Introduction
Primary health care (PHC) is the foundation of healthcare systems around the world, recognized for its ability to deliver efficient, equitable, high-quality, patient-centered care1. Defined simply, PHC is ‘the broad range of primary prevention (including public health) and primary care services within the community, including health promotion and disease prevention; the diagnosis, treatment, and management of chronic and episodic illness; rehabilitation support; and end of life care'2. In 2008, WHO called for the ‘renewal’ of PHC and, globally, many countries have undertaken major PHC reforms in the past 10–15 years3,4.
In Canada, the College of Family Physicians envisioned a model of comprehensive PHC, the ‘Patient’s Medical Home’ (PMH), as the ‘central hub for the timely provision and coordination of a comprehensive menu of health and medical services patients need as well as a place where patients feel most comfortable discussing their health concerns'5. The PMH is supposed to be led by a team of clinicians (family physicians, nurses, and other health professionals) and patients who also hold some responsibility for taking an active role in their care. This model is an example of the kind of reimagining of PHC that has taken place in many jurisdictions over the past 15 years.
As innovative PHC models have developed, so has the need to evaluate their effectiveness. By measuring and reporting on PHC performance, decision-makers can ensure quality improvement and accountability at the practice, community, regional, and national levels1. This is no easy task, since the ideal performance measurement framework has to align the needs of the various levels of the healthcare system with local and community priorities so that there is buy-in from stakeholders – patients and the public, as well as clinicians, administrators, and governments4.
Performance measurement and reporting in PHC need to ensure geographic context is taken into account. While the studies in this article’s results define rurality in a variety of ways, our conception of rurality is aligned with Statistics Canada’s ‘rural and small town’ designation: the areas including small towns and municipalities outside the commuting area of large urban centers (centers with populations exceeding 10 0006). These rural areas, where residents are fewer and widely dispersed across vast areas, present challenges for PHC delivery. For example, rural PHC clinicians offer care in their clinics during the day but may staff the emergency department (ED) during the evening and overnight, and may in fact tell their patients to come to the ED if they need care during these times. In more urban areas, not only do patients have other options (eg a walk-in clinic) for care, but they are unlikely to see their clinician if they were to go to the ED after hours. Understanding the ways in which rural PHC differs from non-rural PHC is therefore a crucial step in developing accurate performance systems for the rural setting.
This scoping review aims to answer the following question: ‘What structural and organizational factors of primary healthcare performance should be measured and taken into account in a rural context?’ Because PHC performance measurement and reporting for the rural context has not been well studied, a scoping review is a particularly appropriate research method. This review maps the existing literature and helps guide further research, a crucial next step to advancing PHC outcomes in rural communities.
Methods
This scoping review follows Arksey and O’Malley’s7 general five-stage approach and is informed by Levac et al’s suggested refinements: (1) identify the research question;( 2) identify relevant studies; (3) select studies for data extraction; (4) extract and chart data; and (5) summarize and report results8.
Searches were limited to articles comparing rural with non-rural aspects of PHC, written in the English p, and published between 2003 and 2017. The year 2003 was chosen as a start date as this coincides with Canada’s First Ministers’ Accord on Health Care Renewal, a document that set out a new vision for a sustainable and accessible healthcare system9.
All searches were conducted in June 2017. Initial limited searches in PubMed were conducted to identify relevant key words and medical subject headings (MeSH), and were used to identify appropriate measures of quality PHC (described below). Full searches were then conducted in the electronic databases PubMed, CINAHL, and Scopus. The grey literature was also searched, including Australian, Canadian, US, and UK government websites and research institutes, as well as the databases Canadian Electronic Library, OpenGrey, and Grey Literature Report. In PubMed, search terms included both key word and MeSH, while key words alone were used for searches in the other databases and websites (Table 1). Search strategies were left deliberately broad to ensure capture of relevant articles. Any published or unpublished literature (whether peer-reviewed or other) was considered.
