Introduction
With a population density of 1.87 people per square kilometer in 2014, Mongolia is the world’s least densely populated country. The sparse distribution of the population impedes the delivery of social services, including health care, to rural and remote areas – especially to herders who lead nomadic lifestyles (Fig1)1. However, the proportion of the urban population (urbanization rate) is increasing in Mongolia; the capital, Ulaanbaatar, is home to about 45% of the country’s population (Fig2). Accordingly, the gap in medical resources has widened and the number of physicians per 1000 people in Ulaanbaatar is 1.5-fold that in rural areas2. One factor that is responsible for considerable health risks in Mongolia is the ‘creeping disaster’ of the dzud, which highlights disparities in medical care.
The dzud is a winter disaster that occurs in Mongolia; it is characterized by deep snow and severe cold, which lead to high livestock mortality, and threaten human livelihood. Livestock rearing constitutes one of the key industries in Mongolia, and the dzud affects many herders, who depend on their animals for food, income, and transportation. From 1999 to 2002, the health and food security of approximately 40% of the country’s population were threatened by the dzud, which killed 11.2 million livestock3,4. In the winter of 2009–10, Mongolia experienced the most severe dzud since the consecutive dzud winters of 1999–20025. Temperatures in January 2010 were more than 6°C colder than average (eg Ulaanbaatar, –21.8°C; Ulaangom (capital of Uvs Province), –32.3°C). There was a greater-than-average snowfall and more than 60% of the country remained blanketed in snow until the end of April 2010. From January to May 2010, over 7.8 million head of livestock had perished nationwide4. Infant and under-five mortality (often used as an indicator of the health level in a country or region) dramatically increased during the dzud of 2009–10. In contrast to the national average of 22.7 per 1000 live births for that year, the infant mortality rate in dzud-affected provinces in March 2010 was 32.3 per 1000 live births; under-five mortality was 39.7 per 1000 in dzud-affected provinces in March 2010, whereas the national average was 28.7 per 10004. The present authors have previously reported that the loss of livestock and shortage of dairy products at that time led to malnutrition in Mongolia, as evident in infant mortality6. However, few studies have fully investigated the health risks related to the dzud. There is thus a need to conduct a detailed assessment of this phenomenon to help reduce the risk incurred by future disasters and formulate longer term solutions. The present study aimed to elucidate the relationship between the lack of medical resources and public health vulnerability with respect to the dzud in Mongolia.
 Figure 1: Typical scene of Mongolian nomads in winter.
Figure 1: Typical scene of Mongolian nomads in winter.
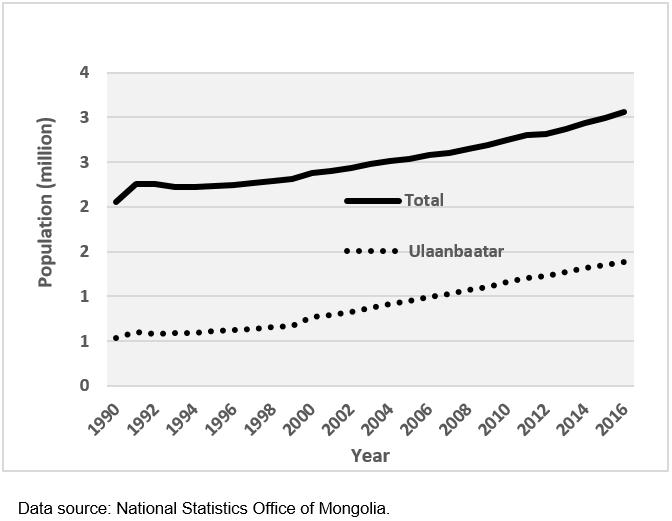 Figure 2: Population trends of Mongolia (total and for Ulaanbaatar population).
Figure 2: Population trends of Mongolia (total and for Ulaanbaatar population).
Methods
Public health markers
Mongolia has 21 provinces (aimag) in addition to Ulaanbaatar, and data from all those provinces and Ulaanbaatar were analyzed. The change in child mortality (CCM) was defined as the difference in the under-five mortality rate (number of deaths of children aged less than 5 years per 1000 live births) for 2009–10. In the present study, CCM was used as a health indicator for the effect of the dzud; however, in the authors’ previous study, the infant mortality rate was used6. The reason for choosing the CCM in the present study is that there is a potential nutritional problem in Mongolia. According to data from WHO, nutrition-related factors contribute to about 45% of deaths in children aged less than 5 years7. The following items were set as the other public health markers: change in mortality of respiratory disease (CMRD) and of cardiovascular disease (CMCD; number of deaths of people of all ages per 10 000 population). Those two disease types have been found to be related to the cold winters in Mongolia8,9. Those health markers were used based on data from the Mongolian government10.
