Introduction
Globally, geographic maldistribution of health workers exists, favouring urban over rural practice1. The central purpose of health workforce training systems should be to produce graduates with positive intentions and relevant competencies for practising across all communities that a training institution purports to serve2.
The literature strongly suggests rural placements are arguably the strongest training activity for promoting positive intentions and relevant competencies for practising health care in rural communities. A good placement experience results in more positive attitudes to choosing a career in rural practice3-7 and generalist medicine3,5, while rural placements develop clinical skills and medical competencies in medical students more so than urban placements6,8-12. Similar outcomes are identified at the James Cook University (JCU) medical school, where all students undergo at least 20 weeks of mandatory rural placements over the 6-year course (Modified Monash Model categories 3–713) – with more than half of JCU graduates later choosing a career as a generalist or generalist specialist14 and working outside major cities15.
While research demonstrates that exposure to rural clinical placements during medical school – especially extended rural placements – improves clinical skills and likelihood of practising in rural or remote locations later in a doctor’s career, evidence also suggests this experience must be a positive one to promote interest for rural medicine16. The JCU medical school rural placement team promotes the likelihood of students having positive experiences by organising placements the year before to ensure that at least one of the ‘three-legged stool’ approaches is managed – that of accommodation17. The other two legs are appropriate student supervision and clinical experience. All of the chosen sites offer sufficient clinical experience, and placement sites are chosen based on their history of appropriate clinical supervision; however, these remain the more precarious stool legs.
Anecdotally, JCU student placement feedback suggests medical students prefer to be supervised by doctors who have worked in that community for some time, come from the same university and/or have good knowledge of the course requirements. Numbers of JCU medical graduates practising in North Queensland towns have slowly increased since the first graduating cohort in 2005, such that, by 2020, JCU medical graduates were practising in 75% of Queensland towns outside the urbanised South East region having a hospital and/or doctor-led health centre15, often as rural generalists. A rural generalist is defined as a doctor able to provide both primary care and emergency care in a rural or remote community, as well as being able to provide components of advanced specialist care training (AST) for that location18. This more recent influx of permanently based JCU-trained doctors, often with advanced skills, has likely benefited the quality of supervision and clinical training experiences experienced by JCU medical students undertaking rural placements in North Queensland sites.
This mixed-methods study aims to identify specific clinical learning experiences that contribute to final-year JCU medical students reporting a ‘high quality’ rural clinical learning experience during their rural placement, with a focus on whether supervising doctors’ backgrounds and training influences the quality of students’ clinical learning experiences.
Methods
Setting and study design
This study followed a sequential, explanatory mixed-methods design with four focus groups and a one-on-one interview and then a cross-sectional survey conducted with year 6 (final-year) JCU medical students during 2023.
Interview participants, procedure and analysis
Final-year students were informed via their student email addresses about the study and asked if they wished to participate in interviews, following several weeks of promotion through both school and student association Facebook websites. All 157 year 6 medical students received the recruitment email, with 17 students (13 female and 4 male) volunteering to participate. Four semi-structured focus groups (12 students attending in-person and 5 attending online) were undertaken to identify and explore themes associated with clinical learning experiences on final-year rural placements. A single one-on-one online interview was undertaken due to a participant not being able to attend their focus group at the last minute but wanting to participate. All participants provided consent for participating voluntarily and for their data to be de-identified and published anonymously.
The focus groups and interview followed a basic qualitative descriptive design used for exploring specific personal experiences19. All 17 participants had undertaken their 10-week year 6 rural placement at the time of interview (and two having undertaken an extended 20-week year 6 rural placement), and thus were information-rich cases that allowed the research questions to be well explored20.
The interviewers were the authors BM (year 6 JCU medical student), and TW (JCU medical school academic with no formal role with the rural placement program). The primary author, BM, brought a personal ‘insider’ perspective from recently completing a rural placement, which could have influenced the analysis and interpretation of data. In contrast, TW, a JCU academic without direct involvement in the rural placement program, offered a more detached analytical perspective to balance potential biases and assumptions. Together, both authors engaged in continual reflective discussions to mitigate these biases and enhance the study’s credibility, acknowledging that their positions within the JCU community could shape their research insights.
