Introduction
Colorectal cancer screening
Colorectal cancer (CRC) is a leading cause of morbidity and mortality for men and women internationally, accounting for 6% of all cancer incidence and 9% of all cancer deaths1. Large-scale population screening campaigns utilizing mail-out faecal occult blood tests (FOBT) have been implemented in several countries in order to increase early detection of CRC and improve survival. Population FOBT screening is a convenient, cost-effective and sensitive method of increasing early detection of CRC2-5, yet in many countries, including Australia, the majority of eligible adults do not participate in organised screening programs6,7.
Geographic variation in faecal occult blood screening
CRC patients in regional and remote areas tend to be diagnosed at a more advanced stage of cancer than metropolitan patients and have poorer 5-year survival rates8-12, outcomes that are also more common in individuals who do not participate in national screening programs5,13. Evidence to support geographical disparity in FOBT screening program participation, however, is limited and inconclusive. In Australia, descriptive data from 2016 suggest similar participation rates across metropolitan, outer regional areas and remote areas. However, it demonstrates slightly higher rates in inner regional areas (42%) and substantially lower rates in very remote areas (27%) compared to the national average of 39%14. Other Australian studies have found that, when controlling for demographics such as age, socioeconomic status and cultural status, participation rates are significantly higher in non-metropolitan groups15.
In addition, estimates of participation rates published thus far reflect the proportion of program invitation recipients who complete and return the kit itself (ie participation) rather than the proportion of eligible recipients who do so according to the broader program guidelines (ie compliance)14-16. Program recipients are instructed to complete and return the kit unless they have had a colonoscopy in the past 5 years (or have one scheduled in the following few weeks) or if their GP has indicated that they do not need to complete screening. It is estimated that as many as 25% of people who do not participate in mail-out FOBT screening chose not to complete and return the kit as they had recently had a colonoscopy17,18. As published findings do not take into account whether the kit recipient has already been adequately screened for CRC (ie via colonoscopy or FOBT through a general practitioner or specialist), they tend to overestimate the amount of recipients who actually remain unscreened. When investigating geographical disparities in CRC screening, compliance with CRC screening guidelines is arguably a more indicative measure of preventive health behaviour than program participation alone.
Rural and regional health behaviour
Evidence suggests that approaches to seeking health care may vary between non-metropolitan and metropolitan residents19-21. For example, rural dwellers tend to respond to, rather than pre-empt, illness, focusing effort on curing, rather than preventing, disease when compared to their metropolitan counterparts22. Health concerns in rural areas are also thought to be based more so on the impact they might have on productivity rather than on actual level of discomfort20,22. This reactive approach to health-related help-seeking might explain why regional and rural areas see lower surgery rates and general practitioner visits, but higher emergency hospital admissions rates23. That is, residents may tend not to seek help until a situation becomes very serious, being less likely to pursue early detection and preventative measures. This approach may be more common in non-metropolitan areas partly due to the extra time and effort it takes to get to a medical appointment24.
According to a socioecological theory on the determinants of health behaviour, social and physical environments can heavily influence health behaviours; however, individual-level factors such as attitudes, personality traits and cognitive styles often interact with one’s environment to reinforce behavior25-27. For example, in an environment where medical services and information are scarce, people with attitudes or thinking styles that discourage preventive health behaviour might be particularly unlikely to be up to date with CRC screening. Regional and rural communities are often described as ‘tough’, ‘resilient’ and ‘self-reliant’, characteristics that can be adaptive when faced with adversity or challenges28. However, maintaining health and wellbeing relies heavily on seeking health care and complying with preventive measures in a timely manner. Thus, a reluctance to acknowledge and expose weakness or illness may prove detrimental, particularly in locations that lack accessible health services.