Medical resources and urbanization
The number of physicians and nurses (per 1000 residents) in 2009 was used as an index for access to medical care. The urbanization rate (proportion of urban population; the population reside in Ulaanbaatar, provincial capitals, and towns) in 2009 was employed as an index for the infrastructural development in each province. The data for these parameters were obtained from the National Statistics Office of Mongolia11. The health markers were compared with those indexes to determine the correlations.
Environmental factors
The average temperature and total precipitation in each provincial capital from October 2009 to February 2010 were set as environmental factors related to health issues. Winter precipitation in Mongolia is mainly snow. Meteorological data were obtained from Mongolia’s Information and Research Institute of Meteorology, Hydrology and Environment, based on regular observations in each province. The health markers were compared with these environmental factors.
Declining rate in livestock numbers
Based on the findings of a previous study6, livestock loss was considered an important public health factor during the dzud. Livestock rearing is a good economic indicator in the country. The declining rate in livestock numbers from 2009 to 2010 (percentage livestock loss) was determined based on the decreasing year-on-year proportion of livestock (expressed as sheep units (relative to feeding requirements of one sheep for one year): horses × 7, cattle × 6, camels × 5, goats × 0.9). These parameters were based on data from the National Statistics Office of Mongolia11. The health markers were compared with percentage livestock loss.
Statistical analysis
The relationship between the health markers and the other factors (percentage livestock loss, average temperature and total precipitation, number of physicians and number of nurses, and urbanization rate) was assessed using Spearman’s rank correlation with a significance level of 5%. To extract the factors that affected the health markers by means of multivariable analysis, the dependent and independent variables were selected based on the results of Spearman’s rank correlation and considering multicollinearity. A linear regression analysis (variable reduction method) was conducted, and a 95% confidence interval of p<0.05 was considered significant. All data analyses were performed using SPSS v22.0 for Macintosh (IBM, http://www.spss.com).
Ethics approval
The Faculty of Medicine, Tottori University granted ethics approval for this study (17A021).
Results
Results of markers and factors
The national average of under-five mortality rates in 2009 and 2010 were 23.5 and 25.6 per 1000 live births, respectively. The national average mortalities for respiratory and cardiovascular diseases were 2.8 and 21.7 per 10 000 populations in 2009, and 5.3 and 25.6 in 2010, respectively. The greatest number of physicians in 2009 was 3.69 per 1000 residents, in Ulaanbaatar. By contrast, the number of physicians in Bayankhongor, Khovsgol, Arkhangai and Bayan-Olgii was less than 1.50: 1.34, 1.39, 1.45 and 1.47, respectively (Fig3). The greatest number of nurses per 1000 in 2009 was 3.69 in Govisumber; the smallest was 2.31 in Ovorkhangai. The highest urbanization rate in 2009 was 100%, in Ulaanbaatar; the lowest was 19.9%, in Arkhangai. The lowest average temperature from October 2009 to February 2010 was –21.4°C, in Uvs; the highest was –7.7°C, in Omnogovi. The highest total precipitation from October 2009 to February 2010 was 40.3 mm, in Uvs; the lowest was 6.7 mm, in Dornogovi. The total numbers of heads of livestock in Mongolia in 2009 and 2010 were 44.0 million and 32.7 million, respectively. The numbers of livestock calculated in sheep units were 69.5 million and 54.8 million, respectively. The highest percentage livestock loss was 42.9%, in Ovorkhangai; the lowest was –12.2%, in Sukhbaatar.
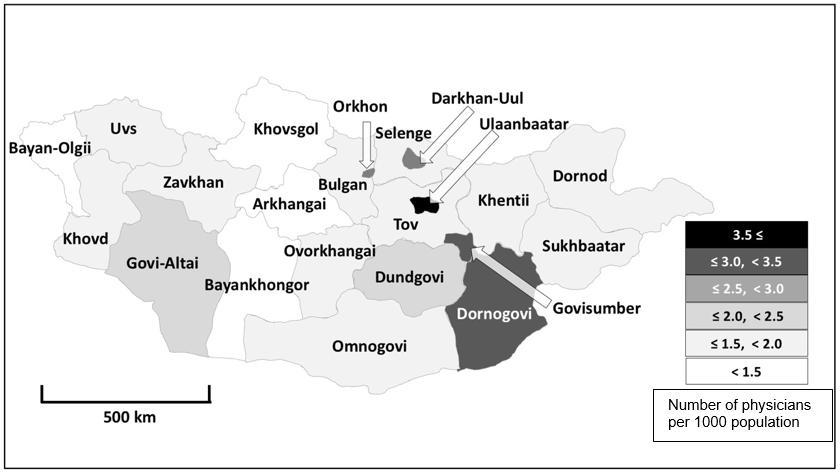 Figure 3: Number of physicians per 1000 population in Mongolia’s provinces in 2009.