The semi-structured questioning was conducted in three major stages. Initially for the focus group, each student was provided a piece of A4 paper with a large circle and asked to divide the circle into the key experiences (with respective percentages) they felt impacted the quality of their overall clinical learning on their recent 10-week rural placement – either positively or negatively. Then, each student in the group was asked individually to talk about each of these key experiences at their placement site. After all students had described these key clinical learning experiences in depth, a group discussion was undertaken to compare and contrast learning experiences across sites to explore the common underlying factors contributing to the quality of clinical learning on final-year rural placements.
After each focus group and the one-on-one interview, transcriptions were read repeatedly by the researchers BM and TW to develop a high level of familiarity with the data via immersion, then analysed initially using a reflective thematic analysis approach21. This thematic analysis was conducted by BM and TW for investigator triangulation; differences were resolved through discussion. The inductive thematic analysis yielded 11 common themes, which were then simplified into three overarching categories using a deductive approach based on the study by Rotem and colleagues22 finding that medical trainees considered clinical placements to have a positive orientation toward learning if they provided `quality supervision, appropriate levels of autonomy, and appropriate variety and workload'. The sample size was sufficient to allow a ‘theory-saturation point’ to be reached, in which new discussions produced no new information20. Quotes were included in the text if they were considered to be a good representation of concepts held by multiple participants.
Survey participants, procedure and analysis
All JCU year 6 medical students are asked to complete a final-year exit survey in a scheduled teaching session towards the end of an academic year, either on paper or online via a SurveyMonkey email link. In the 2023 exit survey, three extra questions related to clinical learning on year 6 rural placements (developed from the results of the focus group transcript analysis from the first three groups) were included, as well as a question to identify the location of the student’s year 6 rural placement. The main outcome variable was student rating of their clinical learning environment on rural placement. This rating was obtained from the exit survey question ‘Overall, how would you rate your clinical learning environment on your rural placement this year, across all hospital, emergency department and GP sites?’ using a visual analogue scale response. Students used a sliding scale to make an 'X' at the point that best reflected their clinical learning between 0 (‘terrible’) and 100 (‘best possible’), and were provided clinical learning examples, based on focus group findings, to assist rating their experience (Fig1). Evidence suggests visual analogue scales have superior metrical characteristics than discrete scales, allowing a wider range of statistical methods to be applied to measurements22.
The second exit survey question asked students to estimate the proportion of their rural placement spent in the following clinical areas: hospital wards, ED, general practice, outreach clinics and ‘other’. The third extra exit survey question was an open-ended question asking, ‘Was the clinical learning you received on rural placement different depending upon the background of your supervising doctor? Please describe if – and how – your clinical learning on rural varied between locums, registrars, doctors who were graduates of JCU, doctors who were rural generalists (including with Advanced Skills) ...’
In addition, several standard exit survey questions were used in the final analysis: confidence in ‘applying clinical knowledge’ and in ‘clinical skills’, ‘readiness to work in the first internship week at chosen tertiary hospital’ and ‘knowing how to manage common presentations of North Queensland patients’; ‘rurality of hometown where applied to the JCU medical school’; intention to work in a rural area ‘at commencement of medical course’ and ‘at completion of the medical course’; and ‘geographical location expected to practice’ (capital city, regional city, regional town, small rural town, remote community).
Data for the closed questions were coded numerically and then analysed using the Statistical Package for Social Sciences v 23 for Windows (SPSS; http://www.spss.com). Free-text responses were extracted into Microsoft Word for content analysis. The main outcome variable ‘quality of clinical learning on rural placement’, with student scores of 0–100 on a visual analogue scale, were dichotomized into 0–84 and 85–100 for analysis (with ≥85 proposed as the ‘high quality clinical learning placement’ category). For the bivariate analysis, two-sided t-tests and χ2 tests were used to determine statistically significant associations (p<0.05) between the dichotomised main outcome variable with all dependent variables (Table 1). Multivariate analysis used binary logistic regression to identify the significant independent predictors of a ‘high quality’ rural placement clinical learning (Table 2), involving all variables found to have a strong statistical association (p<0.10) in the bivariate analysis.
Content analysis of the free-text responses involved an iterative process to categorise each student’s perceptions of the quality of teaching received from the various clinician groups (e.g. registrar, locum, rural generalist, medical super) (Table 3). This categorisation process was based on the key findings of the qualitative research relating to the quality of teaching from doctors: ‘willingness to teach (either formally or opportunistic)’, ‘allowing appropriate levels of autonomy with feedback’, and ‘knowing students’ scope of practice and placement learning objectives’. Every student comment was deductively analysed to identify the proportion of positive responses across each doctor grouping with respect to these three categories.
