Introduction
I was very lucky to grow up and call the Shetland Islands my home. They are located in between Scotland, Norway and the Faroe Islands (Fig1) and are composed of over 100 islands. Only 12 of the islands are inhabited and most people live on the largest island, which is known simply as ‘Mainland’. The other islands are accessible by lifeline ferry and airline services, which are liable to frequent disruption due to poor weather conditions. Shetland can be reached via an overnight ferry from Aberdeen or an 80-minute flight from mainland Scotland, making it extremely remote and rural in comparison with most other parts of the UK.
Shetland’s only hospital is situated in the main town of Lerwick (Fig2). The Gilbert Bain Hospital (GBH) is a three-storey building with 71 beds spread over medical, surgical, rehabilitation, day surgery and maternity wards. It also has a large outpatient department, as well as laboratory, radiology, physiotherapy and occupational therapy services all on site, including the relatively recent addition of a CT scanner.
The GBH accident and emergency (A&E) department serves not only Shetland’s 23 000 inhabitants, who are widely distributed over a relatively large area, but also anyone within the surrounding waters. This includes over 4000 employees in both the oil and fishing industries situated on nearby offshore installations and marine vessels1.
Despite having already undertaken a placement at the GBH, I was eager to spend more time there due to the excellent teaching and clinical experience my previous placement had provided me. For this rotation, I wanted to focus on A&E because this is a speciality I have had limited exposure to during my training. Additionally, I thought that this environment would confer a fantastic opportunity to learn about the basics of A&E care and the challenges associated with providing these services in a unique location such as Shetland. Through researching and writing this essay, I also hoped to both gain a deeper understanding of, and publicise the benefits and challenges of, working in one of the UK’s most remote A&E departments, and discuss how its services might be improved in the future.
 Figure 1: Map showing Shetland’s location in relation to the Faroe Islands, Bergen (Norway) and Aberdeen (Scotland)2.
Figure 1: Map showing Shetland’s location in relation to the Faroe Islands, Bergen (Norway) and Aberdeen (Scotland)2.
 Figure 2: Photo of the Gilbert Bain Hospital in Lerwick, Shetland Islands3.
Figure 2: Photo of the Gilbert Bain Hospital in Lerwick, Shetland Islands3.
Shetland’s A&E facilities
The A&E department is composed of three patient cubicles (including one designed to accommodate children's needs), a plaster room, a two-bay resuscitation room and a waiting area and relatives room. There is also a staff room, which accommodates both kitchen and telemedicine facilities. In terms of general layout, the department is directly connected to both the radiology and laboratory departments on either side.
A&E is permanently staffed by full-time nurses and, between 8am and 8pm, by both a medical and a surgical doctor. However, overnight there is only a single junior doctor covering the whole hospital. There are also dedicated on-call medical, surgical and anaesthetic consultants for each shift.
In addition to its A&E services, the department also acts as a primary care centre out-with normal GP surgery working hours. This service is provided by the National Health Service (NHS) 24 (Scotland’s national telehealth and telecare organisation). Therefore, workload during these times, and especially over the weekend, can be very high due to the need to also treat these primary care issues.
Shetland’s ambulance service provides two ambulances in Lerwick (Fig3), which are staffed by paramedics on seven day shifts and four night shifts per week; the remaining weekend nights are on-call only. There are also smaller community ambulances on several of the outer islands that are crewed by on-call volunteers from the local community.
The Coastguard is also a valuable components of Shetland’s A&E team. They retrieve patients via helicopter and lifeboat, for example, from offshore platforms or from areas inaccessible by ambulance. Finally, Scotland’s emergency medical retrieval service (EMRS) can also be utilised in cases where a patient requires transfer away from Shetland to a tertiary centre, often the Aberdeen Royal Infirmary.
 Figure 3: One of Lerwick’s two ambulances waiting outside the main entrance to the Gilbert Bain Hospital4.
Figure 3: One of Lerwick’s two ambulances waiting outside the main entrance to the Gilbert Bain Hospital4.
Reflection on the A&E department
One thing I immediately realised was how busy the department can be, because I had naively thought that it may be relatively quiet in comparison with its urban counterparts. Attendance rates are almost double the Scottish average5; however, this can be accounted for by the previously mentioned out-of-hours primary care service5. Despite this, NHS Shetland is one of the best performing in the country for patients being seen within the government’s target of 98% of all A&E patients being admitted, discharged or transferred within 4 hours of arrival (Table 1)6.