Figure 3: Number of physicians per 1000 population in Mongolia’s provinces in 2009.
Association between health markers and various social and environmental measures
The correlation coefficient (ρ) between CCM and each measure are shown in Table 1. The CCM was negatively correlated with the number of physicians (Fig4) and urbanization rate; it was positively correlated with percentage livestock loss (Fig5).
The correlation coefficient between CMRD and each measure, and between CMCD and each measure, is also shown in Table 1. CMRD and CMCD were not significantly correlated to these measures.
Table 1: Correlation coefficients (ρ) between health markers and various social and environmental measures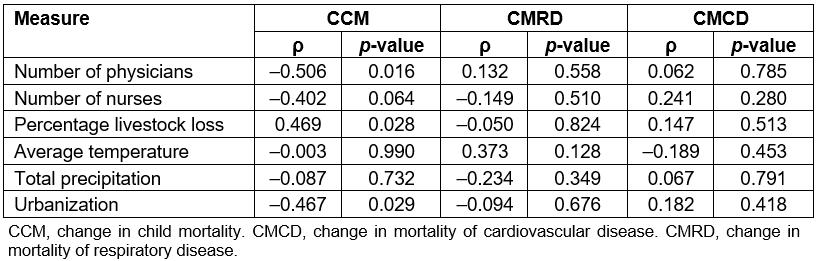
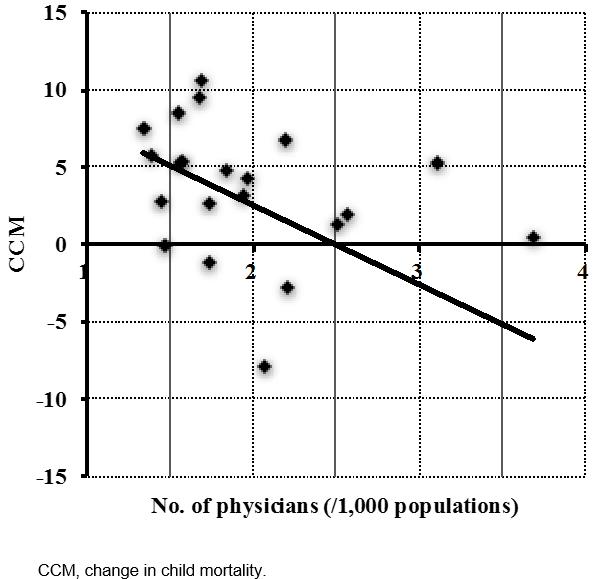 Figure 4: Correlation between the difference in the under-five mortality rate from 2009 to 2010 (CCM) and the number of physicians per 1000 population.
Figure 4: Correlation between the difference in the under-five mortality rate from 2009 to 2010 (CCM) and the number of physicians per 1000 population.
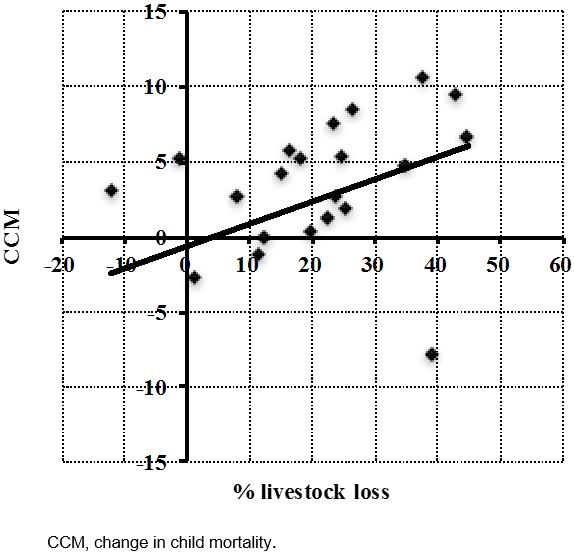 Figure 5: Correlation between difference in under-five mortality rate 2009–2010 (CCM) and the declining rate in livestock numbers in 2010 (percentage livestock loss).
Figure 5: Correlation between difference in under-five mortality rate 2009–2010 (CCM) and the declining rate in livestock numbers in 2010 (percentage livestock loss).