Table 1: Variables associated with James Cook University medical students (n=71) experiencing ‘high quality’ clinical learning (≥85/100 rating) on their final-year rural placement in 2023
| Variable | Response | p-value | |
|---|---|---|---|
| 0–84 out of 100 rating of rural placement learning (n=38) | ≥85 out of 100 rating of rural placement learning (n=33) | ||
| MMM category of placement site | 4.9 | 5.4 | 0.124 |
| Confidence in applying clinical knowledge, rated 1 (very poor) to 5 (very high) | 4.0 | 4.4 | 0.024* |
| Confidence in clinical skills, rated 1 (very poor) to 5 (very high) | 4.1 | 4.4 | 0.073 |
| Confidence in knowing how to manage the common presentations of North Queensland patients, rated 1 (very poor) to 5 (very high) | 4.2 | 4.6 | 0.036* |
| Confidence in being ready to work in first internship week, rated 1 (very poor) to 5 (very high) | 4.2 | 4.5 | 0.211 |
| Placement not on the populated North East Queensland coast (ie placed in towns >100 km away from Mackay to Mossman coast), % | 34 | 61 | 0.026* |
| Intended to work in a rural area when entered the course, % | 78 | 59 | 0.143 |
| Intend to work in rural area at completion of course, % | 85 | 89 | 0.685 |
| Changed intention towards working in a rural area, % | 11 | 30 | 0.091 |
| Geographic region (MMM) will most likely practice medicine, metropolitan (1) to small remote (5) | 2.1 | 2.4 | 0.385 |
| Percentage of time spent in hospital wards | 36.3 | 33.9 | 0.622 |
| Percentage of time spent in ED | 41.7 | 58.6 | 0.002** |
| Percentage of time spent in general practice | 8.1 | 4.5 | 0.172 |
| Percentage of time spent in outreach clinics | 3.2 | 3.4 | 0.898 |
| Percentage of time spent in other locations (eg telehealth consults) | 3.4 | 2.3 | 0.542 |
*p<0.05, **p<0.01, ***p<0.001.
MMM, Modified Monash Model.
Table 2: Binary logistic regression analysis identifying predictors of final-year James Cook University medical students having a ‘high quality’ (self-reported score of 85–100/100) clinical learning experience on their rural placement in 2023
| Predictor | Sample (n=54†) n | Had a ‘high quality’ clinical learning experience (n=27) n (%)¶ | Prevalence odds ratio (95%CI) | p-value | |
|---|---|---|---|---|---|
| Proportion of time (%) spent learning in ED | 0–49 | 33 | 12 (36) | 9.4 (2.0–45.5) | 0.005** |
| 50–100 |
21 |
15 (71) | |||
| Confidence in managing the common presentations of North Queensland patients | ‘OK’ to ‘High’ | 29 | 10 (34) | 8.5 (1.9–38.9) | 0.006** |
| ‘Very high’ |
25 |
17 (68) | |||
| Placement not on populated North East Queensland coast (ie in towns >100 km from Mackay to Mossman coast) | No | 28 | 10 (36) | 4.1 (1.1–15.5) | 0.041* |
| Yes |
26 |
17 (65) | |||
*p<0.05, **p<0.01, ***p<0.001.
† Only data of students with no missing values for predictors accepted into the model were analysed. Model predicts 85% of 0–84 category and 67% of ≥85 category.
¶ % denotes the ‘within-category’ proportions of students who rated the quality of their clinical learning on placement from 85 to 100 out of 100 across categories within the three independent variables.
CI, confidence interval. ED, emergency department.
Table 3: Content analysis of 71 final-year James Cook University medical student responses to the open-ended question, ‘Was the clinical learning you received on rural placement different depending upon the background of your supervising doctor? Please describe if – and how – your clinical learning on rural varied between locums, registrars, doctors who were graduates of JCU, and doctors who were rural generalists (including with Advanced Skills) ...
| Clinical teaching on placement | Student comments |
|---|---|
| Senior doctors (medical super, consultants) |
|
| JCU graduate doctors |
|
| Rural generalists |
|
| Junior doctors and registrars |
|
| One-off and returning locums |
|
| Experienced similar teaching from various supervising doctors on rural placement |
|
AST, Advanced Specialised Training. IDC, indwelling urinary catheter. JCU, James Cook University. RMO, resident medical officer.
 Figure 1: Visual analogue scale question used in the 2023 James Cook University medical student exit survey.
