Introduction
It is estimated that one in five Australians live with persistent pain1, and that the prevalence of chronic pain may be higher in rural and remote Australia than it is in the cities2. It is also recognised that people living in regional, rural and remote areas have less access to evidence-based pain services and community support3. Rural patients needing chronic pain management experience well-known patterns of rural and remote health disadvantage, including lack of access to appropriate information and limited access to local specialist care2. Studies of patients with chronic lower back pain have shown that rural consumers experience difficulties in knowing where to access relevant information and express frustration with the lack of service delivery options to access interdisciplinary and specialist services4. It is also recognised that a consequence of poor geographical access to pain services is a reluctance of general practitioners to refer patients for such specialist services5. Lack of timely access to specialist pain services is recognised as a major contributor to suffering, increased healthcare utilisation and further chronic pain development6. Hence new clinical service models to enhance access to specialist pain management services for all patients, but in particular those from rural/remote communities who face particular challenges accessing multidisciplinary specialist care, are needed.
The National Pain Strategy states that best practice pain management requires coordinated interdisciplinary assessment and management of physical, psychological and environmental risk factors of each participant3. The use of multidisciplinary biopsychosocial rehabilitation interventions have been proven to be more effective than usual care and physical treatments in decreasing pain and disability in people with chronic low back pain7. In a recent systematic review, multidisciplinary rehabilitation for chronic lower back pain has been shown to have a moderate effect on pain and a small effect on function at a moderate standard of evidence when compared with usual care8. These interventions are able to be provided by a range of allied health clinicians within an interdisciplinary team. Interdisciplinary approaches to the management of persistent pain are well documented as being successful9.
Education and development of active self-management strategies are key components of interdisciplinary pain management, with several trials demonstrating significant changes in pain beliefs and attitudes, pain cognition and physical performance following pain neurophysiology education10,11. The evidence for self-management programs for chronic pain conditions is conflicting. A recent Cochrane review suggests that self-management education programs result in no or only small benefits in people with osteoarthritis, with these benefits of unlikely clinical importance12. In contrast, other studies of self-management programs for chronic musculoskeletal pain conditions have shown such programs can be an effective way for participants to manage pain and disability13. For patients with chronic lower back pain, there is evidence that self-management programs have a moderate effect on pain intensity, and a small-to-moderate effect on disability14.
Whilst pain management programs can be delivered directly to individuals, there is also evidence to support the efficacy of group therapy models15-17. Elements of group treatment, such as universality, group cohesiveness and interpersonal learning, all work to promote positive outcomes18. Group pain management programs delivered as a package, compared with either no treatment or treatment as usual, have been shown to improve pain experience, mood, coping, negative outlook on pain, and activity levels19,20. From a service model perspective, delivering pain management programs in a group setting has also been shown to be a cost-efficient way to improve outcomes for individuals with persistent pain21. However, despite the recognised benefits of delivering pain management programs to groups of individuals, this model poses a further unique set of challenges for rural and remote patients, where distance and small population numbers can make it difficult to connect with other individuals to come together as a group.
The use of innovative technology such as telehealth has been highlighted as a key strategy to improve access and to promote and enable pain self-management22. In addition to early feasibility studies that confirmed the potential for using telehealth for pain consultations23,24, a number of recent studies have shown positive outcomes for pain therapy programs delivered directly to individuals using telehealth. In 2002, Appel et al demonstrated that using telehealth to deliver behavioural interventions with individual participants could be feasible, with significant improvements observed in participants’ ability to self-manage pain25. Similarly, Herbert et al in 2017 reported comparable reductions in pain interference when comparing telehealth and in-person therapy for individuals with persistent pain26. In 2009, Pronovost et al explored both costs and consumer perceptions in a randomised, two-period, crossover trial with 26 participants comparing in-person and telehealth delivery of individual consultations for chronic pain management27. Results showed high levels of patient satisfaction with the telehealth consultations, and direct costs of the telemedicine group were significantly lower than the in-person group27.
Although such data provide some supporting evidence for the use of telehealth to help manage patients with persistent pain, there has been no systematic study of pain management programs that use a group model, delivered using telehealth. There is, however, literature from other clinical populations that suggest it should be feasible. A group-based stress management program using tablet videoconferencing has been piloted for 14 cancer survivors28. The authors described the program as being feasible, with participants finding the program helpful overall, although only modest improvements in perceived stress were found and the participants noted challenges in the delivery of the program28. Group treatment to improve emotional regulation in individuals with traumatic brain injury delivered using videoconferencing has also been investigated29. Although also only a pilot study (n=7), the study found high self-reported satisfaction with the treatment29. Although the evidence is only preliminary, studies such as these suggest a group telehealth service model could be viable for pain management.
Improvements in technology that enable live videoconferencing across multiple sites have the potential to enable access to specialist services as well as connection to other individuals with persistent pain living in rural/remote areas. The Manage Your Pain program reported here in this project was designed as a multisite pain management group to be delivered using telehealth. It was established to meet the needs of people with persistent pain living in rural and remote towns in south-western Queensland for whom access to specialist services, and other people with persistent pain, is limited by geographical distance. The aims of this research were to perform a formative evaluation of a persistent pain management program implemented using a multisite telehealth group model, and examine consumer perceptions.
