Introduction
Maternal mortality is a critical global health challenge and a central indicator of health system performance. In 2023 more than 260,000 women died from pregnancy and childbirth-related causes, equivalent to nearly one death every two minutes1. Sustainable Development Goal (SDG) 3.1 aims to reduce the global maternal mortality ratio (MMR) to fewer than 70 per 100,000 live births by 20302. Although the global MMR has declined by about 40% since 2000, progress has slowed in recent years, and over 90% of maternal deaths continue to occur in low- and middle-income countries (LMICs)1. Biomedical complications such as hemorrhage, eclampsia, and sepsis are the direct causes of maternal death, but broader determinants including socioeconomic inequities, cultural practices, and weaknesses in health systems strongly influence survival3.
Indonesia reflects these global challenges. The national MMR decreased from 305 in 2015 to 189 per 100,000 live births in 2020, yet it remains among the highest in South-East Asia and far from the SDG target4,5. National averages conceal extreme disparities: the 2020 Long-Form Population Census reported provincial MMRs ranging from 48 in Jakarta to 565 in Papua5. Such inequities underscore the need to examine maternal mortality in subnational contexts.
Access to maternal health services is deeply unequal across regions. Women in Java and Bali are more than three times as likely to complete four or more antenatal visits compared with women in Papua (odds ratio (OR): 3.6, 95% confidence interval (CI): 2.7–4.7)6. Skilled birth attendance and facility-based deliveries are also low in Papua7,8. Geographic barriers further exacerbate inequities: nationally the average distance to a health facility is 5 km, but in Papua and other eastern provinces it exceeds 30 km. Nearly 28% of Papuans, predominantly in rural areas, require more than an hour to reach a health center compared with fewer than 11% in many western provinces9. These rural–urban disparities delay access to emergency obstetric care and contribute to higher maternal mortality10.
Papua represents one of the most disadvantaged provinces in Indonesia, combining high maternal mortality with remote geography, limited health infrastructure, and entrenched cultural practices that hinder care-seeking11,12. Many districts are mountainous and sparsely populated, complicating the retention of skilled health workers13 and delivery of essential maternal health services. For these reasons, Papua provides a critical setting to investigate how structural and individual factors interact to shape maternal survival.
Previous studies on maternal mortality in Indonesia have mostly emphasized biomedical complications1,3 or relied on national-level averages, without accounting for sharp structural differences across regions. Few have applied a multilevel framework to capture both individual- and community-level determinants simultaneously. This study addresses that gap by analyzing maternal deaths in Papua using the 2020 Indonesia Population Census. Particular attention is given to rural–urban residence, as it reflects systemic inequities. By integrating sociodemographic characteristics with community-level health system indicators, this study provides new evidence to inform equitable maternal health strategies in rural and remote settings.
Conceptual framework
This study adopts the maternal health and mortality determinants framework proposed by Souza et al3, which organizes risk factors across individual, community, and structural levels. The framework emphasizes that maternal deaths arise from an interaction of biological, social, and health system determinants, and that the dominant drivers shift as countries transition from high to lower mortality contexts. Applying this perspective to Papua, where maternal mortality remains high, highlights the importance of both individual sociodemographic factors and systemic barriers such as healthcare access and workforce distribution.
Methods
The study followed the Strengthening the Reporting of Observational Studies in Epidemiology (STROBE) guidelines. Data were drawn from the 2020 Indonesian Population Census, conducted by the Indonesian Statistical Agency (Badan Pusat Statistik, BPS). Access to anonymized data is available through the BPS research service portal. Maternal deaths were identified using the census mortality module, which asked households whether, since 1 January 2017, any woman who was pregnant or had ever been pregnant had died and, if so, whether the death occurred during pregnancy or within 42 days postpartum14,15. This approach, comparable to simplified verbal autopsy methods, enables identification of maternal deaths in contexts where medical certification is limited. Figure 1 illustrates the sample selection process. From 471,794 individuals in the 2020 Papua Province Census, we excluded males, women outside the reproductive age group of 15–49 years, and women aged 15–49 years without a pregnancy record since 2017, as maternal mortality can only be assessed among those with a pregnancy during the reference period. We also removed duplicate records to avoid double-counting. After these exclusions, the final analytic sample consisted of 18,886 women aged 15–49 years with a pregnancy record.
