Introduction
In addition to the need to reduce maternal deaths1, addressing the relatively high prevalence of maternal morbidity (which covers the period of pregnancy, delivery, and six weeks postpartum)2 is a challenge for Indonesia. Previous studies have reported slower improvement in achieving Millennium Development Goals in maternal health3,4, and an increasing self-reported maternal morbidity in Indonesia2,5. Indonesia is one of 10 countries that contributes almost 60% of maternal deaths worldwide6 and therefore maternal mortality has been the focus of many health programs in Indonesia. These programs include the launching of Alert Husband and Alert Village programs7-9. With the increasing burden of maternal morbidity, the focus should extend beyond reducing maternal deaths to include improvement of overall health and quality of life of Indonesian women10,11.
Indonesia is one of the world’s biggest archipelagos, with more than 260 million people living in 34 provinces12. Geographical barriers are a major challenge to distribution of healthcare access and dissemination of public health programs13-15. The significant differences in rural and urban areas beyond socioeconomic status compound the problem of ensuring equal access to healthcare16. Therefore, understanding the pattern of maternal morbidity in terms of geographical area is essential to design effective and specific community and hospital-based intervention. To date, there are limited data for Indonesia on the patterns of different types of maternal complications by rural/urban area and the corresponding sociodemographic factors. This study aims to describe the patterns of maternal complications and the association with sociodemographic characteristics in urban and rural settings, to provide a more specific recommendation for more effective community-based intervention in Indonesia and countries with similar settings.
Methods
This study used data from the Indonesia Demographic and Health Survey (IDHS) 20122. IDHS was a nationally representative cross-sectional survey using multistage sampling design. The present study analysed data from women who gave birth in the previous 5 years and completed the pregnancy and labor complications questions (n=12 679). There was relatively little missing data on knowledge of danger signs during the maternal period (n=7, 0.06%) and WHO standard antenatal care (ANC) (n=472, 3.7%). The present study only included data on self-reported maternal complications in the most recent pregnancy and childbirth. In the IDHS, the pregnancy complications questions included the topics of prematurity, bleeding, fever or infection, convulsion and/or other morbidities during the most recent pregnancy. Meanwhile, prolonged labor, bleeding, fever or foul vaginal discharge, convulsions, premature rupture of membrane (PROM) and/or other morbidities were included in the labor complications questions. In this study, maternal morbidity status was derived from a combination of pregnancy and/or labor complications data10. Only the morbidities during pregnancy and labor were included in the analyses, because of a data limitation for postpartum morbidity in IDHS.
All statistical analyses were conducted in Statistical Analysis System v9.4 (SAS Institute; http://www.sas.com) and were weighted to take account the IDHS sampling scheme. Chi-squared tests were used to assess the differences in the patterns of maternal morbidity by different sociodemographic characteristics. Multilevel mixed-effects logistic regressions were conducted to evaluate the relationship between various sociodemographic variables with maternal morbidity. The individual-level variables included age, parity, family wealth, maternal education, knowledge of maternal complications, and WHO standard ANC of four visits during pregnancy. Region was used as the community-level variable. The region was classified into three categories based on development: Java-Bali, more developed other islands and less developed other islands2,10.
Ethics approval
This study was approved by the health research ethics committee at the Faculty of Medicine, Universitas Sebelas Maret (783/IX/HREC/2016).
Results
Data were analyzed for 12 679 women (weighted n=12926), with 47.2% living in rural and 52.8% in urban areas of Indonesia. There were significant differences between rural and urban areas in all the sociodemographic characteristics assessed in this study. Women in rural areas were relatively young and had higher parity. Additionally, women from rural areas had lower family wealth and lived in the less developed region in Indonesia (Table 1). There were significant differences in knowledge of danger signs during the maternal period. Only 25.2% of women in rural areas knew about any danger signs during the maternal period compared to 34.8% of women in urban areas. Women in rural areas had significantly lower insurance membership (31.9%) than women in urban areas (42.1%).