Methods
Study design
This study involved a formative evaluation using a mixed-methods analysis to examine the clinical feasibility of delivering the program using telepractice. Strengthening the Reporting of Observational Studies in Epidemiology (STROBE) recommendations30 and the Consolidated Criteria for Reporting Qualitative Research (COREQ-32) were used as reporting guidelines for the quantitative and qualitative methods respectively31.
Participants
Participants were recruited from outpatient referrals for management of persistent pain received within the South West Hospital and Health Service in Queensland, Australia. There were no financial incentives to participate in this study and ability to attend the pain program was not dependent on participating in the research. For inclusion in the research study, participants needed to be living in rural/remote south-western Queensland, have had persistent pain for 6 months or more as determined by a medical professional, have either a disability or psychosocial issues related to persistent pain, be able to access a facility in their local district that had the necessary telehealth equipment and staffing support, and attend all four sessions of the pain management program. Participants who were engaged in another pain management program, were under 18 years of age, highly dependent on medical care, diagnosed with cognitive impairment, had known illicit drug use without appropriate specialised treatment or had an active, untreated mental health condition were excluded. Participants whose primary language was other than English were also excluded due to the program being an education-based learning program that required use of a participant manual between sessions.
During the course of the study period (September 2016 to June 2017) 75 outpatients were referred to the pain management program. Of these, 37 declined participation in the service. Anecdotal reasons for patients’ decline included scepticism regarding the program’s aim to improve pain management, illness, commitment to caring for children or family, or work excluding ability to attend. Of the 38 participants who commenced the program, 28 met eligibility criteria and provided written consent to participate. The other 10 did not participate in the research but still continued to engage in the program. Of the 28 consenting participants, seven failed to complete the program and/or pre-/post-program questionnaires, resulting in a final cohort for analysis of 21 eligible participants (Table 1). Of these, one patient had missing data for CPAQ and their results for this outcome measure only were not analysed. These 21 participants had a mean age of 58 years and most experienced persistent pain in several body locations. On commencement of the program, average pain level in the group was self-rated by participants as an average of 5 on a 10-level pain scale (0=‘no pain’, 10=‘pain as bad as you can imagine’).
Table 1: Participant demographics (n=21) 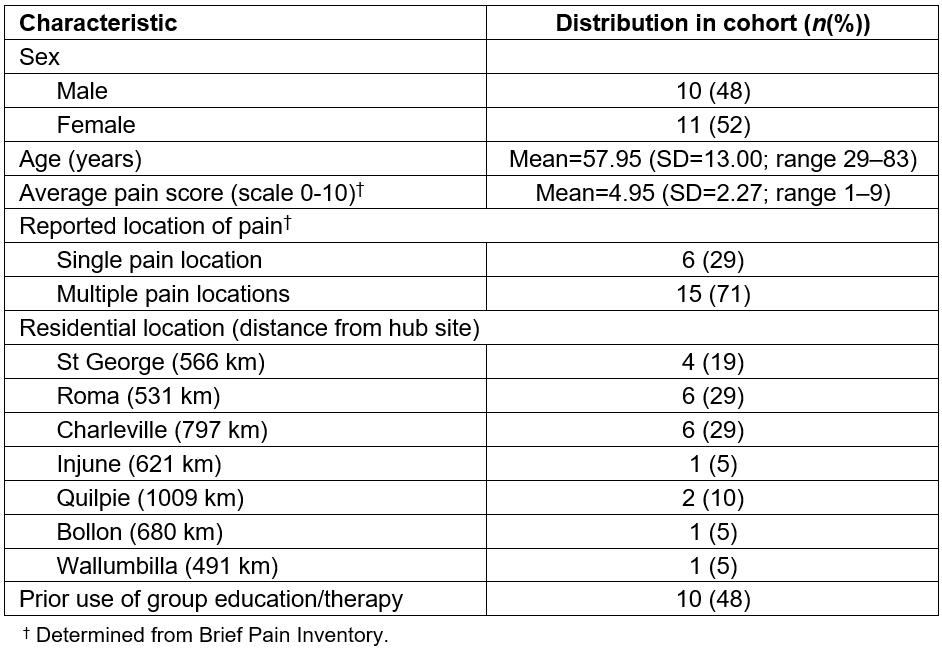
The Manage Your Pain – South West program
The Manage Your Pain – South West (MYP-SW) program was developed as a low-intensity interactive, interdisciplinary, educative pain management program. It is presented by allied health professionals from the metropolitan specialist pain management service and facilitated by local rural allied health professionals. The program uses an educational and Acceptance and Commitment Therapy (ACT) based approach, values focused, emphasising psychological flexibility32. The key components of the program are education in the neurophysiology of persistent pain and the development of active self-management strategies. The purpose of the program is to empower the participants by supporting their engagement in these strategies. This enables them to re-engage in meaningful activities that will help to improve their overall quality of life. An outline of the content of the program is provided in Table 2.
The pain management program is delivered in one 2-hour session per week, for 4 weeks (8 hours of intervention) (Table 2). All participants receive a manual that includes all the information presented in the sessions, committed action tasks, homework activities and links to further published and internet information regarding managing persistent pain. Each session is presented by the specialist allied health professional in their specific discipline (physiotherapy, psychology, occupational therapy and pharmacy). Participants are encouraged to explore the committed action tasks between the weekly sessions and provide feedback to the group each week.
