Introduction
Memorial University of Newfoundland’s Faculty of Medicine (Memorial) was established in 1967 as what could be described as a de facto rural-focused medical school1 with a social accountability mandate to serve the needs of Canada's most rural province. This study analyses the provincial and national geographic practice outcomes of Memorial’s medical school with its focus on rural generalist training compared with other Canadian medical schools and shows how Memorial and other Canadian Medical Schools have responded to the social accountability need to produce rural physicians.
Canadian medical schools are unique in their collective agreement on the importance of their social accountability, as shown in the 2001 Health Canada report ‘Social accountability: a vision for Canadian medical schools’2 and later affirmed as the foundation for their collective vision described in reports from Future of Medical Education medical degree (FMEC MD 2010) and postgraduate (FMEC PG 2012) projects3-6.
Memorial and its Faculty of Medicine were conceived as socially accountable institutions before the term was even invented. Memorial University was originally founded as Memorial College, a living memorial to the soldiers who lost their lives in World War I. Its vision deliberately acknowledges the university’s ‘special obligation to the people of Newfoundland and Labrador (NL)’.
The establishment of Memorial’s Faculty of Medicine as an independent medical school in 1967 was an audacious endeavour, given both the small, dispersed population and the limited resources at the time. Established in a ‘place like no other’, it set out to be a ‘medical school like no other’, with rural-focused experiential learning from the outset. The Canadian Medical Association Journal dedicated its June 1973 cover to the graduation of Memorial’s first medical degree (MD) class and noted: ‘It is not easy to define the essential qualities and characteristics of a medical school. It is apparent, however, that a major element of Memorial’s program for development is its desire for community involvement. The medical community includes not only the five hospitals in St. John's […] but also the regional and cottage hospitals, and the family physicians and other doctors in the province’7. First-year students were ‘[…] introduced to patients in hospital, in family practice, in community and cottage hospitals and in public health programs’8. While accepted as good medical education now, this was quite radical at the time.
The social accountability emphasis on engaging, partnering with, and responding to the needs of the people of NL has remained the core of the medical school. In 2014, the Association for Medical Education in Europe (AMEE) recognized Memorial University Faculty of Medicine with an ASPIRE-to-Excellence award for social accountability. Memorial’s current vision, mission and activities project the same focus towards the future.
Since the founding of Memorial’s medical school in 1967, there has been growing interest and effort in producing medical doctors for rural communities around the world. Often referred to as rural GPs or rural family doctors, in Canada, these are usually rural generalist medical practitioners who provide primary medical and community-oriented primary care and often hospital-based secondary care such as emergency medicine, in-patient hospitalist care, intra-partum obstetrics and, sometimes, basic anesthesia and surgery9-16. In contrast, hospital-based secondary care services in larger urban centers are usually provided by either specialists or by general practitioners with a more limited scope of practice. The Cairns Consensus Statement on Rural Generalist Medicine 2013 outlines the vital roles of the rural generalist physician and articulates training pathways to educate them for practice17.
Tesson et al1 outlined three models for training doctors for rural practice: (1) large medical schools that provide rural training streams; (2) schools that provide a focused, whole-school approach including both de facto rural schools (such as Memorial) that address the needs of rural populations as part of their geographic reach; and (3) stand-alone rural schools recently created specifically to address rural needs. The world literature contains numerous reports of optional rural undergraduate (medical degree; MD) educational streams/programs and postgraduate (PG) rural training tracks that are beyond the scope of this article to review. Outcomes from other Canadian medical school programs are aggregated in this article as the comparison group for Memorial’s whole-school approach to meet rural and regional needs.
There have been few integrated whole-school ‘pipeline to practice’ outcome reports. Northern Ontario School of Medicine (NOSM), a rural-focused Canadian medical school18,19 has reported encouraging although limited data based on its first graduates who have entered residency in 200920. The Zamboanga School of Medicine (Philippines) focuses on integrating students into underserved rural communities with an integrated curriculum as well as clinical learning in rural settings. Since its first 15 graduates in 1999, more than 160 students had successfully graduated by 2011, with over 80% practicing in local underserved regions21. James Cook University (JCU, Australia) has demonstrated promising outcomes, reporting in 2013, that 67% of JCU graduates undertook their internship outside a metropolitan center compared with 17% of others (OR: 10.0), and 47% in outer regional centres compared with 5% (OR: 16.6), respectively22. At Walter Sisulu University’s medical school (South Africa), many graduates are still completing internships or PG training, but preliminary research shows that 36% of graduates practice in small towns and rural settings23.
One of the earliest whole-school outcome reports, from the University of Tromso24, illustrated that this rural-focused medical school had a significant impact on Norway’s rural physician workforce. While this early example of success for a ‘whole-school’ approach is notable, there are no long-term outcome reports in the literature.
Memorial, like other Canadian medical schools, is a graduate-entry medical school. It provides MD education (paradoxically referred to as undergraduate) accredited by the Committee on the Accreditation of Canadian Medical Schools/Liaison Committee on Medical Education (CACMS/LCME), PG vocational residency training programs accredited by the College of Family Physicians Canada (CFPC) and the Royal College of Physicians and Surgeons of Canada (RCPSC) and accredited continuing medical education (CME: professional development for practicing physicians). Note that this Canadian medical school responsibility for MD, PG and CME is much more comprehensive than in Australasia, the United Kingdom and many other countries where undergraduate but not postgraduate training is undertaken by medical schools.
Memorial’s MD education and PG vocational residency training programs and CME are directed towards the province’s physician-resource needs including rural generalists, and to national physician-resource needs especially rural generalists. The main components of Memorial’s pathways to rural practice begin before admission to medical school and feature a rural focus throughout: MD education, Family Medicine (FM) PG residency training, and CME practice/teaching support. These are augmented by a student-led, faculty-supported Rural Medicine Interest Group (RMIG) that has been very active since its inception. The key educational interventions that are part of Memorial’s pathways to rural practice are listed in Box 1. Memorial’s comprehensive end-to-end pipeline/pathways to rural generalist practice is described and analyzed in more detail in the companion article: From pipelines to pathways: The Memorial experience in educating doctors for rural generalist practice25.
Box 1: Memorial’s pathways to rural practice interventions. 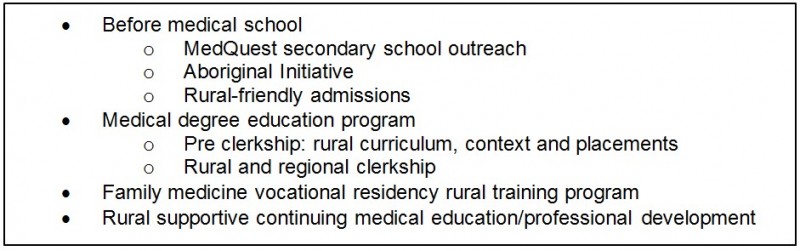
CME, continuing medical education. FM, family medicine. MD, medical degree. PD, professional development.
