Introduction
Geographic maldistribution of urban over rural medical practice exists worldwide. One reason for this is that most medical schools do not consider producing doctors for practice in their country’s medically underserved areas to be a central part of their mission1. Another reason is that the majority of doctors practise in the same region in which they complete their postgraduate training, often in an urbanised, well-resourced region close to a major city2. In response to these and other reasons, the James Cook University (JCU) medical school, Queensland, Australia, and the Northern Ontario School of Medicine (NOSM), Ontario, Canada, entered into a ‘social contract’ with communities in their respective regions to train medical learners locally, with the aim of producing graduates willing and able to address local regional, rural and remote medical workforce needs.
Both JCU and NOSM have their curricula built on the core educational and social values of ‘socially accountable’ medical education: recruiting students from local communities with the greatest healthcare needs; having learning occur in local communities, as well as in university and tertiary hospital settings; having curricula focused on primary care and aligned with the health needs of local communities; recruiting community-based practitioners as teachers; having faculty emphasise and model commitment to community service; and taking a ‘whole of school’ approach to these principles3.
JCU combines a number of strategies shown to increase the likelihood of graduates working in the local (predominantly rural and remote) area: preferentially selecting applicants with a local or rural origin4-6 and/or a preference for specialising in general practice7,8 or rural medicine9,10, and then providing successful applicants with early, repeated and extended exposure to rural and remote experiences during undergraduate training11-14. Records show that the JCU medical school draws students predominantly from northern Australian or rural communities (approximately 60% of total intake) and, as a likely consequence of this selection strategy and other curriculum and early-career training factors15, the JCU medical school’s graduate tracking database shows positive local medical workforce outcomes. For example, almost 50% of the first seven graduating cohorts chose a family practice career, with a further 25% pursuing other general specialties16,17, and approximately 40% of all JCU medical graduates were practising in northern Australia during 2019 (JCU medical school tracking database statistics).
Consistent with its social accountability mandate, NOSM Distributed Community Engaged Learning establishes a comprehensive life-cycle approach from high school, through medical school and postgraduate training, and into continuing medical education18,19. For instance, NOSM’s admissions process selects medical students who reflect the population of northern Ontario20. Once in the program, students or residents in NOSM’s medical education or postgraduate training programs learn in over 90 communities, with the majority of these communities located in northern Ontario21. Data from the Canadian Resident Matching Service for 2009 to 2016 show that 61% of NOSM graduates match to family practice residency spots versus 35% for all Canadian medical school graduates for the same eight cohorts22. Evidence from the first three cohorts of NOSM-trained doctors showed that 45% of family practice doctors were practising in northern Ontario23.
It is becoming accepted that a key strategy for promoting doctors into local practice is to establish a pathway in which students from the region are selected and offered undergraduate and postgraduate clinical training activities in the region, including rural training places24. Recruitment and retention in the local area require adequate numbers of well-supported postgraduate training places across all medicine disciplines.
This study examined the association between local postgraduate training and the current practice location of JCU medical graduates who completed training in their chosen specialty, and the current practice location of NOSM doctors who completed either their undergraduate medical education or postgraduate training or both with NOSM in northern Ontario prior to establishing independent practice.
Methods
Undergraduate and postgraduate medical training in Australia and Canada
In Australia, medical students undergo 4 years of medical education in one of twelve graduate-entry medical schools (Route VI in Table 1) or 5–6 years in one of seven secondary school entry medical schools (Route II in Table 1) (with three schools offering both types of program)25. Undergraduate medical education is based at the university, in hospitals, and in other clinical settings. Graduates then undertake 1 or 2 years of clinical service as junior doctors, mostly in hospitals, followed by entry into vocational training. This vocational training or postgraduate medical education is overseen by one of the 24 medical colleges and takes the form of in-service training combined with clinical service delivery. The trainees, usually known as residents or registrars, apply each year for a new appointment while pursuing studies to prepare to sit the certifying examinations to become a Fellow of the relevant medical college. In Australia, the term ‘Fellow’ is used to describe a doctor who has completed advanced training to become a specialist. The colleges set the standards, accredit training positions and, through the Fellowship examinations, award entry to specialty vocational registration. After completing vocational training, the doctors then enter unsupervised clinical practice with the requirement to keep up to date through continuing medical education.
In Canada, all medical students complete a university degree before undergoing 3 or 4 years of undergraduate medical education at one of 17 medical schools and then graduate with a Doctor of Medicine (MD) degree (Route V in Table 1). This is followed by 2–5 (or more) years of training in a residency program administered by one of the medical schools: 2 years to become a family practitioner certified for unsupervised clinical practice by the College of Family Physicians of Canada (CFPC), or 3–5 years of training to become specialist certified by the Royal College of Physicians and Surgeons of Canada (RCPSC), which may include additional training to become certified as a subspecialist.