Table 2: Manage Your Pain – South West telehealth program timetable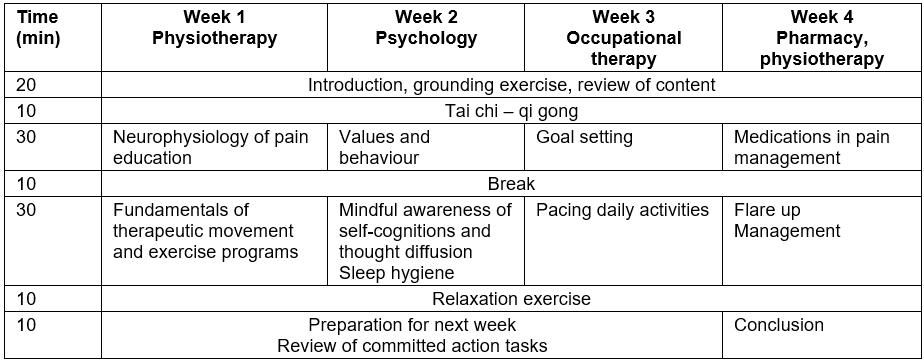
The telehealth multisite group model
The multisite telehealth group model was designed as a hub-and-spoke model that allowed the spokes sites to simultaneously connect/interact to each other and the hub site, as shown in Figure 1. The metropolitan specialist pain management service served as the hub, and specialist allied health professionals at the hub site delivered the program to participants at multiple rural/remote spoke sites simultaneously. Regional/rural participants attended sessions at the nearest health facility (spoke site) to their homes. Potential spoke sites were identified as sites that had both the necessary telehealth equipment and a local health professional (rural allied health or nursing staff member) available to support participants to actively engage in the program and with the hub-and-spoke sites. A total of 15 rural/remote health sites across the health district were identified as potential spoke sites. Of these, only seven sites were used during the study period, with a range of 491–1009 kilometres from the metropolitan specialist pain service hub (Table 1). Five programs were delivered during the length of the study, in which five to eight sites participated at any one time.
The four program sessions were conducted live using videoconferencing. Sites used dedicated videoconferencing units (Cisco C20/SX20) to connect to the hub-and-spoke sites using the secure telehealth network of the public health service. Within each session the videoconference link was established by the allied health professional at the local sites. Using a multipoint videoconference connection, creating a virtual meeting room, participants were able to view and hear each other and the hub site simultaneously in real time. Each user’s screen displayed the main screen as well as the series of smaller insert screens, which displayed all participants from the hub-and-spoke sites at all times during the videoconference, with the active speaker becoming the dominant display on the screen.
Simulating a face-to-face group model, both structured tasks and spontaneous discussion were encouraged to explore the information between the presenters, facilitators and participants. The videoconferencing link was also used to present content, share media presentations (PowerPoint presentations, videos) and to demonstrate physical components of the program (eg tai chi movements) and monitor participants’ ability to do these. During sessions, participants’ level of engagement and understanding was monitored by the hub site presenter using visual cues (body language), and verbal cues and interactions. Standard videoconferencing and group expectations were discussed with all participants at commencement of the program. Sites were advised to remain on mute when not engaging in conversation; to respect individuals’ privacy and shared experiences, and individuals were actively encouraged to interact with the hub-and-spoke sites.
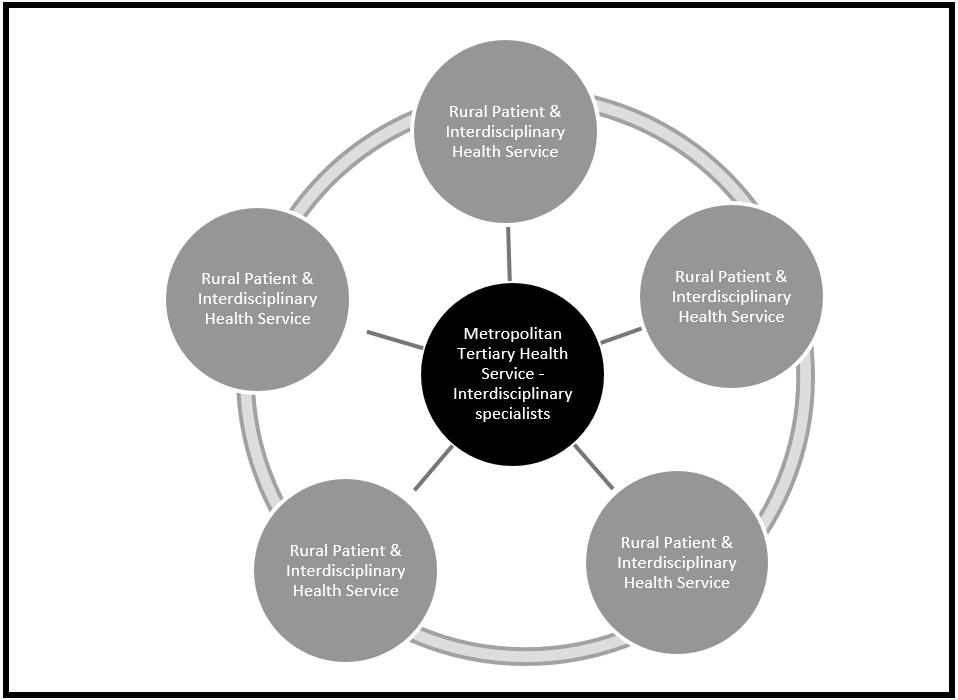 Figure 1: Manage Your Pain – South West telehealth multisite group model.