Regional/provincial context
Newfoundland and Labrador (NL) is Canada’s most rural province, with a population of 527 000. Of this population, 7% is Aboriginal, which include First Nation Innu (Sheshatshiu and Mushuau), First Nation Mi’kmaq (Miawpukek and Qalipu), Nunatsiavut Inuit and NunatuKavut Southern Inuit groups/nations, each with its own unique cultures and healthcare challenges. NL is 52% rural, on the basis of the Statistics Canada definition of communities of up to 10 000 people who do not reside in a metropolitan influence zone (MIZ), (meaning smaller communities where the majority of individuals commute to the larger center for work and leisure purposes are not included as rural26). This Canadian definition is much more restrictive than those used in many other countries such as Australia.
The provincial capital of St. John’s, with a population of 107 000 (the Census Metropolitan Area (CMA) including the core city plus its neighbouring locales has a population just under 200 000), which is relatively small for a city with a medical school. The second-largest city, Corner Brook, is located on the west coast of the island 800 km away from St. John’s. It has only 20 000 people (CMA 27 000). The remaining population is widely distributed in small communities spread out over 400 000 km227. The extensive dispersion of a small populace over a wide expanse of territory, confronted by sometimes severe weather conditions, makes access to medical care very challenging for the people living in the many remote isolated communities that were built around what were once rich fishing grounds.
Memorial’s tradition of developing physicians with exemplary skills for rural and regional practice, and providing distributed education at appropriate sites, has been a hallmark of the MD program from the beginning. Recognizing that rural medical education involves significant activities for both students and their teachers (rural physicians) that occur outside the tertiary care setting, the Rural Medical Education Network (RMEN) was established to provide logistical supports for both. RMEN includes over 600 family physician and other part-time specialty preceptors as well as 13 full-time faculty members. These medical teachers are all located outside St. John’s, across the province and beyond. RMEN is led by an Assistant Dean who is a rural family physician and a full-time faculty member living in a community 440 km from St. John’s (Fig1).
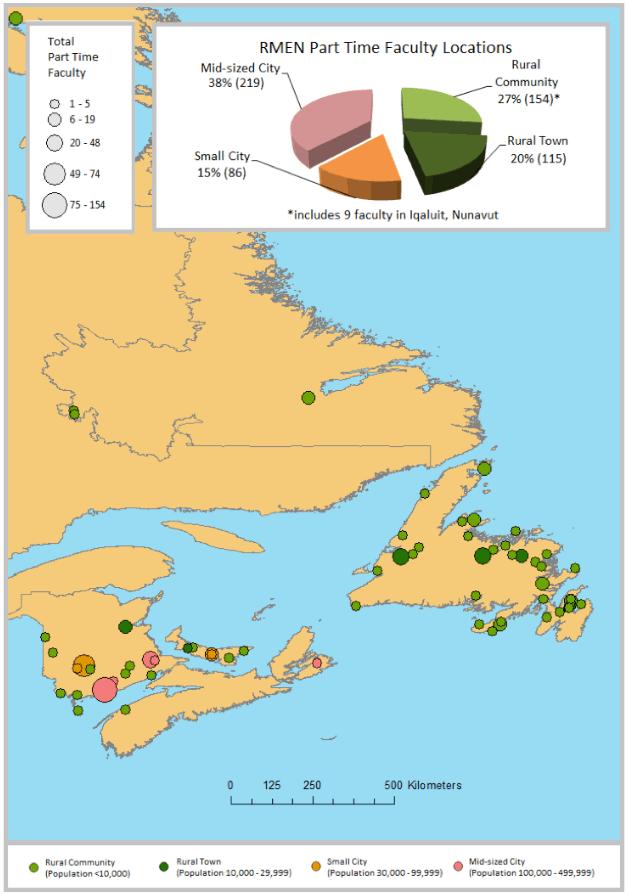 Figure 1: Map showing part time faculty locations outside of St. John’s and Halifax as of August 2015; symbol size indicates total number of part-time faculty at each location.
Figure 1: Map showing part time faculty locations outside of St. John’s and Halifax as of August 2015; symbol size indicates total number of part-time faculty at each location.
Hypothesis
This article tests the hypothesis that Memorial is more effective than other Canadian medical schools in producing physicians for its region (province), and in producing rural physicians for Canada.
Methods
Data source
The data source was the Canadian Post-MD Education Registry (CAPER) Database.
In Canada, medical organizations across different levels of government and jurisdictions established a partnership known as CAPER that collects PG education data for all Canadian-trained physicians. Census data are collected annually from all 17 Canadian medical schools, and includes sociodemographic data, data related to the distribution of medical PGs across Canada, number and specialty type of Canadian medical graduates (CMGs) and international medical graduates (IMGs) among other collected data. For the purpose of this study, practice-location data at both national and provincial levels for CMGs and IMGs who completed their PG training in Canada during the 2004 to 2013 period were provided courtesy of CAPER (the most recent available at the time of the study).
Study design
The authors conducted a retrospective cohort study using secondary data from CAPER. Every physician practicing in Canada who had completed their PG training in Canada between 2004 and 2013 was followed from the time they were awarded their MD up until 2 years after completing their PG training. Practice locations were determined 2 years after they completed their PG training and were cross-referenced by the medical school where they completed their MD or PG training or both their MD and PG training. The same approach was used for a subset of physicians who completed FM PG training.
Study population
The study population included physicians who completed their PG training between 2004 and 2013 in Canada. In this study, CMGs are physicians who completed both their MD and PG training in Canada and IMGs are physicians who completed their PG training in Canada but completed their MD outside of Canada.
Study variables
Canadian MD and PG Training Location: Canada has 17 medical schools that are unevenly distributed among its 10 provinces; the majority can be found in major population centres. Five of these seventeen Canadian medical schools are the only institution in their respective province (Fig2).
For the purpose of this study, MDs and PGs from every medical school were categorized into three groups based on the university they received their MD or their PG training or both their MD and PG training (Fig3). Using the same approach, the authors categorized FM graduates into the same categories (Fig4). IMGs who completed their PG training in Canada were also classified into the same three categories; however, for the PG by MD and FM by MD categories, they were listed as IMGs as their MD was completed outside of Canada.
Practice location: Practice locations of all Canadian PG-trained physicians were georeferenced and assigned to three geographic classes determined by CAPER (large urban, small city/town and rural). CAPER geographic classifications included: (1) large urban (≥100 000); (2) small city/town (10 000–99 000) and rural (<10 000); data for which were derived using postal codes and census geographic information.