Table 1: Differences in stages of medical education and terminologies between the James Cook University medical school in Australia and the Northern Ontario School of Medicine in Canada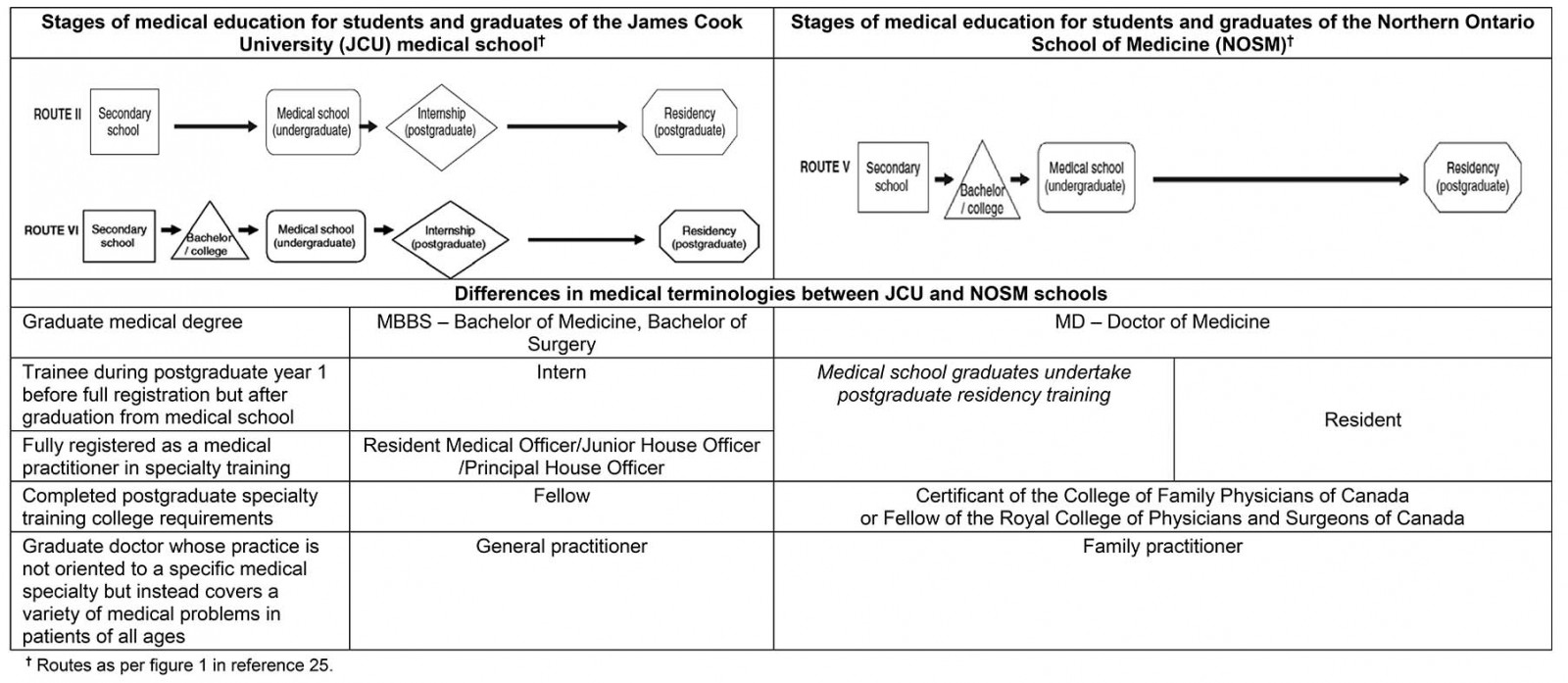
JCU’s and NOSM’s respective service areas
JCU’s service region of northern Australia (Fig1) constitutes about half of the total area of Australia. Although it includes only about one quarter of the Australian population, it has significantly higher proportions of Aboriginal and Torres Strait Islander peoples (14% in northern Queensland and 30% in the Northern Territory). Relative to the rest of the Australia, JCU’s service region is less populated, less developed and has poorer access to healthcare services, as well as often poorer health outcomes, particularly for the Aboriginal and Torres Strait Islander population26.
NOSM’s service region in northern Ontario was defined in 2005 to include the area contained within three (former) northern Ontario District Health Councils (Fig2)27. In 2016, the region included 860 000 people living in an area of 807 000 km228. Approximately 55% of the population live in five urban centres with 42 000–162 000 people. Relative to all of Ontario, NOSM’s service region has a higher percentage of two cultural-linguistic minorities: Indigenous people (14% v 2%) and Francophones (18% v 5%)29-31. As in Australia, NOSM’s service region is less densely populated, less developed and has poorer access to healthcare services, as well as poorer health outcomes relative to the rest of Ontario32,33. Similarly to Australia, Indigenous and Francophone minority populations typically have worse health status34,35.