The outcome variable was maternal death, defined according to WHO guidelines as the death of a woman while pregnant or within 42 days of termination of pregnancy, excluding accidental or incidental causes15. The variable was coded as binary (maternal death and survival). Predictor variables were chosen based on prior literature3 and census data availability. Individual-level variables included age, parity, marital status, educational attainment, and place of residence.
Age and parity capture reproductive risk, while marital status and education proxy for social and economic support. Parity was categorized into three groups: nulliparity, defined as a first pregnancy; low multiparity, defined as one to three previous births; and grand multiparity, defined as four or more previous births. Educational attainment was classified into three categories based on the highest level of schooling completed. Low education included respondents who had never attended school, did not complete primary school, or completed only primary education. Middle education comprised those who had completed junior high school senior high school or a diploma. High education referred to those with a bachelor’s degree or higher. Place of residence was classified as rural or urban using pre-coded criteria, which consider population density, infrastructure, and administrative status. Rural residence in Papua is strongly associated with longer travel distances to health facilities, limited availability of skilled health workers, and reliance on traditional practices, making it a central variable of interest.
Community-level variables included the density of health workers per 1000 population, the number of hospitals, and the number of community health centers per regency. In Indonesia, a regency (kabupaten) represents the second-level administrative division beneath a province, governing both rural and semi-urban areas. It functions at a scale broadly equivalent to a county-level jurisdiction in the US or UK, or a local government area in Australia, and is administratively parallel to an urban city (kota). Community-level data were obtained from the Indonesian Statistical Agency and are publicly accessible through its official website.
 Figure 1: Sample selection process based on data from 2020 Indonesian Population Census.
Figure 1: Sample selection process based on data from 2020 Indonesian Population Census.
Statistical analysis
Descriptive statistics summarized the distribution of individual- and community-level variables. Bivariate associations between maternal death and covariates were examined using χ2 tests. Considering the hierarchical nature of the data, with individuals nested within regencies, multilevel logistic regression analyses were performed using the generalized linear mixed model procedure (PROC GLIMMIX)16. The modeling was conducted sequentially: beginning with an empty (null) model estimating baseline regency-level variance in maternal mortality; followed by a model adjusting for individual-level characteristics; and culminating in a fully adjusted model incorporating both individual- and community-level determinants.
Model fit and performance were evaluated by comparing −2 log likelihood values across sequential models. To quantify the proportion of variance attributable to contextual factors, the intraclass correlation coefficient (ICC) was calculated at the regency level. Additionally, the median odds ratio (MOR) was computed to provide an interpretable measure of heterogeneity in maternal mortality risk across regencies, representing the median increase in odds when moving between regencies with differing risk profiles.
For sensitivity analysis, modified Poisson regression with robust variance estimation was conducted through PROC GLIMMIX, aligning with the main approach by modeling cluster-specific random effects. Consistency of estimates across models supported the robustness of the results. All analyses were conducted using Statistical Analysis v9.4 (SAS Institute; https://www.sas.com), with a two-sided p-value <0.05 considered statistically significant.
Ethics approval
The study was based on anonymized secondary data from the 2020 Indonesia Population Census. No personally identifiable information was used, and institutional review board exemption was obtained from the Public Health Faculty, Jember State University, Indonesia, No. 541/KEPK/FKM-UNEJ/VIII/2024. The study followed the STROBE guidelines, and a completed checklist is provided in Supplementary table 1 to support transparency and reproducibility.
