Introduction
Indonesia is one of the largest archipelagic countries in the world, with a total land area of 1,916,862 km2 as well as 3,257,483 km2 of water1. The archipelago consists of 16,771 islands, including 111 small and outer islands2. According to data from Statistics Indonesia (Badan Pusat Statistik, BPS) for 2022, the Indonesian population was 275.77 million, with constant annual growth3. Indonesia is a pluralistic country that is highly harmonious and rich in cultural diversity. It is known by its national motto bhinneka tunggal ika, which means ‘unity in diversity’. It is home to more than 300 ethnic groups and 1340 ethnic communities, and it officially recognises six official religions: Islam, which is the predominant religion (87.2% of the population), Protestant Christianity (6.9%), Roman Catholicism (2.9%), Hinduism (1.7%), Buddhism (0.7%) and Confucianism (0.05%). People from these various ethnic and religious backgrounds have a rich tapestry of cultures spread across the archipelago4, preserving traditions that emphasise not only human relationships but also harmony with the surrounding natural environment5.
This diversity is unified under a fundamental set of principles known as Pancasila. The values of Pancasila are a solid moral foundation based on universal principles: belief in one supreme God, humanity, unity, democracy and social justice6. Pancasila reinforces the spirituality in healthcare services, thereby fostering meaningful relationships between healthcare providers and patients. Furthermore, in the context of social justice, Pancasila promotes the equitable provision of healthcare services for all segments of society, regardless of economic status, ethnicity, religion and geographic location. Every citizen has the right to equal access to healthcare facilities and to receive quality health services7.
The 2030 Agenda for Sustainable Development Goals (SDGs) aims to promote transformative changes toward sustainable development based on human rights and equality. These goals emphasise the integration of social, economic, and environmental development while ensuring that no individual is left behind. SDG 3 is about ensuring the good health and wellbeing of all individuals at all ages. This goal is to be achieved by providing access to quality basic healthcare services and by supporting the development, training and retention of healthcare professionals, particularly in developing countries, least developed countries and small island developing states8.
Indonesia faces several significant public health challenges. Between 2019 and 2021, 7389 maternal deaths were registered. The primary causes were hypertension, obstetric haemorrhage, and various complications during pregnancy and childbirth. The majority of pediatric fatalities (80.4%) transpired during the neonatal phase. The most prevalent causes of mortality in this age group were pneumonia and diarrhea. Furthermore, Indonesia has the second highest burden of tuberculosis globally, following India. The incidence rate is 385 cases per 100,000 population, with a mortality rate of 49 per 100,000 population. Additionally, a significant surge in HIV/AIDS cases has been observed in comparison to the peak of the COVID-19 pandemic period (2020–2021)1. Communities living in insular and remote regions are particularly vulnerable to severe illness, especially in the absence of immediate medical intervention or the inability to access advanced healthcare facilities.
Communities residing on small islands tend to encounter suboptimal health standards due to several factors, including limited access to clean and safe water, inadequate availability of nutritious sustenance and restricted healthcare services9. Furthermore, these regions frequently face natural hazards such as earthquakes, severe weather conditions, high transportation costs, difficulties in implementing community-based health programs, and the absence of healthcare workers in some villages10. Small islands have also been observed to serve as disposal sites for waste and as recipients of marine debris11. It is evident that the level of public awareness and understanding of chronic diseases remains limited. The high incidences of arboviral diseases, such as dengue fever, chikungunya, malaria and diarrhea, in island regions is primarily attributed to insufficient access to potable water, and deficient sanitation facilities12. Moreover, island communities often encounter disparities in healthcare services due to deficiencies in healthcare personnel and inadequate infrastructure13.
The Indonesian government has made significant endeavours to enhance public health and ensure the provision of equitable healthcare services accessible to all segments of the population. A total of 9993 officially recognised community health centres (puskesmas), from which the population seeks primary health aids, are spread across 514 regencies and cities in Indonesia. These community health centres fulfil a pivotal role in the Indonesian healthcare system, acting as the primary entry point for individuals seeking healthcare services. They address various health needs, including health promotion, disease prevention, early detection and diagnosis, basic care and treatment, and referrals and coordination14. The Indonesian government, through the auspices of the Ministry of Health, is committed to the enhancement of community health centre services and referral systems in order to ensure optimal access to quality healthcare services for all citizens of the country15.