One explanation for this may be the excellent multi-disciplinary team (MDT) working in the department. I was struck by the camaraderie I observed between this small team who work together every day, many of whom also having grown up together. Interestingly, I believe that the layout of the hospital contributes to this teamwork; the A&E staff have strong links with both the laboratory and radiology teams due to working in such close proximity with them, which is less common in urban hospitals where these departments are separated by larger distances. This results in quick face-to-face communication of any issues, contributing to the speed at which patients can be treated.
Being the only medical student in the department was invaluable in allowing me to build relationships with each MDT member who, in turn, provided me with opportunities to expand my clinical skills and receive one-to-one teaching. It has been shown that medical students undertaking rural placements usually see more medical conditions, gain more clinical exposure and feel more ‘useful’ and ‘a part of the team’ than students on urban placements7. My experience supports this. For example, the nursing staff would kindly fetch me when a patient had ‘great veins!’ in order to improve my cannulation skills, and the surgical team often asked for my assistance with stabilising fractures and applying casts.
I was especially appreciative to be the only medical student present when undertaking evening and weekend work, as I was encouraged to see patients before the single doctor in the hospital arrived. This experience allowed me to develop different ways of examining and communicating with a huge variety of patient groups, including children and their worried parents, those in severe pain and people who are intoxicated. It also provided opportunities to consider differential diagnoses and management plans for each patient before discussing them with the doctor. This meaningful patient contact and chances to ‘act like a junior doctor’ are known to be important in preparing medical students for life after graduation8.
Working in such a small team also has disadvantages, including pressure on relatively few staff to provide 24/7 cover. One issue many rural hospitals have is that laboratory and radiology services are not immediately available out of working hours. Staff are available on-call, but one particular case made me appreciate that utilising this service can also have issues (See Example 1). This pressure and prolonged periods on-call has been found to contribute to poor recruitment rates of allied health staff to remote and rural areas9,10.
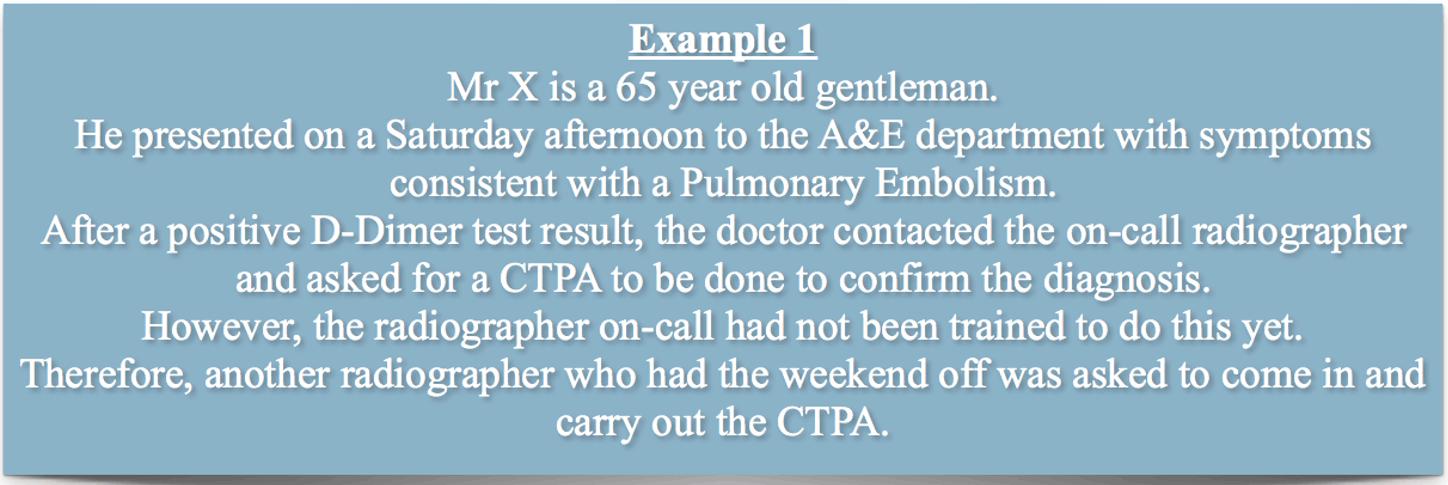
Another obstacle for the recruitment of staff to remote areas is that the staff must be ‘generalists’. Yet, there is a growing tendency and pressure for doctors to specialise soon after graduating from, and even during, medical school11. My supervisors often asked ‘Have you decided what you want to specialise in yet?’. One of the disadvantages of having limited specialist input became particularly apparent to me when paediatric cases presented, with junior staff much more cautious of making decisions without input from the on-call consultants. Paediatrics was also the speciality mentioned by almost all staff when I asked which speciality would be the most useful addition to the current MDT in Shetland.