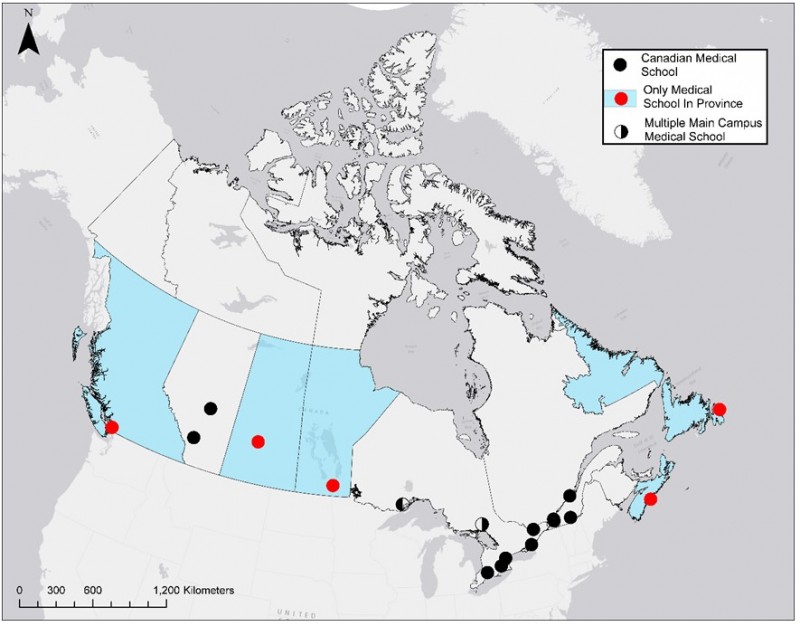 Figure 2: Canadian medical school locations.
Figure 2: Canadian medical school locations.
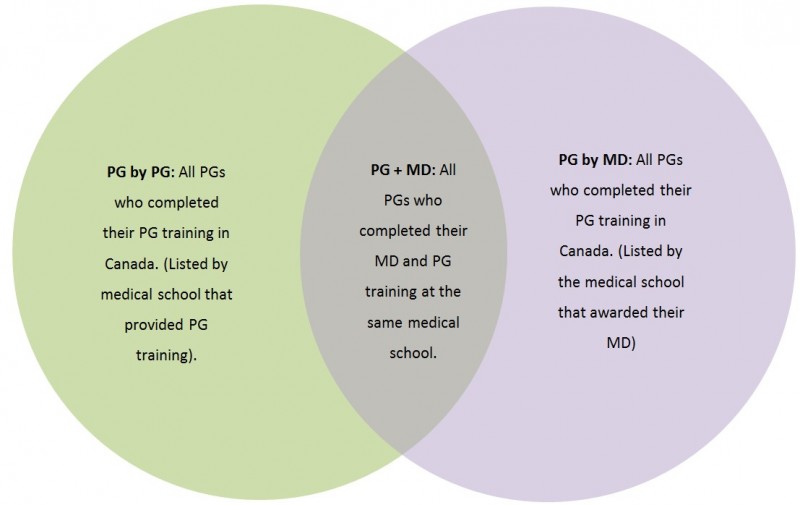 Figure 3: Canadian medical graduate types and their relationship.
Figure 3: Canadian medical graduate types and their relationship.
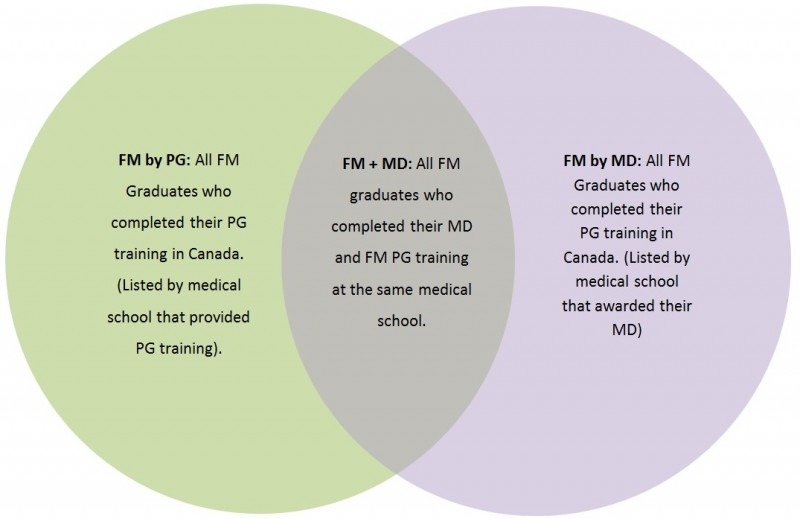 Figure 4: Canadian Family Medicine graduate types and their relationship.
Figure 4: Canadian Family Medicine graduate types and their relationship.
Statistical analysis
Statistical analysis was performed at two distinct levels. (1) Provincial-level analysis considered the total number of graduates practicing in the same province in which they completed their PG training and/or received their MD by the total number of Canadian PG-trained graduates practicing in that province from the same timelines. The same was applied for the total number of Canadian PG-trained graduates practicing rurally by the total number of Canadian PG trained graduates from the same timelines in each province. Only provinces with a single medical school were considered so that a direct comparison could be made between Memorial and other medical schools in terms of their ability to provide the workforce for the province in which they are situated. A series of two-sample proportion tests as well as odds ratios were applied between Memorial and other universities where they are the only medical school. (2) National-level analysis considered all 17 medical schools and examined the percentage of graduates practicing in rural Canada 2 years after completing their PG training by the university where they completed their PG training and/or MD. Another set of two-sample proportion tests were applied to compare Memorial’s graduates and the national average for each graduate type as well as odds ratios.
Statistical analyses were performed using STATA SE (www.stata.com). Significance was assigned where p-values were less than 0.05. Confidence intervals for odds ratios were calculated using the Cornfield method. Odds ratios and proportion tests were performed to assess both the differences and the ratio of the proportions.
Ethics approval
As the interventions were part of the medical school program and de-identified administrative data are reported, ethics approval from the Health Research Ethics Authority (HREA) was not required for publication.
Results
Overview
There was a total of 18 766 physicians practicing in Canada that completed Canadian PG training between 2004 and 2013, where 8091 (43%) completed FM training (Table 1). There were 1254 physicians practicing rurally and, of those, 1076 (86% of rural physicians) were family physicians. There were 379 graduates practicing in Canada that completed Canadian PG training at Memorial between 2004 and 2013, where 208 (55%) completed FM training. There were 72 physicians practicing rurally and, of those, 56 (26.9% of FM graduates) were family physicians (Table 1).
For the province of Newfoundland and Labrador, 65.7% of all practicing graduates from the same timelines did their PG training at Memorial and made up the majority of physicians for both rural and total number of practicing graduates as seen in Table 2.