Identified articles were eligible for inclusion if they reported or described (1) practice characteristics or structures, physician scope of practice, physician practice patterns, or patient patterns of health care use. Articles were excluded if they reported or described (1) specific patient populations, health concerns, or health outcomes; or (2) patient/clinician preferences or experiences with PHC. This second criterion was indicated in order to narrow the focus of selected studies to more structural and organizational level concerns. It was determined from initial, preliminary searches that studies focusing on patient and clinician preferences and experiences mostly included practice-level concerns (eg quality improvement measures, such as specific testing capabilities). This review was concerned first and foremost with what structural and organizational factors ought to be considered in performance measurement.
Database searches generated 7413 citations (t1). Reviewing titles and abstracts of these citations for relevancy and eliminating duplicates yielded 72 articles for further analysis. Grey literature searches resulted in two additional articles, and hand-searching the reference lists of these 74 articles generated another five articles, for a total of 79. As described above, date limitations were originally set at 2000–2017, but this was changed to 2003–2017, which excluded 10 further articles, leaving 69 for full-text review. Applying the preset inclusion and exclusion criteria to these 69 articles yielded 26 studies for full review, and it was these studies from which a data extraction table was generated.
Table 1: Database search results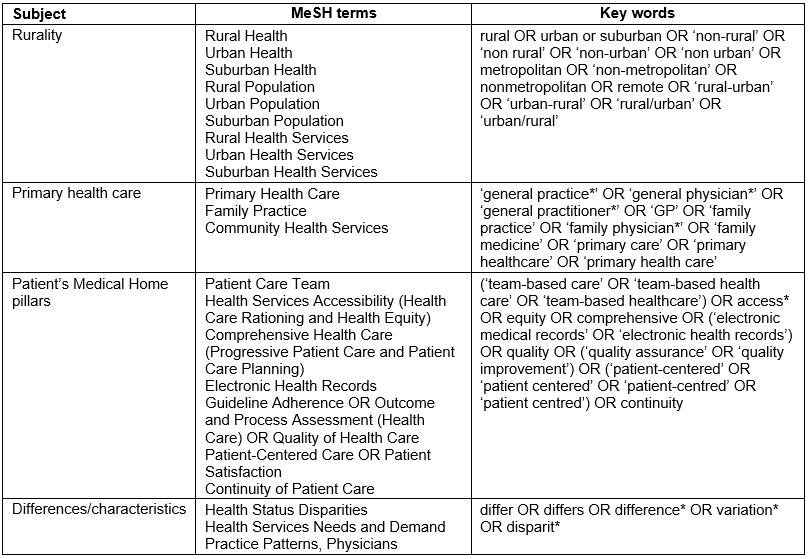
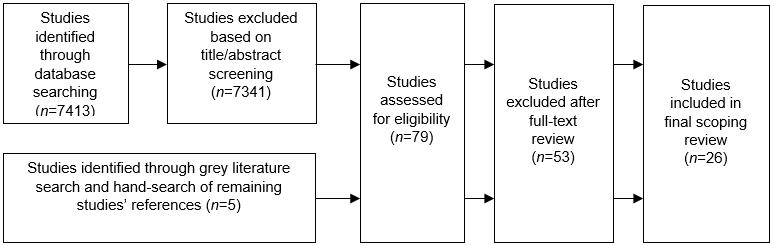 Figure 1: Flow diagram of included studies.
Figure 1: Flow diagram of included studies.