The Sangihe Islands Regency is one of the outermost regions in Indonesia, sharing a maritime border with the Philippines. Tahuna, the regency capital, is located 8 hours by sea from the provincial capital. The region is served by one regional hospital, one primary hospital and 14 community health centres located on the mainland. Additionally, three community health centres are located on small islands in this regency: Marore, Kahakitang and Nusa Tabukan. Despite the provision of inpatient facilities at these three community health centres, patients may need referrals for further examination or hospitalisation, necessitating sea travel of approximately 3–5 hours by fishing boats to reach the nearest hospitals, or a 19-hour journey by large vessel.
The implementation of the referral system has been generally successful in urban areas, supported by the existence of government policies. However, systematic assessments of the referral system in isolated and island areas, with a view to deriving insights about realities, have yet to be adequately conducted. This study attempts to explore the intricacies of the referrals process, proffering interventions designed to enhance the referrals of patients from the community health centres situated within small islands and within border regions to regional hospitals.
Methods
This study employs an implementation research design, which is typically used to assess the implementability of a specific program, to understand how an implementation works or fails, and to identify various techniques for enhancing the implementation success16. This approach has wide applications within the health sciences, such as policies, programs and practices. It also studies different aspects of implementation, including the facilitators and barriers, the implementation process and the outcomes, guided by the Standards for Reporting Implementation Studies17,18.
A specific method is required to systematically investigate the implementation of the referral system from the community health centres on small islands to regional hospitals. The intervention mapping approach, which allows for a more systematic research process, is deemed suitable for addressing the research questions and objectives19,20. The intervention mapping framework comprises six structured stages (Fig1), with each stage building upon the previous to ensure the continuity and sustainability of the overall process. The active involvement of the target population is critical to the successful adoption, implementation and long-term maintenance of the protocol. The target population for this study will include a range of key actors such as stakeholders, participants, facilitators, and other individuals who may be directly or indirectly engaged in the program21.
In the first stage of the study (the needs assessment), the needs related to the referral system at community health centres will be assessed using both quantitative and qualitative research methodologies. In the second stage (matrix development), the findings from the first stage will be disseminated through focus group discussions (FGDs) involving key policymakers and health providers. The feedback from the participants is essential for developing charge plans, setting objectives and constructing a matrix of priority changes. The third stage of the research process (theory-based methods and practical strategies) involves conducting a literature review to identify theory-based methods and practical strategies that can be used to optimise the referral process at puskesmas, These methods and strategies are based on a priority change matrix agreed upon in the second stage of the study. The fourth stage consists of designing a practical strategy program derived from the third stage and discussing it with experts in the relevant field. In the fifth stage, a brainstorming session will be conducted with the primary healthcare services division of the district health office. The sixth stage involves the evaluation of the acceptability, appropriateness and feasibility of the program based on the perceptions of key decision-makers. The stages of this research are detailed in Table 1.
The study is to be conducted in Sangihe Islands Regency, North Sulawesi Province, Indonesia. The research will focus on three community health centres on three small islands: Kahakitang, Nusa Tabukan and Marore. Figure 2 shows a map of the research site. The study is scheduled to be conducted over a period of approximately 12 months.
Table 1: Research stages for implementation research on challenges associated with the referral system using the intervention mapping approach, Sangihe Islands Regency, North Sulawesi Province, Indonesia.