Table 1: Practice locations in Canada for all postgraduate (PG)- and family medicine (FM)-trained graduates 2 years after completing PG training at Memorial and at other Canadian medical schools (2004–2013)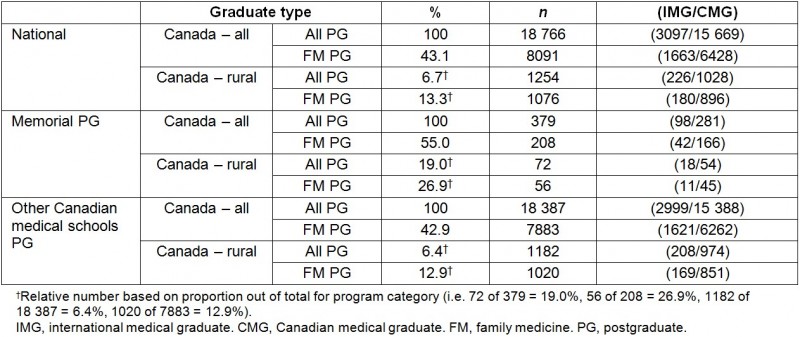
Table 2: Practice locations in Newfoundland and Labrador (NL) for all postgraduate (PG)- and family medicine (FM)-trained graduates 2 years after completing PG training at Memorial and at other Canadian medical schools (2004–2013)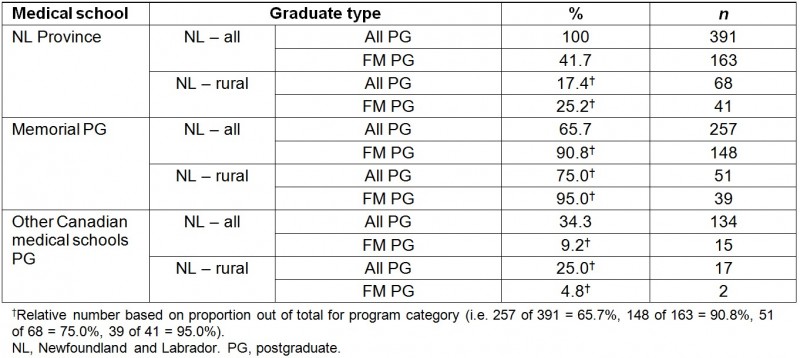
Provincial level
Memorial is one of five universities that are the only medical school in their respective province. When comparing Memorial to these four other universities with regard to the percentage of all graduates practicing in the province who received their PG training and/or MD in the same province, Memorial provided a higher percentage for all categories of graduates in terms of the total number of physicians practicing in the province (Tables 3,4; Figs5, 6). Memorial also had a higher percentage of rural practicing physicians when compared with the average of other single medical schools except for PG by PG (Tables 3,4; Figs5,6). Two-sample proportion tests demonstrate Memorial provided a much larger proportion of its provincial physician resource supply than the other four single provincial medical schools, by medical school MD for FM (72.4% vs 44.3%, p<0.000) and for overall (63.2% vs 43.5%, p<0.000), and by medical school PG for FM (90.8 % vs 72.0%, p<0.000). Medical school PG for overall was the same (65.7% vs 65.9%, p=0.520). Memorial was significantly higher for the rural FM proportion of the total study FM cohort in province by medical school MD (13.5% vs 6.9%, p=0.001) and by medical school PG (23.9% vs 11.3%, p<0.000) and similarly for overall rural proportion of total study cohort in the province by medical school MD (7.9% vs 3.5%, p<0.000) and by medical school PG (13.0% vs 5.4%, p<0.000) (Tables 3,4). The authors also found that 95.1% of FM graduates practicing rurally in NL received their PG training at Memorial vs 73.0% from other single medical schools in their provinces (p=0.001) and 53.7% of FM graduates practicing rurally in NL received their MD at Memorial vs 44.4% from other single medical schools in their provinces (p=0.134). Memorial graduate provincial retention was not significantly different than the average of the four other single medical schools for every graduate type except for FM by MD, which was found to be significantly better (63.1% vs 55.6%, p=0.026) (Table 5).