 Figure 1: Map showing region of northern Australia, designated as ‘from Rockhampton to the north, and west to the Northern Territory and to Carnarvon in Western Australia’.
Figure 1: Map showing region of northern Australia, designated as ‘from Rockhampton to the north, and west to the Northern Territory and to Carnarvon in Western Australia’.
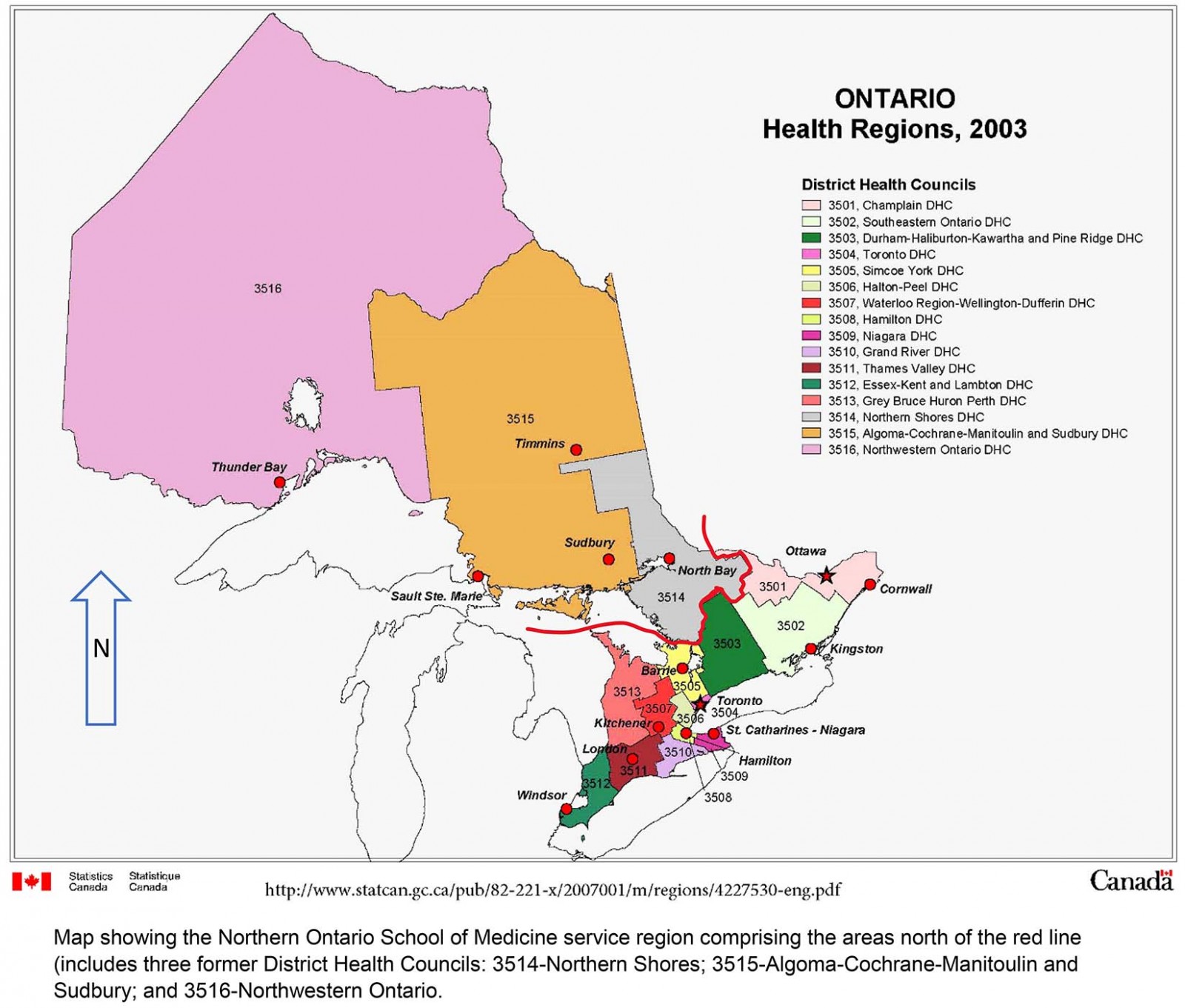 Figure 2: Map showing the Northern Ontario School of Medicine service region comprising the areas north of the red line (includes three former District Health Councils): 3514–Northern Shores, 3515–Algoma-Cochrane-Manitoulin and Sudbury, and 3516–Northwestern Ontario.
Figure 2: Map showing the Northern Ontario School of Medicine service region comprising the areas north of the red line (includes three former District Health Councils): 3514–Northern Shores, 3515–Algoma-Cochrane-Manitoulin and Sudbury, and 3516–Northwestern Ontario.