| Research stage | Duration | Purpose | Methods | Results |
|---|---|---|---|---|
| 1. Needs assessment | 4 months |
Identify the supporting factors of implementation. Identify the actors involved in implementation. Identify the barriers faced by beneficiaries and implementers. Identify the role of nurses in primary care. |
Quantitative Qualitative |
Perceptions of implementers and beneficiaries regarding the supporting factors, challenges, and team involved in the implementation of referrals |
| 2. Matrix development | 2 months |
Present the results of the first step. Discuss priority issues. Set priority change goals. Develop a change matrix. |
FGDs | Change matrix Objectives of priority change |
| 3. Theory-based methods and practical strategies | 2 months |
Set an intervention based on the problems faced to achieve the change goals. Prepare the intervention materials. |
Literature review | An intervention addressing priority issues |
| 4. Program preparation | 2 months |
Convey the change objectives and matrix agreed upon with the implementer in the second stage. Discuss the interventions recommended by researchers. Elicit expert ideas and opinions. Discuss the methods and strategies for implementing the intervention. |
FGDs | Methods and strategies appropriate to the context |
| 5. Adoption and implementation plan | 1 month | Obtain inputs, suggestions, and opinions regarding the intervention plan prepared in the previous stage. | FGDs | Consensus on the intervention plan |
| 6. Evaluation plan | 1 month |
Increase the knowledge of health workers on policies that support the implementation of the intervention. Explain the intervention that has been prepared in the previous research stage. Conduct an antecedent assessment of the intervention that has been described. |
Quantitative | Acceptability, appropriateness, and feasibility |
FGD, focus group discussion
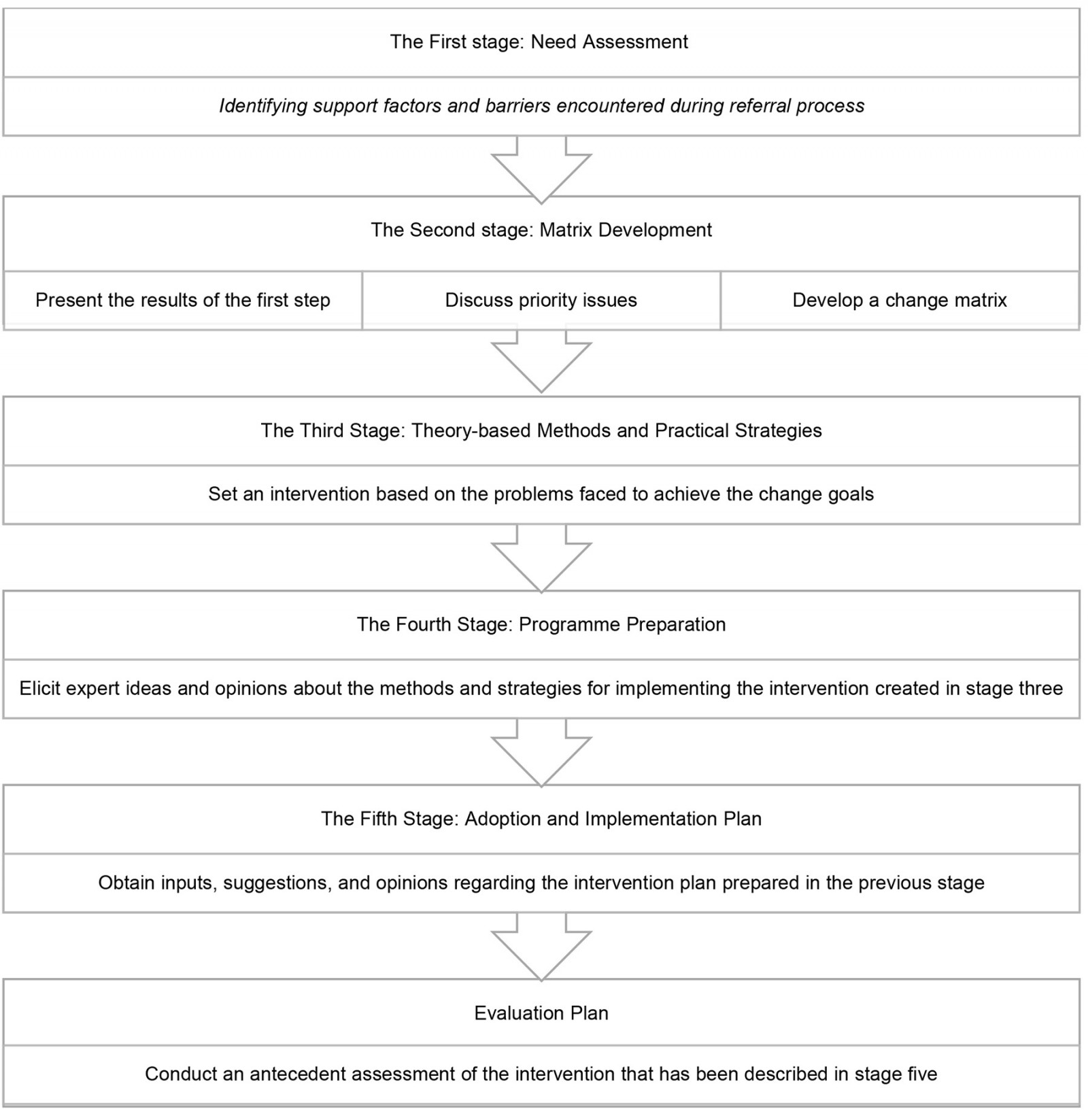 Figure 1: Research stages based on intervention mapping.