Table 3: Percentage and odds ratio (OR) out of total cohort in province for graduates practicing in the province who received their training in the same province – training by graduate type (Memorial vs other single medical schools (n=4))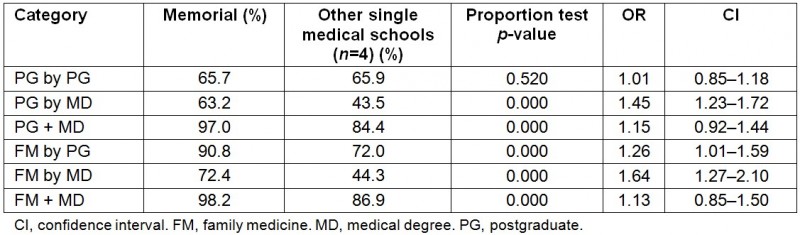
Table 4: Percentage and odds ratio (OR) out of total cohort in province for graduates practicing rurally in the same province in which they received training – by graduate type (Memorial vs other single medical schools (n=4))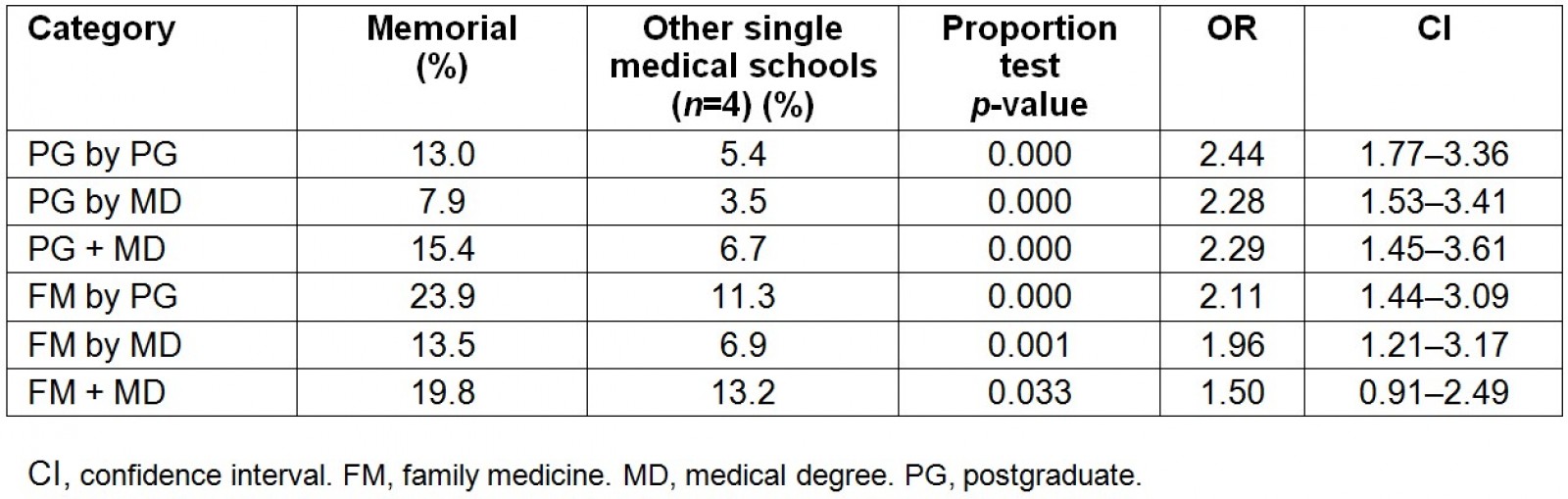
Table 5: Percentage and odds ratio (OR) for provincial graduate retention by graduate type (Memorial vs other single medical schools (n=4))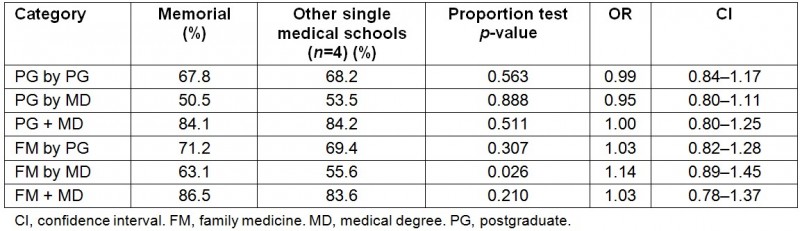
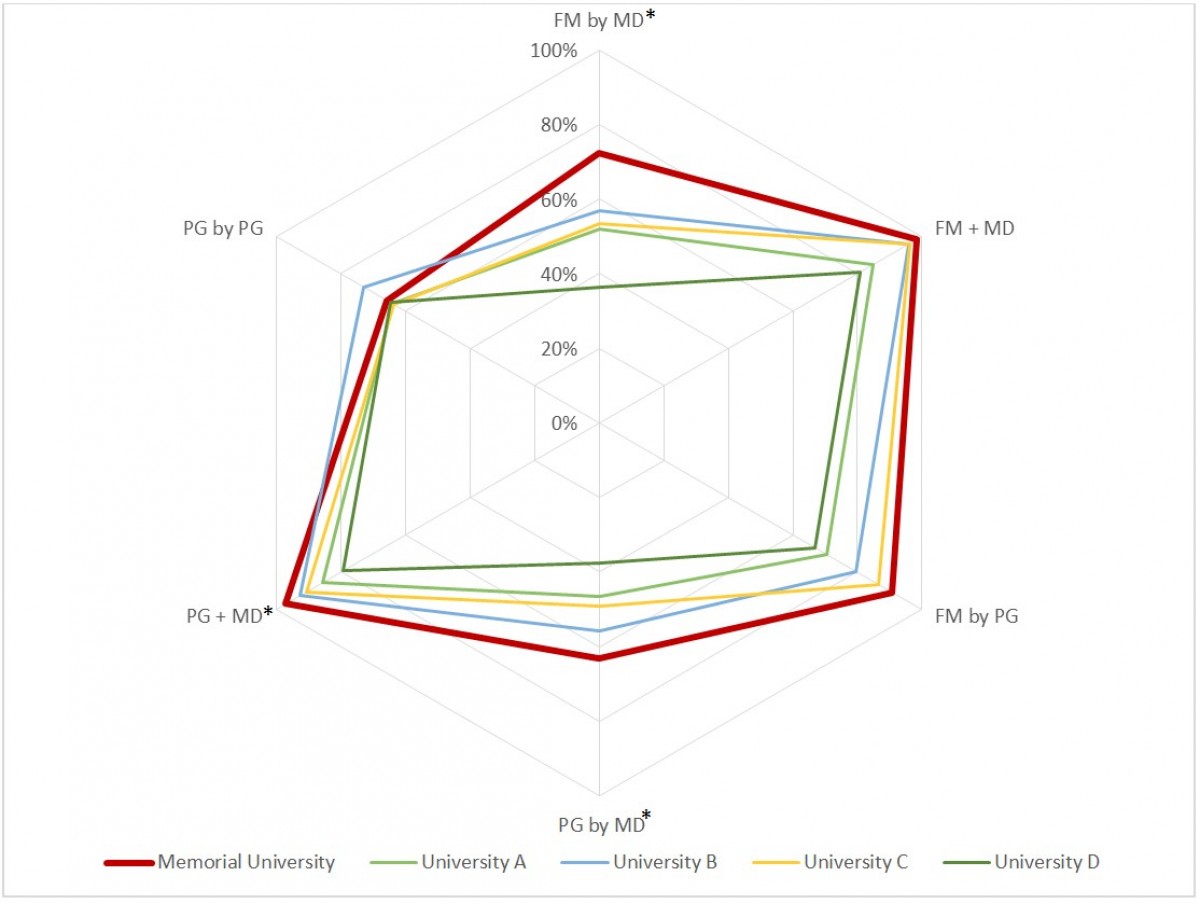 Figure 5: Percentage of all graduates practicing in the province who received their training in the same province – training by graduate type. *Memorial significantly different than other medical schools (two-sample proportion test p-value < 0.05).
Figure 5: Percentage of all graduates practicing in the province who received their training in the same province – training by graduate type. *Memorial significantly different than other medical schools (two-sample proportion test p-value < 0.05).
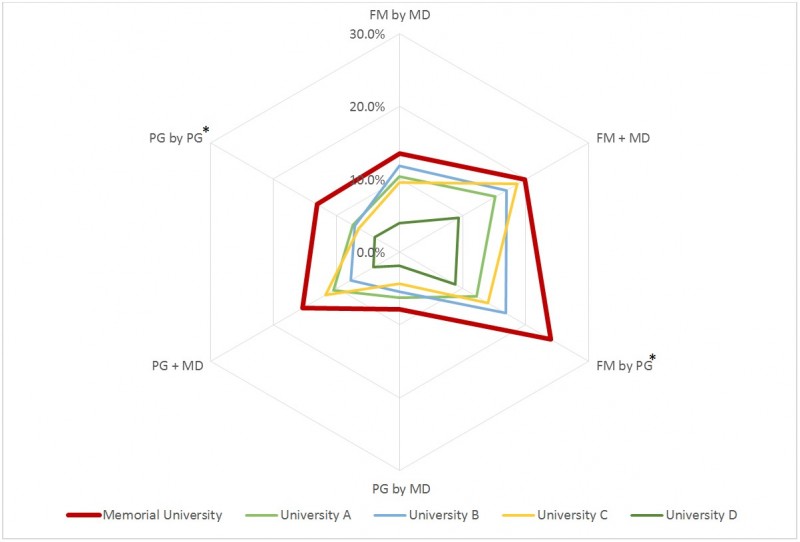 Figure 6: Percentage of graduates practicing rurally in the province who received their training in the same province – training by graduate type.*Memorial significantly different than other medical schools (two-sample proportion test p-value < 0.05).
Figure 6: Percentage of graduates practicing rurally in the province who received their training in the same province – training by graduate type.*Memorial significantly different than other medical schools (two-sample proportion test p-value < 0.05).
National level
At the national level, the percentages of all Memorial PGs practicing rurally 2 years after completion of PG training for all PG categories were significantly better than the national average, which can be seen in Figure 7 (see values listed in Table 6). The percentage of rural FM-trained physicians were significantly higher for Memorial compared with the national level (Table 6, Fig8). The two-sample proportion tests for each type of Memorial graduate indicated that each is significantly different than the national average for all categories (Table 6). Memorial was not found to be significantly different than other Canadian medical schools that had the highest percentages of those practicing rurally for FM + MD (p<0.051), FM by PG (p<0.467) and PG by PG (p<0.479).
