Introduction
Mental health problems are prevalent among Australian adolescents1, with suicide a leading cause of death for Australians aged 15–24 years2. The majority of same-sex attracted adults realise their same-sex attraction between the ages of 10 and 19 years3. The current study focuses on adolescents who report a same-sex attraction. For sexual minority adolescents (which includes adolescents who endorse same-sex attraction, same-sex behaviour, as well as those with a bisexual, transgender or intersex identity), mental health problems are even more prevalent4. This includes higher levels of depression, substance abuse, risk of suicide, more family problems, more frequent and violent victimisation, and stress associated with ‘coming out’5. A meta-analytic review found significantly higher rates of depression and suicidality in sexual minority adolescents compared to heterosexual adolescents6.
Recent Australian data show mental health problems are more prevalent among 4–17 year olds living outside capital cities (capital cities 12.6%, rest of state 16.2%)1. While there is limited Australian research to date examining mental health problems in sexual minority status rural adolescents, a population-based Canadian survey found that gender, sexual minority status and place of residence were related to the emotional wellbeing of adolescents. Sexual minority boys living in a rural community were more likely to report suicidal behaviours compared to their urban peers. In addition, rural sexual minority adolescents, especially girls, reported higher use of substances compared to their urban peers7. Similarly, Australian research with same-sex attracted and gender questioning young people has reported higher levels of suicidality and higher concern about their lives for those living in rural and remote areas compared with those living in urban areas, with issues including isolation, discrimination and inadequate services described8.
Minority stress theory9 has been proposed as a framework to understand disparities in mental health outcomes among sexual minority adolescents. The theory suggests that sexual minority adolescents ‘experience distinct, chronic stressors related to their stigmatized identities, including victimization, prejudice, and discrimination’ (p. 4) which, along with stressors in common to all adolescents, results in poorer mental health. Work from the USA has supported this with Willging, et al10 reporting findings from interviews with providers of mental health services in rural areas. Providers indicated that living in a rural area makes it hard for adolescents to access the right service that is sensitive to their needs as a sexual minority adolescent. Providers reported adolescents had been denied services and discouraged to access services due to their sexual orientation, increasing the risk of not receiving the appropriate service.
While there is little work with rural adolescents themselves exploring the applicability of minority stress theory, work with rural sexual minority adults focusing on factors related to mental health has been reported that broadly supports this theory. McLaren, et al11 found that a sense of belonging to the general community mediated the relationship between sexual orientation and depression and that, after sense of belonging was factored in, sexual orientation was no longer associated with depression among rural Australian men, with the authors concluding that stigmatisation is linked with social exclusion and depression. Gottschalk3 also reported that in an Australian rural community the discrimination and stigma experienced by same-sex attracted adults was exacerbated by a lower sense of belonging; social exclusion, alienation and isolation; fewer services and support networks; a lack of anonymity; higher levels of harassment; a fear for one’s safety; less information; and negative stereotypes. Further, the majority of participants believed that negative stereotypes influenced their feelings of self-worth when they were coming out, which often resulted in anxiety or depression. Gottschalk3 also reported that discrimination can lead to stigma consciousness and that this can be internalised and lead to increased psychological distress. In rural areas there is not often an identifiable gay community and so a sense of group identification is also hindered12.
Research comparing mental health among sexual minority adults in rural and urban settings has not reported consistent findings. Wienke and Hill13 examined responses to a single-item self-rating of happiness. US adults who identified as gay or lesbian did not differ in their happiness rating from their peers in urban areas. Using a more comprehensive assessment of mental health, Lyons, et al14 argued that Australian gay-identified men living in rural and remote areas have more health and wellbeing issues than those in urban areas. They reported that gay-identified men who lived in rural and remote Australia had significantly lower self-esteem, love life satisfaction, fewer social groups and less support and were significantly more likely to be psychologically distressed around the acceptance of their sexual orientation than those who lived in urban areas.