Results
Table 1 presents the distribution of sociodemographic and healthcare-related factors according to maternal survival status. Maternal deaths were significantly more frequent among adolescents (<19 years, 2.1%) and women older than 35 years (0.8%) compared with those aged 19–35 years (0.5%; p<0.001). Nulliparous women experienced the highest proportion of deaths (2.3%) relative to women with low multiparity (0.4%) or grand multiparity (0.2%; p<0.001). Similarly, single or divorced women had a substantially higher risk of death (2.3%) compared with married women (0.4%, p<0.001).
Education showed a clear gradient, with deaths most common among women with low education (0.9%), compared with middle (0.5%) and high education (0.3%; p<0.001). Rural residence was also associated with higher maternal mortality (0.8%) than urban residence (0.4%, p<0.001).
At the community level, maternal deaths were more common in districts with a health worker density less than 2.5 per 1000 population (1.0%) compared with those at or greater than this threshold (0.3%, p<0.001). On average, regencies reported 2.06 hospitals (standard deviation (SD) 1.75) and 18.71 community health centers (SD 6.25).
Table 2 shows the variance components and model fit statistics from the multilevel logistic regression analysis. In the null model, the variance at the regency level was 5.50 (2.52), indicating substantial heterogeneity across districts. The corresponding ICC was 0.62, suggesting that 62% of the total variation in maternal deaths was attributable to differences between regencies. The MOR was 9.37, meaning that, on average, the odds of maternal death could increase almost 10-fold if a woman moved from a lower risk to a higher risk regency.
When individual-level covariates were added (model 1), the variance remained high (5.57), with an ICC of 0.62 and MOR of 9.51, indicating persistent contextual disparities even after adjusting for personal characteristics. In the fully adjusted model (model 2), which included both individual- and community-level factors, the variance decreased slightly to 5.27, with the ICC at 0.61 and MOR at 8.95. This suggests that community-level health system factors only modestly reduced unexplained regional variation. The model fit improved considerably from the null model (−2 log likelihood reduced from 9021.14 to 7909.43), confirming that the inclusion of covariates substantially enhanced explanatory power.
Figure 2 presents the community-level random intercepts with 95% confidence intervals, illustrating the heterogeneity in maternal mortality risk across regencies. Several regencies had significantly higher or lower baseline risks even after adjusting for individual- and community-level covariates, consistent with the high ICC and MOR values. This visualization reinforces the finding that large unexplained disparities persist between regencies, highlighting the importance of contextual factors beyond individual sociodemographic characteristics and facility availability.
Estimates for individual-level variables are reported from model 1, while contextual factors are presented from the full multilevel model 2. This presentation allows comparison between individual- and community-level effects on maternal mortality. As shown in Table 3, several individual-level characteristics were significantly associated with maternal deaths. Compared with women aged 19–35 years, those older than 35 years had almost threefold higher odds of death (aOR: 2.92, 95%CI: 2.45–3.47), while adolescents (<19 years) did not differ significantly. Nulliparous women had markedly elevated odds of death compared to women with low multiparity (aOR: 5.94, 95%CI: 4.74–7.44), whereas grand multiparity was not associated with increased risk (aOR: 0.90, 95%CI: 0.68–1.19). Single or divorced women faced almost three times higher odds of maternal death compared with married women (aOR: 2.79, 95%CI: 2.19–3.56). Educational attainment was inversely associated with maternal mortality: women with low education (aOR: 2.03, 95%CI: 1.38–3.00) and middle education (aOR: 1.58, 95%CI: 1.08–2.31) had significantly greater risk compared with those with high education. Residence also played an important role: women in rural areas were almost twice as likely to die as their urban counterparts (aOR: 1.95, 95%CI: 1.56–2.45). At the community level, however, none of the contextual variables showed statistically significant associations with maternal death. Sensitivity analyses using modified Poisson regression with robust variance produced similar estimates, confirming the robustness of the main findings (see supplementary table 3).