When considering specialists who practice rurally, Memorial is the best performing medical school for all categories as illustrated in Fig9 (values listed in Table 6). The two-sample proportion tests for each type of Memorial specialist graduate also indicated that each is significantly better than the national average for all categories (Table 6).
Table 6: Percentage of physicians practicing rurally 2 years after exiting post-undergraduate (MD) training by graduate type (2004–2013)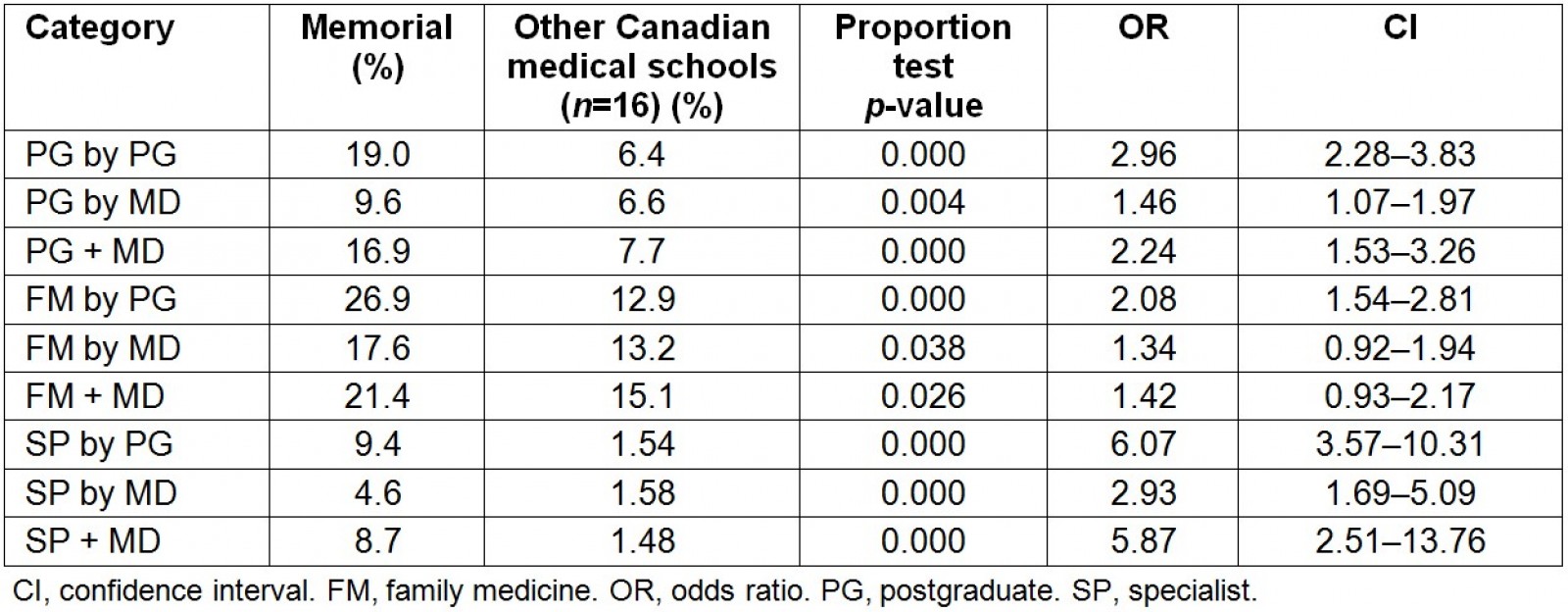
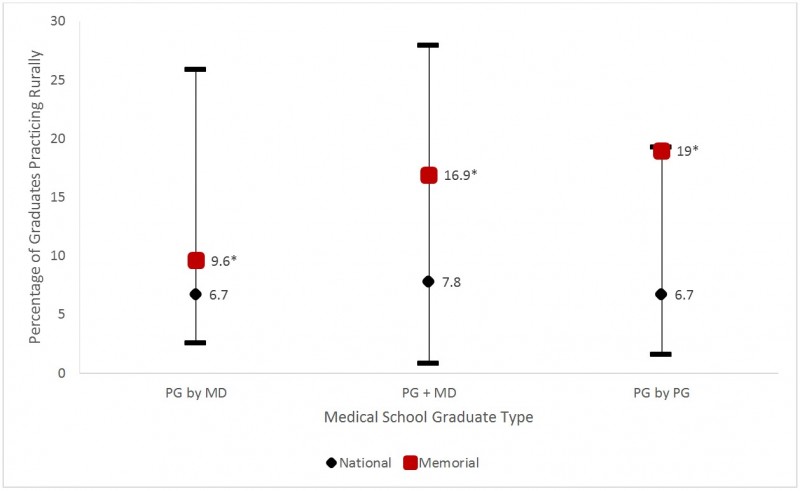 Figure 7: Percentage of all Canadian Medical Graduates (CMGs) practicing rurally 2 years after exiting post-undergraduate (MD) training by graduate type (2004–2013). *Memorial significantly different than national average (two-sample proportion test p-value < 0.05).
Figure 7: Percentage of all Canadian Medical Graduates (CMGs) practicing rurally 2 years after exiting post-undergraduate (MD) training by graduate type (2004–2013). *Memorial significantly different than national average (two-sample proportion test p-value < 0.05).
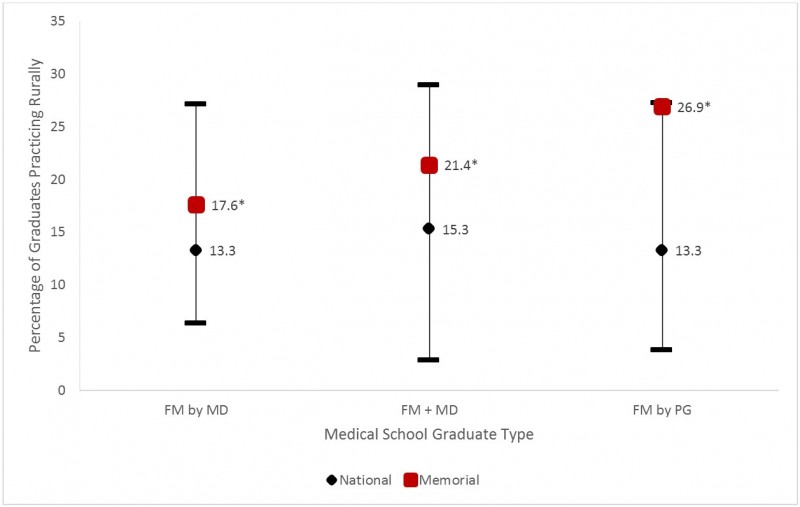 Figure 8: Percentage of family medicine (FM) Canadian medical graduates (CMGs) practicing rurally 2 years after exiting post-undergraduate (MD) training by graduate type (2004–2013). *Memorial significantly different than national average (two-sample proportion test p-value < 0.05).