Study design
A cross-sectional design was used to obtain data on JCU and NOSM graduates.
JCU graduates: The first nine JCU medical graduate cohorts were surveyed (from 2005 to 2013, practising in postgraduate (PGY) years 5–13), based on a list of graduates who had given consent to be contacted. The study focused on JCU PGY 5 graduates onwards, because many PGY 1–4 graduates are spending their early careers gaining experience relevant to their future career plans and starting to enrol in their chosen postgraduate training pathway; from PGY 5 onwards, graduates have begun to obtain their Fellowship.
Consent for further contact was collected in the annual exit survey of final-year students, which has been conducted since 2005 and includes a request for permanent email and mobile phone details of students. Overall, 529 of the total 770 graduates in the first nine cohorts gave their consent to be contacted for further research.
The survey was administered in March 2019 via SurveyMonkey and mobile phone text to 529 JCU medical graduates who had given consent for future contact. The survey asked respondents a variety of questions, including, ‘What town did you practise in for the majority of 2018?’, ‘What career/training pathway are you currently undertaking (or have completed)?’, ‘In what hospital/town did you enrol in your specialty training pathway, and in what year?’ and ‘Did you move to another hospital(s) or town(s) as a requirement of your training pathway? If yes, please list …’.
All data were coded numerically and entered into the Statistical Package for the Social Sciences v22 (IBM; https://www.ibm.com/analytics/spss-statistics-software). Current practice location (in 2018) was categorised dichotomously into whether or not the town was in northern Australia (from Rockhampton northwards, and westwards to the Northern Territory and to Carnarvon in Western Australia). Similarly, each hospital/town that the participants practised in while enrolled in a postgraduate training pathway was categorised dichotomously according to whether the hospital/town was situated in northern Australia.
Completion of postgraduate training was confirmed by accessing the Australian Health Practitioner Regulation Agency website (http://www.ahpra.gov.au). Graduates were removed from the analysis if they had not completed their Fellowship (n=39), had chosen non-specialist hospital practice (n=2) or were currently not practising as a doctor in Australia (n=7).
Binary logistic regression was used to test the association between doctors currently (2018) practising in northern Australia and having trained in a northern Australian location at least once during their postgraduate specialty training. Separate analyses were conducted for general practice (including rural generalist), general specialist disciplines (general medicine, general surgery, general paediatrics, geriatric medicine, emergency medicine, general psychiatry, anaesthesia, public health, and obstetrics and gynaecology) and subspecialist disciplines (surgical and medicine subspecialties, psychiatry subspecialties such as addiction medicine, intensive care medicine, dermatology, and diagnostic specialties such as radiology and pathology).
NOSM physicians: Researchers at the Centre for Rural and Northern Health Research (CRaNHR) obtained data for 409 NOSM-trained fully licensed physicians from administrative records held by NOSM and from 10 provincial and three territorial regulatory agencies that are responsible for licensing medical doctors in Canada (eg the College of Physicians and Surgeons of Ontario). These licensing agencies have information in the public domain on doctors’ practice location and their medical education and postgraduate training. Practice location data were extracted in November 2018 for all physicians who had completed residency in 2017 or earlier. The minimum of a 1-year delay was chosen because in their first year some doctors take time off after residency, some are mobile, others undertake locums, and a few take additional training. Research ethics boards at Laurentian University and Lakehead University, which serve as the host universities for NOSM, have provided ethics approval since the study’s inception in 2005, with approval renewed every 3–5 years.
CRaNHR’s study of NOSM’s medical learners (medical students and postgraduate residents) followed three groups (pathways) of doctors defined by the school at which the doctor completed their undergraduate medical education and their postgraduate residency training (undergraduate/postgraduate pathway): NOSM undergraduate and NOSM postgraduate, NOSM undergraduate and other school postgraduate, and other school undergraduate and NOSM postgraduate. Graduates in these pathways are further distinguished by broad specialty groupings: CFPC family practice specialty and eight RCPSC specialties offered through NOSM in northern Ontario (anaesthesiology, general surgery, internal medicine, obstetrics and gynaecology, orthopaedic surgery, paediatrics, psychiatry, and public health and preventative medicine).
NOSM MD graduates who undertook postgraduate training in RCPSC specialties that were not offered at NOSM were excluded because there is no NOSM postgraduate comparison group. International medical graduates were excluded because these doctors can only appear in the Other school undergraduate/NOSM postgraduate group and cannot be used to compare among pathways. In November 2018, family practitioners would have finished their postgraduate training 1–7 years previously, whereas RCPSC general specialists would have finished their residency training 1–5 years previously.
