Introduction
Scotland continues to face doctor shortages, particularly in remote, rural and socioeconomically deprived areas, alongside an ageing population, rising chronic disease and widening health inequalities. Recruitment and retention in these regions remain challenging1. Students often perceive rural practice as demanding because of geographical isolation, limited resources and the breadth of generalist skills required2. Although multidisciplinary teams have expanded in primary care, persistent difficulties include adapting to rapid workflows, building relationships and managing increased workloads3. Addressing these issues is essential to secure a sustainable rural medical workforce.
Conventional medical training has not resolved geographical or specialty imbalances. Increasing student numbers alone is insufficient; curricula must provide sustained rural and primary-care exposure to cultivate the skills, resilience and adaptability these settings demand. The Scottish Graduate Entry Medicine (ScotGEM) program seeks to meet this need through a 4-year program that immerses graduates in community and rural practice4. Jointly delivered by the universities of St Andrews and Dundee with National Health Service partners, ScotGEM offers early, continuous exposure to general practice and rural healthcare, case-based learning5 and a longitudinal integrated clerkship (LIC)6, and a final year aligned with the Dundee University 5-year medical degree.
While internationally distributed rural GEM programs have been successful, place-based medical education considers the unique contextual elements of different settings. As such, it is essential to assess preparedness for practice within our own context. As the program matures, evaluating graduates’ self-reported preparedness is crucial. Their confidence and perceived competence will inform curriculum refinement and workforce planning. The General Medical Council Foundation Year 1 (F1) Preparedness Survey7 provides an early benchmark, allowing comparison between ScotGEM graduates and their peers.
Methods
The F1 Preparedness Survey, conducted annually by the GMC, serves as an important nationwide instrument for evaluating the transition of medical graduates into their first year of postgraduate training. This four-item survey captures self-reported perceptions of preparedness among newly qualified doctors across the UK. The items included in the survey are:
- I was adequately prepared for my first foundation post.
- My skills in clinical practical procedures were adequate to prepare me for my first foundation post.
- My skills in prescribing were adequate to prepare me for my first foundation post.
- My skills in managing acutely unwell patients were adequate to prepare me for my first foundation post.
For ScotGEM graduates, the F1 Preparedness Survey represents an early and important benchmarking tool to assess how this novel graduate-entry program aligns with national standards and expectations. Given ScotGEM's emphasis on early and sustained clinical exposure, rural and community-based placements, and the integration of leadership and reflective practice, analysing the preparedness data offers an opportunity to evaluate the program's effectiveness in delivering its intended outcomes. By comparing ScotGEM graduates' self-reported preparedness with national benchmarks, this analysis can provide evidence to support ongoing curriculum refinement and innovation.
A total of 52 ScotGEM students graduated as the inaugural cohort in the Northern Hemisphere summer of 2022 and 40 completed the questionnaire and are included in this study (response rate = 77%). The inaugural cohort began their studies in September 2018.
Statistical analysis
The self-reported preparedness of ScotGEM gradates was compared to the national (UK) responses as well as those of Dundee University graduates; Dundee University serves as a meaningful comparator due to the shared assessment framework in the final 2 years, allowing for direct comparison of preparedness outcomes. To assess differences in perceptions of preparedness among cohorts (ScotGEM, national and Dundee University), we performed pairwise comparisons of response proportions for each question. The proportion of respondents selecting ‘strongly agree' was calculated for each cohort based on the percentage of agreement and the total number of responses within the cohort.
Pairwise comparisons were conducted using Z-tests for proportions, which compare the agreement levels between two groups while accounting for sample sizes. The Z-test evaluates whether the difference in proportions between two cohorts is statistically significant, assuming a null hypothesis of no difference. Pooled proportions were used to calculate the standard error, ensuring that differences in sample sizes across cohorts were appropriately addressed. Statistical significance was defined as a p-value less than 0.05.
To complement statistical significance testing, Cohen’s h was calculated for each pairwise comparison to quantify the effect size. Cohen’s h measures the magnitude of differences between two proportions and is interpreted as small (h<0.2), medium (0.2≤h<0.5) or large (h≥0.5). This approach highlights the practical significance of differences between cohorts, providing additional context beyond p-values.
All analyses were conducted using the provided response data and corresponding agreement percentages. Results are presented as proportions, Z-statistics, p-values and Cohen’s h values, with interpretations indicating the direction and magnitude of differences between cohorts.
Ethics approval
Formal ethics approval was not required for this study as it involved analysis of existing, anonymised secondary data collected and controlled by the national regulator.
Results
ScotGEM graduates reported similar levels of preparedness to the national average (Table 1): 57.5% of ScotGEM graduates felt adequately prepared for practice (compared to 57.9% nationally), 84.6% felt their skills in clinical practical procedures were adequate (compared to 80.3% nationally), 75.0% felt their prescribing skills were adequate (compared to 79.3% nationally) and 75.0% felt they were adequately prepared to manage an acutely unwell patient (compared to 68.4% nationally).