Analysis
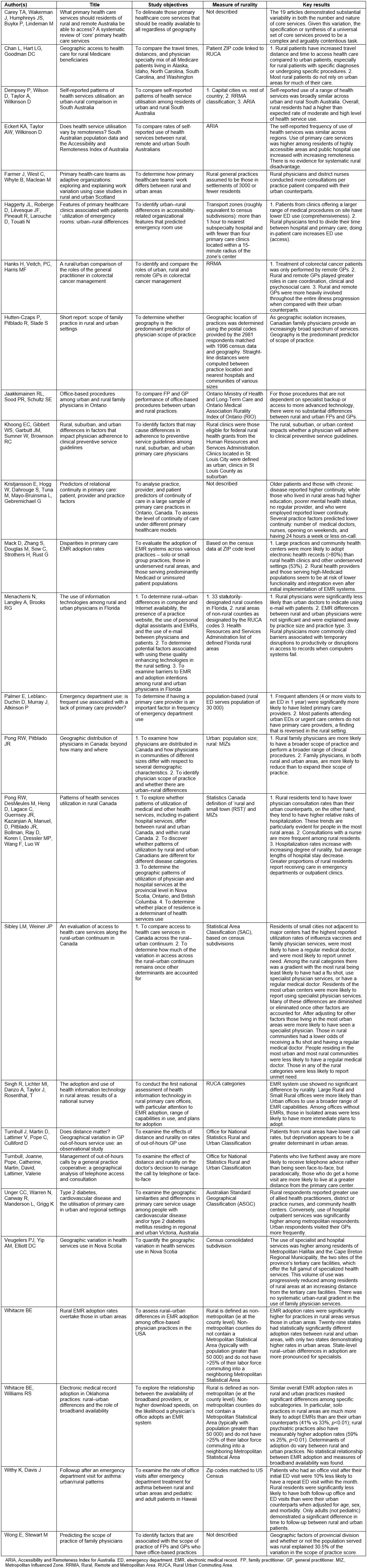
Data extracted from all articles included title, authors, publication date, date of study, demographic characteristics of the study sample, as well as primary objectives. The main results and their implication for rural PHC performance measurement were also extracted. All data were entered in a Microsoft Excel spreadsheet (Table 2). From thematic grouping of the resulting studies found in the literature, the articles were organized into four of the nine pillars of the PMH model. The four were access, continuity, comprehensiveness, and EMR use. They are defined in the model as follows. ‘Access’ means timely access to appointments in the practice as well as ensuring/advocating for timely access for other specialist appointments. ‘Continuity’ means continuity of care, relationships, and information for all patients, including when being delivered in different settings (long-term care, office, hospital, etc.). The model defines ‘comprehensiveness’ as the full scope of family practice services, delivered in conjunction with other team members, as necessary, for patients of all ages. Finally, the ‘EMR’ pillar refers to full EMR functionality, including e-prescribing, clinical decision support, and e-referral functions.
Table 2: Full results of data extraction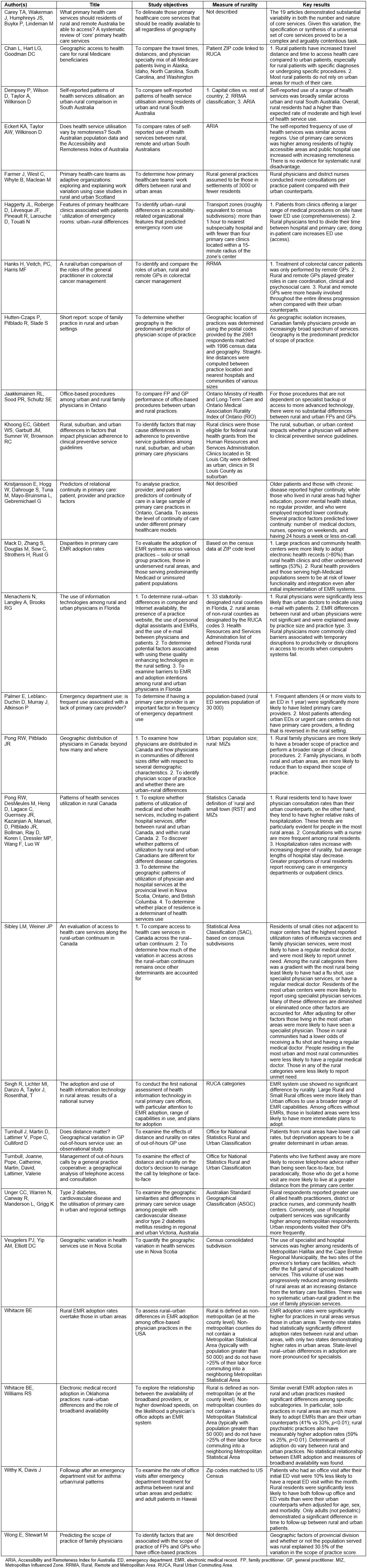
Results
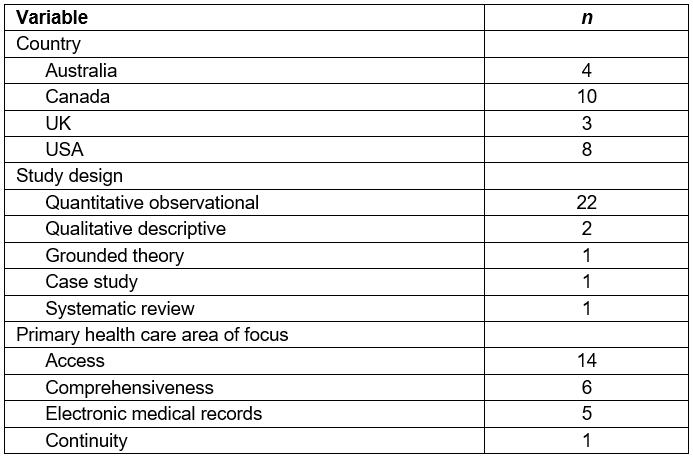
Twenty-six studies were identified for analysis. Table 3 provides an overview of the search results. In brief, 10 of the studies were from Canada, eight from the USA, four from Australia, and three from the UK. The studies’ publication dates ranged from 2003 to 2016, with a median publication date of 2009. Twenty-two of these studies could be considered to have a quantitative observational design. In terms of the PMH ‘pillar’ identified, 14 of the studies were concerned with access, six with comprehensiveness, five with electronic medical records, and one with continuity.
Table 2 shows the full results of data extraction. Key results are described below, organized by the four pillars of quality PHC (access, comprehensiveness, continuity, EMR use) chosen from the PMH model.
Access
Access was a frequently cited challenge for rural patients. As with the other three pillars of PMH, results were somewhat mixed across the studies identified, but some common themes did emerge.
First, rural patients travel greater distances and spend a greater amount of time accessing health care compared to urban patients10. Two studies concluded the frequency of use of health services and the types of services consulted were broadly similar between rural and urban patients11,12. This finding was challenged by two other studies that demonstrated a marked increase in the use of specialist services among urban residents and a greater likelihood of receiving care from allied health professionals, nursing, and community health centers among rural residents13,14.