Data were entered and coded into the Statistical Package for the Social Sciences v24 (IBM; https://www.ibm.com/analytics/spss-statistics-software), which used binary logistic regression analysis to predict whether the doctors practised in northern Ontario based on undergraduate/postgraduate pathway, specialty group, and the interaction between pathway and group.
Ethics approval
Ethics approval was provided by James Cook University Human Research Ethics Committee (#H1804 and #H6921), Laurentian University Research Ethics Board (#6020443) and Lakehead University Research Ethics Board (#1467348).
Results
JCU graduates
There was a total of 770 JCU medical graduates in the first nine cohorts, of whom 241 did not provide consent for follow-up contact. Of the 529 graduates who consented, emails and/or text messages bounced back from 203, which delineated an effective survey sample of 326 graduates. Surveys were returned by 197 graduates who had completed at least PGY 5 by 2018. This yielded a gross response rate of 26% (197/770) and an effective response rate of 60% (197/326). Of the 197 respondents, 149 had obtained a Fellowship from a postgraduate training pathway, in family practice (57/149, 38%), general specialist (42/149, 28%) or subspecialist (50/149, 34%) disciplines.
Overall, 38% (56/149) of the JCU graduates who had completed their Fellowships were currently practising in 2018 in the JCU medical school’s reference area of northern Australia (Table 2). Significant associations between training in a northern Australian hospital at least once during postgraduate training with current northern Australian practice were found for all three discipline subgroups: family practitioner (p<0.001; 30/36 v 3/21; prevalence odds ratio (POR)=30.0; 95% confidence interval (CI): 6.7–135.0), general specialist (p=0.002; 11/19 v 1/23; POR=30.3; 95%CI: 3.3–273.4) and subspecialist (p=0.027; 9/25 v 2/25; POR=6.5; 95%CI: 1.2–34.0).
Marked differences in percentages across the three subgroups were found with respect to currently practising (or not) in northern Australia, and training in a northern Australian hospital (or not). Family practitioners were more likely to currently practise in northern Australia (58%, 33/57) compared with general specialists (29%, 12/42) and subspecialists (22%, 11/50). The proportion of Fellows having trained in at least one northern Australian hospital but not currently practising in northern Australia also varied between subspecialist (64%, 16/25), general specialist (42%, 8/19) and family practice (17%, 6/36) disciplines.
Table 2: Association between James Cook University medical graduate Fellows (n=149) spending some time training in northern Australia for their postgraduate specialty training pathway with whether or not they are currently practising in northern Australia (All Fellows completed their undergraduate medical degree at James Cook University.)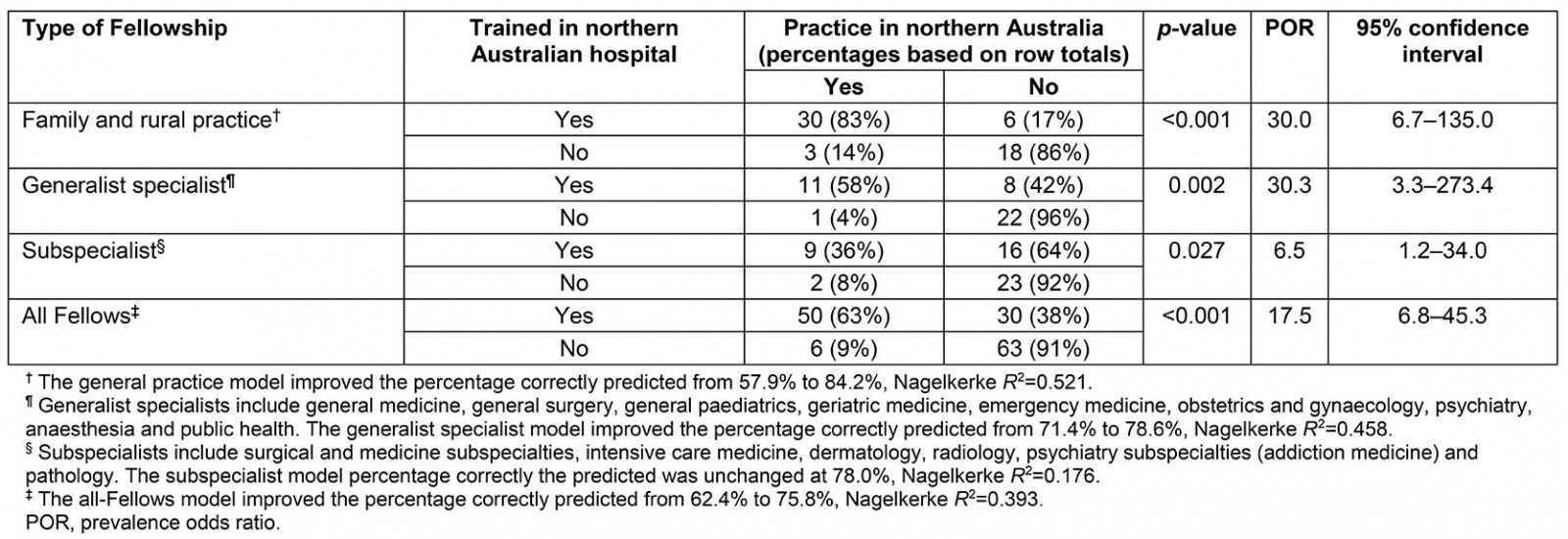
NOSM graduates and residents
The CRaNHR tracking study of NOSM graduates and residents had 485 records of fully licenced physicians who had completed their undergraduate, postgraduate or both studies at NOSM and have been in practice for at least 1 year as of November 2018 as a family physician or an RCPSC generalist specialist. The study excluded 76 international medical graduates who completed their undergraduate medical education outside of Canada, which yielded 409 doctors for analysis. The November 2018 practice location was obtained for 97.8% (400/409) of these doctors. Of the 400 doctors, 327 (81.8%) had completed their CFPC residency training while 73 (18.3%) had completed their residency training in RCPSC general specialties.