Figure 1: Research stages based on intervention mapping.
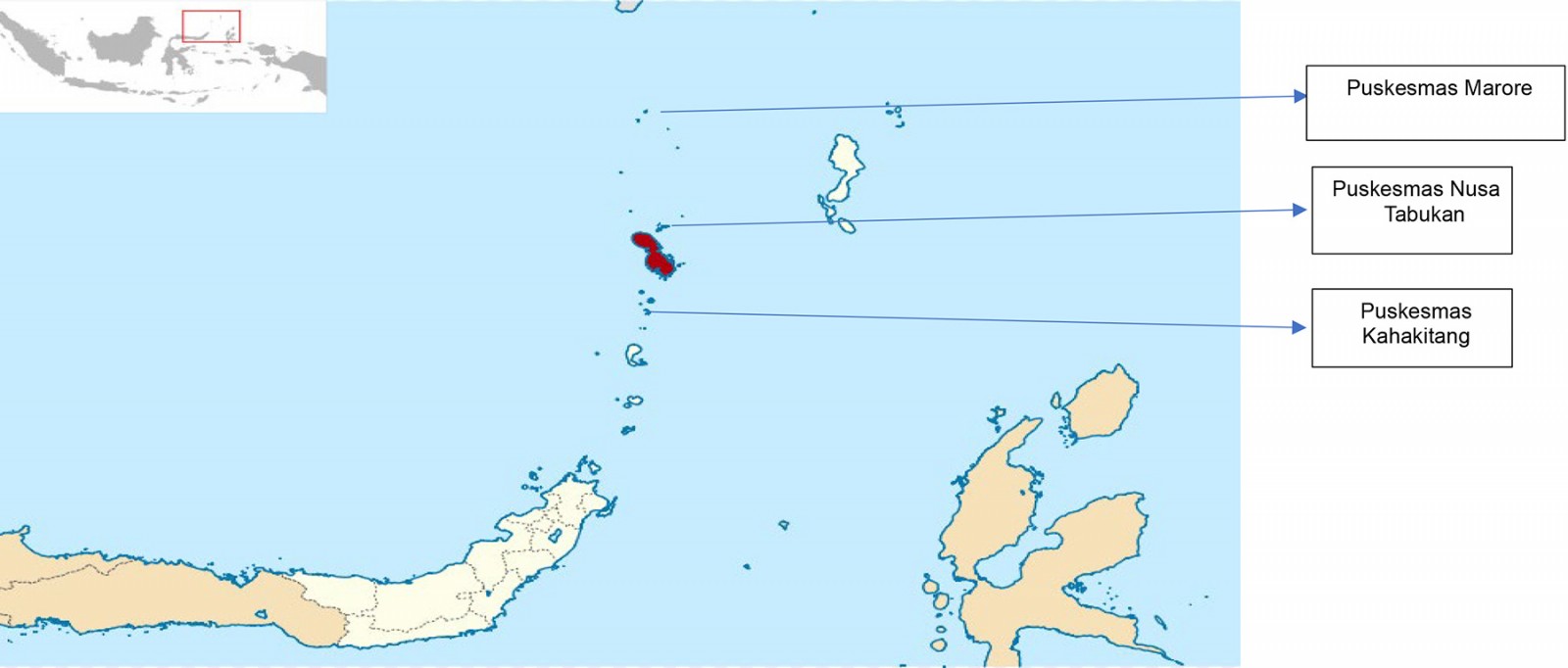 Figure 2: Study site map: Kahakitang, Nusa Tabukan and Marore, Sangihe Islands Regency, North Sulawesi Province, Indonesia.