Table 1: Sociodemographic and healthcare-related factors of maternal deaths in Java province, Indonesia (2020 Indonesian Population Census)
| Factor | Characteristic | Variable | Total | Survived (n=18,717) | Died (n=169) |
p-value (weighted χ2) |
||
|---|---|---|---|---|---|---|---|---|
| n | n | Weighted % | n | Weighted % | ||||
| Sociodemographic | Age (years) | <19 | 1924 | 1875 | 97.9 | 49 | 2.1 | <0.001 |
| 19–35 | 12,146 | 12,070 | 99.5 | 76 | 0.5 | |||
| >35 | 4816 | 4772 | 99.2 | 44 | 0.8 | |||
| Parity | Nulliparity | 3964 | 3853 | 97.7 | 111 | 2.3 | <0.001 | |
| Low multiparity | 10,619 | 10,577 | 99.6 | 42 | 0.4 | |||
| Grand multiparity | 4303 | 4287 | 99.8 | 16 | 0.2 | |||
| Marital status | Single/divorced | 3407 | 3311 | 97.7 | 96 | 2.3 | <0.001 | |
| Married | 15,479 | 15,406 | 99.6 | 73 | 0.4 | |||
| Education | Low | 9159 | 9054 | 99.1 | 105 | 0.9 | <0.001 | |
| Middle | 8618 | 8558 | 99.5 | 60 | 0.5 | |||
| High | 1109 | 1105 | 99.7 | 4 | 0.3 | |||
| Residence | Urban | 5723 | 5685 | 99.6 | 38 | 0.4 | <0.001 | |
| Rural | 13,163 | 13,032 | 99.2 | 131 | 0.8 | |||
| Healthcare-related | Health worker density | <2.5/1000 people | 7712 | 7596 | 99.0 | 112 | 1.0 | <0.001 |
| ≥2.5/1000 people | 11,193 | 11,121 | 99.7 | 57 | 0.3 | |||
| Number of hospitals: 2.06±1.75 | ||||||||
| Number of community health centers: 18.71±6.25 | ||||||||
Table 2: Estimates of multilevel logistic regression model of maternal deaths in Java province, Indonesia (2020 Indonesian Population Census)
| Parameter | Null model | Model 1 | Model 2 |
|---|---|---|---|
| Variance (standard error) | 5.50 (2.52) | 5.57 (2.24) | 5.27 (2.15) |
| Intra-class correlation | 0.62 | 0.62 | 0.61 |
| Median odds ratio | 9.37 | 9.51 | 8.95 |
| –2 log likelihood | 9021.14 | 7916.46 | 7909.43 |
Table 3: Assessment results of sociodemographic and healthcare-related factors associated with maternal deaths in Java province, Indonesia (2020 Indonesian Population Census)
| Level | Characteristic | Variable | Null model | Model 1 | Model 2 | |||
|---|---|---|---|---|---|---|---|---|
| aOR (95%CI) | p-value | aOR (95%CI) | p-value | aOR (95%CI) | p-value | |||
| Individual | Age (years) | <19 | – | – | 0.91 (0.74–1.12) | 0.3603 | 0.91 (0.74–1.12) | 0.3605 |
| 19–35 | – | – | 1.00 | 1.00 | ||||
| >35 | – | – | 2.92 (2.45–3.47) | <0.0001 | 2.92 (2.45–3.47) | <0.0001 | ||
| Parity | Nulliparity | – | – | 5.94 (4.74–7.44) | <0.0001 | 5.94 (4.74–7.44) | <0.0001 | |
| Low multiparity | – | – | 1.00 | 1.00 | ||||
| Grand multiparity | – | – | 0.90 (0.68–1.19) | 0.4625 | 0.90 (0.68–1.19) | 0.4595 | ||
| Marital status | Single/divorced | – | – | 2.79 (2.19–3.56) | <0.0001 | 2.79 (2.19–3.55) | <0.0001 | |
| Married | – | – | 1.00 | |||||
| Education | Low | – | – | 2.03 (1.38–3.00) | 0.0004 | 2.03 (1.08–3.00) | 0.0004 | |
| Middle | – | – | 1.59 (1.09–2.32) | 0.0172 | 1.58 (1.08–2.31) | 0.0176 | ||
| High | – | – | 1.00 | |||||
| Residence | Rural | – | – | 1.60 (1.30–2.00) | <0.0001 | 1.95 (1.56–2.45) | <0.0001 | |
| Urban | – | – | 1.00 | |||||
| Community | Health worker density | <2.5/1000 | – | – | – | 1.20 (0.15–9.34) | 0.8612 | |
| – | – | – | 1.00 | |||||
| Number of hospitals | – | – | – | – | 1.66 (0.83–3.34) | 0.153 | ||
| Number of community health centers | – | – | – | – | 1.14 (0.97–1.33) | 0.1161 | ||
aOR, adjusted odds ratio. CI, confidence interval.