Attitudinal and cognitive barriers to screening
Individual factors including attitudinal traits such as fatalism and stoicism, and cognitive styles that lack consideration for future consequences, have been identified in previous literature as barriers to preventive health behavior29-31. Fatalism is conceptualised within the health literature as a belief that one’s future health is predetermined by fate or destiny31. Fatalistic attitudes are consistently linked to low screening rates for breast, colorectal and cervical cancers32-34. This trend is thought to reflect the tendency of fatalistic individuals to perceive little internal control over, or power to change, the outcome of a positive diagnosis31,33. A related but conceptually different construct known to impact a person’s approach to health care is their consideration of future consequences (CFC). CFC describes the degree to which cognitions regarding future outcomes influence people’s decisions about their current behaviour35. Like high fatalism, low CFC often manifests as reduced attempts to pre-empt or alter one’s future health30. Thus, it is positively associated with the endorsement of CRC screening35,36. Considering the priorities of regional and rural dwellers are often focused on maximising work productivity20,22, attitudes that promote lack of concern or suppress proactive behaviour regarding health are likely to exacerbate delays in healthcare seeking in non-metropolitan areas.
Stoicism, according to modern conceptualisations, manifests in a tendency to endure pain or hardship without complaint or the display of emotion. That is, individuals high in stoicism often avoid appearing weak, vulnerable or in need of help from others29,37. Stoic attitudes to health have been identified as significant barriers to help-seeking. For example, prostate cancer patients with a high need for control and self-reliance are less likely to engage with telephone support services29, and intimate violence victims who tend to minimise or resign to problems are less likely to approach family, friends or professional sources for help38. Interestingly, Australian research linking stoicism to health-related help-seeking comes largely from non-metropolitan samples, inferring that stoic attitudes may be particularly concerning in rural and regional areas29,39,40.
To date, fatalism, stoicism and CFC have not been investigated in terms of their unique effects on health behaviour in rural, regional and metropolitan populations. Based on a socioecological framework, one might expect these individual factors to play a particularly influential role on the cancer screening behaviours in non-metropolitan environments.
The current study
Evidence surrounding geographical disparity in CRC screening behaviour is inconclusive and potentially confounded by geographical differences in the eligibility of residents to participate in FOBT programs (ie prior screening status). Also, the effect of attitudinal and cognitive barriers to compliance with CRC screening programs have not been compared between metropolitan and non-metropolitan environments where both access to health services and approaches to seeking health care differ. Accordingly, two key research questions are addressed in this study: (1) Is there a difference in mail-out FOBT program compliance across rural, regional and metropolitan residents? (2) Are traits such as stoicism, fatalism and CFC significant barriers to screening program compliance in regional and rural areas compared to major cities? It was hypothesised that kit return would be significantly lower in regional and rural areas when compared to major cities and that fatalism, stoicism and CFC would be associated with kit return, particularly in regional and rural settings. Specifically, the authors predicted that high fatalism and stoicism would be associated with lower rates of kit return and high CFC would be associated with higher rates of kit return in regional and rural participants. Findings will inform the development of interventions aimed at increasing the early detection of CRC in non-metropolitan communities.
Methods
Participants and procedure
Australian adults (n=490), aged 50 years or more were recruited via several methods designed to capture a representative sample of metropolitan, regional and rural residents. Participants were largely sought through paid advertising through Facebook and Google Ads. Online advertisements were displayed to potential participants based on what were considered to be the likely interests and subject searches of users in the target group (eg over 50s living, cruises, retirement, bowling and volunteering). Participants were also recruited through personal and community Facebook pages and face to face by researchers at venues frequented by older Australians, such as bowling clubs and community centres. Participants recruited face to face (n=63) were issued a paper version of the survey, whereas participants recruited online completed a digital version through the Qualtrics website (http://www.qualtrics.com). Completing a paper survey was significantly associated with being male, older and having higher socioeconomic status. No significant differences in compliance or attitudinal variables of interest between the two survey methods were evident. Only individuals who reported ever receiving an FOBT kit in the mail as part of the National Bowel Cancer Screening Program were included in the final sample (n=371). Of these participants, 71% were female, ages ranged from 50 to 87 years (mean = 61.26, standard deviation (SD)=7.05) and 75% were born in Australia, with the remaining participants born in the UK (10%), New Zealand (4%) and other countries (11%).