Statistical analysis revealed no statistically significant differences in perceptions of preparedness between the ScotGEM cohort and the other cohorts (national and Dundee University) across all evaluated questions. While ScotGEM generally reported some differences in the proportions of agreement compared to students nationally or from Dundee University, these differences did not reach statistical significance (p>0.05). Effect sizes for these comparisons were small (h<0.2), suggesting minimal practical differences in preparedness levels. These results are summarised in Table 2 and Figure 1.
Table 1: Number of ‘strongly agree’ responses for each question in the F1 Preparedness Survey for each cohort (ScotGEM, national and Dundee University)
| Survey item | n | % strongly agree | Lower bound | Upper bound | |
|---|---|---|---|---|---|
| 1. I was adequately prepared for my first foundation post. | ScotGEM | 40 | 57.5 | 42.2 | 71.5 |
| Dundee University |
113 |
69.0 | 60 | 76.8 | |
| National† |
5894 |
57.9 | 56.7 | 59.2 | |
| 2. My skills in clinical practical procedures were adequate to prepare me for my first foundation post. | ScotGEM | 39 | 84.6 | 70.3 | 92.8 |
| Dundee University |
114 |
88.6 | 81.5 | 93.2 | |
| National |
5895 |
80.3 | 79.3 | 81.3 | |
| 3. My skills in prescribing were adequate to prepare me for my first foundation post. | ScotGEM | 40 | 75.0 | 59.8 | 85.8 |
| Dundee University |
114 |
83.3 | 75.4 | 89.1 | |
| National |
5897 |
79.3 | 78.3 | 80.3 | |
| 4. My skills in managing acutely unwell patients were adequate to prepare me for my first foundation post. | ScotGEM | 40 | 75.0 | 59.8 | 85.8 |
| Dundee University |
114 |
82.5 | 74.4 | 88.3 | |
| National |
5896 |
68.4 | 67.2 | 69.5 |
† UK cohort.
ScotGEM, The Scottish Graduate Entry Medicine.
Table 2: Outcome of statistical analysis, comparing responses of each cohort for each question
| Survey item | Comparison | Z-statistic | p-value | Cohen’s h |
|---|---|---|---|---|
| 1. I was adequately prepared for my first foundation post. | ScotGEM v national† | –0.05107 | 0.959272 | –0.0081 |
| ScotGEM v Dundee University |
–1.31944 |
0.187022 | –0.23923 | |
| Dundee University v national |
–2.36895 |
0.017839* | –0.23113 | |
| 2. My skills in clinical practical procedures were adequate to prepare me for my first foundation post. | ScotGEM v national | 0.681837 | 0.495342 | 0.113233 |
| ScotGEM v Dundee University |
–0.65953 |
0.509555 | –0.11773 | |
| Dundee University v national |
–2.21359 |
0.026857* | –0.23096 | |
| 3. My skills in prescribing were adequate to prepare me for my first foundation post. | ScotGEM v national | –0.66863 | 0.503733 | –0.10251 |
| ScotGEM v Dundee University |
–1.15465 |
0.248236 | –0.20523 | |
| Dundee University v national |
–1.0455 |
0.295794 | –0.10272 | |
| 4. My skills in managing acutely unwell patients were adequate to prepare me for my first foundation post. | ScotGEM v national | 0.895156 | 0.370704 | 0.146742 |
| ScotGEM v Dundee University |
–1.03112 |
0.302487 | –0.18399 | |
| Dundee University v National |
–3.21469 |
0.001306** | –0.33073 |
*p<0.05, **p<0.01, ***p<0.001.
† UK cohort.
ScotGEM, The Scottish Graduate Entry Medicine.
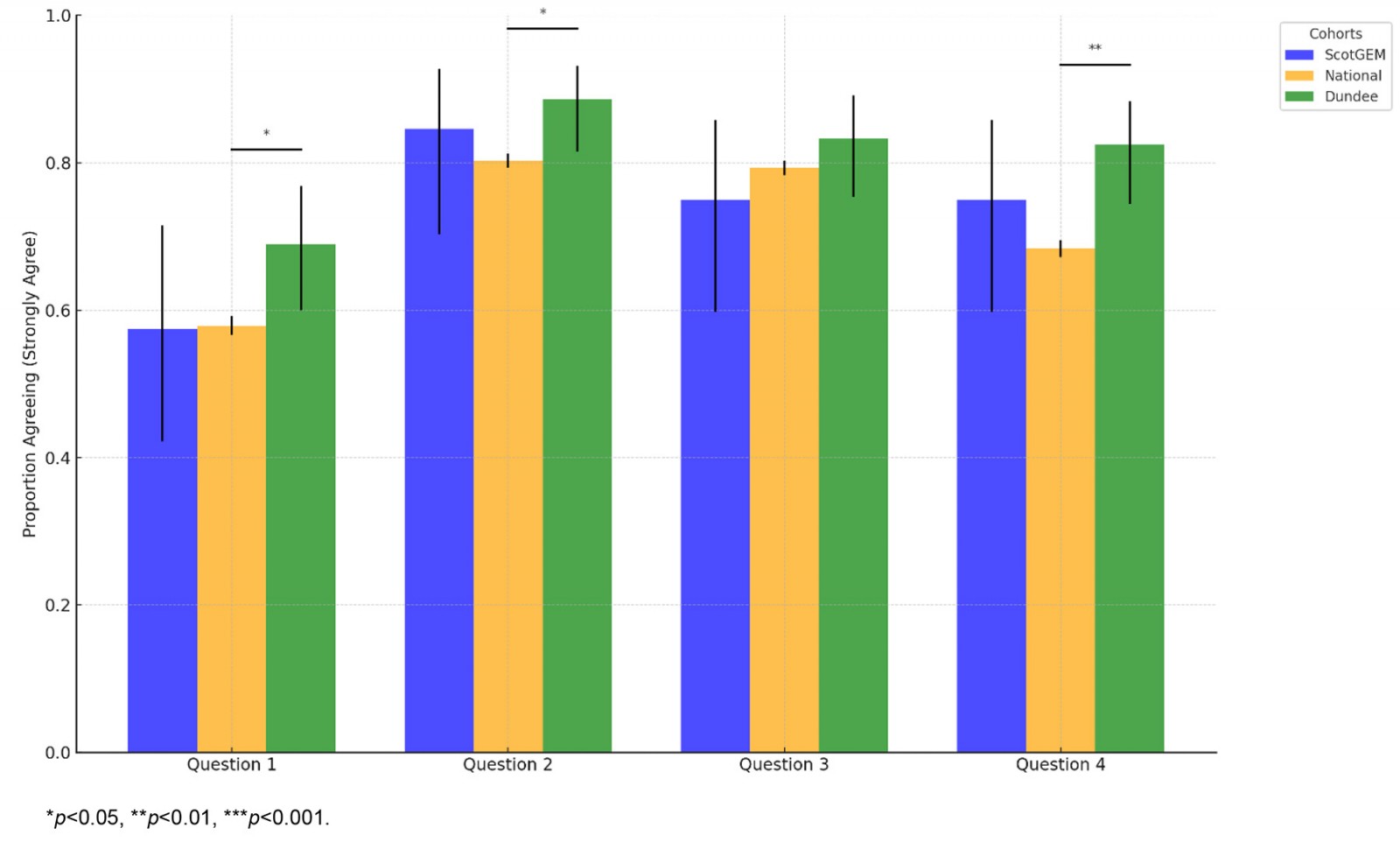 Figure 1: Comparison of self-reported preparedness between cohorts (ScotGEM, national and Dundee University) and survey items.
Figure 1: Comparison of self-reported preparedness between cohorts (ScotGEM, national and Dundee University) and survey items.
Discussion