Binary logistic regression analysis of whether the doctors practised in northern Ontario using models that included undergraduate/postgraduate pathway, specialty group and the interaction showed a strong interaction between the two factors (p<0.035), with differences among undergraduate/postgraduate pathways for CFPC specialty, but not for RCPSC specialty. To simplify analysis and interpretation, separate binary logistic regression analyses were conducted for each specialty group.
Ninety-two percent (115/125) of family practitioners who completed undergraduate medical education and postgraduate training at NOSM stayed to practise in northern Ontario (Table 3). The statistically significant (p<0.001) POR was 36.6 (95%CI: 16.9–79.2) for this group of family practitioners, relative to those doctors who completed their undergraduate medical education at NOSM and went elsewhere for their postgraduate training. In the reference group, only 24% (28/117) returned to practise in northern Ontario. Fifty-four percent (46/85) of family practitioners who completed only their postgraduate residency training at NOSM stayed to practise in northern Ontario with a statistically significant POR of 3.7 (95%CI: 2.1–6.8) relative to the reference group.
There were no significant PORs for RCPSC general specialties (p>0.60). Overall, 30% of doctors from RCPSC general specialties were practising in northern Ontario and this rate did not differ significantly among pathways. The analysis of all NOSM-trained doctors (regardless of specialty group) yielded results similar to that of family practitioners, albeit with smaller PORs.
Table 3: Association between location of medical education and residency training of Northern Ontario School of Medicine-trained medical doctors (n=400) and November 2018 practice location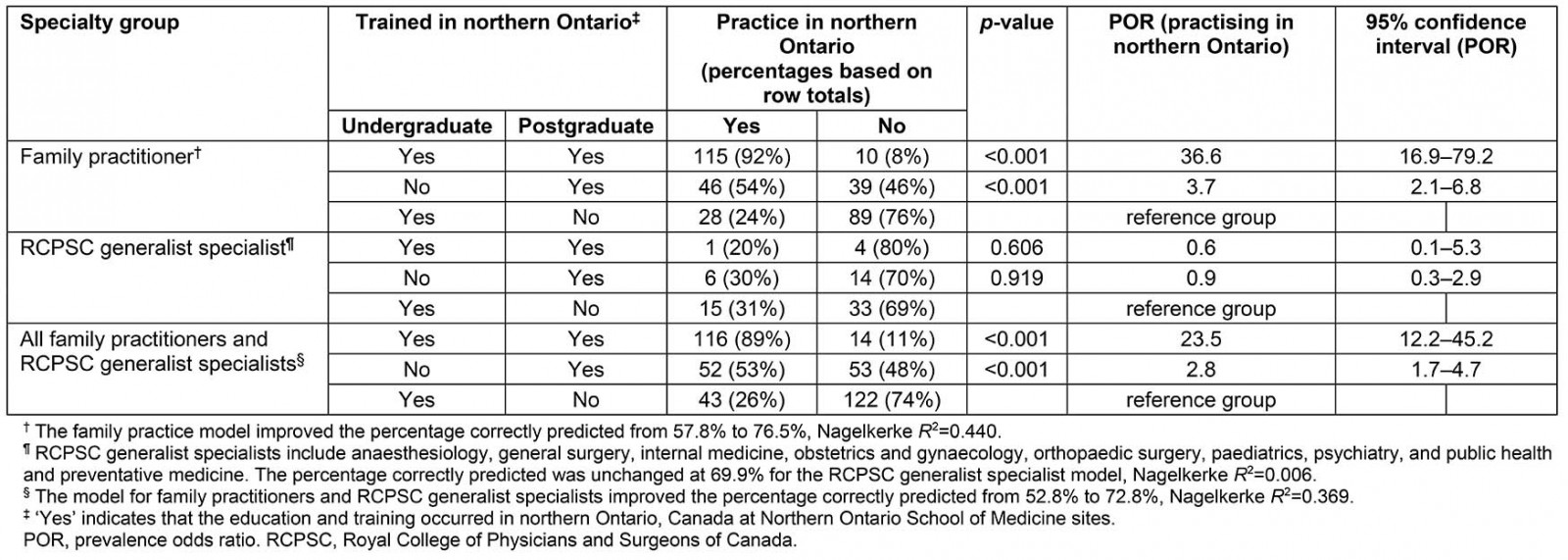
Discussion
This study found that graduates of two regionally located, socially accountable medical schools were more likely to practise in the reference area of their schools when postgraduate specialty training places were more available in the local hospitals and medical facilities. For JCU post-Fellowship doctors in Australia and for NOSM fully licensed family practitioners in Canada, local training was strongly and positively associated with their later medical practice in their respective school’s reference area. In contrast, if their postgraduate training was undertaken outside of the school’s reference area, then only a small percentage returned to practise in the region; 14% returned to northern Australia and 24% returned to northern Ontario.