Figure 1: Manage Your Pain – South West telehealth multisite group model.
Outcome measures
To evaluate whether any improvements in outcomes were observed, participants completed a battery of pre- and post-intervention measures relating to their pain and its impacts. These were selected based on the Initiative on Methods, Measurement and Pain Assessment in Clinical Trials (IMMPACT) recommendations33, which outline the core outcome domains that should be performed in clinical trials of the efficacy and effectiveness of treatments for persistent pain. The following assessments were included.
Chronic Pain Acceptance Questionnaire 20 (CPAQ 20): This is a validated tool constructed as part of the development of an acceptance oriented treatment approach for persistent pain participants34. It contains two subscales (pain willingness and activity engagement), which are totalled separately and combined for an overall score. Items in the scale are rated on seven-point scales (0=‘never’, 6=‘always’), with a higher result indicating a higher level of pain acceptance.
Brief Pain Inventory (BPI): This validated tool measures both the intensity of pain (sensory dimension) and interference of pain in a participant’s life (reactive dimension)35. The BPI is scored on an 11-point (0–10) scale where higher scores indicate higher levels of intensity or interference.
Depression Anxiety Stress Scale 21 (DASS 21): This tool measures along the axis of depression, anxiety and stress (degree of severity of symptoms) as compared to the normal rates of the population36. It is not a diagnostic tool, but rather an indicator that the participant is exhibiting symptoms.
Patient Impression of Change Scale (PICS): This tool quantifies a participant’s improvement or deterioration over time to determine the effect of an intervention37. It measures current health status, compared to a previous time point, using a seven-point scale (1=‘very much improved’, 7=‘very much worse’). Scott and McCracken have reported on the validity and predictors of PICS ratings following interdisciplinary, psychologically based treatment for chronic pain37.
Pain Self Efficacy Questionnaire (PSEQ): This 10-item inventory tool targets a participant’s beliefs about their ability to accomplish a range of activities despite their pain38. The scale uses a range from 0 to 60, with higher scores indicating stronger self-efficacy beliefs.
Patient Reported Outcomes Measurement Information System (PROMIS): This is a system of highly reliable, precise measures of patient-reported health status for physical, mental and social wellbeing39. A short form involving 10 self-report global health items from PROMIS was used in this study. Hayes et al showed support for the construct validity for the use of 10 global health items to investigate two subscales: physical and mental health40. From the PROMIS, EuroQol (EQ-5D) scores can be accurately predicted as a measure of quality of life and for use in economic evaluations41. Preference-based health index scores, like the EQ-5D, provide a single summary score assessing overall health-related quality of life and are useful as an outcome measure in clinical studies, for estimating quality-adjusted life years for economic evaluations, and for monitoring the health of populations41. Scores range from −0.10 to 1.0, with greater scores indicating better overall health. The paper-based questionnaires were completed before and after completion of the program except for the PICS, which was completed before the program only.
Participants also provided feedback on their perceptions of the multisite telehealth group and the program through a 10-question post-telehealth participant satisfaction survey (using a five-point scale from 1=‘strongly disagree’ to 5=‘strongly agree’) that was designed by the authors and based on prior published surveys42,43. A week after completion of the program, participants took part in individual telephone interviews, where they were asked to respond to/discuss six questions (Table 3) related to their experiences of being a part of the multisite telehealth group. Prompt questions were used within each question to encourage participants to fully discuss their perceptions/feeling/issues raised in each question. All interviews were recorded and later transcribed verbatim.
Table 3: Semi-structured individual participant telephone interview questions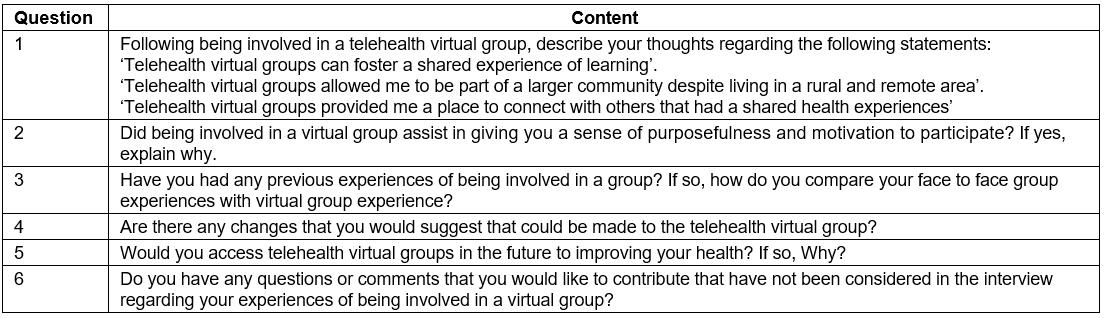
Analysis
Data from all outcome measures collected before and after group participation were compared using matched pairs t-tests using the Statistical Package for the Social Sciences v24 (IBM; https://www.ibm.com/products/spss-statistics). Significance was set at p<0.05. Effect size (Cohen’s d) was calculated where >0.2 is a small effect, >0.5 a medium effect and >0.8 is a large effect44. Two of the core outcomes (CPAQ and BPI) were selected and further analysed using reliable change analyses. In accordance with the approach of Jacobson and Truax45 the percentages of participants who demonstrated reliable improvement, no change and reliable deterioration were calculated at 95% (a=0.05) confidence interval. Descriptive statistics were used to report outcomes from the PICS, the telehealth group satisfaction survey and the questions pertaining to perceptions of the telehealth group, which were all completed after the program only.