Measures
Remoteness: Level of remoteness was based on participant postcode of residence and classified according to the Australian Standard Geographical Classification – Remoteness Area41, whereby each individual’s residence is coded as metropolitan (n=201), inner regional (n=107), outer regional (n=29), remote (n=17), or very remote (n=6) based on the road distance to their nearest urban centre. Metropolitan residents live in major cities with the highest level of access to services and facilities including hospitals and medical centres, whereas inner regional residents live in smaller cities surrounding metropolitan areas where service and facilities are moderately accessible. Outer regional, remote and very remote residents live in smaller towns and communities with increasing distance from major cities, and have limited access to services and facilities. For the current study, due to small numbers of participants, outer regional, remote and very remote categories were collapsed into one ‘rural’ category (n=52).
Health fatalism (predetermined health): The degree to which participants held fatalistic beliefs about health was measured using a 10-item predetermination subscale from a health fatalism scale31, which includes statements such as ‘If someone is meant to get a serious disease, they will get it no matter what’ and ‘My health is determined by fate’. Items are rated on a five-point Likert scale, ranging from 1 (‘strongly disagree’) to 5 (‘strongly agree’). Mean fatalism scores were calculated by averaging item responses, and higher overall scores represent greater fatalistic attitude. Internal consistency in the current sample was high at a=0.91.
Consideration of future consequences: The Consideration of Future Consequences Scale42 was used to measure the extent to which individuals consider distant consequences of their behaviour. The 12-item scale asks participants to rate the degree to which each statement described them (eg ‘My behaviour is only influenced by the immediate outcomes of my actions’ and ‘I think it is important to take warnings about negative outcomes seriously even if the negative outcome will not occur for many years’) on a five-point Likert scale, ranging from 1 (‘not at all like me’) to 5 (‘completely like me’). Mean overall CFC score was calculated by averaging the item responses, and higher overall scores represent greater CFC. Internal consistency in the current sample was a=0.85.
Stoic attitudes to help-seeking: The need for control and self-reliance (NCS), and minimising problems and resignation (MPR) subscales from Mansfield et al’s Barriers to Help-Seeking Scale were used to measure stoicism43. These subscales consist of items that reflect a desire to avoid being perceived as weak or vulnerable to others (eg ‘I’d feel better about myself knowing I didn’t need help from others’) and the tendency to ignore, suppress or accept discomfort (eg ‘Symptoms like this are part of life; they’re just something you have to deal with’). In the current study, participants were asked to imagine a scenario whereby they were experiencing physical pain or discomfort before reading a list of reasons why they may not seek help for these symptoms. Participants rated the degree to which each reason might stop them from seeking help on a five-point Likert scale, ranging from 1 (‘not at all’) to 5 (‘very much’). Means for each scale were calculated by averaging the scores for each item, and higher overall scores represent greater stoicism. Cronbach’s alpha statistics in the current sample suggested the NCS (a=0.91) and MPR scales (a=0.90) had excellent internal reliability.
Bowel screening program compliance: Participants were asked two questions regarding bowel screening program compliance. Firstly, participants who reported ever receiving an FOBT kit in the mail were asked to report whether or not they had completed and returned it (recorded as ‘participation’). If they had not returned the kit mailed to them, they were asked to select the reason(s) they did not do so. If more than one reason was selected, they were asked to select the reason that had the most influence on their decision. Responses were categorised into valid and invalid reasons. Valid reasons included complying with kit instructions, a general practitioner advising against the test, a recent or scheduled colonoscopy or a recent FOBT through another provider (outside the bowel screening program). Invalid reasons included being unsure or unsatisfied with the FOBT itself, not understanding instructions, the test requiring too much time and effort or being too messy or unpleasant, fear of receiving a positive result, misplaced or forgotten kit, and not being concerned about bowel cancer. Participants could also select ‘other’ and specify a different reason. The validity of ‘other’ reasons specified (n=11) was assessed manually by the researchers, with reasons pertaining to medical conditions or professional advice (n=0) deemed valid. Compliance in this study was defined as either having completed and returned the FOBT kit or having had a valid reason not to, whereas participation was defined as having completed and returned the FOBT kit regardless of eligibility.