Several studies commented on the relationship between access to PHC and use of community EDs. Because rural physicians tend to divide their time between hospital and primary care, one study found that when physicians perform in-patient care at an emergency department, their patients tend to access care through the ED15. The behaviour is likely driven by clinicians’ attempts to satisfy their patients’ desire for continuity by making themselves available at EDs. A greater number of rural residents than urban described receiving care from an ED, another reflection of the structure of rural primary care, where EDs often double as primary care treatment centers16. Interestingly, most patients attending rural EDs or urgent care centers have primary care clinicians, but among urban patients attending an ED, this finding is completely reversed (ie urban patients in the ED are less likely to have a PHC clinician), another indication of the rural ED as an extension of PHC17.
One population-based study used a more complex method of determining rural–urban status, so that residents could be placed along a continuum. The study concluded that when such sophisticated measures of rural–urban are used, access to PHC declines among both the most rural and most urban residents18. Interestingly, however, as rurality increased, residents were less likely to report having unmet health care needs despite a decrease in access to PHC. The study’s findings suggest potential differences in expectations between rural and urban patients.
In terms of other clinician and practice characteristics, rural physicians and district nurses conduct more consultations (i.e more visits to clinic) per practice patient compared with their urban counterparts19. Adult asthma patients in rural areas were significantly less likely to have follow-up care for an asthma diagnosis than urban adults20. This finding did not hold for children in rural areas with recent asthma diagnoses, suggesting that, for this group, barriers to access are overcome.
Comprehensiveness
The six studies that provided results about PHC comprehensiveness did so mainly through examining differences in physicians’ scope of practice. Four of the six articles commented on the way increasing rurality is associated with an increase in primary care physicians’ scope of practice, with two of those concluding geography is the main driver behind an individual physician’s scope of practice.