While there is a body of theory and research pointing towards the likely higher rates of mental health issues for sexual minority adolescents compared with heterosexual adolescents in rural areas, the authors are not aware of any data that compares the functioning of same-sex attracted and heterosexual adolescents living in rural Australia. Further, while minority stress theory and prior research suggests that same-sex attracted adolescents are likely to experience higher levels of stressors in their relationships, and higher levels of bullying and victimisation, this has not been examined in a rural adolescent population. Finally, while prior research also suggests that same-sex attracted adolescents are likely to perceive more barriers to accessing mental health services, such as concerns about confidentiality, this has not been examined in a rural adolescent population. This study aimed to address these gaps in understanding using self-reported survey data.
It was hypothesised that the prevalence of symptoms of depression would be greater in adolescents who identified as same-sex attracted compared to heterosexual adolescents. This was examined for both level of symptoms of depression and a positive screen for depression. It was also hypothesised that suicidality would be higher in adolescents who identified as same-sex attracted compared to heterosexual adolescents. This study hypothesised that same-sex attracted adolescents would report more experiences of stressors relating to relationships, bullying and physical assault than heterosexual adolescents. Finally, this study also hypothesised that same-sex attracted adolescents would perceive more barriers to seeking support for mental health problems than heterosexual adolescents.
Methods
Participants
Adolescents residing in rural South Australia participated in the current study (N=531). Ages ranged from 13 to 18 (mean=15.1, standard deviation (SD)=1.2) years. Remoteness of location assessed by ARIA+ scores ranged from 0 to 14.5 with a mean ARIA+ score of 4.7 (SD=2.4).
Measures
This study is a component of the Adolescent Mental Health, Behaviour and Life Experiences Survey. This study was designed to assess a range of risk factors relating to wellbeing among rural adolescents with other findings reported previously15.
Same-sex attraction: Participants were asked if they ever had (1) a romantic attraction to a male or (2) to a female, and if they have ever had (3) a romantic relationship with a male or (4) with a female. If participants indicated they had ever had a romantic attraction or relationship with a person of the same sex they were described as ‘same-sex attracted’ or as having been in a ‘same-sex relationship’. (Note: While some participants indicated attraction or relationships with both sexes, due to small numbers the authors did not consider these adolescents separately.) These questions are taken from Russell and Joyner5. They believed these questions were more suitable for measuring same-sex orientation in adolescents as they may not yet identify as heterosexual, homosexual or bisexual. Stigma may also prevent those that are attracted to the same sex from identifying as bisexual or homosexual and some adolescents may have been attracted to a member of the same sex but not acted on the attraction.
Depression and suicidality: The Kutcher Adolescent Depression Scale (KADS-6)16 measured symptoms of depression. The KADS-6 assesses symptoms consistent with a Diagnostic and Statistical Manual of Mental Disorders (DSM-IV) diagnosis of major depressive disorder17. The scale consists of six items in which respondents indicate the frequency of symptoms using a four-point scale ranging from 0 (‘hardly ever’), 1 (‘much of the time’), 2 (‘most of the time’) to 3 (‘all of the time’). Item 6 asks adolescents whether they have had ‘Thoughts, plans, or actions about suicide or self-harm’. On this item response options are 0 (‘no thoughts or plans or actions’), 1 (‘occasional thoughts, no plans or actions’), 2 (‘frequent thoughts, no plans or actions’), 3 (‘plans or actions’). The total score is the sum of the scores from the six items, including the suicidality item (possible range 0–24). The KADS-6 has high sensitivity (92%), specificity (71%), and test–retest reliability (Cronbach’s α of 0.80) using a cut-off score of 6,17 as well as having a high correlation with the Beck Depression Inventory18. This cut-off was used to indicate a positive screen for depression. Internal consistency reliability in the current study was good (Cronbach’s α of 0.83).
Stressors: Stressors experienced by participants were assessed using a life event rating scale using the same format as established measures of adolescent life events such as the Junior High Life Experiences Survey19 and the Life Events Checklist20. Participants indicated whether they had experienced 27 stressful life events. The life events covered a wide range of events such as serious injury or illness. The present study focused on eight stressful life events: relationships with peers, teachers or relatives (parents, siblings and extended family), bullying at school or home, and being the victim of physical assault. Participants were asked to ‘indicate whether you have experienced any of these life events, and if so indicate by circling a mark on the line the impact you think the life event has had on you’. Participants indicated their response from five options: (1) ‘have not experienced’, (2) ‘have experienced, but no impact’, (3) ‘have experienced, slightly bad’, (4) ‘have experienced, pretty bad’ and (5) have experienced, very bad’.