Figure 1: Visual analogue scale question used in the 2023 James Cook University medical student exit survey.
Ethics approval
Ethics approval was granted by JCU Human Ethics (H6921).
Results
Survey
Seventy-one out of 157 JCU year 6 medical students completed the survey in the 2023 graduating cohort (45% response rate), with 33 (47% of participants) reporting their overall rural placement experience as 85 or more out of 100 (a ‘high quality’ clinical learning experience), with 39% rating 60–84 and 14% less than 59.
A ‘high quality’ clinical learning experience’ (≥85/100) was significantly associated with ‘confidence in applying clinical knowledge’ (p=0.024), ‘confidence in knowing how to manage the common presentations of North Queensland patients’ (p=0.036), placement not being on the populated North East Queensland coast (ie placed in towns >100 km from the coast between Mackay and Mossman) (p=0.26) and more than 50% of time spent learning in the ED (p=0.002) (Table 1).
Binary logistic regression analysis identified the predictors of final-year JCU medical students having a ‘high quality’ clinical learning experience on their rural placement as spending 50% or more of their learning in ED (p=0.005; prevalence odds ratio (POR) 9.4), ‘very high’ confidence in knowing how to manage the common presentations of North Queensland patients (p=0.006; POR 8.5) and being placed in towns more than 100 km from the populated North Queensland coast (from Mackay to Mossman) (p=0.041; POR 4.1) (Table 2).
Interview themes
Eleven key themes were identified in the initial component of the interviews, when each student was provided A4 paper with a circle and asked to divide the circle into the key experiences (with respective percentages) impacting their clinical learning on the year 6 rural placement (Fig2). Nine of the 11 themes fit under Rotem et al’s key factors impacting clinical learning23:
- appropriate levels of autonomy under supervision – ‘doctors provide appropriate levels of autonomy’ (24%); ‘doctors know students’ scope of practice and placement learning objectives’ (2%)
- quality teaching supervision – ‘doctors willing to teach’ (20%); ‘doctors provide formal teaching sessions’ (8%); ‘doctors provide opportunistic teaching’ (5%); ‘good teaching from non-medical staff’ (5%)
- appropriate variety and workload – ‘variety of the roster across ED, GP and outreach clinics’ (12%); ‘patient variety, number and willingness to be examined’ (12%); ‘access to local workshops & simulated clinical presentations’ (3%).
A fourth category, student factors, was created for the final two identified themes (‘sharing placement with medical student peers and other allied health students’ (7%); ‘teaching learned knowledge and skills to more junior medical students’ (3%)). After identifying the key factors underlying a highly satisfactory clinical learning experience, discussions then focused on in-depth understandings of each factor, grouped under the four overall key themes, summarized in the following text.