Figure 2: Study site map: Kahakitang, Nusa Tabukan and Marore, Sangihe Islands Regency, North Sulawesi Province, Indonesia.
Stage 1: Needs assessment
Research design
The first segment of the present study is oriented towards the identification of needs and the exploration of the critical variables of referrals, involving both intervention beneficiaries and implementers. The collection of data from the target participants will be conducted using a structured questionnaire. A quantitative research design will be employed to explore the facilitating factors of referral implementation based on patients’ perception. Additionally, a qualitative research design will be applied to identify the barriers to referral implementation faced by both intervention beneficiaries and implementers, as well as those who plan the referral interventions.
Participants
The target population consists of healthcare professionals, heads of community health centres, patients on the three small islands where the study is going to be conducted, and patients of the three purposively selected community health centres.
The collection of qualitative data will be achieved through FGDs with health workers and individual interviews with the heads of these community health centres. In order to participate in the FGD, it is necessary for the participants to meet the following criteria: they must be professional nurses or midwives, as evidenced by a valid and active registration licencee; they must have worked at a community health centre for more than 1 year; and they must have experience in facilitating patient referrals. Participants in in-depth interviews must serve as the head of a community health centre (puskesmas), as proven by an official appointment letter issued by the Regent of the Sangihe Islands Regency.
The focus of quantitative data is on patients, specifically those who have utilised referral services from community health centres. The population from which the study will draw participants will be identified through referral data reports collected from each community health centre, which will serve as the study’s primary data source. Based on the available data, a sample size calculation will be undertaken in order to determine the number of participants needed to ensure statistical validity and representativeness. Participants in the quantitative study must meet the following criteria: be an adult aged 18–60 years; have received a referral within the past 6 years; and be able to communicate effectively, both verbally and in writing, in the Indonesian language. The sample size for this study will be estimated using StatCalc from Epi Info 7 (US Centers for Disease Control and Prevention; https://www.cdc.gov/epiinfo/cloud.html). The estimation was based on the following assumptions: confidence interval (CI) 80%, margin of error 5% and estimated proportion of referred patients 30%, as reported by Porter et al22
Data collection
The Health Referral System User Acceptance questionnaire will be used to capture the quantitative nature of the first stage of the study23. In order to obtain qualitative data, the patient satisfaction interview guide will be used, which has been translated from English to Indonesian in accordance with the guidelines on the translation, adaptation and validation of measures from WHO24,25. In addition, an FGD guideline, which has undergone expert evaluation, has been developed for the purpose of guiding data collection from health workers.
Data analysis
Univariate analysis will be conducted for quantitative data. Descriptive statistical analysis will be used to gain insights into referrals made by both intervention beneficiaries and implementers. For the qualitative data, analysis will be conducted simultaneously with data collection, allowing interesting findings to inform subsequent data collection sessions26. The data collected through in-depth interviews and FGDs will be synthesised and coded. These data will then be analysed based on themes using Microsoft Excel or any other appropriate computer programs.
Stage 2: Matrix development
This second stage of the research aims to identify the context of change based on the priority issues encountered in the first stage of the study. The research employs a qualitative method, using FGD for data collection. FGD is conducted in the form of group discussions, aimed at exploring attitudes, perceptions, feelings, experiences or ideas regarding a specific topic, guided by a moderator26. The objectives of this stage are to present the findings from the first stage, discuss one priority issue, establish priority change objectives and develop a change plan together with the FGD members.
Participants
In this second stage, the focus will be on innovation deliverers, namely individuals who are directly involved in the referral system. This will be based on the findings from the first stage of the study. The innovation deliverers encompass the following: heads of nursing at the community health centre, healthcare workers who have facilitated referrals, the head of the community health centre and the district government. The head of a community health centre is an individual who has been formally appointed to the leadership within a community health centre. This appointment is formalised through the issuance of an official letter of appointment. The head of a nursing division denotes an individual who holds an official letter in accordance with the relevant regulations, and who has served in this capacity for a period of more than 6 months. Healthcare workers refer to registered nurses or midwives who possess a valid practical licence and prior experience in assisting or facilitating patient referrals. District government staff are individuals who are in possession of an official letter, which is issued in accordance with the role and applicable regulations.