Demographics: Each respondent provided their gender, age and postcode, and was assigned a percentile rank based on the Socio-Economic Index for Areas. This reflected their estimated socioeconomic status according to postcode, with a rank of 1 indicating that the participant resided in an area assigned the lowest socioeconomic status and 100 reflecting the highest.
Statistical analyses
Means and standard deviations were calculated for each variable of interest as well as the bivariate correlations between each of them. Four binary logistic regression analyses were run to test the interaction effect of location on the relationship between the four attitudinal variables (CFC, NCS, MPR and fatalism) and bowel screening program compliance, controlling for age, which was negatively associated with rural status and positively associated with compliance in preliminary correlation analysis. Two contrast variables were created and entered into the models to compare (1) regional to metropolitan and (2) rural to metropolitan status. Using the Statistical Package for the Social Sciences data analysis software (IBM; https://www.com/analytics/data-science/predictive-analytics/spss-statistical-software), odds ratios (OR) and 95% confidence intervals (CI) for each effect were calculated. Where interaction terms were non-significant, significant main effects of attitudinal variables were interpreted. A power analysis using a standard online tool44 suggested that 371 was a sufficient sample size to detect at least a small effect (OR³1.50).
Ethics approval
All participants provided informed consent and the study was approved by the University of Southern Queensland’s human research ethics committee (ref. H17REA070).
Results
Table 1 presents bivariate correlations between each of the study variables as well as the means and standard deviations for each of the numeric variables. Compliance with the bowel screening program was weakly associated with NCS, MPR, regional location and rural location and positively associated with age and CFC. (all p<0.05). That is, compliance was more likely in those who were older and with higher CFC and less likely in those with higher levels of NCS, MPR and fatalism.
Table 1: Pearson’s bivariate correlation matrix depicting associations between demographics and all key variables (n=370)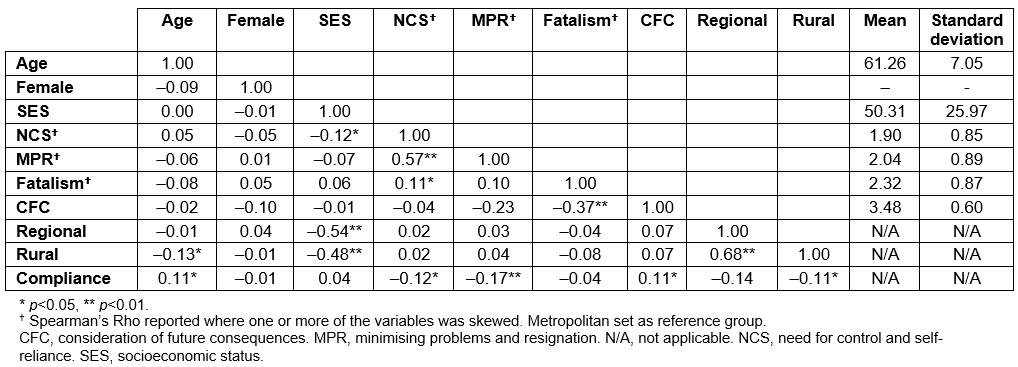
Compliance according to geographic location
In the current sample, 60% of participants reported participation in the bowel screening program, while 74% reported compliance with program guidelines. As shown in Table 2, compliance was significantly lower in regional compared to metropolitan areas (OR=0.49, 95%CI=0.29–0.84), but compliance in rural areas, although 19% lower than in metropolitan areas, was not statistically significantly lower (p=0.18). The proportional differences are visually depicted in Figure 1. Participation in the bowel screening program (number returning the kit v not returning the kit) was not significantly different in regional (p=0.22) or rural (p=0.49) compared to metropolitan areas.