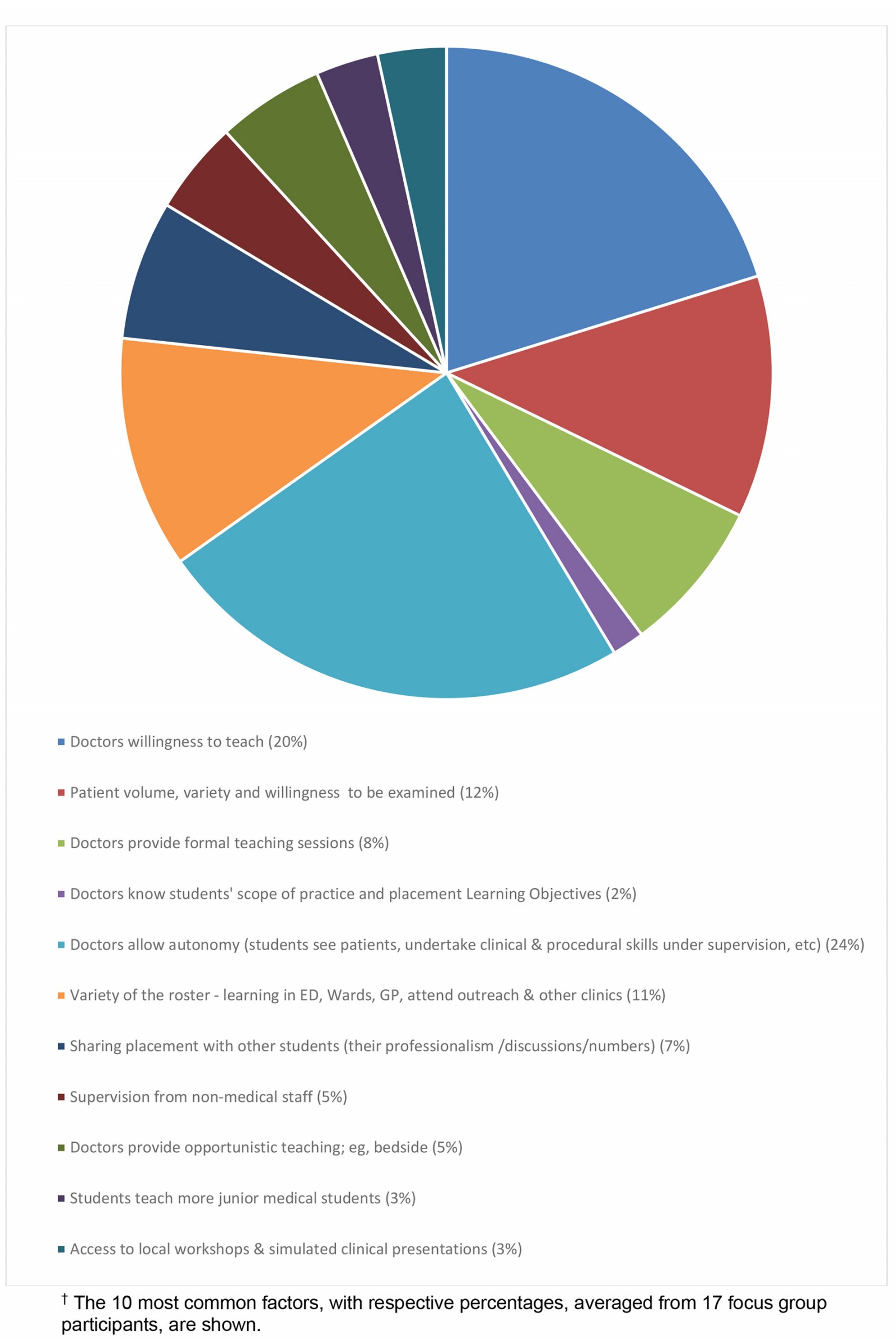 Figure 2: Factors identified by final-year James Cook University medical students as impacting their clinical learning on rural placement.†
Figure 2: Factors identified by final-year James Cook University medical students as impacting their clinical learning on rural placement.†
1. Students given appropriate levels of autonomy under supervision
There were fewer clinicians overall (especially in more remote placements), but most placements had sufficient numbers of highly trained and rurally experienced doctors to allow students the opportunity for autonomous practice under supervision and to practise managing patients’ conditions independently, procedural skills and work-ups, give presentations, and receive significant feedback.
The ED was a key place for training, where students were more likely to see interesting and varied cases, and have the opportunity to become a valued part of the clinical team. In the words of one student participant, ‘Important to have opportunities [in ED] to improve your procedural skills, and to be involved in the team when there's sort of resuscitations and things like that – a real key point’.
The EDs also experience ‘quiet’ periods where supervisors have time for unstructured teaching by going through previous cases. As one student participant said, ‘Rural ED doctors teach a lot of things they don’t teach in medical school’.
Placements with lots of permanently based senior doctors (and nurses) means more time together to establish a strong supervisory relationship (as opposed to locums, who often are in the placement for 1 or 2 weeks), and many permanent staff give the placement an established ‘structure’ that makes it easy for medical students to ‘slot in and be taken care of’, assisting students to establish a level of autonomy on wards and in ED.
Negative aspects
There is less opportunity for autonomous practice under supervision in smaller, more remote placements that are staffed mostly by locums. According to one student, ‘Once the permanent doctor [GP] left there was no point in going to the GP anymore as locum doctors didn’t understand our role despite being told’.
2. Doctors willing to provide quality teaching/supervision
This theme includes doctors willing to teach and establish a positive supervisor–student relationship, doctors providing formal and opportunistic teaching sessions, and teaching from non-medical staff.
A positive and supportive teaching-learning relationship was often built more quickly with JCU graduate doctors as they know the scope of year 6 JCU students’ competencies and their placement learning objectives, and have a previous shared experience of attending the same medical school. One student said, ‘Because the majority of the junior doctors are all ex-JCU grads, they pretty much gave us independence of practice. So, they had us go do whatever – see patients by ourselves, go put in a cannula, do this and that’.
Rural generalist supervisors were willing to teach and get students involved as they were passionate about rural practice and understand the community and rural medicine.