Data collection
The instrument used in this stage is the FGD guideline. It will be developed by the researchers and consulted by experts. The guideline will be used to gather feedback from the participants regarding the findings from the first stage of the study, establish change objectives and develop matrices.
The problem prioritisation process will use the self-assessment surveys in accordance with the Regulation of the Minister of Health Regulation No. 44 of 2016 on Community Health Centre Management Guidelines. A self-assessment survey is defined as an activity that aims to identify the conditions and challenges faced by the community. In this stage, all the participants will be invited to provide feedback on any issues they have encountered. The identification of problems is a two-stage process. First, issues are categorised and listed. Second, an assessment is made of the community’s ability to address them. This assessment is a key factor in establishment of a priority scale, which is determined through a consensus-based approach. The self-assessment survey is based on the USG (urgency, seriousness, growth) method, which involves the evaluation of the issues according to three factors: urgency (how pressing is the issue?), seriousness (how severe is the issue?) and growth (how likely is the issue to escalate?)27. An overview of the USG method is shown in Table 2.
Table 2: Overview of the USG method†
| Problem | Urgency | Seriousness | Growth | Total |
|---|---|---|---|---|
| A | 1 – 2 – 3 – 4 – 5 | 1 – 2 – 3 – 4 – 5 | 1 – 2 – 3 – 4 – 5 | |
| B | 1 – 2 – 3 – 4 – 5 | 1 – 2 – 3 – 4 – 5 | 1 – 2 – 3 – 4 – 5 | |
| C | 1 – 2 – 3 – 4 – 5 | 1 – 2 – 3 – 4 – 5 | 1 – 2 – 3 – 4 – 5 |
† Based on Likert scale: 5, very large; 4, large; 3, moderate; 2, small; 1, very small.
Data analysis
The results of the FGD, including audio- and video-recordings, will be transcribed and analysed using content analysis. Problem prioritisation based on the USG method will be processed using descriptive analysis. All scores in the USG columns will be summed up, and the issues with the highest total score will be identified as the top priority. After the highest scoring issue is determined, the results will be presented back to the participants for validation and further discussion.
Stage 3: Theory-based methods and practical strategies
Research design
This stage of the study will entail a review of the extant literature concerning current implementation strategies. The objectives are to identify a program that aligns with the problem encountered, with the aim of achieving the agreed-upon change objectives from the second stage of the study, and to develop program materials based on the selected program.
Data collection
The search for relevant literature and the development of material will be conducted using appropriate databases. The identification of keywords for the literature search will be informed by problems being addressed. Following the identification of a suitable program to resolve the issues, materials for the program will be developed. The literature review process and material development will be discussed with the relevant experts.
Stage 4: Program/preparation
Research design
This stage involves brainstorming on the enhancement of the referral system. In this stage, experts or individuals with knowledge in their respective areas are asked for the opinions through FGD. The brainstorming with the experts will be conducted after the researchers finalise the program and materials.
Participants
In this fourth stage, experts and specialists in the field will be invited to participate. Participants in this stage are purposively selected based on their specific roles and responsibilities within the health system. Individuals with relevant decision-making authority, direct involvement in referral processes or experience in primary healthcare service delivery are prioritised. The selection aims to ensure that participants possess sufficient knowledge and practical experience to contribute valuable insights to the study. The experts to be involved in this study are the head of the district health office, a professional nursing organisation in Sangihe District, nurses working in island-based community centres whose referral system functions well, and academics.
The head of district health office is someone who has served as head of the district health office for more than 6 months. Representatives of the professional nursing organisation should possess knowledge of the healthcare system, have educational background in a health-related discipline, minimum of a bachelor degree, and experience working at a community health centre (puskesmas). Healthcare workers should have a practical licence, be assigned at a puskesmas located on an island, have relevant skills, have served at that puskesmas for more than 6 months, and have experience assisting referrals. Participants from the academics’ health-related fields should hold a minimum master’s degree in a health-related field and have knowledge of health policy, primary care management or emergency care.