Barriers to seeking mental health support: Barriers to seeking mental health care for Australian adolescents, identified by Aisbett, et al21 and Quine, et al22 were listed. Participants were instructed as follows: ‘The following is a list of reasons it may be hard to seek help for a mental health issue. Please tick the box beside any reason why you think it would be difficult to seek mental health care.’ There were seven barriers listed, and participants were also asked if there were other barriers and, if so, to describe them. A total score (maximum total = 8) was calculated.
Perceptions of seeking mental health support: In addition, to examine perceptions about seeking support for mental health issues, participants were asked to indicate their agreement with three statements with the following response options: (1) ‘true all of the time’, (2) ‘true most of the time', (3) ‘sometimes true’ and 4 ‘never true’. The statements were ‘I would be comfortable seeking help for a mental health issue’, ‘I should be able to deal with mental health issues without help from others’ and ‘It is hard to find help for a mental health issue’.
Remoteness of location: Remoteness of the postcode of participants was assessed using the ARIA+. This measures access in terms of remoteness along the road transport network to service centres23. For each postcode, distance to service centres is converted to a ratio to the mean, which produces a continuous variable with remoteness values ranging from 0 to 1524. An ARIA+ score of zero indicates high access to services and 15 indicates very poor access to services.
Procedure
Principals of all 72 public schools located in regional and rural South Australia (ie not in Adelaide) were mailed invitations to participate in a study on rural student wellbeing, and then contacted via telephone to discuss participation; 23 chose to participate. After parental written consent was provided, students completed the questionnaire in hard copy or electronic form. The most common reason for non-participation was time pressures (n=27), difficulty establishing contact with the principal (n=12), not interested (n=4), discomfort with the survey subject matter (n=3) and difficulty getting consent forms returned (n=3).
Questionnaires were completed in 2010. Data were analysed using SPSS Statistics for Windows, v23 (IBM; http://www.spss.com).
Data analysis
Differences between same-sex attracted and heterosexual adolescents were examined using independent samples t-tests or, where data were not normally distributed, using Mann–Whitney U-tests. Similarity of data distribution was assessed using histograms and box plots prior to analysis using the Mann–Whitney U-test. Where data were in the form of proportions, differences between groups were tested using the χ2 test for independence (with Yates Continuity Correction) or Fisher’s exact test where there were small expected cell sizes (expected frequency of at least 5). Statistical analyses were conducted using SPSS Statistics for Windows. Level of significance was set at 0.05 for all analyses, and the magnitude of relationships for analyses using Mann–Whitney U-tests (r) and c and Fisher’s exact tests (phi) were described according to Cohen’s25 guidelines, with 0.1, 0.3 and 0.5 indicating small, moderate and large relationships, respectively. Effect sizes (eta squared) for analyses using t-tests were interpreted as 0.01, 0.06 and 0.14 indicating small, moderate and large effects, respectively.
Ethics approval
Ethics approval (no. 10/07) was obtained from the relevant university and education department ethics committees.
Results
Of the 3008 students from 23 schools invited to participate, 531 students completed the measures (18% participation rate). Of the 531 participants, 55% were female and 43% were male (2% no response). Six percent identified as same-sex attracted (n=31) with fewer adolescents reporting that they had had a same-sex relationship (n=21). Of the participants reporting that they had had a same-sex relationship, all but two also reported identifying as same-sex attracted. A comparison of the demographic characteristics of same-sex attracted and heterosexual participants showed that same-sex attracted adolescents were older, and were more likely to be female. There were no differences between same-sex attracted and heterosexual participants in degree of remoteness, place of birth or Aboriginal or Torres Strait Islander background (Table 1).