Negative aspects
‘Friendship fatigue’ was a negative experience in placements where many medical students, junior doctors and registrars rotate throughout the year. Small placements with few doctors could lead to missed learning opportunities, such as when no senior doctors were present (‘Didn’t have a chief doctor, so serious issues all had to go to an external doctor), spending significant time in a particular ward (‘Got stuck in ED, very busy, and no-one else to help. I had to come in for weekends’) and undertaking more mundane or clerical tasks such as clearing out a backlog of discharge summaries, running telehealth clinics, which ‘a nurse could do’. Leadership/workplace culture and issues at the placement site sometimes affected staffing levels, which in turn affected teaching opportunities. As one student said:
And that [power struggle] sort of creates a work environment where a lot of the doctors aren't happy with their rostering. And people are getting burnt out and then sort of tempers flare. And then there’s this downstream effect that can affect the juniors to a certain degree, but there are some doctors who are really affected, and it can be a pretty unpleasant shift when you're with them, because there's obvious sort of tension between then and [management]. It's not like a glaringly adverse experience, but I think it trickles down because it affects the doctors and affects the nurses.
3. Students experience appropriate clinical variety and workload
This theme includes seeing a variety of rural patient presentations across a range of clinical areas.
Being placed in ED, wards, attending visiting specialty clinics and travelling to outreach clinics increase students’ variety of clinical learning and patient exposure, as well as contributing to a more interesting and engaging placement experience. ‘Getting good variety between ED and the wards – getting the experience of both of them’, said one student.
Rural patients were generally ‘more happy for students to have a go’. More access to patients means more exposure to learning opportunities, seeing strange cases and ‘real world’ procedures not experienced in medical school (such as resuscitation).
Another positive aspect was experiencing a wide range of patient presentations. One student said:
Because where Mt Isa is, the catchment area that it covers, it has a very diverse range of presentations. So yeah, we had, you know, we've got cattle stations around, we've got mining camps as well, and we cover everything from pretty much the Gulf all the way down to the [Queensland] border. So, we would just literally transfer patients every single day or had someone coming to us every single day – we got a big range of stuff there.
Negative aspects
Patient numbers in some small remote placements are variable throughout the year (‘Certain times of the year there are no patients’) or patients are sent elsewhere for procedures, such as in relation to birthing. Sometimes students were placed for too much time in ED: 'So yeah, there's a lot of people in hospital, but it was pretty good, because we had our own section – ED – that we kind of could rule. But, like I maybe would have appreciated some more time in the wards, just to get some paper-based experience for next year’.
4. Student factors
Clinically confident and competent students were more likely to embrace autonomy, see patients independently, ask questions of doctors, apply their knowledge and skills, and be more involved in general. Confident and competent students were also more likely to want to teach younger students who may also be on placement. One student said, ‘The only thing is, we didn't teach any junior medical students because we were by ourselves in the ED, which was good as no-one was in our way, but a bit annoying’.
Students need initiative to get involved in additional clinical learning opportunities with allied health staff and participation in community outreach. Students who engage in the community outside of the hospital learnt more about the region and consequently its demographics and epidemiology, and to develop better rapport with patients and staff – and had a better mindset when starting their placement day.
Smaller, more remote placements often involve out-of-hours social events that assist students to build relationships with local health staff – such as dinners at the senior medical officer’s house and trivia nights with other doctors at the local hotel.
Negative aspects
The presence of too many students can impact learning opportunities, and not all remote communities have as many opportunities for community engagement and/or social activities with health staff – which often depend on number and permanency of workforce. More permanent staff, as opposed to locum staff, tend to invite students to social activities and for weekend excursions,.
Content analysis
Content analysis of the 71 responses to the open-ended survey question (asking if the quality of learning varied depending upon the background, skills and experience of placement doctors) identified that students did experience very varied teaching from doctors, and that they strongly enjoyed teaching from JCU graduate doctors (n=21) because they were familiar with the scope of practice expected of year 6 students and their rural placement learning objectives, and from experienced rural generalist doctors (n=15), especially those with Advanced Skills Training. Being placed with several rural generalists having different Advanced Skills was particularly advantageous. All student comments are listed in Table 3, with some typical comments being:
Variable [teaching] depending on the confidence of the senior supervisor. Often the more rural experience the doctor had, the more trust in students they had.
Each doctor, but particularly rural generalists, had their own experiences and special interests, allowing for a nice variety of clinical learning.