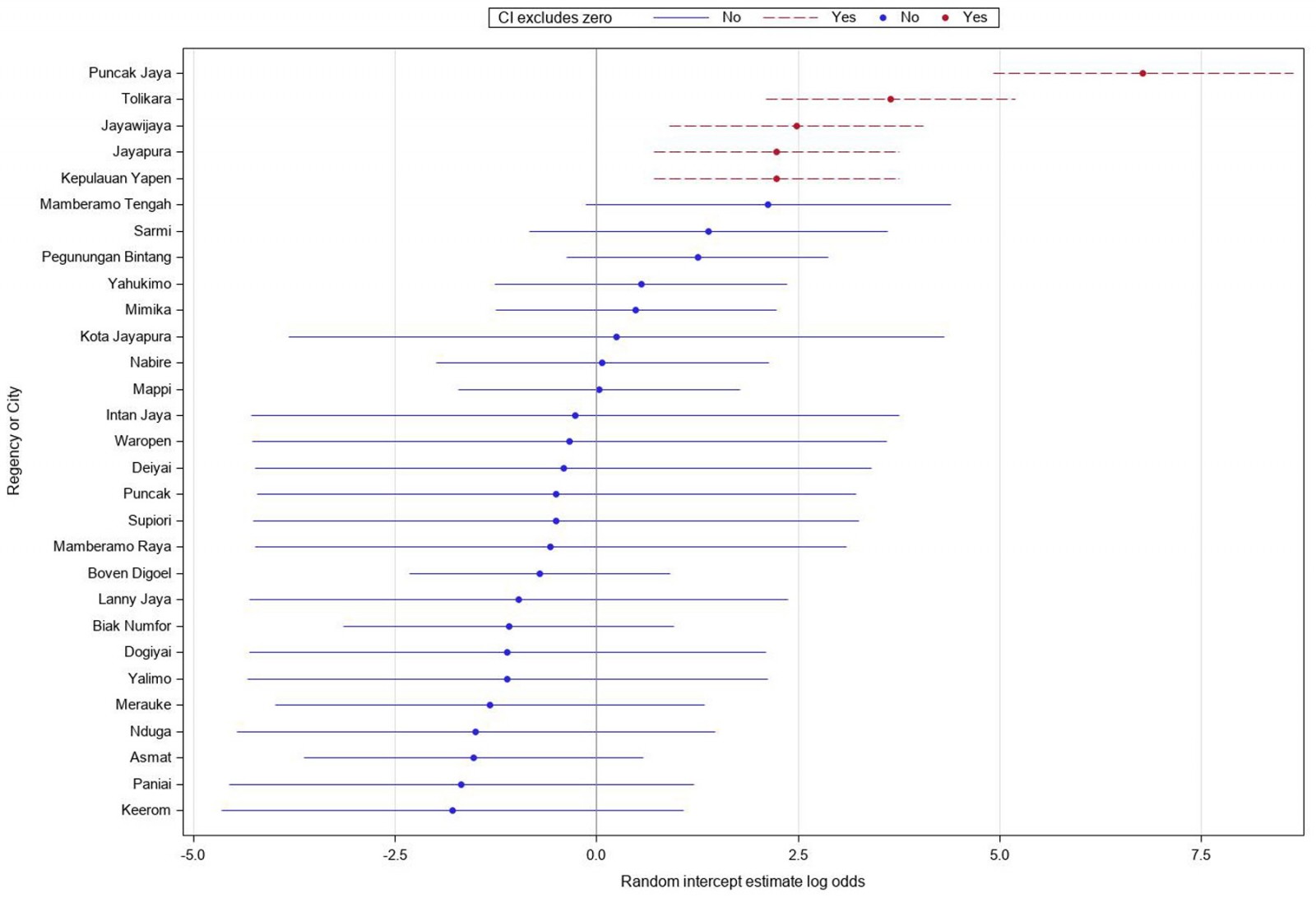 Figure 2: Caterpillar plot of community-level random intercepts from multilevel logistic regression.
Figure 2: Caterpillar plot of community-level random intercepts from multilevel logistic regression.
Discussion
This study applied a multi-level analysis to examine both individual- and community-level factors associated with maternal death events, aiming to inform evidence-based policy strategies to reduce maternal mortality in Papua province. While the data were collected in 2020, they remain relevant for analysis of maternal mortality because the census provides the most comprehensive source of maternal death events in Papua. We also acknowledge that subsequent events, particularly the COVID-19 pandemic and recent health policy reforms, may have influenced maternal health outcomes. This limitation should be considered when interpreting the findings. Nevertheless, the 2020 Indonesian Population Census remains the only province-wide dataset capturing maternal deaths in Papua, and thus provides uniquely valuable evidence despite the time gap.
At the individual level, sociodemographic characteristics of women were significantly associated with maternal deaths. Pregnancy in women aged more than 35 years was associated with a higher risk of maternal death, whereas pregnancy in women aged less than 19 years was not statistically significant compared with those aged 19–35 years. Nevertheless, the proportion of maternal deaths among adolescents was highest (Table 1). Evidence from the US consistently shows elevated risks beginning at age 35 years17,18, likely due to chronic comorbidities and physiological changes that reduce adaptability to pregnancy, compounded by social determinants such as limited healthcare access and sociodemographic disadvantage. In contrast, the risk associated with adolescent pregnancy is more variable and context-dependent. Some