Table 1: Demographic characteristics, positive screen for depression, symptoms of depression (Kutcher Adolescent Depression Scale Total score) and suicidality item scores (KADS Item 6)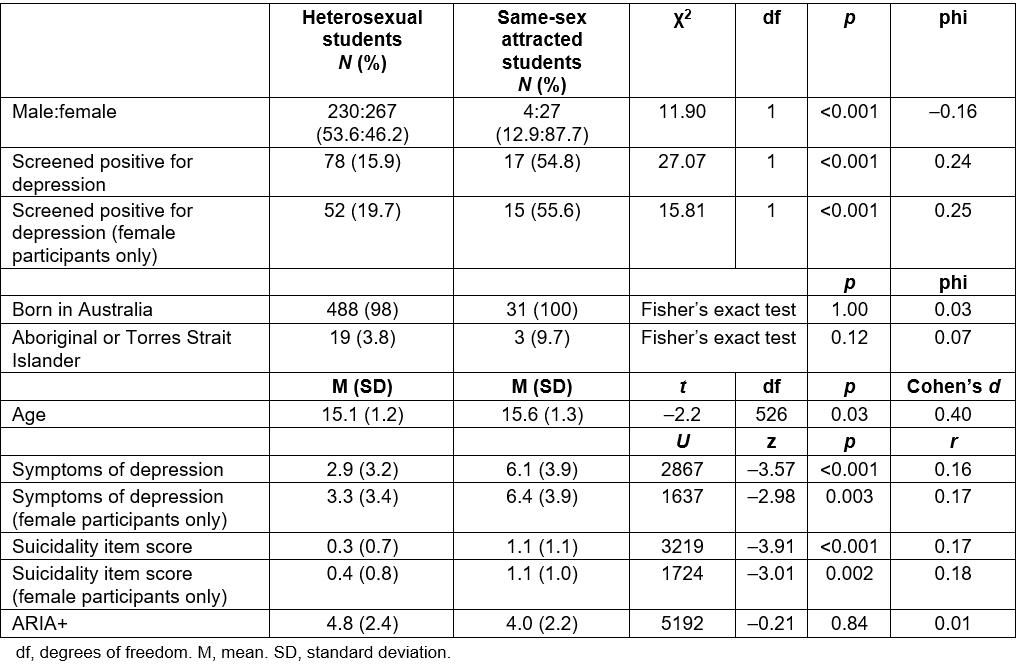
Depression and suicidality
As hypothesised, a Mann–Whitney U-test indicated a small and significant difference in KADS-6 scores between same-sex attracted and other adolescents. Same-sex attracted adolescents reported more symptoms of depression (mean=6.1, SD=3.9) than other adolescents (mean=2.9, SD=3.2). Further, more same-sex attracted adolescents screened positive for depression (54.8%) compared to other adolescents (15.9%) and there was a significant difference in responses to the item assessing suicidality between same-sex attracted and other adolescents. Same-sex attracted adolescents reported higher levels of suicidality (mean=1.1, SD=1.1) than other adolescents (mean=0.2, SD=0.7; Table 1).
As the majority of same-sex attracted participants were female, and given the higher overall rates of depression and suicidality among female adolescents compared with male adolescents, the relationships between symptoms of depression, screening positive for depression and suicidality were analysed for female study participants only. The same pattern of small and significant differences in KADS-6 scores, suicidality item scores and screening positive for depression were found (Table 1). There were insufficient numbers of male participants identifying as same-sex attracted to undertake this analysis for males.
Experiences of stressors
As predicted, same-sex attracted adolescents reported more experiences of stressors relating to relationships with schoolmates, teachers, parents and siblings, bullying at home and physical assault than heterosexual adolescents (Table 2).