ScotGEM graduates reported levels of preparedness broadly comparable to the national average across all surveyed domains, with no statistically significant differences observed. While minor variations were noted in specific areas, effect sizes were small, indicating minimal practical differences in perceived preparedness between ScotGEM, national and Dundee University cohorts.
These findings are in alignment with similar reports elsewhere in the literature. While analysis of preparedness data is limited, research comparing graduate-entry medical (GEM) and traditional-entry medical students in the UK suggests that GEM students perform as well as or better than their traditional counterparts. Byrn et al found that GEM students perform at least as well as traditional students in final examinations, regardless of academic background8. Garrud and McManus observed no significant differences in completion rates or performance measures between GEM and traditional-entry program students, despite differences in student profiles9. They noted that aptitude test scores, sex, age and ethnicity were predictive of success, while prior degree subject and class were not. These findings support the viability of accelerated GE programs in medical education, demonstrating that GEM students can achieve comparable or superior outcomes to traditional-entry students despite the compressed time frame. Manning and Garrud made similar observations, with GEM students achieving slightly lower scores on knowledge-based exams but similar skills-based and attitudinal assessments10.
These findings add to the existing body of evidence that LICs and rural placements do not disadvantage medical students and instead have positive impacts on medical students' academic attainment and career choices. Studies have found no significant differences in academic performance between rural LIC students and those in traditional urban rotations11,12. LIC students reported increased confidence in clinical skills and felt better prepared for internship12,13. Rural placements provided students with more hands-on experience, closer relationships with patients and supervisors, and increased access to patients12,13. Importantly, LIC experiences, especially when combined with additional rural training, were associated with a higher likelihood of choosing rural work locations after graduation14. These findings suggest that rural LICs are effective in preparing students for medical practice and may contribute to improving rural medical workforce distribution11,14.
The lack of statistically significant differences between ScotGEM and the other cohorts may, in part, reflect the smaller sample size of the ScotGEM cohort, which limits statistical power. With only 40 respondents, the ability to detect subtle differences is reduced compared to the much larger national cohort, which had more than 5000 respondents. This underscores the importance of interpreting both statistical and practical significance when evaluating the results.
Conclusion
As ScotGEM continues to grow and future cohorts enter the workforce, ongoing evaluation with larger sample sizes will be essential to capture more nuanced insights and further refine the program’s contributions to addressing Scotland's healthcare challenges, particularly in rural and underserved areas. Future research should explore how these experiences translate into career choices, particularly in addressing workforce shortages in rural healthcare settings.
Conflicts of interest
The author is the Deputy Programme Director of the ScotGEM program, based at the University of St Andrews. There are no further interests to declare.