Transcripts from the qualitative interviews were analysed using a generic qualitative approach46.The generic qualitative approach is not restricted to any set philosophic assumptions, or intent to develop theory; rather, in this study it was used to provide a simple framework to analyse the major themes and messages to come from the experiences of the participants47. For analysis, transcripts were first coded and then two of the study authors examined the transcripts and discussed content similarities and differences and common emerging sentiment. This led to development of subthemes, which were ultimately grouped into themes. The set of transcripts was then re-examined by both study investigators to ensure all core content was captured within the final set of themes and subthemes.
Ethics approval
The project was conducted with full multisite ethics and governance by Gold Coast Hospital and Health Service Human Research Ethics Committee (EC00160) under the registration number HREC/16/QGC/110.
Results
Results of the statistical comparisons between the pre- and post-performances on the standardised tests are outlined in Table 4. Post-program results showed a significant (p<0.05) improvement, although small effect size, in both the activity subscale score and the total score of the CPAQ. Individual analysis of these parameters revealed 12 (60%) participants showed some improvement in on the CPAQ activity subscale and total score. Reliable improvement was observed in 6 (30%) participants on the activity subscale, but only 1 (5%) on the total score. No participants were found to have reliable deterioration on these parameters. There was no significant change in PSE, PROMIS, EQ-5D or DASS scores, with stress levels remaining mild pre- and post-program and anxiety and depression both remaining moderate.
Although there was no significant change in BPI inference scores at the group level, 3 (14.3%) participants were found to have made a reliable improvement (95% confidence interval). Similarly, results of the post-treatment PICS indicated that 50% of participants reported improved pain (29% no change), 57% improved physical activities (43% no change), 61% had improved mood (23% no change) and 65% indicated improvements in overall function (36% no change) (Table 5). A decline in mood and pain was reported by 16% and 21% of participants, with no change reported across the four variables by 23–43% of participants.
The majority (95%) of participants were positive about using telehealth in the future and two-thirds preferred telehealth as an alternative to travelling to the tertiary specialist centre (Table 6). Most (83%) felt connected to the other telehealth group members. Despite these positive responses, 18% indicated they would prefer to attend specialist metropolitan services face to face (Table 6). There were minimal technical issues noted during the sessions and all sessions were delivered successfully. Over 90% of participants indicated that technical difficulties did not interfere with their experience as a group or their engagement in the telehealth program. A few individuals with existing vision and hearing issues reported it was harder to view people at the sites due to the small size of the multisite split screen display. Having an existing hearing impairment impacted interactions for one individual. Other participants discussed the importance of all sites using the mute function to reduce issues of extraneous conversations impacting the sessions.