Table 2: Stressors experienced by participants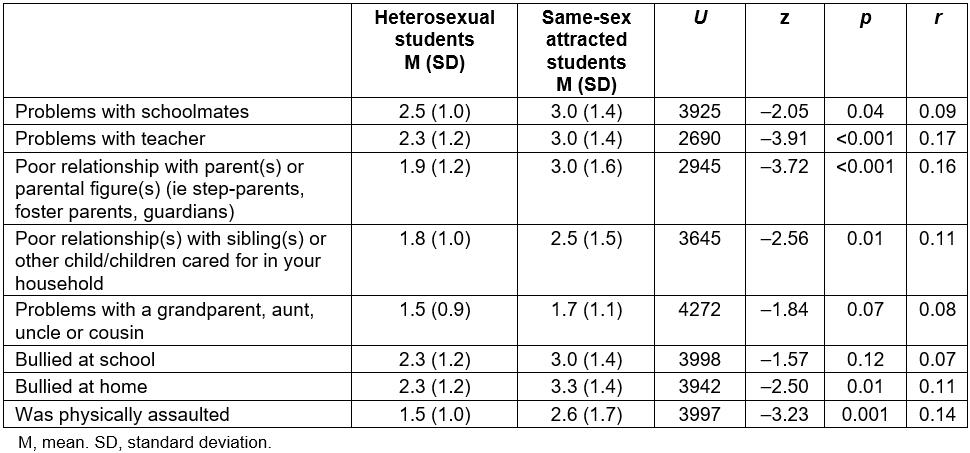
Perceptions of barriers to seeking mental health services
The hypothesis that same-sex attracted adolescents would report more barriers to seeking mental health services was not supported. Same-sex attracted adolescents did not report higher frequencies of any of the seven listed potential barriers, including being concerned about others finding out, not wanting to talk about their problems or being embarrassed about their problems. While there was a greater number of same-sex attracted adolescents who indicated that there were ‘other’ barriers, only a small number of participants wrote what this other reason was, and so this was not able to be examined further. Similarly, same-sex attracted adolescents did not report being less comfortable seeking help for a mental health problem, finding it harder to find help for a mental health problem, nor did they consider that they should be more able to deal with mental health issues without help from others (Table 3).
Table 3: Perceptions of barriers to seeking mental health services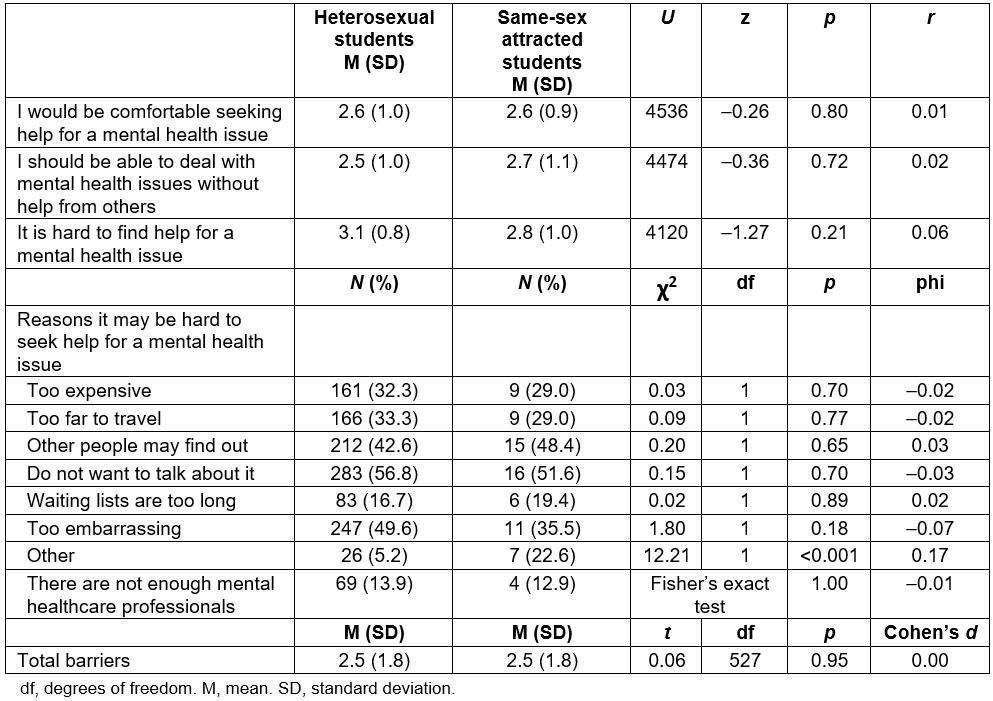
Discussion
This article reports one of very few research studies to compare the functioning of same-sex attracted and heterosexual adolescents living in rural Australia. First, the current study aimed to examine symptoms of depression in adolescents who identified as same-sex attracted living in rural Australia. As anticipated, same-sex attracted adolescents reported greater symptoms of depression, higher rates of screening positive for depression and higher levels of suicidality than other adolescents living in rural Australia. As only a small number of males identified as same-sex attracted, additional analysis of data from just female participants was undertaken and showed the same pattern of results when comparing female same-sex attracted adolescents to other female adolescents. The effect size for differences in depression symptoms in the current study was small (r =0.16, r=0.17 for female participants only). This is consistent with a recent meta-analysis finding the mean difference to be small in studies comparing depression symptoms between sexual minority youth and heterosexual youth (d=0.33)6. These findings are also consistent with North American research with rural sexual minority adolescents7. Although the aim of the present study was not to compare functioning between rural and city living adolescents, findings do suggest higher rates of depression among the rural-living participants of the present study, when compared with adolescents living in cities. Australian research has found gay-identified men living in rural and remote areas to have lower wellbeing than those in urban areas14, and, consistent with this, the overall rates of depression were higher for rural adolescents