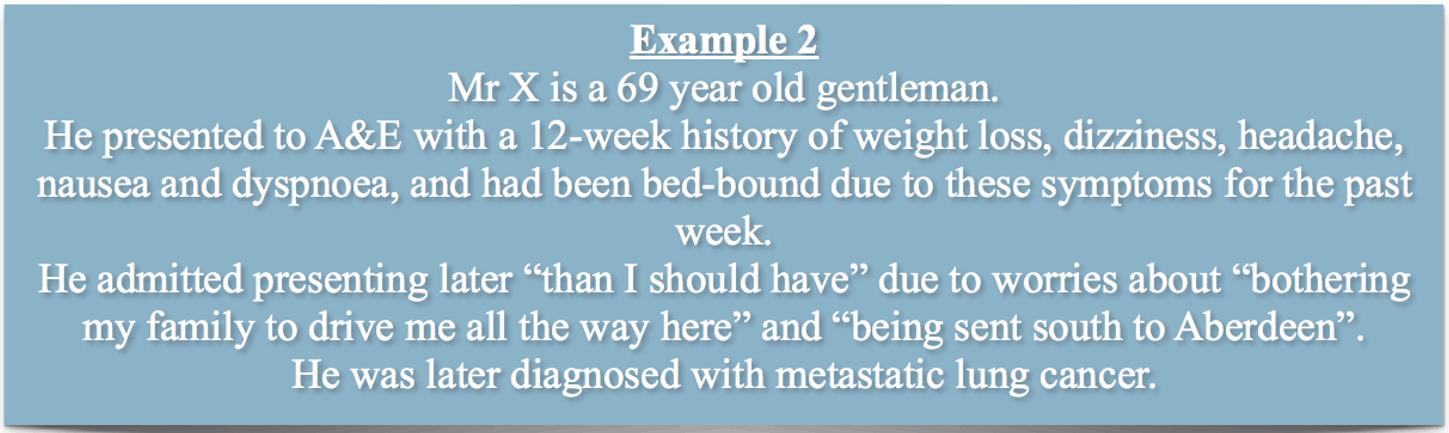
Another aspect I found interesting during my research is that patients in rural areas tend to present to A&E later, with more advanced or severe disease than urban patients12-14. One possible explanation is that rural patients wish to avoid being sent either to the local hospital after presenting to their GP, or to a more distant tertiary hospital, due its distance from their home. I found this to be true in Shetland, especially for many of the elderly patients living on the outer islands who were often very unwell on presentation (See Example 2).
Finally, I spent a day with the paramedics of the Scottish ambulance service in Lerwick. It soon became apparent to me how important this service is and the challenges it must overcome in order to provide essential patient care. One such challenge is Shetland’s often adverse weather conditions. On this day in January, the weather happened to be particularly terrible with wind speeds in excess of 100 miles per hour, and many of the calls were related to this.
Table 1: Most recent figures available showing the two best and worst performing National Health Service (NHS) Boards in Scotland for achieving the 98% target6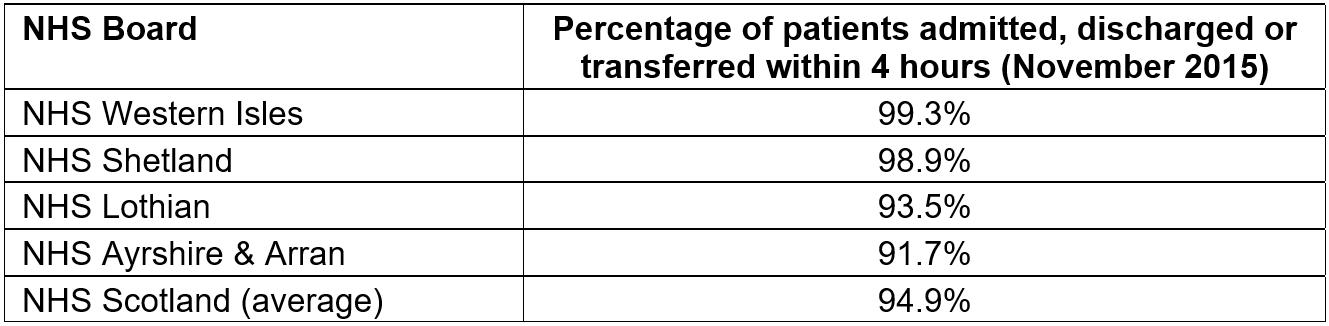
Reflection on A&E care in the especially remote areas of Shetland
It is known that rural patients highly value having access to local emergency medical care15, and I was eager to learn more about how living in the extremely remote and rural areas of Shetland alters patient access to this care.