Data collection
The FGD will discuss the recommended program, and the experts will give their opinions regarding the source of the proposed innovation program, evidence of success supporting the innovation and the adaptability of the innovation to local conditions. The FGD will be conducted online and the session will be recorded.
Data analysis
A research assistant will transcribe the recording into Microsoft Word format. The transcript will be reviewed multiple times by both the researchers and assistants to ensure accuracy and alignment with the recordings. The transcribed data will be coded and analysed using the thematic framework analysis. The analysis results will be reviewed with the research advisory team to validate the accuracy of the findings, relevance of the program and alignment of the strategies with the priority issues identified in the second research stage. The final outcome of this stage is a consensus on the intervention plan developed by researchers.
Stage 5: Adoption and implementation plan
Research design
In this stage, meetings will be convened in order to deliberate the innovation plan with mid-level leaders. The focus of these meetings will be on program recommendations to optimise the referral system. The goal of this stage is to gather feedback, suggestions and opinions regarding the program plan that has been developed in the previous stage.
Participants
The individuals involved in this stage include the chairperson and members of the Health Services and Health Insurance Division of the Health Office of Sangihe District proven by an official letter issued by the head of the district health office. In accordance with Regent Regulation No. 37 of 2019 concerning the structure, duties and functions of the Type A Regional Health Office of Sangihe Islands, the Health Services and Health Insurance Division is tasked with the formulation and implementation of operational policies in primary healthcare services and referral services in healthcare, including quality improvement, traditional healthcare services and accreditation of healthcare facilities28.
Data collection
The discussion will be guided by a set of guidelines for FGD, which have been prepared for the study. The session will comprise interactive discussions with relevant stakeholders regarding the potential for modification or adaptation of the local conditions, the feasibility of conducting a small-scale trial prior to full implementation, the complexity of the recommended innovation and its design, and the budgetary feasibility for implementation.
Data analysis
The discussion results will be transcribed into Microsoft Word format and analysed using content analysis. The findings will be presented in narrative form and reviewed by advisors. The expected outcome is to obtain feedback and direction from program managers at the health office regarding the proposed program.
Stage 6: Evaluation
Research design
In this stage, a seminar will be held to introduce and explain the proposed program. This will be followed by an evaluation process. The program will feature contributions from invited experts in the field. The research evaluation is designed to facilitate the dissemination of the program design among healthcare professionals. The objectives of this stage are to enhance healthcare workers’ knowledge of policies supporting the implementation of referral systems, to explain the program developed in the previous stage of the study and to conduct an antecedent assessment of the program.
Participants
The participants of this stage will be as follows: the heads and nurse coordinators of community health centres located on the small islands, namely Nusa Tabukan Community Health Centre, Marore Community Health Centre and Kahakitang Community Health Centre; the head of the Health Office of Sangihe Islands District; the head of Primary Health Services and Health Insurance Division of the Health Office of Sangihe Islands District; and a representative of the Indonesian Health Nurses Association of Sangihe District. The legitimacy of these participants must be proven by official appointment letter.
Data collection
After the seminar, the researchers will evaluate the program that was introduced by the experts to the participants. The evaluation variable which will be assessed is based on Table 3.
Table 3: Study variables and operational definitions
| Variable | Definition | Instrument | Measurement |
|---|---|---|---|
| Accessibility | Stakeholders’ perception of the recommended program is approved, suitable, satisfactory. | Acceptability of intervention measure29 |
Top third of scores are categorised as highly acceptable. Middle third of scores are categorised as moderately acceptable. Bottom third of scores are categorised as not acceptable. |
| Appropriateness | Stakeholders perceive the recommended program as relevant and appropriate for addressing issues or problems in the community health centres. | Intervention appropriateness measure29 |
Top third of scores are categorised as highly appropriate. Middle third of scores are categorised as moderately appropriate. Bottom third of scores are categorised as not appropriate. |
| Feasibility | Stakeholders believe that the recommended program can be successfully implemented or carried out in a specific environment. | Feasibility of intervention measure29 |
Top third of scores are categorised as highly feasible. Middle third of scores are categorised as moderately feasible. Bottom third of scores are categorised as not feasible. |
Data analysis
After the survey is closed, the questionnaire results will be calculated using Microsoft Excel. The data will be totalled and grouped into three categories30. The results of the data analysis will be presented in tables.