in the present study than rates of depression reported for adolescents living in Adelaide, the capital city of South Australia. The proportion of rural adolescents from the present study screening positive for depression was higher for both same-sex attracted adolescents (54.8%) and other adolescents (17.8%) than a comparable study of adolescents recruited through schools by the present research group in the city of Adelaide, South Australia (9.2%)26. This study used a different measure of depression, and participants did not identify whether they were same-sex attracted, and so further work that recruits from both city and rural areas is needed to make direct comparisons between urban and rural youth mental health outcomes according to sexual orientation.
Written parental consent was required for all adolescents. This required paper-based consent forms and study information sheets to be taken from school to home, and then returned to school staff. Low participation rates when this approach to recruitment is used is common and, although the authors used some strategies recommended for improving response rates such as promoting the research directly to principals, and having a member of the research team closely monitoring the research process by telephone and visiting some high schools, there were no reminder contacts, direct contact with parents or incentives for participation as this was beyond the resources of the project27. In addition, the authors recruited from schools across the state and did not have the resources to be physically present at all schools. As a result of low participation rates, it is likely that rates of symptoms of depression and suicidality are higher than reported as the students less likely to participate in studies requiring active parental consent are students who are truant, from minority groups, lower socioeconomic status, or who engage in risky health behaviours27. These students groups are likely to be at greater risk of depression and suicidality. As noted by Wolfenden et al27, students from minority groups are less likely to have participated in the present study. Recent estimates indicate that up to 11% of Australians may have a diverse sexual orientation, sex or gender identity28. Given the low number of same-sex attracted male students who participated (1.7% of male participants) it is likely that this group of students participated at a much lower rate than same-sex attracted female students. Given this issue, the authors reported findings separately for female students. There were insufficient male participants to provide any meaningful data for male students. As a result of this issue, the experience of same-sex attracted males students remains to be clarified, and it is recommended that future research use different approaches to recruitment to ensure these students’ experiences are considered8.