Figure 8: Percentage of family medicine (FM) Canadian medical graduates (CMGs) practicing rurally 2 years after exiting post-undergraduate (MD) training by graduate type (2004–2013). *Memorial significantly different than national average (two-sample proportion test p-value < 0.05).
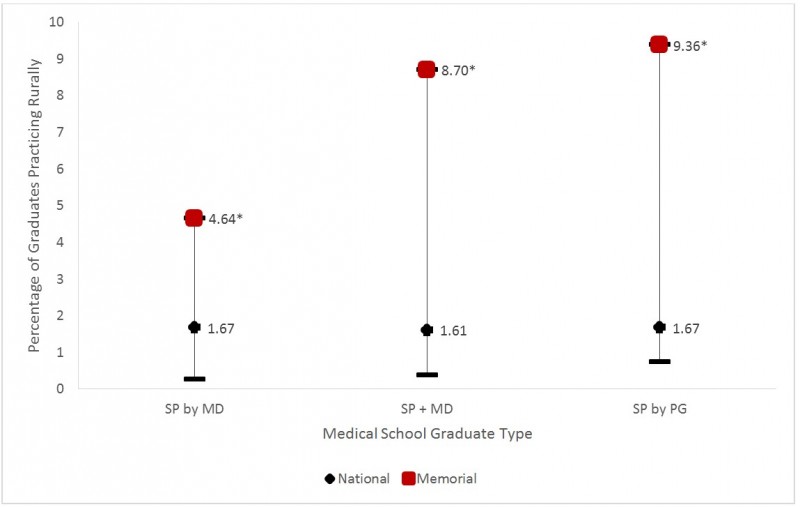 Figure 9: Percentage of all specialist Canadian medical graduates (CMGs) practicing rurally 2 years after exiting post-undergraduate (MD) training by graduate type (2004–2013). *Memorial significantly different than national average (two-sample proportion test p-value < 0.05). **Northern Ontario School of Medicine (NOSM) was not included in this chart since they had yet to implement programs that produced specialist graduates at the time of the study.
Figure 9: Percentage of all specialist Canadian medical graduates (CMGs) practicing rurally 2 years after exiting post-undergraduate (MD) training by graduate type (2004–2013). *Memorial significantly different than national average (two-sample proportion test p-value < 0.05). **Northern Ontario School of Medicine (NOSM) was not included in this chart since they had yet to implement programs that produced specialist graduates at the time of the study.
Discussion
The findings from this study illustrate that the majority of Memorial graduates are establishing practice in rural areas both locally and nationally, and that the majority are staying in NL. Proudly, the medical school founders’ vision to build a medical education program based on NL's unique geography, demography and healthcare needs is being realized.
Provincial impact
This study analysis of CAPER data found that most physicians who set up practice in NL after Canadian PG training completed their PG training at Memorial (overall 65.7%) as well as those who established rural practice (75.0%). Of those who established practice in NL after FM PG training, 90.8% had completed their FM PG training at Memorial and for those who established rural family practice in NL, 95% were trained at Memorial.
Of the physicians in practice in NL after completing PG training in Canada, 63.2% did their MD at Memorial and 65.7% did their PG training at Memorial. In the other four provinces with only one medical school, the proportional contribution of their MDs averaged 43.5% and 65.9% for those who completed PG training. In terms of the percentage of graduates who have established practice in a rural area in the same province they received their PG training, MD or both, Memorial is significantly better than the four other single medical schools with OR 1.5–2.44 (Table 4). Memorial’s contribution to its provincial physician workforce is significantly higher than other Canadian medical schools to theirs. Memorial has been able to strike a functional balance between producing specialists and rural family doctors to address the needs of Newfoundland and Labrador.
A high percentage of Memorial graduates established practice in NL. There is very little difference when comparing Memorial’s MD and PG programs with that of the four other provinces with a single medical school with regard to physicians who train in their province who also establish their practice in the same province (Table 5). This is remarkable given the larger diversity and volume of opportunities available elsewhere in Canada compared with what is available in NL, the relative free movement of physicians from province to province as a result of similar licensing requirements. Newfoundland and Labrador has a population of only 528 thousand compared with the four other provinces with a single medical school, which have populations of 924 thousand, 1.13 million, 1.28 million and 4.6 million. Other provinces have been more successful than Newfoundland and Labrador in attracting and retaining physicians who completed their MD or PG training in other provinces in addition to their own provincial medical school(s).
It is important to note that there was a total of 81 IMGs in this cohort of graduates practicing in NL. These IMGs were physicians who completed their PG training at a Canadian medical school between 2004 and 2013 but had obtained their MD outside of Canada. Of the 81 IMGs, there are 25 (31%) practicing FM, 23 (28%) are practicing in rural NL, and 9 (11%) are practicing FM in rural NL. Memorial trained 54 (67%) of the 81 IMGs who were found to be practicing in NL during the study period and this demonstrates the effectiveness of Memorial PG programs to produce physicians for the province.
Other research has found those excellent rural practice outcomes are continuing as 42% of 2011 and 2012 Memorial MD graduates practicing FM were practicing in rural communities or rural towns in 201528.
This study is consistent with provincial licensure data analysis. By 2014, four out of five fully licensed physicians in NL were Memorial graduates (based on the extrapolation of licensure study data) (Fig10)28-31. Of the 180 who are not Memorial graduates, approximately 100 of those received their PG residency training at Memorial. Many of the Memorial MD specialist physicians have established full-scope generalist specialty practices in NL’s rural and regional centres, while those in St. John’s actively support those in rural practice building on their knowledge and learning experience gained at Memorial MD and residency training programs. Of the 305 Memorial MDs that were practicing FM in NL in 2015, 112 (36.7%) were practicing in rural communities and rural towns (Fig11)28-31.
Nevertheless, there still remains more to be done, especially to improve the transition from vocational FM training into rural practice as well as the healthcare teams, facilities and networks that support rural practice. This action will require ongoing collaboration with governments, medical associations, health authorities, communities and their physicians to develop improved recruitment and retention supports to make rural practice more inviting and sustainable32-37.
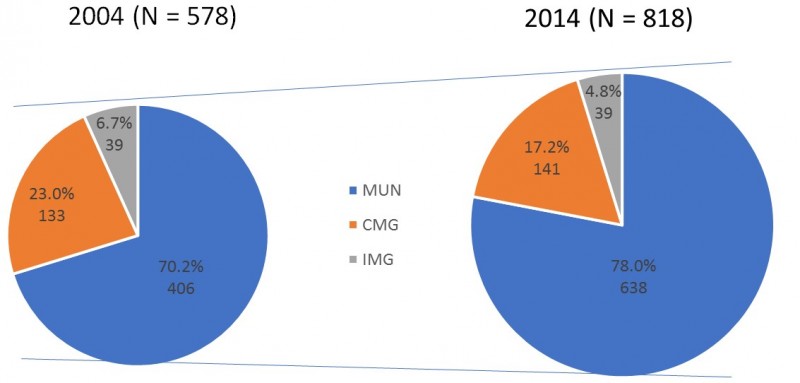 Figure 10: Fully licensed physicians practicing in Newfoundland and Labrador (2004 and 2014).