Table 4: Results of primary and secondary outcome measures pre- and post-program 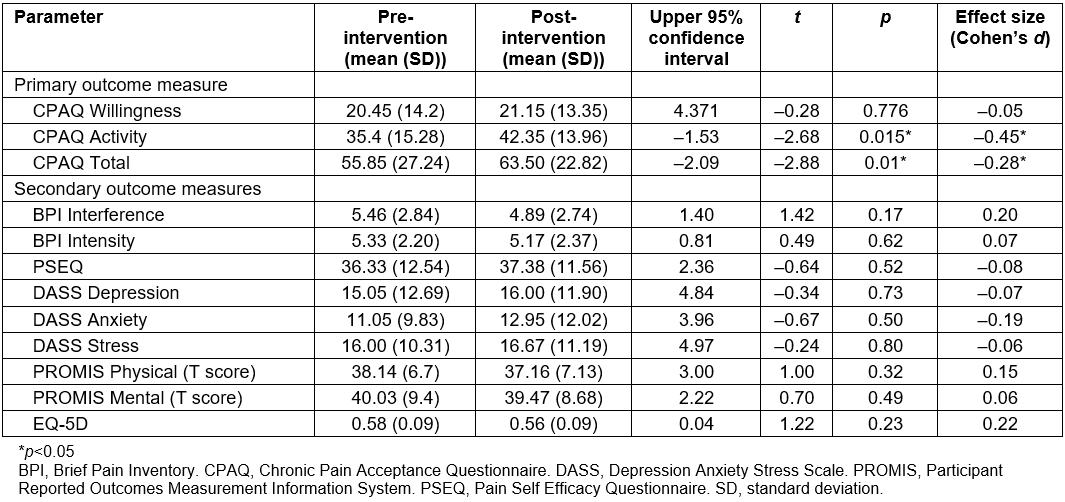
Table 5: Scores on the Patient Impression of Change Scale (n=21) 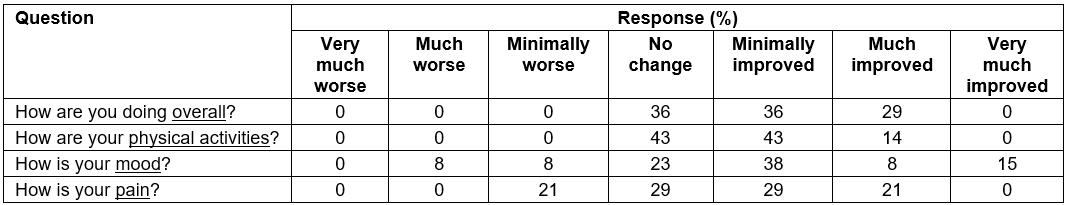
Table 6: Percentage of participant agreement (n=21) on the post-telehealth survey 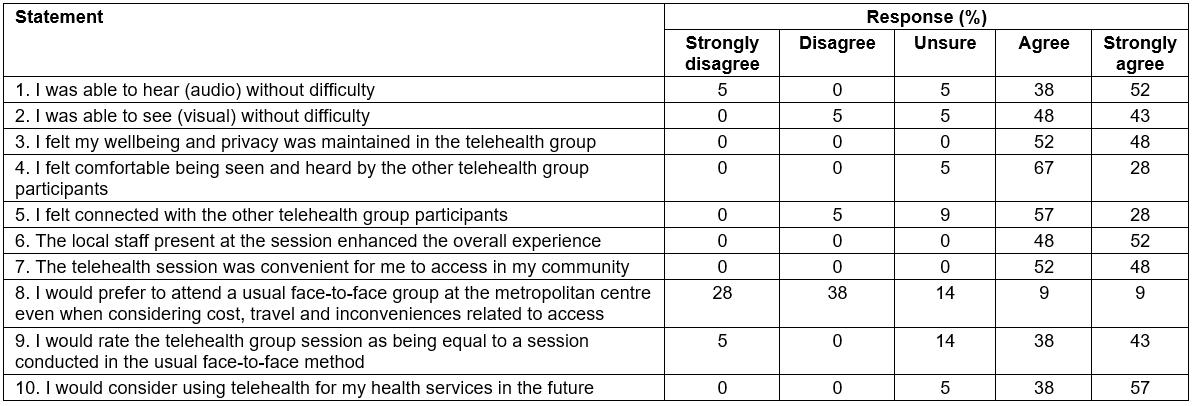
Information obtained from the interviews revealed the majority agreed with statements related to the multisite telehealth group being a place of connectivity and shared learning experience despite living in a rural remote area (Table 7). Three-quarters (76%) felt the group model gave them a sense of purpose and motivation. Most (90%) indicated they would use a multisite telehealth group in the future in their health care (Table 7).
The interviews revealed three major themes: ‘group experiences’, ‘telehealth accessibility’ and ‘limits and concerns’. Each had a number of subthemes, and these and example quotes for each are outlined in Table 8. The dominant of these themes was ‘group experience’. This theme included a number of subthemes including using the group to help validate individuals’ experiences of pain, discussion of group dynamics, and the support/relationships that developed within the multisite telehealth group (Table 8). For example, interviewee 18 stated:
… hearing different stories … helped me to be able to adapt different things in my life …
The second main theme was about issues raised regarding accessibility issues. Over two-thirds commented on the benefits of the geographical bridge that telehealth created between services, the ease of accessing specialists and the model that enabled people to connect between towns, for example:
We don’t have to get in the car and travel to … or anywhere … it’s at our doorstep (interviewee 12)
The third and much smaller theme related to issues raised by the interviewees about the model itself. In this group of comments, issues were raised regarding some suggested technical improvements and personal views on how to improve the program, for example:
… I’m so deaf … talking in the background [systems not on mute] … it was making it difficult for me to hear (interviewee 1)
Table 7: Participant agreement with interview statements (n=21)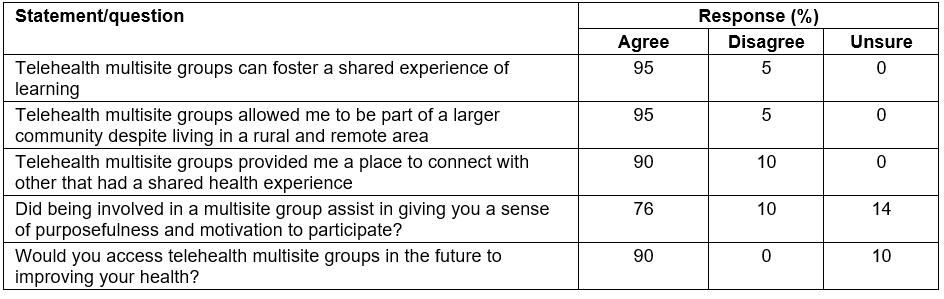
Table 8: Thematic analysis 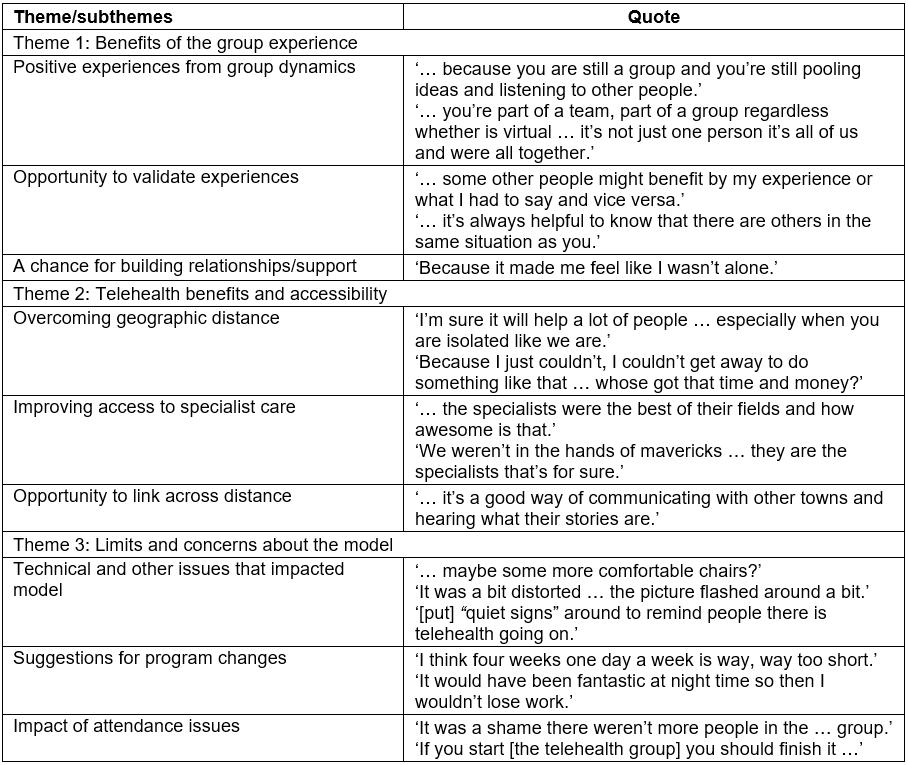
Discussion
The present research examined the implementation of a multisite telehealth group model for persistent pain management for rural/remote participants. Performance across a range of measures indicated some positive change in patient adjustment and function after the intervention. Surveys and qualitative interviews results also showed positive perceptions regarding both engaging in a group experience and receiving health care using telehealth. Overall the results support the use of a group pain model delivered using telehealth to help facilitate access to specialist pain services.
