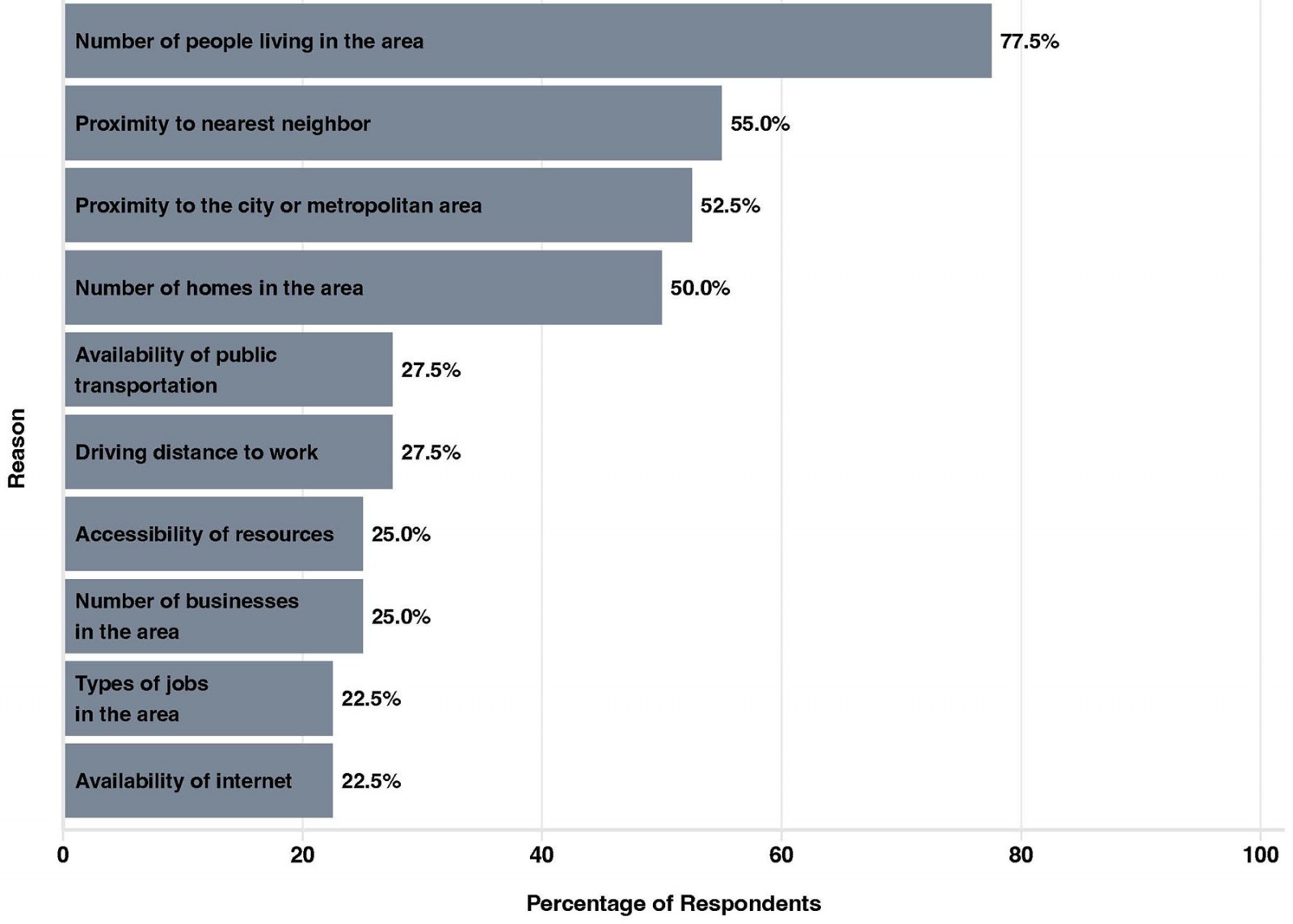 Figure 3: Reasons given by 40 respondents for selecting rural residence (RUCA 2 and RUCA 3).
Figure 3: Reasons given by 40 respondents for selecting rural residence (RUCA 2 and RUCA 3).