Graduates from JCU knew what we were doing and what would benefit us from placement. They were able to tailor specific teaching sessions to our current learning needs.
JCU grads were aware of our skill set and abilities and allowed us to maximise our learning potential as 6th year students.
There were less positive comments on teaching by visiting locum doctors (n=16), in particular those visiting the community for the first time. While there were positive comments on locums who regularly visited a placement town (‘Best teaching via regular locum doctors who would visit [placement town] for 1/4 weeks per month’), locum teaching was described several times as ‘hit and miss’, with specific comments around locums being less willing to teach and provide feedback as they were temporary staff focused on the work at hand rather than teaching, and not knowing a year 6 JCU students’ competency level and placement learning objectives:
Did not have any permanent doctors in [placement town]; completely locum based. They did not know our scope of practice or were very supportive of students. There was no teaching provided throughout the placement. Sometimes there would be a ward round but more often there wasn't. Whilst locums gave us autonomy to see patients freely, they often did not give feedback on how we could improve presentation, management, investigations or anything. Additionally, no teaching on procedural skills. Would have been better with permanent doctors who you could build rapport with.
Had some very poor locums that did not have much faith in medical students compared to some of the local senior doctors and experienced locums that were very happy for us to mostly work independently. Most doctors were locums, did not know our scope of practice and had not previously worked with JCU students.
Discussion
This is the first study to explore aspects of local rural placement site supervision and clinical learning experiences that influence the perceived quality of medical students’ clinical learning. Of particular interest is that this research occurred at a time when the local rural medical workforce is increasingly being staffed by rural generalist doctors, many with advanced rural skills and many of whom are also graduates of a more recently established rural medical school in the region.
These results align with prior studies that emphasise the positive impact of immersive rural placements on student outcomes, such as increased likelihood of choosing careers in rural practice and/or primary care post-graduation24-26. Similar to Smith’s (2019) understandings27, our findings also underscore the importance of hands-on learning opportunities and adequate supervision in enhancing health educational outcomes. However, our study extends this literature by quantifying the impact of placement duration in EDs and student confidence, which have been less explored in previous research.
Overall, this study suggests that four overall factors contribute to JCU medical students having a ‘high quality’ rural clinical placement experience: appropriate levels of autonomy, doctor’s willingness to teach and supervise, appropriate clinical variety and workload, and student-related factors. Similar to findings of Avegno et al28, our results suggest that high-value clinical learning is significantly associated with placements that allow substantial ED exposure. The fast-paced and diverse ED environment offers students a breadth of acute, hands-on experiences not commonly found in other departments. This aligns with studies by Satran et al8 and Woolley et al15 that highlight the role of the ED in enhancing critical thinking and practical skills through exposure to a wide array of patient presentations that require rapid clinical decision-making. In addition to this, the ED fosters an increased sense of responsibility and autonomy among students – factors that are instrumental to the development of students' confidence in their clinical abilities29. Supervisors also placed a higher level of trust and dependence on students in the ED setting, which may account for the increased satisfaction and perceived quality of learning identified in our study. This trust is essential for students’ feeling of being valued members of the healthcare team, which is known to positively influence their educational experience and development of professional identity29.
The finding of more geographically isolated placements being rated higher overall is in line with GP registrar research30. This is likely for a variety of reasons, including smaller hospitals periodically having quiet times where senior doctors are available to teach, supervise and provide feedback to students. As one student commented, ‘I found the ED consultants provided the most insightful feedback and had the most time to invest into teaching as it was a small centre, whilst the Regs [registrars] and RMOs [resident medical officers] were quite busy’. Other reasons may involve the remoteness aspect of the placement leading to reduced numbers of clinical staff (but still having a core number of highly experienced rural doctors) and thus creating more autonomy for students to practise independently, better connection with fewer staff and increased rural patient willingness to be seen by student doctors.
Both the interviews and survey findings identified that final-year medical students preferred a primarily ED-based roster but with a variety of experiences in other wards, GP rooms and outreach, and visiting specialist clinics. It is likely that spending significant time in ED benefited students by allowing them increased opportunity to establish trust with the regular doctors, leading to more autonomous practice and greater opportunity to practise procedural skills, undertake work-ups and give patient presentations back to the doctor. Additional opportunities to see ward-based cases and attend visiting clinics and outreach services also provided unique experiences, with a variety of patient presentations and consequent management.