The battery of measures completed before and after the program revealed a number of positive improvements. On both the activity subscale and total score of the CPAQ, significant improvements were noted, indicating less restriction of activity engagement because of pain and overall improvement in pain acceptance after the program. Previous research has suggested that acceptance may be a key process involved in behaviour change in individuals with chronic pain48. The observed improvement in activity engagement subscale and overall pain acceptance were most likely influenced by the nature of the pain program itself. The program utilises the essence of an ACT-based approach to promote acceptance of negative experiences such as negative thoughts, emotional distress and physical discomfort to increase activity in support of value-consistent goals26,49. The present finding suggests that even the relatively brief intervention period of 8 hours was able to achieve statistically and clinically significant changes in pain acceptance, similar to studies that were more intensive but rated as low intensity (<20 hours), face-to-face ACT-based programs50-52. The positive change in activity subscale, shown by the reliable improvement calculations, reflects the program’s focus on supporting meaningful activity engagement through supervised practice in-session and committed actions tasks between sessions. The outcomes of this study did not mirror past research that showed larger improvements in reliable change in pain acceptance concurrently with the other psychometric measures analysed53-56. Although rated as low intensity, past studies had a longer treatment duration, which may be required for improvements to be seen in the outcome variables. Past studies have also found improvements in pain acceptance and an increase in physical performance after an ACT intervention57.
Overall the MYP-SW program endeavoured to empower participants by presenting and supporting their engagement in active self-management strategies for persistent pain with the aim of improving overall quality of life. The program’s focus was not to reduce pain intensity so it was not predicted that there would be a significant change in pain severity ratings on scales such as the BPI, but perhaps changes in the BPI pain interference measure could be anticipated. Although results revealed no group-level change in BPI scores, some individuals demonstrated positive changes on the interference scale, with almost one-fifth of the group reporting individual-level changes consistent with a clinically meaningful reliable change. The trend for improvement in BPI interference scores demonstrates that the program was able to benefit participants by improving their ability to function and engage in life despite their persistent pain.
The greatest extent of change was noted on the PICS scores, with almost two-thirds of participants reporting improvements in overall function and mood and half reporting improved physical activity and some improvement in pain. The benefits of the group dynamic along with the program’s emphasis on engaging in meaningful activity, therapeutic movement and mindfulness may influence the reported improvements in these scores. PICS are increasingly being recognised as influential outcome measures in clinical trials for chronic pain treatment58. They have been recommended for use as a core outcome measure for chronic pain trials and have been advocated for improving the applicability of information from clinical trials to clinical practice59. Similar to the pattern observed in the current study, previous studies have shown significant improvements in PICS without significant improvements in other outcome measures60. This discrepancy highlights that PICS may be a more sensitive measure for evaluating an individual perception of the influence of pain management programs on their functioning and pain state.