Table 1: Sociodemographic characteristics of women in rural and urban areas of Indonesia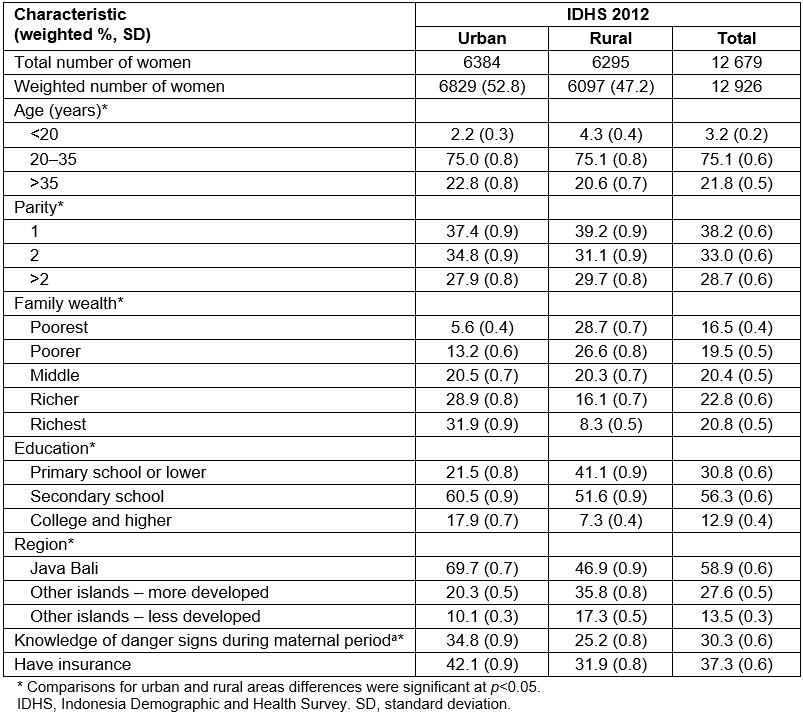
Pattern of self-reported maternal morbidity types
Table 2 shows the self-reported prevalence of maternal complication types during pregnancy and labor in IDHS 2012. Overall, 53.3% of women reported pregnancy and/or labor complications during their most recent pregnancy or childbirth. Women in rural areas reported significantly fewer maternal complications (51.3%) than women in urban areas (55.1%). Similarly, self-reported pregnancy and labor morbidities were lower in rural areas than in urban areas (Table 2).
The patterns of pregnancy morbidities were similar for rural and urban women. The highest proportion of pregnancy morbidity was the category of complications classified as ‘other’, followed by ‘bleeding’. However, women in urban areas had a significantly higher prevalence of bleeding compared to women in rural areas. There were no significant differences between rural and urban for the remaining pregnancy complications: prematurity, fever, convulsions and ‘other’ (Table 2).
There were slight differences in the types of labor morbidities. In urban areas, the highest proportion was for prolonged labor, followed by the PROM, bleeding and infection categories. In rural areas, prolonged labor and PROM were followed by the infection and bleeding categories. Compared to urban women, women in rural areas reported a higher proportion of bleeding and infection, but a significantly lower proportion of PROM and other complications (Table 2). There were no significant differences in the proportion of self-reported prolonged labor and convulsions among women in urban and rural areas.
Table 2: Self-reported morbidity types for rural and urban women in Indonesia during most recent birth 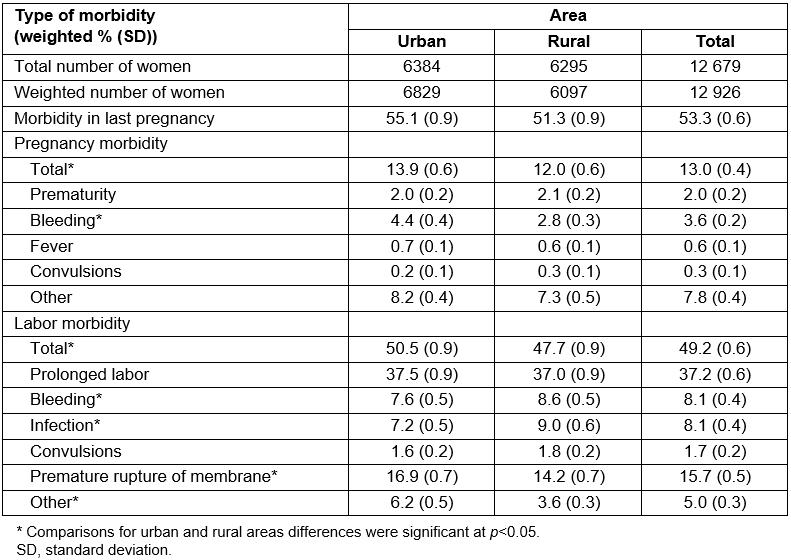
Sociodemographic pattern of self-reported maternal complications
The proportion and association of maternal complications by sociodemographic characteristics were also analyzed (Table 3). Overall, there were significant differences in the proportion of maternal morbidity by sociodemographic factor. There was a higher proportion of self-reported morbidity in women who were younger, primiparous, knew about danger signs in pregnancy, were of higher family wealth and living in Java-Bali (Table 3). In multivariate regression, only two factors were significantly associated with self-reported morbidity: parity and knowledge of maternal complications.