Discussion
Among a national sample of US residents, we found that conventional location and commuting-based definitions of rurality poorly correlate with individuals’ perceptions of their own residential rurality. Concordance between RUCA classification and self-perception was lowest among those living in RUCA codes 2 and 3. Reclassifying RUCA codes 2 and 3 as rural improved the overall concordance and represented a more patient-centric measure of rurality. Our findings have important implications for efforts to identify and address mechanisms of health outcome disparities experienced by rural residents.
Prior work has described both discordance across standardized measures of rurality and between these standardized measures and individuals’ self-perceived rurality of residence8,12,20,24. We found that individuals residing in RUCA codes 2 and 3 self-identify as rural, despite living in an area considered urban by the conventional classification systems. When asked why they identified as rural, they cited reasons that most closely relate to population density. This suggests that population density is important for the shared understanding of ‘rurality’ as a concept. However, other socioecological characteristics such as the availability of infrastructure resources or the types of jobs in the area were also frequently identified as informing their self-classification of living in a rural area. These are inadequately accounted for in existing measures of rurality, which rely heavily on population density and commuting patterns.
Rurality as a concept is complex and lacks a single unifying definition that is widely accepted. While most standardized measures focus on rural versus urban dichotomies, this fails to reflect the heterogeneity in geographic and socioecological experiences of place. Our findings suggest that patient-reported rurality diverges from standardized RUCA classifications, probably reflecting that individuals have nuanced interpretations or connections with a rural identity based on these experiences. While our sample size is insufficient to fully explore this heterogeneity across sociodemographic characteristics, we identify an important area for future work. Critical next steps include further exploration of how individuals’ and groups’ other identities influence and intersect with rural identities. Qualitative work to determine the key components leading to self-identifying as rural would help to refine a patient-centered definition and measure of rurality.
Identifying and addressing the mechanisms of disparities experienced by rural residents requires measuring rurality, even when complex or heterogenous. Our findings provide insight into how to optimize this within ongoing or future research. To the extent possible, measures of rurality should be tailored to the study or need based on the proposed mechanism being evaluated or intervention being tested. The evaluation of mechanisms that may be influenced by an individual’s perception or identity, such as health behaviors or equity, should prioritize using a patient-centered definition. Ideally, collecting participants’ self-identities should be used when feasible, given the only moderate concordance with standardized measures, particularly for research based on health behaviors, implementation of new programs or treatments, or related to disparities in experiences or outcomes. Ongoing comparisons between self-identification of rurality and standardized measures will help with further refinement of these patient-centered definitions, particularly as they relate to key health outcomes. However, when self-identity is not captured or feasible, the development of measures of rurality that better reflect individuals’ perceptions and behaviors is needed. Until such a measure is developed, the use of RUCA codes may be improved by categorizing RUCA 2–3 as rural based on our findings. We suggest investigators consider sensitivity analyses that identify how changing RUCA-based definitions of rurality alter their findings or conclusions. Additionally, because 22% of those living in RUCA 1 (ie a metropolitan area core) self-identify as rural, additional refinement may be possible in the future.
Our study has several limitations to consider. First, the use of an online survey cohort may not be generalizable to the general population, specifically leaving out those who do not have internet access. However, using a national cohort and oversampling rural participants represents an improvement over previous studies. Our sample population may not adequately represent non-White rural residents or those with limited English proficiency, who may have different perspectives on rurality. While our sample demographics approximate the demographics in rural areas, this limited our ability to explore associations between rural self-identification and sociodemographics. Lastly, our reliance on dichotomized rural versus non-rural framing, while aligned with existing standardized definitions, limits our ability to comment on the heterogeneity of geographic identity.
Conclusion
A patient-centered rural–urban classification is required to effectively evaluate the impact of rurality on health, healthcare delivery, and health equity. This study presents a more patient-centric RUCA-based classification of rurality that can be easily operationalized in future research in situations in which self-reported rural status is missing or challenging to obtain.
Funding
This research project was generously supported by the Patient-Centered Outcomes Research Institute.
Conflicts of interest
The authors have no conflicts of interest to disclose.