Also significantly, both the interviews and survey findings identified that many students felt that their best clinical teachers were JCU graduates. Specifically, students often described JCU graduates as being very good at creating supportive learning environments, understanding their placement learning objectives and their scope of practice, as well as having a range of rural medicine knowledge and skills (with many being rural generalists and many with Advanced Skills Training). It may be that more understanding of students’ learning objectives and scope of practice would tend to facilitate a teaching relationship more quickly, which would lead to more student autonomy earlier during placement, and thus to more opportunities overall for hands-on experience and tailored feedback, as well as opportunistic teaching sessions tailored to the students’ competency levels.
Additionally, many students felt rural generalist doctors were generally very good clinical teachers, as they well understood rural medicine and were passionate about rural practice, making them more willing to teach both standard and advanced rural medicine skills. Some placement sites had several rural generalist supervisors, each with varying experiences and special skills or interests, which furthered teaching opportunities for students by providing greater variety and depth in clinical learning at these sites. As with JCU graduate supervisors, rural generalist supervisors facilitated active student involvement and autonomy in patient management and practical learning. For these reasons, in conjunction with a smaller number of clinical staff in many geographically isolated placements, students had more autonomy in the clinical team.
Students’ teaching experiences were often different with locum doctors who, due to the transient nature of their work, did not always have time or motivation to establish good teaching relationships with students, or have the level of experience practising in rural communities. The content analysis and interviews identified many students had experiences where the locums did not understand the scope of final-year JCU medical students or take the time to teach or supervise them; rather, they were more focused on completing their own work. This, however, varied between locums based on their background and experience. For example, ‘regular’ locums – who usually returned to do locum work at the same placement site – were often perceived as still able to build supervisory relationships with the students as they often had previous experience with JCU students, as well as more knowledge of common local cases and the local community. Given that a significant number of rural Australian communities still rely on overseas-trained and locum doctors to provide adequate medical coverage31, these findings suggest medical student placements in smaller more rural and remote towns should be selected with some consideration of providing a mix of permanent and locum doctors to ensure the quality of medical student clinical learning is not affected.
Good rural placement experiences are known to result in medical students having more positive attitudes to choosing careers in rural practice and generalist medicine, as well as development of clinical skills and medical competencies. This study identifies that good learning experiences on rural placement can be promoted by choosing sites staffed by rurally experienced clinicians with time to teach and with knowledge of students’ scope of practice and specific placement learning requirements. Further, the student placement roster needs to include a variety of clinical training environments but also opportunity for longer term stays – particularly in the ED – so students develop trusting learning relationships with supervisors and other staff to become both members of clinical teams as well as experience appropriate autonomous practice.
Limitations
A limitation of the study is the survey’s 45% response rate; therefore, selection biases may potentially influence study findings. Conclusions are ultimately based on small numbers and from a single student cohort of a regionally located medical school. Also, 7 out of the 71 students who completed the survey and 2 out of 17 focus group participants had undertaken a 20-week final-year rural placement rather than the standard 10-week placement. However, this is unlikely to have influenced findings to any significant degree as this equates to approximately 10% of the sample, and clinical learning experiences would be similar to those of all participants.
While the study should be reproducible in other Australian medical schools, final-year rural placements by JCU students are likely to involve a high proportion of supervision by rural doctor graduates from their own medical school, which may not be the case for students training in other regions. Additionally, the generalisability of these findings may be somewhat limited by the unique geographical and cultural context of North Queensland. The core principles identified, however, such as the value of stable, experienced supervision and the benefit of specific types of clinical exposure, can be adapted to other rural settings nationally and internationally, particularly in regions where healthcare access mirrors that of North Queensland. Future research should explore the dynamics identified in this study across multiple rural settings and with larger participant pools, to validate and extend our findings.
Conclusion
The study findings suggest the key to JCU medical students having ‘high quality’ clinical learning on rural placements is by developing supportive learning relationships with senior, permanently based rural doctors who know their scope of practice and specific placement learning requirements, and experiencing a diverse roster across hospital, GP and outreach clinics but also with significant placement time in the ED. By focusing on these key aspects of rural placements, program coordinators can more effectively plan, develop and support training sites and thus improve future placement experiences for student and junior doctor trainees. These enhancements may improve the immediate educational experience and promote greater interest in rural and generalist medical careers among trainees, contributing to more positive outcomes in rural healthcare delivery.
Acknowledgements
The authors thank the 2023 cohort of year 6 JCU medical students for participating in this study.
Funding
No funding was received for this study.
Conflicts of interest
The authors report no conflicts of interest.