Table 3 shows differences in the sociodemographic pattern of maternal complications when stratified by area. For rural areas, significant differences in self-reported maternal morbidity were observed by parity, family wealth and region (p<0.05). In rural areas, a higher proportion of morbidity was reported in women of high family wealth. However, in mixed-effects regression, only parity showed significant association with self-reported complications in the maternal period. Compared to primiparous women, multiparous women were less likely to report maternal complications (adjusted odds ratio 0.8, 95% confidence interval 0.7–0.9). In contrast, there were no significant differences in the proportion of self-reported complications by family wealth in urban areas. Furthermore, although insignificant, a higher proportion of morbidities in urban areas was observed where social disadvantage was high. For urban areas, significant differences in proportion of morbidity by age, parity and region were found (Table 3). In multivariate regression, only parity and knowledge of danger signs during the maternal period were significantly associated with self-reported morbidity. Multiparous women were less likely to report maternal complications (adjusted odds ratio 0.7, 95% confidence interval 0.6–0.8) than primiparous women.
Table 3: Weighted proportion and multilevel logistics regression of maternal morbidity for rural and urban women in Indonesia during most recent pregnancy in maternal period 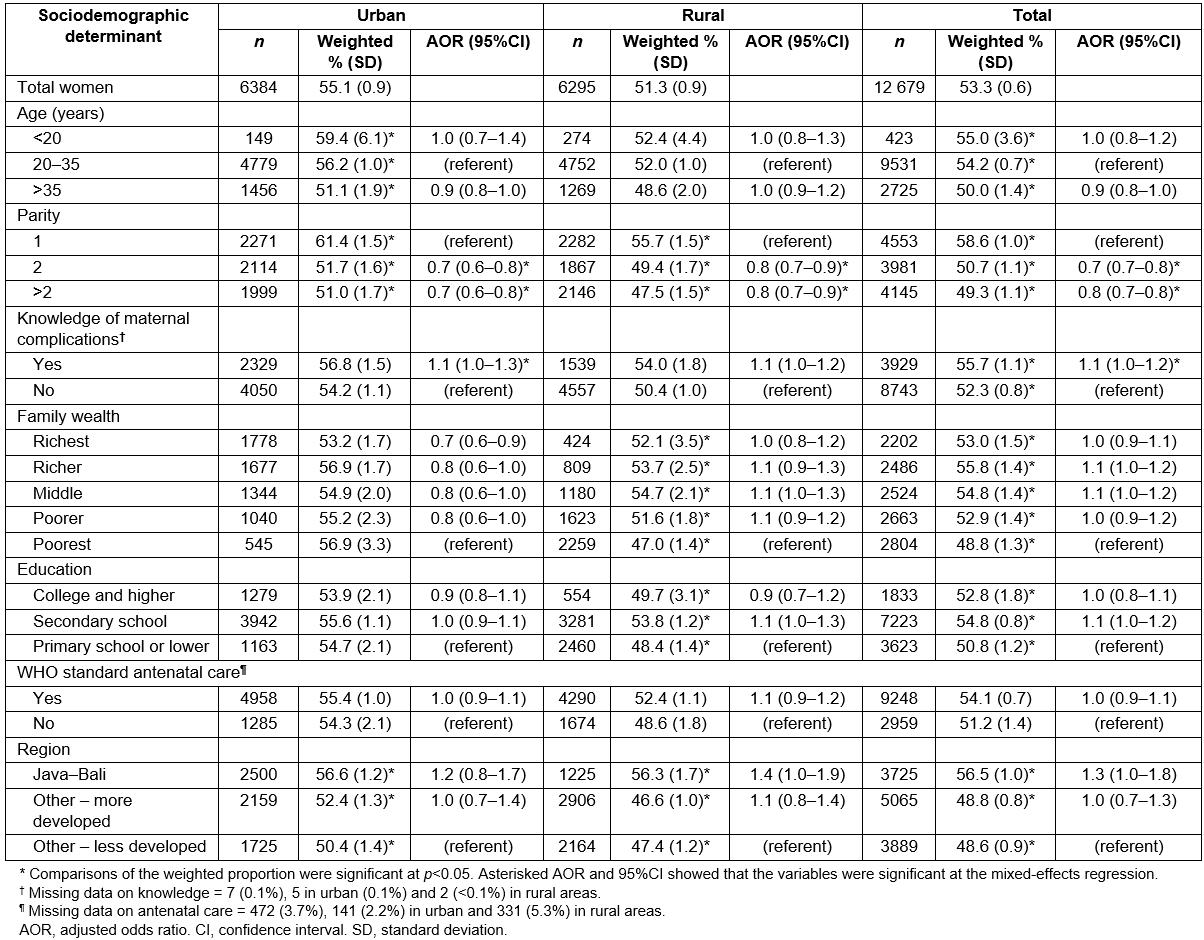
Discussion
Pattern of self-reported maternal morbidity types
This study showed differences in the proportion of maternal morbidities between rural and urban areas. Previous studies looking at different health outcomes also reported differences between rural and urban areas in Indonesia17,18 and other low–middle income countries19-22. All of these previous studies reported a preferable condition in urban areas compared to rural areas. In contrast, this study found that women in rural areas had a lower prevalence of pregnancy morbidity and/or labor morbidity than women in urban areas. However, these findings should be interpreted cautiously, particularly due to the self-report nature of this study.