Research risk management
Research risk management is a process of identifying and mitigating potential challenges associated with a study. The objective of this process is to minimise any potential negative impacts that may arise, and to ensure that the study can be conducted safely and effectively. The preliminary risk assessment of this study indicates the possibility of several potential risks arising during the data collection process in the field, as outlined in Table 4.
Table 4: Potential impact of and mitigation plan for risk management elements
| Element | Risk | Potential impact | Mitigation plan | Responsible party |
|---|---|---|---|---|
| Data collection process | Resignation of team member during data collection | Delay in data collection and compromised team productivity |
|
Principal investigator |
| Team member prioritising routine work over research activities | Missed deadlines and incomplete data | Implement a strict schedule | Principal investigator | |
| Prolonged nature of data collection due to remote research sites | Prolonged project timeline, increased costs and lower data quality |
|
Principal investigator | |
| Travel to research sites | Inclement weather conditions (high waves, strong winds, dynamic tides) | Delayed fieldwork and safety risks to the research team |
|
Research team |
| Limited transport availability | Fieldwork cancellations and budget overruns |
|
Research team | |
| Long distances to reach the remote islands | Team fatigue and increased logistical burden | Rent houses from local residents Stay in the field for a longer period Bring food supplies to designated location | Research team | |
| Infrastructure at research sites | Limited supply of electricity | Inability to charge electrical devices or to conduct night-time work | Use electric generator Bring fuel | Research team |
| Lack of projector for presentations | A reduced engagement with stakeholders during the dissemination process | Bring projector to the study site Prepare printed media | Research team | |
| No available venue for conducting focus group discussion | Difficulty having structured discussions with stakeholders or participants | Coordinate to use the village hall | Principal investigator |
Ethics approval
This research obtained ethics clearance from the Medical and Health Research Ethics Committee of the Faculty of Medicine, Public Health, and Nursing, Universitas Gadjah Mada, as well as Dr. Sardjito General Hospital, Yogyakarta, with approval number KE/FK/1162/EC/2024.
Results
Emergencies, work accidents, acts of violence, dangerous diseases and other urgent situations have become increasingly frequent, requiring effective referral interventions to prevent further complications or death31. However, people living on small and remote islands often refuse to be referred to more advanced medical facilities due to financial problems. Therefore, it is essential to comprehensively evaluate the implementation of healthcare services, particularly in terms of referrals from these small and remote islands.
The assessment of the referral implementation from community health centres on small islands to hospitals on the mainland needs to be guided by a systematic protocol. The findings of this research will provide contextual information about the referral implementation process, including its facilitating factors and barriers for both patients and healthcare workers. The evaluation of health services based on feedback from the community and key informants can effectively and efficiently convert data and information into actionable knowledge for policymakers32.
This research is aligned with the SDGs, which promote sustainable development based on human rights and equality across social, economic and environmental dimensions. SDG 3 is about ensuring healthy lives and promoting wellbeing for people of all ages. Achieving these goals requires access to quality primary health services, as well as the development, training and retention of healthcare providers in developing countries and particularly least developed nations, including small islands8.
Conclusion
This study contributes a valuable guide for assessing the quality of health services in remote places. It also offers insights into the challenges experienced by both beneficiaries and providers of health services in those areas, which can inform government intervention strategies. In addition, this study will generate recommendations on interventions that take into account the circumstances of certain healthcare facilities, local practices and existing government regulations.
Funding
This research has been funded by the Indonesian Education Scholarship, Center for Higher Education Funding and Assessment, and Indonesian Endowment Fund for Education as acknowledged in decree number 02986/BPPT/BPI.06/9/2024.
Conflicts of interest
The author and co-authors declare no conflict of interest.
References
You might also be interested in:
2014 - How accurate is the diagnosis of diabetic retinopathy on telescreening? The Indian scenario