The findings of the present study are consistent with accumulating evidence for a positive relationship between the location of postgraduate training and the geographic region in which doctors later establish their practice. A 1995 study found that, overall, 51% of doctors stayed to practise in the same American state in which they did their residency, with family practitioners more likely than specialists to stay (OR=1.36, 95%CI: 1.33–1.40)2. A 2018 study of primary care doctors practising across the US state of Michigan found similar trends for specialty groupings, although differences existed between each of the participating Michigan medical schools36.
As previous researchers have noted, a strong association does not mean that there is a strong causal effect – it could be that doctors are choosing a postgraduate training location in anticipation of setting up a practice nearby. Nonetheless, having residency training locations in underserved areas such as northern Australia or northern Ontario provides doctors with the option to train in the region in which they intend to practise. In addition, offering undergraduate and postgraduate medical education in these areas serves to further strengthen social and personal ties to the region, as well as provide the more specific skills and knowledge required for practice in that region.
Thus, these findings suggest that a ‘flipped training’ model may contribute to increasing the number of medical graduates practising in underserved rural and regional areas. The derivation of the concept of ‘flipped training’ is from the ‘flipped classroom’ in education, and refers to the notion that basing specialty trainees in rural or regional clinical settings with some rotations to the cities may lead to better rural workforce outcomes rather than basing trainees in the big cities with occasional rotations to rural/regional settings. In these circumstances, the doctors see their regional or rural centre as ‘home base’ for preparing to practise near where they train, with the city rotations as a necessary requirement to complete their specialty training.
Although there was evidence of a positive pathway effect for all JCU specialty groups, retention of JCU general specialists and subspecialists in the school’s reference area was much lower than for general practitioners/family practitioners. Indeed, the findings of this study show that only about half of JCU’s general specialists and subspecialists trained in northern Australia for any period of time, often starting their Fellowship training in northern Australia but completing in southern metropolitan hospitals, with these doctors rarely returning to practise in northern Australia.
These differences among JCU Fellowship groups may be due to rural general practitioner/family practitioner training pathways now becoming established in northern Australia, such as the Queensland Rural Generalist Pathway for training in rural hospitals and JCU General Practice Training for training in rural medical facilities. This contrasts with the current lack of adequate numbers of general specialist and subspecialist training places from entry to completion of Fellowship requirements in this region for many medical and surgical disciplines.
This lack of local regional training places for general specialist and subspecialist disciplines occurs elsewhere in Australia. For instance, a study of medical graduates from Monash University (Victoria, Australia) found that the effect of having a rural background on subsequent rural practice diminished over time, with the authors opining that it may have been due to a lack of training opportunities or practice support in rural areas37,38. A follow-up study of Monash graduates found a significant association between rural placement duration and eventual rural practice39, while a literature review published in 2019 came to the same conclusion – longer training rotations in rural areas are strongly associated with later practice in rural locations40.
This lack of local training places was also noticeable for NOSM graduates who became RCPSC general specialists – less than one in ten were trained in northern Ontario. There was no evidence of a pathway effect for this group, which may be due to low numbers in the analysis, with only five NOSM MD graduates in the database staying to train at NOSM for their RCPSC general specialty. Most NOSM graduates who stay in northern Ontario for their residency training do so in family practice, and the majority of those seeking training in RCPSC general specialties go to other Canadian medical schools, recognising that those seeking training in RCPSC subspecialties have no choice but to go elsewhere.