In their review of telehealth services in rural and remote Australia, Bradford et al concluded that success depends on adaptability and efficiency of the service model in response to patient needs61. During the development of the MYP-SW telehealth model, clinicians (rural and tertiary centres) and patients were consulted, and, throughout the study, health professionals actively engaged patients and remained committed in delivering the program using telehealth. It was therefore positive to note that the majority of participants were very positive about receiving pain management support using telehealth. Participants clearly recognised the opportunities telehealth offered them to help bridge the geographical gap between rural/remote and specialist metropolitan services, and also to connect with other individuals.
The convenience of receiving care close to home was also a highlighted benefit. Convenience is important when patients are considering participation in programs that require a substantial time investment over several weeks. Recent data reported for cardiac rehabilitation programs indicate that participation rates can be as low as 10–30%62. In the present study, only half of the referred patients accepted the opportunity to participate. While reasons for this were not specifically explored in the present study, work and home commitments were cited by many. Hence it could be assumed that participation rates would be even lower if patients had to fly to the hub site to receive the program using intensive face-to-face delivery.
Participant comments also highlighted that the benefits of groups: working together with a group was able to be achieved, even in the online environment. Nearly all participants felt connected with other participants in the group and felt the group experience fostered a shared experience of learning. Participants indicated that using the multisite group model created a community that provided validation and support regarding their persistent pain experiences. Their sense of being isolated in relation to their experiences of persistent pain was reduced because they were able to have their persistent pain experiences validated by hearing from others in the multisite telehealth group. This is an important finding because studies have shown that perceived levels of social isolation can be a predictor of disability related to lower back pain63.
Zhou et al reported that, in their pilot videoconference group project, technical interference compromised group connectivity28. In comparison, the present study experienced minimal technical difficulties, with no connection dropouts or significant visual and audio issues that prevented a successful session. Control of extraneous noise from each of the multiple sites was, however, an ongoing issue, necessitating ongoing reminders to remain on mute when not engaging with the group. From the user end, individuals with existing vision or hearing impairments had some issues with engaging using telehealth. In any telehealth service it is important that systems have the flexibility and design capabilities to adjust to and accommodate patients with varying levels of function and physical comorbidity64. Options such as maximising audio outputs at the patient’s site or using headphones while using videoconferencing units with larger screens can improve the visual display so people at each site can be viewed more easily. Other issues specific to this pain population, such as the need to occasionally stand and move around, can also impact the distance from the microphones and camera. Compensating for this with wider angle camera settings and lapel microphones can be effective in these situations.
Limitations
The present cohort was relatively small – numbers were directly influenced by the available population in this rural health service during the study period. However, the sample size was sufficient to demonstrate that a positive change in pain-related function is possible, and participant perceptions were highly consistent regarding the benefits of telehealth and successful formation of a group using the service. Limited demographic information was collected on the study participants, because the focus of the research was on examining the feasibility of implementing a telepractice model, not the efficacy of pain management groups. Similarly, the efficacy of the pain program used in this study has not been validated in a face-to-face format. The study was not explicitly linked to an implementation framework but the design and outcomes align with those recommended for evaluating musculoskeletal modes of care65. In the analysis, ‘reliable change’ was used to determine if there were any clinically meaningful differences within the cohort; however, it is acknowledged that converting a continuous score into a dichotomous measure does have significant weaknesses66. The absence of any long-term monitoring of the group outcomes also limits discussion of the maintenance of the benefits observed in this cohort. Finally, patient and service costs were not examined for this model. As part of any economic evaluation, it would be important to consider benefits other than traditional travel expense and service staff cost savings. Issues such as whether having convenient access to pain services using telehealth improves uptake of pain services, compared to the traditional option of travelling long distances to the specialist hub site, could highlight other potential benefits of this service model.
Conclusions
This study aimed to examine both the feasibility and effectiveness of delivering a persistent pain management program using a multisite telehealth group model, and to examine consumer perceptions. The study found that participants benefited through improvements in pain acceptance and pain interference similar to that of face-to-face programs. Participants also reported improvements in overall function, mood and physical activity, and some reported improvements in pain levels. The perceptions of the telehealth experience were positive overall, with the participants benefiting from accessibility and experiencing group cohesiveness with minimal technical difficulties. The high consumer ratings for the use of the videoconferencing technology reinforces the benefits of its use in health care. This study highlights the potential of group-based telehealth programs for the management of persistent pain for rural/remote participants and provides evidence for the support of telehealth programs to address the issues of rural/remote health disadvantage.
Acknowledgements
The authors acknowledge the support of the clinicians in the South West Health Service district for their assistance with the program: Mrs Amanda Ashton, Ms Kylie Sutton and Allied Health Assistants Ms Kim Duncan and Ms Angela Orupe. The authors acknowledge the senior clinicians at the Gold Coast Interdisciplinary Persistent Pain Centre for developing the content and presenting the program: Dr Karl Bagraith, Mr Anthony Hall, Mrs Margaret Vandermost and Mrs Tara Malone. The authors acknowledge the funding provided by the Health Practitioner Research Grant Scheme 2016–2017.