studies demonstrate that very young maternal age, particularly in resource-limited settings, increases maternal mortality through biological immaturity and restricted access to care19, while others find no significant or only modestly elevated risk compared with women aged 20–35 years. This suggests a J- or U-shaped relationship between maternal age and mortality, with the lowest risk observed among women aged 20–29 years20.
Globally, WHO identifies complications in pregnancy and childbirth as the leading cause of death among girls aged 15–19 years1,21. In Indonesia, child marriage is often influenced by sociodemographic and cultural factors and remains a critical contributor to adolescent pregnancy22-24. Although the legal minimum age for marriage has recently been raised, the dispensation system still allows early marriage in practice23. Stronger policy enforcement, together with comprehensive reproductive health education and community engagement, are essential to reduce the risks associated with early marriage and adolescent pregnancy.
Nulliparous women were found to be at higher risk of maternal death compared with women who had previous childbirth experience, a finding consistent with systematic reviews from LMICs25. In our analytic sample, nulliparity accounted for approximately 21% of pregnancies, underscoring the importance of first pregnancies as a vulnerable group in Papua. Nationally, the 2017 Indonesian Demographic and Health Survey reported that about 7% of girls aged 15–19 years had already begun childbearing, and the prevalence is higher in rural and eastern provinces, including Papua26. These patterns indicate that both adolescent and first pregnancies remain important contributors to maternal risk in the region. Evidence from China indicates that advanced maternal age elevates the risk of gestational hypertension and pre-eclampsia, particularly among nulliparous women27.