There are several potential explanations for the findings. First is the higher maternal mortality in rural areas. In 2010, approximately 64% of maternal deaths in Indonesia happened in rural areas23. Second is under-reporting due to lower awareness of maternal complications, lower coverage of ANC and a higher proportion of socially disadvantaged women in rural areas. Previous research has noted the importance of ANC visits in improving knowledge and awareness of maternal morbidity24-26. Additionally, studies have reported that socially disadvantaged women (ie women of low education and economic status) have lower knowledge of maternal morbidity24-28. In this study, the proportion of women who knew about danger signs during pregnancy and had the recommended ANC was significantly lower in rural areas compared to urban areas. These factors might influence the self-reporting of maternal morbidity and the rural–urban disparities observed in this study.
The results also showed similarities between Indonesian rural and urban areas in the types of self-reported pregnancy morbidities. However, there were slight differences in labor complication types. The differences in patterns of maternal morbidities might require different intervention approaches. With the relatively low knowledge of danger signs during the maternal period, increasing awareness of maternal morbidity is critical to improve mothers’ health-seeking behaviors and birth preparedness28-30. In 2012, the IDHS reported that only 53.0% of women received information on danger signs during pregnancy during their ANC visits, with significant rural–urban differences. Approximately 57.1% of urban women received information on danger signs of pregnancy complications compared to only 48.7% of women in rural areas31. Therefore, integration of focused education on maternal morbidity in ANC is indispensable. The educational intervention to improve knowledge should emphasize the types of morbidities more prevalent in the respective areas. This step must be followed with healthcare readiness for emergency cases, focusing on the more prevalent morbidity cases in the area32.
The higher prevalence of self-reported infection and bleeding in rural areas highlights the importance of improving awareness of these morbidities. This study corroborates findings from a systematic analysis by WHO, which reported that, globally, more than 50% of maternal mortalities were attributed to bleeding, hypertension or sepsis. In addition, indirect causes (pre-existing conditions including HIV and other medical conditions) contribute to almost 25% of overall maternal deaths in the world33. In rural Tanzania, a hospital-based study found that the most prevalent severe maternal morbidities and mortality included obstructive labor hemorrhage, hypertensive disorders and abortion-related complications34. Although the Tanzanian study had a different source population from the present community-based study, the similarities in the most prevalent morbidity reported (ie bleeding/hemorrhage) signify the importance of focusing on bleeding prevention and treatment during the maternal period. Previous research in rural Malawi and Pakistan reported a higher prevalence of infection-related morbidity, with approximately one-third of women experiencing this morbidity during the maternal period35. The findings from the present study as well as evidence from previous research underline the need to improve the mothers’ and healthcare providers’ awareness of and readiness to infection and bleeding during the maternal period, specifically in rural areas of Indonesia.
In this study, the authors were unable to estimate the prevalence of hypertension in pregnancy due to data limitations. Although the IDHS reported whether women had blood pressure measurements during ANC visits, the actual values of blood pressure were not recorded. Hypertension and other symptoms were classified as ‘other’ pregnancy morbidities, and could not be further classified. Therefore, it will be important to further investigate hypertension in pregnancy as well as other pre-existing medical conditions that might influence pregnancy outcomes and cause maternal morbidity36. This step is especially important because this study found that ‘other’ pregnancy morbidities were the most prevalent morbidities, both in rural and urban areas. In addition, a previous study on maternal morbidity in Indonesia reported that hemorrhage and hypertensive disease were the most common diagnoses for maternal near miss (in which a woman survived life-threatening complications during the maternal period)37.