Although training in the more subspecialised disciplines will likely continue to occur nearly always in the larger urban centres, numerous initiatives are seeking to raise the profile of rural generalists and other more generalist medical specialties in both Australia and Canada40-44. To counter the lack of general specialist and subspecialist training pathways outside of metropolitan areas of Australia, the Integrated Rural Training Pipeline for Medicine program was implemented in 201745. The program has three components: establishment of Regional Training Hubs to better coordinate training opportunities for junior doctors and build local training capacity, establishment of a rural junior doctor training innovation fund to deliver general practice rotations for junior doctors undertaking their internship in rural areas, and support for an additional 100 places on specialist training programs targeted specifically in rural areas46. One such hub is the Northern Queensland Regional Training Hub, formed as a partnership between James Cook University and local public and private hospitals, health services and general practice clinics in the north Queensland region.
Other potential ways for improving the proportion of doctors practising in the service area of regionally based medical schools would be for the medical school to stay in contact with graduates who are not currently practising in the region via social media (eg Facebook, Twitter), university alumni programs, emails and mobile phone text messages to more widely promote local practice incentives, available specialty training places and other career progression opportunities.
However, with few exceptions, the specialty colleges (other than general/family practice) currently only allow trainees to complete their postgraduate training in large metropolitan teaching hospitals, with few rotations to regional hospitals. The findings of this study suggest that locating full specialty training programs in non-metropolitan areas – the ‘flipped training’ approach of basing trainees in rural or regional clinical settings with some rotations to the cities – should help address the shortage of specialists outside major cities.
Limitations
A number of factors affect where doctors set up their practice once fully qualified, and this study examined only one such factor (postgraduate training location), with the assumption that all other factors were more or less equal among the specialty groups in the study47,48. Evidence for an association between demographic factors such as age or sex and practice location is equivocal, and it seems reasonable that the analyses in this study assumed these associations to be negligible. Having grown up in the underserved region or in a rural area is a strong predictor of practice location and the analyses in this study did not estimate the strength and direction of this association. However, given that JCU and NOSM specifically select medical students from their region and from rural areas, there may not be enough variation among JCU and NOSM graduates in these attributes to detect this association.
Another factor known to strongly influence the number of doctors of a given specialty that can be sustained in a region is population catchment size49. A priori, it was expected that fewer of the highly specialised doctors would be practising in sparsely populated regions of northern Australia or northern Ontario. However, it is a disappointment that only one-third of the Australian and Canadian general specialists were practising in northern Australia or northern Ontario, respectively. Additional research is needed to assess the relative importance of rural or northern background, population catchment size, available residency training places or other factors.
In addition, practice location data for JCU and NOSM reflect early to mid-career practice – not late career, although retention in a community can be high once a doctor has established his or her practice50. While the actual response rate to the JCU survey was reasonable at 60%, only 197 (26%) of the total 770 JCU medical graduates in the first nine cohorts responded to the survey, so selection bias was possible. However, compared with all JCU PGY 5–13 medical graduates with a career choice identified in the JCU longitudinal tracking database, the study sample had similar proportions with respect to postgraduate training in general practice (38% v 46%), general specialty (22% v 22%) and subspecialty (40% v 32%) disciplines. With 98% data coverage for NOSM-trained doctors, any bias caused by missing data should be minimal. However, some groups had small sample sizes, and this may reduce detection of a local pathway effect; for example, only five doctors completed their undergraduate medical education at NOSM and their RCPSC generalist specialty training at NOSM.
Conclusion
The majority of JCU and NOSM medical graduates who qualify to become general/family practitioners stay in their respective medical school’s underserviced reference area for their specialty training and later practice. However, this study found the opposite for JCU and NOSM graduates who chose general specialist and subspecialist postgraduate careers, with less than a third of these undertaking specialty training in the local area and/or continuing to practise in the area once qualified.
These findings are likely the result of the two reference areas having well established general/family practice postgraduate training programs with sufficient training places, but less established pathways and places for general specialist and subspecialist training. Thus, the findings support not only increasing the number of medical schools located in underserved and less urbanised regions, but also locating full specialty training programs in regional and rural centres. Under this ‘flipped training’ approach, specialty trainees would see their regional or rural centre as ‘home base’ with the city rotations as necessary to complete their training requirements while preparing to practise near where they train.
Acknowledgements
We are grateful to the JCU and NOSM medical graduates who consented to be part of this research and thank our colleagues Margaret French at CRaNHR for her help in collecting and processing data, and Professor Tarun Sen Gupta at JCU for reviewing the manuscript. The CRaNHR–NOSM tracking study was initially funded by the Province of Ontario’s Ministry of Health and Long-Term Care (MOHLTC) and in later years by the NOSM. The opinions expressed in this article are those of the authors and are not necessarily shared by JCU, the NOSM or the MOHLTC.
References
You might also be interested in:
2008 - National Centre of Rural Medicine in Norway: a bridge from rural practice to the academy