From my experience growing up in Shetland, I have always had the impression that these especially remote communities are exceptionally resilient and eager to take responsibility for their own health16. This is demonstrated by the community ambulances on the outer islands, which are staffed solely by on-call volunteers. These individuals are trained in advanced first aid skills and are able to provide treatment until the patient can be transferred to Lerwick, which can be a considerable length of time depending on weather conditions and availability of medical transfer services, especially since the helicopter service is often only used for severely unwell patients. For example, even with perfect weather conditions, the journey from Shetland’s most northerly island, Unst, down to Lerwick by public transport still takes over 2 hours. Therefore, these volunteers are a vital part of rural health care in Shetland and their good will ensures that patients in rural communities have confidence in the emergency care available17.
I have personally seen an example of how these communities can ‘pull together’ to both deal with a medical emergency and make positive changes afterwards (See Example 3). After the event described in Example 3, the local community raised money to organise training days to teach cardio-pulmonary resuscitation and automatic external defibrillator (AED) operation. Early utilisation of both of these techniques is crucial in reducing mortality from myocardial infarctions in rural areas18. AEDs were also installed throughout the island and on local fishing boats because increased access to these devices has been previously shown to have a significant impact on patient survival rates19.
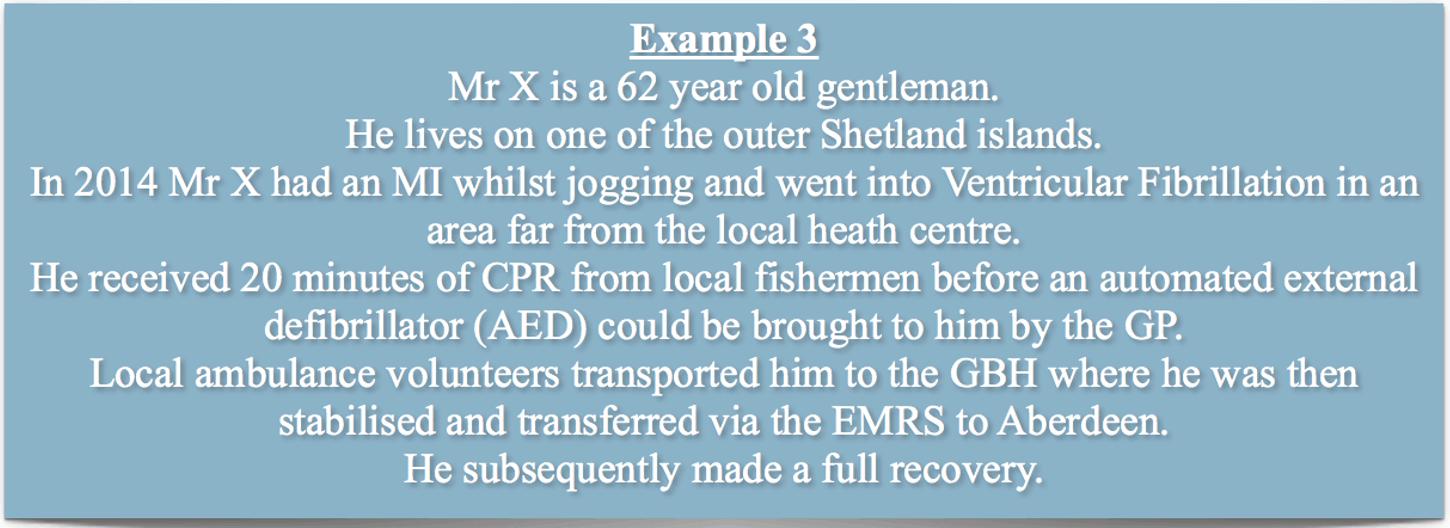
This community resilience and teamwork is known to be a huge asset to these extremely remote areas, which are often understaffed due to difficulties in recruiting and retaining healthcare staff20. Doctors and nurses are often less willing to work in such areas due to long periods on-call, frequent travel disruptions and both social and professional isolation21.