Table 2: Results of logistic regression analyses assessing regional and rural versus metropolitan differences in screening compliance and participation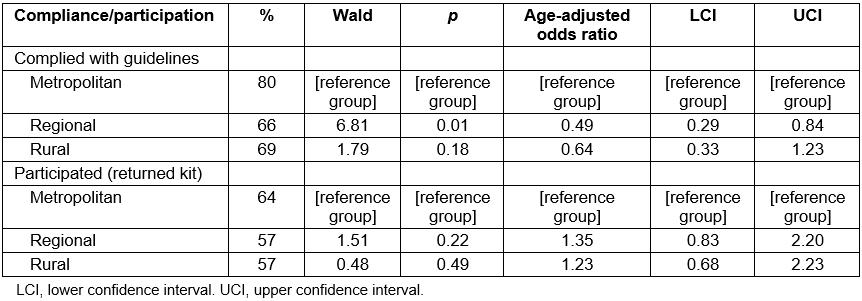
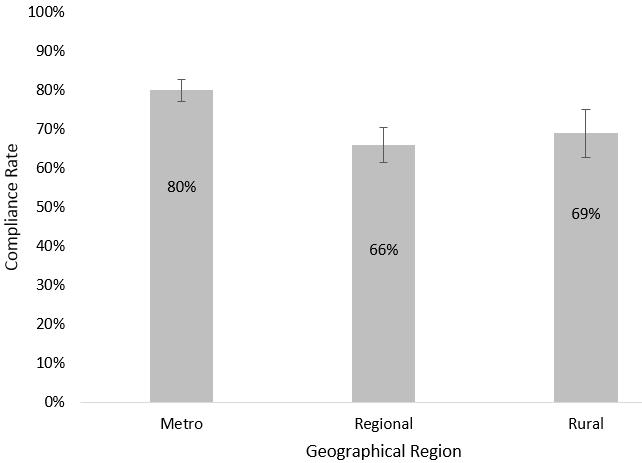 Figure 1. Clustered bar chart comparing the National Bowel Cancer Screening Program compliance rates (percentages and standard errors) in metropolitan, regional and rural areas.
Figure 1. Clustered bar chart comparing the National Bowel Cancer Screening Program compliance rates (percentages and standard errors) in metropolitan, regional and rural areas.
Attitudinal factors and screening compliance
In assessing the impact of attitudinal traits on compliance across regions (Table 3), the only significant main effect was between NCS and compliance (OR=0.75, 95%CI=0.57–0.99), with higher NCS associated with lower compliance. Neither regional (p=0.17) nor rural (p=0.36) status moderated this effect. Rural (OR=0.28, 95%CI=0.11–0.71), but not regional (p=0.16) status significantly moderated the negative effect of MPR on compliance. A simple slopes analysis (Fig2) shows that rural participants who were higher in MPR were less likely to comply with the bowel screening program (OR=0.26, 95%CI=0.11–0.59) than those lower in MPR. This relationship was also apparent for regional participants (OR=0.60, 95%CI=0.38–0.95) although the effect size was smaller in regional areas.
There was no significant main effect of fatalism on compliance (OR=0.90, 95%CI=0.68–1.18) nor did fatalism significantly interact with regional or rural location to predict compliance. Rural (OR=6.66, 95%CI=1.80–24.63) and regional (OR=3.41, 95%CI=1.37–8.44) location significantly moderated the positive effect of CFC on compliance. A simple slopes analysis (Fig3) shows that regional (OR=2.30, 95%CI=1.19–4.43) and rural (OR=4.46, 95%CI=1.39–14.47) participants that were high in CFC were more likely to comply with the bowel screening program than those lower in CFC.