One study of colorectal cancer patients established that primary care physicians spent more time in care coordination and psychosocial care than urban counterparts; in general, these physicians were more involved, and for a longer duration, than urban primary care physicians21. Only the most remote primary care physicians were involved in active treatments for their colorectal cancer patients, findings that support the idea of increasing responsibility and scope of practice with increasing rurality.
EMR use
Results regarding EMR use in the studies reviewed were variable. One study found rural PHC clinicians were less likely than their urban counterparts to adopt electronic records – and if they did adopt, their EMR systems were more likely to have lower functionality and integration22. Another found that any rural–urban differences in EMR use were explained by adjusting for practice size and type, and that rates of use were roughly similar23. Still another found that EMR adoption rates were significantly higher among rural practices compared with urban ones24.
Although one study reported roughly similar adoption rates between rural and urban practices, this similarity ‘masked’ significant differences when accounting for practice size25. For example, solo practices in rural areas were more likely to adopt EMRs than solo urban practices (41% vs 33%). This same study found that, among practices with EMR capabilities, the determinants of adoption varied. This finding was echoed in a second study, which found that, among practices that had not adopted, rural practices were more likely than urban ones to indicate temporary disruptions to productivity and access to records as being a barrier23.
Continuity
In health care, continuity can have different meanings depending on context. For the purposes of this review, continuity is referring specifically to relational continuity, the ‘ongoing therapeutic relationship between a patient and one or more providers’26.
Only one study was concerned primarily with continuity of care, and its survey results described several factors, including rural setting, associated with lower reported continuity27. Other practice factors associated with lower reported patient continuity included a higher number of physicians in the practice, employing nurses as part of the practice staff, weekend appointments, and 24 hours or less per week of on-call services. Practice characteristics are therefore the likely contributor to the differences in continuity reported between geographical settings.
Discussion
This scoping review has identified a small but important set of studies that highlights differences between rural and urban PHC. These differences hold key messages for the development of PHC performance measurement and reporting systems in rural settings. Further research in this area should more directly address the notion of performance measurement and vulnerable populations, including rural patients.
Access
Rural and remote areas frequently describe barriers to accessing health services, including primary care, and so it is not surprising that, of the four ‘pillars’ of PHC selected for analysis, access was the most commonly discussed. Studies described how physicians in rural communities divide their time between hospital- and clinic-based practice15. This has implications for how access to PHC in rural areas is measured. For example, increased ED use among rural patients, a behavior often attributed to a poorly functioning healthcare system, may in fact reflect patient and clinician decision-making around efficient health system structure use. This scoping review did not consider patient decision-making – when and where a rural patient seeks care – but this aspect is certainly present in the literature and is worthy of further attention28,29; measures of PHC performance will need to acknowledge this divergence.
With the WHO’s call for renewal of the PHC system has come innovations in delivery. As models of PHC delivery diversify, performance measures will need to consider how a given model might be encouraging (or discouraging) certain practices among clinicians. For example, PHC models that emphasize collaborative, interdisciplinary care will require a measure of access that can include the work of the various health professionals involved – not just physicians. A model that expects physicians to perform more procedural care will need to be measured and reported on in such a way as to weight such activities appropriately. For rural areas, where healthcare resources are more often scarce, these innovations in PHC delivery are particularly important to measure and report.
Comprehensiveness
This review found consistent evidence for an increased comprehensiveness of care among rural PHC clinicians compared to non-rural clinicians. This wider scope of practice means rural PHC clinicians should be evaluated differently than their non-rural colleagues. One study concluded that geography was in fact the ‘predominant predictor’ of scope of practice30. Three main reasons were postulated for this increase in scope of practice among rural PHC clinicians. First, compensation models that reward a diversity of practice activities can certainly affect scope of practice. In some rural jurisdictions, alternative payment plans can incentivize physicians to provide a sought-after range of clinical services, in contrast to traditional fee-for-service arrangements. Second, the structure of rural PHC, where clinicians may be practicing in different settings (eg hospital and clinic), can explain the variation. Third, existing gaps in the larger healthcare system, whether primary or specialist, can influence clinician behavior. For example, one study in this review found that rural and remote primary care physicians play a larger role in managing colorectal cancer patients21. These patients face increased distances to major treatment centers, and primary care physicians can fill the gap in care when patients aren’t able to access those centers as frequently. Understanding the connection between external pressures and the services provided by individual physicians and PHC clinicians will be crucial for measuring and reporting performance in rural areas.