Results of multiple regression analysis
To examine the factors that influenced the health markers during the dzud, CCM was selected as the dependent variable and number of physicians and percentage livestock loss as the independent variables; this was done based on the results of the correlation coefficients and considering multicollinearity. The number of physicians was significantly negatively related to CCM (standardizing coefficient −0.492, p=0.020); however, there was no significant relationship between percentage livestock loss and CCM (standardizing coefficient 0.258, p=0.258). R2 value was 0.293 and adjusted R2 value was 0.219.
Discussion
These results suggest that a shortage of medical resources has a negative effect on children’s health in Mongolia’s severe winter dzud. Many countries face the need to address medical resource shortages in rural areas. In many countries, there is also a huge discrepancy between urban and rural areas in terms of physician supply, and that is certainly true in Mongolia. According to WHO, the number of physicians per 1000 population in Mongolia in 2010 was 2.73; that year, it was 41st highest in the world and higher than the global average of 1.8012. However, there is a significant difference between rural and urban areas in Mongolia regarding the number of physicians providing secondary care. General hospitals in rural regions are short of certain specialists, including pediatricians13. Moreover, the lack of infrastructure in Mongolia, especially in rural areas in winter, dramatically hampers access to medical care institutions.
According to a report by the United Nations, the main causes of child mortality in Mongolia in 2010 were complications of acute respiratory diseases due to inaccessibility to essential medicines and emergency or intensive care4. There are few intensive care units (ICUs) in Mongolia; even in Mongolia’s largest cities, ICUs are an under-resourced and underdeveloped medical specialty. The main problems encountered are insufficient staff training and lack of medical equipment, disposables and drugs14. Moreover, the density of pediatricians has been reported as inversely associated with under-five mortality15. Another study in Mongolia found that the number of physicians was protective against amenable mortality: death could have been prevented if effective health care had been provided in a timely manner1. Increasing the number of medical specialists will have a positive effect on child health in Mongolia.
A shortage of medical staff, including nurses, midwives and pharmacists, is, however, still a major problem in Mongolia. The number of nurses per 1000 population in Mongolia has been 3.0–3.3 since the 1990s; this is very low compared with OECD countries (eg Switzerland (16.6), Norway (16.4) and Japan (11.5)) in 201116. The nurse-to-physician ratio was 1.32 in Mongolia in 2011; this is also very low by international standards (eg Philippines (5.2), Thailand (5.11) and Japan (2.01)), and it points to an overdependence on doctors in Mongolia’s health sector13. The present study found that the number of nurses was negatively correlated with CCM, although the difference was not significant. Thus, the shortage of nurses would appear to have an effect on child mortality in Mongolia. To improve child health, it is necessary to supply other medical staff, including nurses, in addition to doctors.
Among the limitations of the present study is that authors were unable to evaluate the impact of the dzud on elderly adults. Cardiovascular and respiratory diseases are generally exacerbated, even among adults, in Mongolia’s harsh winter. However, Mongolia has a low proportion of elderly people at high health risk: in 2010, life expectancy at birth was 68.05 years10,11. Health effects of the dzud in elderly Mongolian adults cannot be studied due to their low life expectancy.
Another limitation of this study is that infrastructure development could not be assessed in detail. The level of medical practice in Mongolia is still very low. Based on the country’s well-established health system, each municipality (soum) has a health center for primary care, and each province (aimag) has a general hospital13. However, Mongolia’s transport infrastructure is poorly developed: road conditions in rural areas are unsatisfactory, and those conditions worsen in winter. It is difficult to evaluate those parameters comprehensively; thus, the urbanization rate was used as a rough index of infrastructure development.
The Mongolian government, UNICEF and other non-governmental organizations provided emergency assistance (including management of severe acute malnutrition and other emergency health services) for dzud-affected provinces. This study did not consider such interventions owing to the lack of data about these supportive actions. Notwithstanding such actions, under-five mortality in dzud-affected provinces was still high4.
A previous study reported that the loss of livestock in the dzud was associated with infant mortality6. Nutritional disorders because of a shortage of dairy products were suggested as a possible reason for that finding. In the present study, it was likewise found in univariate analysis that under-five mortality was related to livestock loss. However, with multivariate analysis, the relationship between child mortality and livestock was unclear. There is of course no question about the necessity to undertake appropriate measures to mitigate livestock damage during the dzud. However, the results of the present study indicate that increased medical resources in affected areas – particularly rural areas lacking easy access to medical institutions – would help improve child health during those severe winters.
Conclusion
Lack of medical resources and infrastructure, and loss of livestock, have negative effects on child health in the dzud, a severe winter disaster in Mongolia. A system that achieves optimal medical treatment by effectively using limited resources is required.
Acknowledgements
This work was supported by a Grant-in-Aid for Scientific Research (Kakenhi) from the Japan Society for the Promotion of Science (grant number 25220201). We thank the Edanz Group for editing a draft of this manuscript.