Marital status also emerged as an important determinant. Women without partners experienced a substantially higher risk of maternal death compared with married women. Indonesian evidence shows that unmarried women and adolescents with unintended pregnancies are less likely to complete the recommended four antenatal care visits, reflecting both stigma and barriers within the health system. Although programs such as the youth care health program Pelayanan Kesehatan Peduli Remaja (Adolescent-Friendly Health Services) are designed to provide confidential and supportive reproductive health services, coverage and utilization remain limited in Papua28. This is consistent with findings from the US, where married women demonstrated better maternal outcomes, partly due to greater social and financial support29. In Malaysia, unmarried women were more likely to underutilize prenatal services, engage in unhealthy behaviors such as smoking and alcohol consumption, and report a higher prevalence of depressive symptoms30. Such factors increase vulnerability during pregnancy and childbirth. Collectively, these findings underscore the importance of supportive programs that enable both nulliparous and unmarried women to access timely and high-quality prenatal care without stigma.
Education and place of residence were also significant contributors to maternal death. Women with lower levels of education and those living in rural areas faced a higher risk, consistent with findings from previous studies 3,25,31,32. Higher educational attainment is known to enhance reproductive decision-making, promote positive health-seeking behaviors, strengthen women’s autonomy, and facilitate the timely use of maternal health services33. In contrast, rural residence often reflects structural barriers, including limited availability of healthcare facilities, slower adoption of medical technologies, and greater travel distances to reach obstetric care, all of which contribute to delays in receiving appropriate treatment34,35.
At the community level, more than half of the variability in maternal deaths was attributable to contextual factors, underscoring the importance of applying a multilevel analytical approach. This finding should be interpreted with caution. Health workforce availability emerged as an important factor. Health worker density below WHO’s recommended threshold of 2.5 per 1000 population was not statistically associated with higher maternal mortality in this study. This finding is consistent with a previous published study in Indonesia36. Previous research from Sub-Saharan Africa and other settings has demonstrated that greater health workforce density correlates with improved maternal health outcomes37,38. Retention of healthcare workers in remote and rural areas of Indonesia remains a national challenge39, particularly in Papua, where difficult geographical access and limited career opportunities hinder long-term retention. Strengthening incentives, professional development, and community-based deployment strategies will be essential to improve health worker availability in these underserved regions.
Although the number of hospitals and community health centers in a regency was included as community-level variables, neither showed a statistically significant association with maternal mortality. This finding suggests that the mere availability of facilities may not be sufficient to reduce maternal deaths. Similar results have been reported in other low-resource settings, where hospital proximity or distance alone was not necessarily associated with maternal mortality40. Several explanations are possible. First, facility presence does not guarantee functionality, quality of care, or readiness to manage obstetric emergencies41. Many rural health centers in Indonesia lack trained personnel, essential supplies, and reliable referral systems42,43, which limits their ability to prevent maternal deaths even when facilities are physically available. Second, geographic barriers remain substantial, and women living in remote areas may still face long travel times to reach hospitals, particularly in emergency situations44,45. Third, under-reporting and misclassification of deaths outside health facilities may distort the apparent association46,47. As reporting systems improve and more deaths are captured within facilities, stronger associations may emerge.