This study found that same-sex attracted adolescents experienced a greater number of relationship stressors (with schoolmates, parents, teachers and siblings), were more likely to report bullying at home, and were more likely to have been physically assaulted than their heterosexual peers. Minority stress theory proposes that stressors related to stigma and prejudice will be experienced more frequently by same-sex attracted adolescents. The present study utilised a general measure of stressors applicable to adolescents, and did not assess whether stressors experienced (eg bullying, physical assault) were perceived as related to stigma and prejudice towards participants, or whether adolescents were socially excluded or experienced a poor sense of belonging. While these stressors may well indicate social exclusion related to stigma and prejudice, this should be assessed more specifically in future work. In addition it is likely that the sense of belonging of same-sex attracted adolescents in this study would have varied, depending on their local community, as found in rural Australian men11. Nevertheless, these findings are consistent with minority stress theory. Recent Australian work has shown that adults with non-heterosexual orientation were more likely to experience mental health risk factors, with non-heterosexual orientation not a major risk factor for long-term mental health outcomes29. However, this has yet to be tested in adolescents. Authors of a recent meta-analysis of disparities in depression and suicidality between sexual minority and other adolescents6 reported strong evidence for victimisation being a significant mediator between sexual orientation and depression. While the present study was not sufficiently powered to test this, the higher rates of relationship stressors, bullying and physical assault among same-sex attracted adolescents suggest that this may also be a mediator of depression among rural adolescents. Prevention strategies to reduce victimisation may play a key role in the reduction of mental health problems among same-sex attracted adolescents.
This study also found, contrary to predictions, that same-sex attracted adolescents did not report more barriers to seeking mental health support, or more negative perceptions about seeking support. While this potentially reflects well on current health and counselling services in rural South Australia, and may reflect changes in public understanding and acceptance of same-sex attracted individuals4, the higher number of same-sex attracted adolescents who reported an ‘other’ barrier suggests that more in depth, qualitative research with this population may uncover barriers not examined in the present study. Of concern though is that, for both groups of adolescents, the three most frequently reported barriers to seeking support were that they did not want to talk about it, that other people may find out and that they were too embarrassed, suggesting that these issues are of concern for all rural adolescents, and that further work is needed to reduce barriers to seeking support for all rural adolescents.
Due to the modest sample size and likelihood that male students who were same-sex attracted either did not participate in the study or chose not to identify as same-sex attracted, the authors did not have sufficient numbers of participants to further examine outcomes for male students, nor was it possible to consider sexual minority status in a more finely grained manner (eg including transgender and bisexual adolescents). Several school principals chose not to participate in the present research due to the nature of the survey questions, and this issue would need to be considered in taking this research further. Moreover, adolescents who were not attending school were not included in the present study. This group of young people may be more likely to be experiencing poor mental health (a potential reason for non-attendance). Future work should endeavour to include these young people by using additional recruitment strategies, as already discussed. Further, the authors did not have sufficient numbers of participants to examine relationships between mental health outcomes and degree of rurality; previous work suggests that there may be significant differences in the experiences of young people living in regional, rural or remote areas8 and this should also be considered in future work. This is important given that research with adult women living in rural South Australia reported that access to the city of Adelaide, and the social opportunities that afforded, supported their developing understanding of their sexuality12.
While the authors used a psychometrically sound measure of symptoms of depression, the need to minimise the burden on participants who completed a range of measures in this study meant that a single item measure of suicidality from the depression scale was used. This means the measures of suicidality and symptoms of depression were not independent of each other. Single item measures of suicidality are frequently used and have been used in research with sexual minority youth (eg Ybarra, et al30. However, the use of a more comprehensive measure of suicidality that is able to examine various aspects of suicidality in future work should be considered.
Conclusions
Overall, the results of the study suggest that adolescents living in rural Australia who are same-sex attracted are much more likely to experience symptoms of depression compared to other rural adolescents. They are also more likely to screen positive for depression, and to report suicidality. A similar pattern of findings emerged when examining female participants only. These findings are concerning, but are consistent with other work indicating that same-sex attracted adolescents are at high risk of experiencing mental health problems6. The finding that same-sex attracted adolescents experienced a higher number of relationship stressors, bullying and assault underscores the need for more focus on supporting this group of vulnerable adolescents, particularly as victimisation may mediate the relationship between sexual orientation and depression. Greater focus on understanding and reducing the modifiable risk factors in rural communities is needed. While the current study did not find that same-sex attracted adolescents perceived more barriers to seeking mental health support, as all adolescents reported significant barriers to seeking help, greater understanding of same sex adolescents’ access to appropriate services in rural areas is needed to be able to improve mental health functioning in this population. In addition, addressing the wider issues (eg stigma) contributing to the greater number of stressors faced by same-sex attracted adolescents should be a priority.