Sociodemographic pattern of self-reported maternal complications
This study showed that, in both rural and urban areas, a higher proportion of maternal morbidity was observed in primiparous women. Consistent with previous findings, this study found that nulliparity remains an important factor for self-reported maternal morbidity38-40. Previous studies also reported that younger age is a predictor of maternal morbidity40-42. In this study, significant differences by age were observed in urban areas, but not in rural areas. Younger urban women had a higher proportion of maternal morbidity. In this study, there was no increase in morbidity proportion in women who were older than 35, which was reported as a risk factor for morbidity38-40. Other risk factors for morbidity include prior history of complications39-41 and pre-existing medical conditions38,43, which could not be measured in this study. The findings suggest the importance of a high-risk approach for high-risk individuals: younger, primiparous women. The intervention should be conducted both in rural and urban areas, and include identification of high-risk mothers, screening and early management of complications.
Previous studies have reported that social disadvantage including poverty and low education can increase the risk for severe maternal morbidity44-47. Less contact with healthcare providers also increases the risk of these morbidities45-47. Although not significant, the authors found similar patterns in urban women, where women with social disadvantage reported a relatively higher proportion of morbidity. However, in rural areas, a higher proportion of self-reported morbidity was found in women with higher family wealth. This discrepancy might be due to the higher knowledge of maternal morbidities in more socially advantaged women. Women who are more aware of maternal morbidity are more likely to recognize the symptoms and report their experience. This was reflected in the higher proportion of morbidity among women who knew about danger signs in pregnancy, which was found in the present study. In previous studies, education and household assets were reported to increase knowledge of maternal morbidity28,48. Additionally, the information received during ANC can improve women’s knowledge and awareness26, and increase the reporting of maternal morbidity. The rural–urban differences in sociodemographic patterns of maternal complications might be confounded by the differences in socioeconomic background and knowledge of maternal morbidities between rural and urban women. Therefore, more attention on improving knowledge and awareness on maternal morbidity should be directed to rural women and women of low family wealth. Additionally, research with more valid measures for maternal complications (ie medical records or medical examination) is needed to corroborate the findings from this study.
Limitations and strengths
There are several limitations to this study. First, the authors were unable to report several major maternal morbidity types, including morbidities caused by pre-existing medical conditions. Second, the self-reported morbidity status was susceptible to information bias. This was particularly due to the knowledge of maternal morbidity, family wealth and level of education. Although self-reported morbidity has its limitations, a previous validation study showed that the specificity and sensitivity are quite good49.
Despite these limitations, this study makes significant contributions. First, this study presents the types of morbidity by rural/urban area, which can inform recommendations for intervention. Second, this study was able to identify vulnerable populations for maternal morbidity within rural and urban areas. These women can be the target of high-risk prevention strategies. Third, this study highlights the relatively high prevalence of maternal morbidities, which was amplified by the low knowledge of danger signs during the maternal period. These findings should further emphasize the importance of not only focusing maternal mortality but also addressing maternal morbidities in public health interventions.
Conclusions
The authors found similar patterns in pregnancy morbidity between rural and urban areas. Meanwhile, the patterns of labor morbidity were slightly different. These findings also suggest rural–urban disparities, specifically in knowledge and prevalence of maternal morbidity. Therefore, intervention to improve knowledge and awareness of maternal morbidity is needed. The educational intervention can be integrated in routine ANC, with more emphasis on the types of morbidity more prevalent in the respective areas. Further research to classify types of pregnancy morbidity, specifically complications related to chronic diseases, is needed.
This study observed differences in factors related to self-reported morbidity. Although nulliparity was the dominant risk factor for morbidity in rural and urban areas, there were differences by family wealth and education in rural areas, but not in urban areas. The higher proportion of self-reported morbidities in socially advantaged populations in rural areas, but not urban areas, might reflect differences in the knowledge and awareness of maternal morbidity between rural and urban women. Therefore, it is crucial to improve the knowledge and awareness of maternal complications, specifically for women of low family wealth living in rural areas.
Acknowledgements
The authors thank the Demographic and Health Survey Program for providing access to the data for this study. IDHS was a joint effort of the Statistics Indonesia, National Population and Family Planning Board – BKKBN/Indonesia, Ministry of Health Indonesia, and ICF International.