The importance of the coastguard services (Fig4), and the vital role the A&E department has in providing care for anyone in Shetland’s surrounding waters, was highlighted to me by one memorable case (See Example 4). I observed that the seamless interaction between a variety of services ensured the safe transfer of the patient from his unique location to receive the care he required in Lerwick, and believe this certainly prevented him from developing any serious, or even fatal, complications.
 Figure 4: Coastguard helicopter landing at the helipad in Lerwick close to the Gilbert Bain Hospital22.
Figure 4: Coastguard helicopter landing at the helipad in Lerwick close to the Gilbert Bain Hospital22.
How to improve A&E services in Shetland
Firstly, after now completing two rural placements in Shetland, I am sure that these have been both the most enjoyable and the most educational placements I have undertaken during my medical degree so far. Therefore, I believe that it is important for medical schools to increase the quantity and availability of these placements from the relatively small number currently available2. It is known that rural placements provide more clinical exposure and access to a wider variety of conditions7, which provides a great learning environment for students. Completing a rural placement is also associated with a higher likelihood of working in a rural area in the future23,24, which could improve recruitment.
One way to improve access to speciality services in Shetland could be to make use of GPs with special interests, which is already being done with great results in other areas of Scotland25. These are GPs who do additional training to allow them to provide additional services within a speciality; for example, running clinics or undertaking A&E on-call work. This could hugely benefit patients in Shetland by providing access to specialist services in the GBH and reducing the need for patients to travel to mainland Scotland for their care. It could also benefit local GPs and improve both recruitment and retention rates, because a desire to pursue a speciality is often the reason many rural physicians relocate to urban areas26.
The use of telemedicine (Fig5) could further improve access to specialist care, and is increasingly being used in other rural A&E departments26. In principal, this service allows isolated doctors quick access to specialist services and advice; however, I had little exposure to this despite the resources being available at the GBH. The main reason for its lack of use concerns the poor quality and reliability of broadband internet connection in Shetland27. If the available facilities could be improved, and thus be used more regularly and reliably, this could potentially also reduce the number of transfers to tertiary centres28.
Finally, healthcare workers in remote and rural areas are much more likely to regularly engage in complex and critical emergency care, including stabilising injured and severely ill patients pending retrieval, than their urban counterparts29. This obviously requires an expanded skill set, so it comes as no surprise that uptake of courses relating to these skills is already highest amongst staff in rural areas26. However, I recently attended the Rural GP Association of Scotland conference where doctors discussed how difficult, both financially and logistically, they find it to attend these courses due to transport issues and arranging locum cover. I believe that, in order to maintain this high skill level, it could be beneficial to organise these courses within the rural areas themselves to encourage and maximise attendance by even the most remote GPs.
 Figure 5: A specialist consultant taking a history and examining a patient living in a rural location via telemedicine technology27.
Figure 5: A specialist consultant taking a history and examining a patient living in a rural location via telemedicine technology27.
Conclusion
Before this placement, I had limited experience of the practicalities of working in any A&E department; however, following 5 weeks of excellent teaching and support from all of the GBH staff, I now feel I have a true appreciation of how A&E care is delivered and the challenges associated with providing this care in such a unique, isolated location. I also began with little confidence in my ability to examine and treat patients in acute situations because almost all of my previous placements had been in ward settings. However, this experience provided countless opportunities for me to practice and gain confidence in these skills.
This placement also provided the opportunity to research and write this essay, which gave me a much deeper understanding of how emergency care is provided in remote areas and allowed me to consider how care could be improved for future patients. I believe key areas for improvement include increasing links with medical schools to provide more student placements, possibly through publicising positive testimonies from students who have already been (such as myself), and also improving recruitment and retention of staff through increased access to further training opportunities.
In summary, this placement has confirmed to me that a career in rural medicine is exciting and rewarding but also extremely challenging and stressful at times. I remain hopeful that it will be a speciality that I can become a valuable part of in the future.