Table 3: Main effects of attitudinal factors and moderating effects of region on relationship between attitudinal factors and compliance with bowel cancer screening program
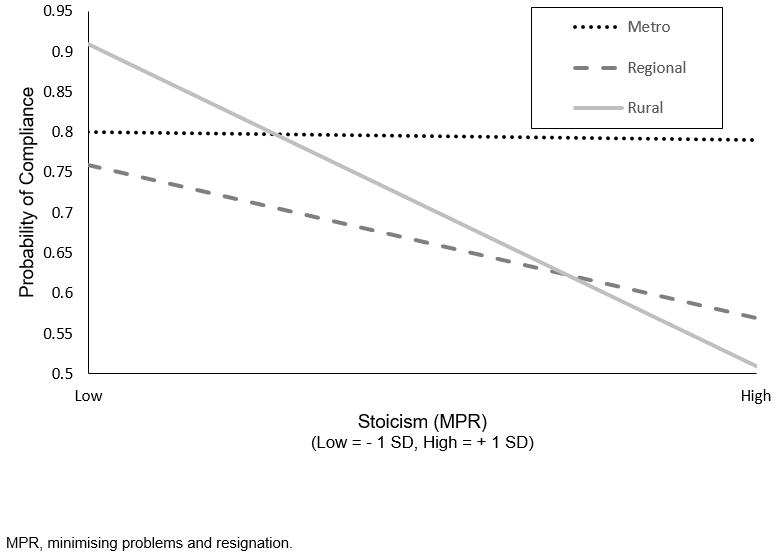 Figure 2: Visual depiction of simple slopes analysis: relationship between minimising problems and resignation and National Bowel Cancer Screening Program compliance for metro, regional, rural groups.
Figure 2: Visual depiction of simple slopes analysis: relationship between minimising problems and resignation and National Bowel Cancer Screening Program compliance for metro, regional, rural groups.
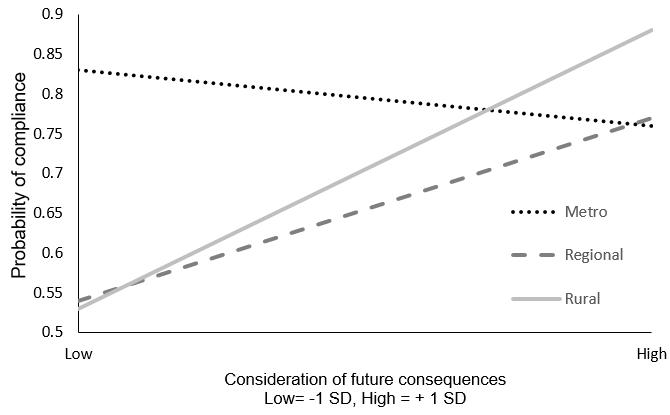 Figure 3: Visual depiction of simple slopes analysis: relationship between consideration of future consequences and National Bowel Cancer Screening Program compliance for metro, regional, rural groups.
Figure 3: Visual depiction of simple slopes analysis: relationship between consideration of future consequences and National Bowel Cancer Screening Program compliance for metro, regional, rural groups.
Discussion
Distributing home-administered FOBT kits via mail should greatly reduce regional inequality in accessing CRC screening services; however, current findings suggest that population FOBT mail-outs are not having this desired effect. Although bowel screening program participation was relatively even across metropolitan, regional and rural areas in this sample, compliance was not. Compliance is defined here as participating in the bowel screening program or having a valid reason not to, which for the most part meant having already been adequately screened for CRC prior to receiving the kit in the mail. One way that these findings can be interpreted, therefore, is that metropolitan residents who did not participate in the bowel screening program were more likely to have already attended to CRC screening whereas, in comparison, inner regional non-participants were more likely to provide invalid reasons (ie those that did not involve prior screening). This is concerning, given that individuals over 50 years who do not participate in early screening are susceptible to CRC progressing undetected and subsequently have a poorer chance of survival should they develop the disease5,13. It may be that addressing poor CRC survival rates in inner regional areas needs to begin with initiatives to promote early detection.
According to the current findings, this tendency for non-metropolitan residents to be less compliant with CRC screening programs is somewhat exacerbated by attitudes and thinking styles that discourage preventative health measures, namely the minimisation of symptoms and lack of consideration for future consequences. Major cities boast extensive health infrastructure in terms of physical resources, activities, organisations and health campaigns45,46. It may be that environmental factors such as physical access to other forms of screening, cultural norms or exposure to awareness campaigns might act as protective factors against barriers to screening, such as stoic attitudes or tendencies to neglect future consequences, in metropolitan areas.