EMR use
EMR use is the most problematic since keeping electronic records in general is not necessarily associated with better performing PHC. But the literature describes several differences in EMR use in rural and non-rural settings, and exploring these differences can help guide future measurement systems. First, practice size may be a better predictor of EMR use than rurality, likely because larger practices are better able to support implementation of such systems. This review suggests measuring and reporting intent to adopt among non-adopters, as well as comprehensiveness and functionality of EMR systems among adopting practices. Such measures may uncover important rural–urban differences that are not otherwise apparent. It is also worth pointing out that the conflicting conclusions that emerged from the studies identified may be attributed to the 2007–2016 publication dates. As EMRs became more mainstream and included better functionality over this date range, overall patterns of EMR use likely changed. Finally, it is worth considering the impact of increased EMR use in rural areas where clinicians may be more likely to work across multiple settings (clinic, hospital, long-term care facilities). Effective EMR functionality may therefore be a challenge for informational continuity in the rural environment.
Continuity
This review suggests that increasing access and comprehensiveness in a rural setting comes with the cost of lower relational continuity, and evaluating innovations to rural PHC should consider these trade-offs. PHC models that consist of practices with a larger number of physicians and include allied health professionals may wind up increasing access to care at the expense of continuity. Rural patients may be willing to make this trade-off, but further research and consideration of this aspect of PHC in is important.
Limitations
This review has some limitations. The studies identified come from only four countries, all in resource-rich parts of the world: Canada, the USA, Australia, and the UK. This is likely a result of limiting searches to English-language articles. Subjective physician and patient experiences of PHC were excluded from the search, and this decision rendered many qualitative studies ineligible, as described in the methods section.
The studies in this review defined rurality in various ways. Several methods were proposed: population size, often mapped to zip/postal code; specific indices of rurality, such as the Accessibility and Remoteness Index for Australia (ARIA) or the Rurality Index of Ontario (RIO); or official government designations, such as the UK’s Office for National Statistics Rural and Urban Classification or Florida’s Health Resources and Services Administration list of defined rural areas. Whether or not these varying definitions of rurality impact the conclusions that can be drawn is unclear, but it would be wise to consider this limitation in any further research.
The PMH was a useful model for conceptualizing quality PHC, and helped organize the literature search, although it must be acknowledged that using a different way of conceptualizing PHC may have produced different conclusions. Preliminary searches suggested access, comprehensiveness, EMR use, and continuity would be the most useful and frequently discussed PMH pillars in the literature. The model’s pillars not used in the literature search are, for the most part, not explicitly discussed in the literature. Nevertheless, limiting the search strategy to four pillars may have excluded other relevant studies. Finally, it became clear during the literature search that the EMR pillar was unique in the way its studies were identified. A useful way of thinking about this is through the Hogg et al. primary care framework31. In the Hogg framework, PHC is organized into ‘domains.’ In this model, access, comprehensiveness, and continuity are considered ‘performance domains’ concerned with the manner in which services are delivered, whereas EMR use is considered a ‘structural domain,’ a practice-level process31. The conclusions drawn from the ‘EMR use’ studies may therefore need to be considered distinctly from the others.
Associating each of the resulting twenty-six studies with one of the four measures of quality PHC was not without difficulty. For example, comprehensiveness and continuity are closely linked (since comprehensive care often means an increase in continuity of care), and for many of the studies with the ‘comprehensiveness’ label, continuity was a related aspect.