Figure 10: Fully licensed physicians practicing in Newfoundland and Labrador (2004 and 2014).
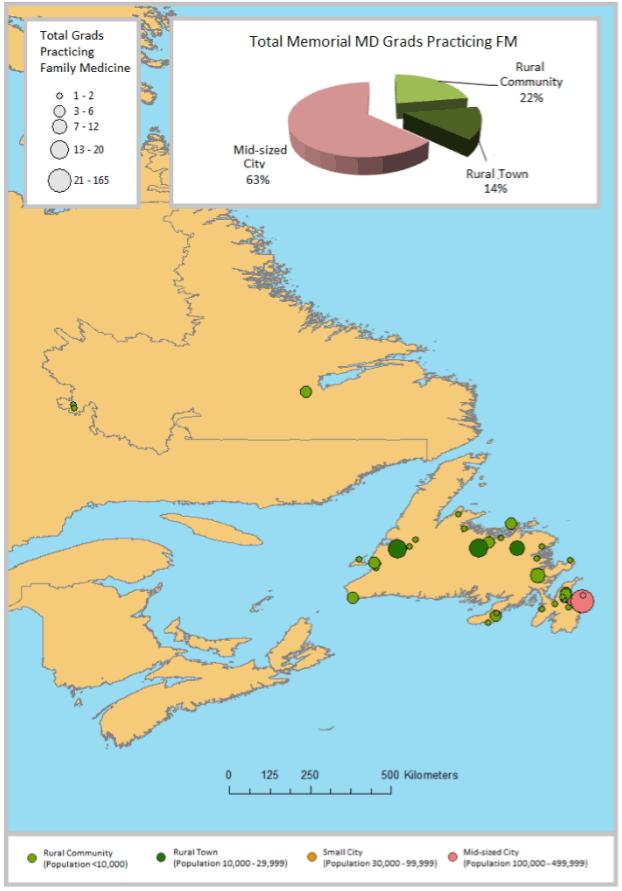 Figure 11: Map showing locations of all Memorial undergraduate (MD) graduates currently practicing family medicine (FM) in Newfoundland and Labrador as of January 2015; symbol size indicates numbers of Memorial MD graduatess practicing at each location; n=30528.
Figure 11: Map showing locations of all Memorial undergraduate (MD) graduates currently practicing family medicine (FM) in Newfoundland and Labrador as of January 2015; symbol size indicates numbers of Memorial MD graduatess practicing at each location; n=30528.
National impact
According to the Canadian Medical Directory, of all Memorial MDs practicing in Canada as of January 2015, 324 of 1584 (20.5%) were practicing in rural communities and rural towns. Of those who were known to be practicing FM anywhere in Canada, 172 of 517 (33.3%) were practicing in rural communities and rural towns.
Based on analysis of CAPER data, the authors found significantly higher proportions of physicians practicing rurally for graduates who completed their MD and/or PG training at Memorial practice compared with graduates from other Canadian medical schools.
The effect was greatest for those who did their PG training at Memorial (19.0% vs 6.4%) and the subset who did their FM PG training at Memorial (26.9% vs 12.9%). Memorial was also found to be significantly better at producing rural practicing graduates for all categories including all specialist graduate types with OR 2.93–6.07 (Table 6).
This study shows that Memorial’s programs are much more effective at graduating physicians who establish rural practice. Although this study did not look at retention of graduates in rural practice, there is corroborating evidence that Memorial graduates do stay in rural practice. The most useful national outcome data in Canada on retention of graduates in rural practice related to medical school rural education programs are published by the Society of Rural Physicians of Canada (SRPC) as the Keith award, presented at their annual meetings. The SRPC collects and analyzes robust data from the Canadian Medical Association database as well as from CAPER to determine Keith Award recipients based on the number of FM physicians practicing rurally in Canada 10 years after graduation from FM-training programs. Memorial most recently won the Keith award in 2016 (38.9% vs national average: 18.8%), 2013 (43.8% vs national average: 20%), and 2010 (52.0% vs national average: 20.9%)28.
Limitations
Although the literature traditionally uses the term ‘pipeline to practice’, Memorial developed a more flexible ‘pathways’ approach, recognizing the different paths that people take through their life in choosing rural practice. Although specific professional and personal pathways may differ from one individual to the next, common points of decision making involve: pre-medical school influences; medical school experience; PG residency training; physician practice; community/social factors (e.g. schools, recreational facilities, partner support services); relationships/marriage/children; and other lifestyle choices. This study did not include the relationships of these factors in the geographic analysis of practice locations.
This study analyzed all those who established practice and completed PG training in Canada and as a result did not include IMGs who completed both their MD and PG training outside Canada but went straight into practice. The geographic classification by CAPER that was used for this study fits with the standard Canadian geographic classification and helped determine rural and overall workforces for each medical school and province. This definition is much more restrictive compared with that of other countries that include larger population centres as rural.
One might suggest multiple comparisons tests to verify whether or not certain graduate types are truly significant. After accounting for the number of comparisons for each program type, there were no differences in terms of statistical significance except for the following graduate types: FM + MD in provincial level analysis examining graduates practicing rurally in the same province they received their MD and/or PG training; FM by MD in provincial graduate retention analysis; and both FM by MD and FM + MD in national level analysis.
This study took place in Canada, where medical schools provide both MD and postgraduate PG training that is extensively integrated. This study shows that medical school MD programs and PG programs make a significant difference to where graduates establish practice in terms of provincial and rural locations. Caution should be used when extrapolating these results to other countries where undergraduate but not postgraduate training is provided by medical schools. The authors were unable to individually compare Memorial outcomes with specific program outcomes at each of the other 16 Canadian medical schools since they did not have access to detailed comparative program information at the other schools.
Conclusion
This study shows that a rural-generalist-focused medical school and FM program can be very effective at producing the physicians needed for its region’s workforce and also be a leader in training rural generalist physicians for its nation. The analysis of national- and provincial-level CAPER data demonstrates successful outcomes for Memorial’s social accountability commitment to the needs of the province and rural Canada. This study also illustrates Memorial’s ability to balance the training of both specialists and rural family doctors, the majority of which stay in NL to practice. Memorial graduates were found to be more likely to establish practice in rural areas at the national level for most program types compared with other Canadian medical school graduates. This supports Memorial’s recognition as a Canadian leader in producing physicians for rural generalist practice. Memorial graduates occupy a larger portion of practicing graduates in NL (both overall and rural) than other single medical school graduates in their provinces. This study demonstrates the importance and strength of a comprehensive social accountability approach to develop medical education to specifically address the rural and generalist needs of regions and nations.