Interestingly, fatalism was not associated with bowel screening program compliance in this sample, which was unexpected given substantial previous evidence to the contrary32-34. These conflicting results might reflect the fact that general health fatalism levels were measured, whereas many studies into fatalism and cancer screening have measured fatalistic attitudes specific to cancer. This might indicate that fatalistic attitudes vary according to the health condition of interest and that it is not appropriate to use general health fatalism measures to predict behaviour regarding specific conditions. A need for control and self-reliance was associated with bowel screening program compliance overall, strengthening findings from previous research that suggest that stoicism is linked to poorer health behaviours37-40. However, in terms of stoic traits, the desire to be self-reliant may not have the same impact on preventative health as a tendency to avoid appearing weak or vulnerable does in non-metropolitan groups.
The present findings support a socioecological perspective on health behaviour, highlighting the importance of considering environmental, sociocultural and psychosocial determinants when addressing geographical disparities in health and health behaviours19,25-27. A one-size-fits-all intervention strategy for increasing compliance rates will be less effective than a series of interventions tailored to target the unique barriers of recipients. That is, uptake in CRC screening programs in metropolitan areas is unlikely to benefit from interventions based on discouraging stoic attitudes and raising awareness of the future consequences of screening behaviour, whereas such interventions might prove useful for residents of non-metropolitan areas, particularly those in rural settings. Furthermore, although MPR and CFC were associated with compliance in both regional areas and rural areas, these factors accounted for less variance in compliance in the regional group. Therefore, attempts to change or alter such attitudes and cognitions may have a weaker impact in regional compared to rural areas. Potentially, people residing in regional areas experience different barriers to compliance that require uniquely targeted interventions. Given the differences in accessibility to services and facilities between the regional and rural groups, unique environmental factors could explain lower compliance in regional areas. Further research may be needed to identify these.
Limitations and considerations for future research
FOBT participation rates in this sample were substantially higher (participation = 60%, compliance = 74%) than the recently published population participation rate of 41% in Australia43. Potentially this highlights a substantial discrepancy between the currently published participation rates and the rate of program participants who have complied with the program guidelines either by completing and returning the kit or by attending to their CRC screening independently before receiving a kit. In order to get a more accurate indication of who is at risk of not being screened, efforts might be made in future to estimate the proportion of kit recipients who have attended bowel screening elsewhere. Given the sampling method, amount or characteristics of non-responders could not be measured, meaning it was impossible to gauge response bias. However, it could be argued that biases (eg inflated bowel screening program participation rates) may be apparent due to the fact that responders were likely to be particularly health conscious and/or more agreeable individuals given that they responded to an invitation to take part in health-related research.
The sample recruited for this study was over 70% female. Given that females tend to be more likely to participate in FOBT screening14, this may also have contributed to the high participation rates recorded. In addition, those living in very remote, remote areas and outer regional areas were grouped together, limiting the ability to delineate participation rates in areas of moderate versus extreme isolation. The sample was, however, was representative of the older adult Australian population in terms of age, socioeconomic status and country of birth distributions.
Although clear associations between location, attitudes and CRC screening were evident in the current study, future research in a sample containing more males, a higher proportion of remote and very remote dwellers and more non-participants in the bowel screening program may yield more generalisable effects. Finally, it is important to note that the outcome measure (compliance) in this study reflects one case of kit receipt for each participant and therefore cannot be interpreted as current compliance/participation. Although it is likely that participants who had received more than one kit in the past referred to the most recent when answering questions, this cannot be assumed. Future research would benefit from collecting data regarding the recency and frequency of kit receipt and use.
Conclusions
Findings from the current study inform the development of future interventions to improve compliance with population FOBT bowel screening programs in terms of both target and strategy. As well as providing a case for placing more emphasis on recording compliance with CRC screening as opposed to program participation alone, they suggest that intervention is most needed in regional areas where program compliance is the lowest. Suboptimal compliance rates are evident in all non-metropolitan areas and interventions in these communities may be successful if they encourage the consideration of one’s future health and discourage stoic attitudes such as the minimisation of, and resignation to, health problems. In developing appropriately tailored interventions, the way in which individual attitudes and thinking styles impact preventive health behaviours in different communities must be considered.
Acknowledgements
This research was jointly funded by the University of Southern Queensland and Cancer Council Queensland.