Finally, the 26 studies identified through this review seemed to define clinicians as physicians only, and there was little about the kinds of interdisciplinary and team-based care that might be expected with rural PHC. It was expected that the review process would find studies that commented on the enhanced role of nurse practitioners and other clinical staff in rural areas, but this was not the case. Future study should be done to clarify the role of other clinicians and professionals in rural PHC.
Conclusion
This scoping review mapped the existing literature that describes differences between rural and non-rural PHC across four predetermined pillars of the PMH: access, comprehensiveness, continuity, and EMR use. The 26 identified studies offer valuable evidence that should be considered when developing performance measurement systems for rural PHC. While the PMH model used to organize the results is a North American one, its components are internationally recognized as being significant in designing and delivering comprehensive primary care in all health systems.
This review found that rural residents had a greater likelihood of receiving care from allied health professionals, nursing, and community health centers, and similarly that rural patients reported lower levels of relational continuity overall. The likely explanation is that rural residents are generally underserved by PHC providers, and so are often forced to seek care from whomever is ‘on call’ at that particular time. The use of collaborative practice models in rural areas may also contribute to this phenomenon, and further research should continue to examine the ways such models affect patients’ perceived continuity of care.
Studies in this review describe an increased use of the ED among rural residents compared with non-rural residents. Interestingly, most patients attending EDs or urgent care centers in rural areas have primary care providers, a finding reversed for urban EDs (ie urban patients in the ED are less likely to have a primary care provider). It may be that rural residents are seeking primary care from EDs not only because it is the only option available to them, but also because their PHC provider may be accessible through the ED during off-hours. Further research should clarify this dynamic as it has implications for how PHC performance is evaluated.
Finally, the studies selected for this review were clear that rurality is associated with an increased scope of practice among primary care physicians. There was evidence that urban residents use more specialist services than non-urban residents do. Measuring the performance of rural PHC physicians, then, will need to account for their apparent increased scope of practice compared with their non-rural colleagues.
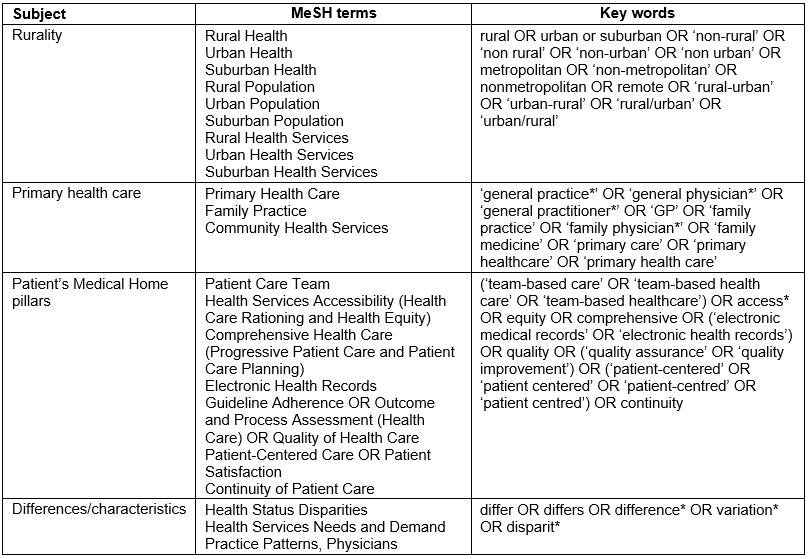
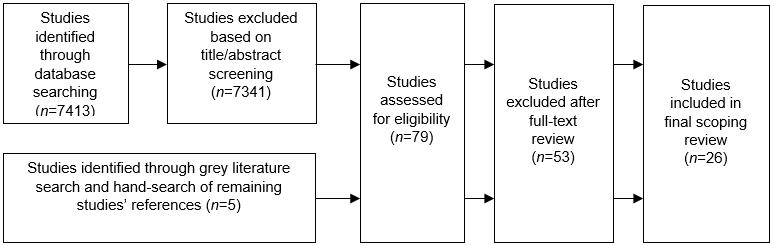 Figure 1: Flow diagram of included studies.
Figure 1: Flow diagram of included studies.