Our results should also be interpreted within the specific context of Papua. Previous work has highlighted that maternal health services in Papua are constrained by systemic challenges, including shortages of skilled personnel, weak referral networks, and the difficulty of delivering services across mountainous and remote areas48. These constraints may explain why the number of hospitals and community health centers was not significantly associated with maternal deaths in our analysis: the presence of facilities does not guarantee functionality, quality of care, or timely access in emergencies. In addition, qualitative research from Jayawijaya district, Papua, found that recognition of maternal and newborn complications was often delayed, and that cultural norms, reliance on traditional birth attendants, and transport barriers limited care-seeking even when services were available49. Together, these findings suggest that reducing maternal mortality in Papua requires strategies that go beyond increasing facility counts to address both structural and sociocultural barriers. Practical approaches include improving the integration of traditional birth attendants into referral pathways, strengthening emergency transport systems, and expanding maternity waiting homes in remote districts as an interim strategy to improve timely access to life-saving care.
Strengths and limitations
This study is the first to examine the combined effects of individual- and community-level healthcare-related factors on maternal deaths in Indonesia. A major strength lies in the use of census data, which provides nationwide coverage and captures a large number of maternal death events across diverse populations, thereby enhancing the representativeness and generalizability of the findings.
Several limitations should also be acknowledged. First, under-reporting of maternal deaths by census respondents is possible, which may have led to an underestimation of the true burden. Second, the census relied on retrospective reporting of deaths that occurred within the previous 3 years, raising the possibility of recall bias, especially for sensitive events such as maternal deaths. Third, the data did not capture pregnancies that did not progress to a live birth, thereby excluding an important subgroup of high-risk women. For example, women with a history of miscarriage, abortion, or stillbirth often face elevated risks in subsequent pregnancies, yet these events were not recorded in the census.
In addition, the census lacked detailed biomedical and clinical variables, which limited the ability to identify the direct medical causes of maternal deaths including antenatal or postnatal care utilization. Important contextual factors such as distance to the nearest health facility, travel time, transportation barriers, number of private clinics, presence of a traditional healer, and referral pathways were also unavailable. A traditional healer is a non-medical practitioner who relies on herbal, spiritual, and belief-based practices, and is distinct from a traditional birth attendant, who assists with childbirth, although both are non-medical providers. These factors are well-recognized determinants of maternal survival, particularly in geographically remote areas such as Papua, and their absence may have led to underestimation of health system barriers. Consequently, our analysis may not fully reflect the role of health system performance in shaping maternal outcomes.
Future research should address these gaps by linking census data with geospatial information, health facility assessments, and biomedical data. Such integrated approaches would provide a more comprehensive understanding of how sociodemographic, cultural, and health system factors interact to influence maternal mortality in Indonesia.
Conclusion
This study demonstrates that maternal mortality in Papua province is shaped by a combination of individual and community factors. Advanced maternal age, nulliparity, unmarried status, low education, and rural residence were all strongly associated with higher risk of maternal death. Although community-level health system indicators such as health worker density and the number of facilities were not significantly associated with maternal deaths, the large contextual variation observed between districts highlights the influence of systemic and geographic barriers.
The findings underscore that reducing maternal mortality in Papua requires interventions that go beyond increasing the number of health facilities or workers. Practical strategies should prioritize improving access and quality of care for vulnerable groups, particularly first-time and unmarried mothers, through adolescent- and youth-friendly health services. For rural and remote districts, strengthening emergency referral systems, investing in maternity waiting homes near referral hospitals, and integrating traditional birth attendants into formal referral pathways are feasible measures that can provide immediate impact. Long-term efforts to retain health workers in remote areas and address structural inequities in education and health access remain essential.
By situating individual risks within the broader rural and remote context of Papua, this study highlights the importance of targeted, context-sensitive strategies to accelerate progress toward reducing maternal mortality and achieving national and global goals.
Funding
This research did not receive any specific grant from funding agencies in the public, commercial, or not-for-profit sectors.
Data availability
The Indonesian Statistical Agency (Badan Pusat Statistik, BPS) provided consent for their data to be used for research and analysis purposes and publish the findings. BPS-provided anonymous census data is available for the public by request at https://pst.bps.go.id.
Conflicts of interest
The authors declare that they have no relevant financial or non-financial interest to disclose.

