Introduction
Native Americans are more likely to live in poverty than any other racial or ethnic group in the USA, and to experience a significantly higher disease burden and lower life expectancy than the general US population1. Native Americans are significantly under-represented in the health professions, constituting only 0.4% of the physician workforce and 0.3% of the registered nursing workforce2, while representing 1% of the population at large3.
Diversity plays an important role in the delivery of quality health care, particularly for minority patients4-6. Racial concordance between patients and providers improves patient satisfaction7-10 and may lead to better outcomes11 as provider bias can affect decision-making in patient care12,13. Increased diversity of the health professional workforce could have a positive effect on patient satisfaction and health outcomes, particularly for non-White patients. Minority physicians are also more likely to work in underserved and rural areas14,15.
Healthcare professionals of all backgrounds would benefit from cultural competency education to improve their ability to care for diverse communities16-19. Direct contact with people from diverse ethnic backgrounds should be a central component of this education20.
Background
The Spirit Lake Reservation, founded in 1867, is the home of the Spirit Lake Dakota Tribe. It is located on the southern shore of Devils Lake in north-eastern North Dakota, across from a primarily White community on the northern shore. According to the 2010 US census, approximately 4000 people live at Spirit Lake and 7000 at Devils Lake21,22. The only hospital in the area has 25 beds, and access to most specialty services requires a 1.5 hour drive through sugar beet farm country to Grand Forks, the third largest city in the state and the home of the University of North Dakota. Spirit Lake is the home of the Cankdeska Cikana Community College (CCCC), a tribal college founded in 1974. Like the other tribal colleges and universities, CCCC aims to provide local opportunities for higher education in a culturally sensitive manner23,24.
In 2009, in response to a needs assessment by stakeholders from CCCC and members of the Spirit Lake Dakota Tribe, a collaborative relationship was formed with the Icahn School of Medicine at Mount Sinai and the Columbia University Mailman School of Public Health in New York. Together, the collaborators developed a survey course designed to increase the number of Native healthcare providers by exposing students to topics in public health and health careers, while simultaneously giving medical trainees exposure to a minority group they might not otherwise encounter during their education in New York City. In 2012, North Dakota State University (NDSU) school of nursing joined this partnership, bringing financial support through a Health Professional Opportunity Grant, and local nursing perspective. Each year, public health students, medical students, resident physicians and faculty from New York collaborated with colleagues from NDSU and CCCC to teach an introductory survey course in public health and the health professions. The course aimed to increase interest in health professional careers among Native American students and to improve the cultural competence of visiting health professions students25.
Intervention curriculum
The course was offered every summer from 2009 to 2015. The curriculum included didactic sessions on topics related to public health interventions, environmental health, substance abuse and health policy. Also offered were practical sessions that included visits to relevant community sites and discussions of the logistics of various health professions including nursing, social work, medicine and home health care. Workshops titled ‘Becoming a nurse’ or ‘Becoming a social worker’ provided students with tangible descriptions of prospective professions to pursue. Each year, the course curriculum was developed by a new group of student teachers (health professions students from New York) who revised it to incorporate their unique skills and interests. Student teachers developed the course curriculum during the academic year leading up to the summer course and then tailored the curriculum to the specific learning needs of the individual students enrolled in the class each summer. Sessions were led by student teachers and other instructors from Mount Sinai Medical Center, Columbia University, NDSU and CCCC, as well as invited professionals and para-professionals from the Spirit Lake community. Course participants included Native American students enrolled at the college, staff members at the college and elders in the community. Participants received a $700 stipend to cover travel, child care and the unearned wages from a summer job they would be unable to hold while participating in the course.
In the final year of the program, the collaborators sought to evaluate the impact of the course within the Native community and among the non-Native student teachers who traveled to North Dakota from New York. A two-part mixed methods study was designed with this aim in mind. Focus groups composed of former students in the program were held in Spirit Lake, North Dakota in 2015. The researchers chose to hold focus groups in order to learn firsthand about the former students’ experiences and so that participants could compare and contrast their experiences. Focus groups were also a way to ensure that participants with varying degrees of literacy would have the opportunity to share their experiences. The following year, the non-Native student teachers, who live throughout the country and unfortunately could not be gathered for in-person focus groups, were surveyed using an online survey tool.
Methods
Focus groups
With the help of CCCC staff members, former course participants were contacted in person, by phone, email and Facebook. They were invited to attend one of four focus groups held at CCCC. The research group was primarily composed of highly educated non-Native physicians and therefore great care was taken to consider the biases held by researchers, the cultural power differential between the primarily White researchers and the Native participants, and any potential for exploitation. Participants were offered a light meal and a $10 Walmart gift card as compensation for their time. Ground rules were set during each group to ensure respect, confidentiality and anonymity. To preserve anonymity, limited demographic data were collected or reported.
Fifteen Native American former class members participated in the focus groups, representing 27% (15/56) of possible participants (Table 1). Representatives from the first 6 years of the program were invited, but not all years were represented in the group. Students who took the course in 2015 were excluded because the focus groups were held while they were taking the course; therefore, their impressions of long term effects could not be accurately assessed.
Focus group discussions were semi-structured based on a topic guide, with open ended questions designed to elicit participant memories and thoughts about the course. Participants were invited to describe the influence that the course may have had on their career choices and plans for education and/or training. Participants were also queried about their views regarding the low number of healthcare professionals from their own tribe and what could be done to increase this number. Finally, they were asked about their perceptions of the visiting student teachers’ experiences in the Spirit Lake Nation.
Focus groups were audio-recorded and then transcribed verbatim. Two separate researchers coded all four of the transcripts using an inductive approach26. After coding the transcripts independently, the researchers met, compared coded data and resolved discrepancies in coded data to create a unified dataset. The researchers then independently re-coded the new transcripts with the new codes, and the process was repeated until saturation was achieved.
Table 1: Characteristics of focus group participants (Native American former class members; n=15) 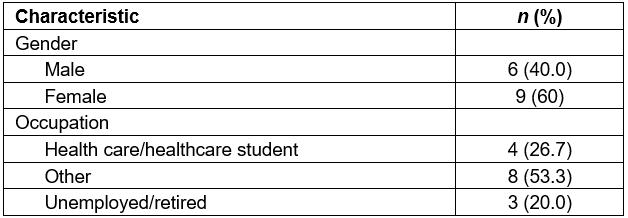
Every student teacher who participated in the intervention from 2009 to 2015 was contacted via email and invited to participate in the study by completing a written survey. The survey asked participants to state the degree to which they agreed or disagreed with various statements about their experience working with the students and collaborators from the Spirit Lake Nation. The survey also included open ended questions for participants to contribute personal reflections on the experience. The first author of this article, also a student-teacher, was excluded. The survey was designed to elicit participants’ general reflections about the program, to assess the influence of the program on perceptions of impoverished and under-represented minority patients and to assess whether this impacted their own career choices. Participants were also asked what, if anything, they believed the Native students gained from their experience taking the course. Demographic data, including current employment status, were collected. None of the questions were mandatory.Survey
Eighty-six percent (24/28) of former student-teachers responded to the survey. The respondents to the survey included public health professionals, physicians and medical students in a variety of specialties (Table 2).
Survey data were analyzed using descriptive statistics.
Table 2: Characteristics of survey respondents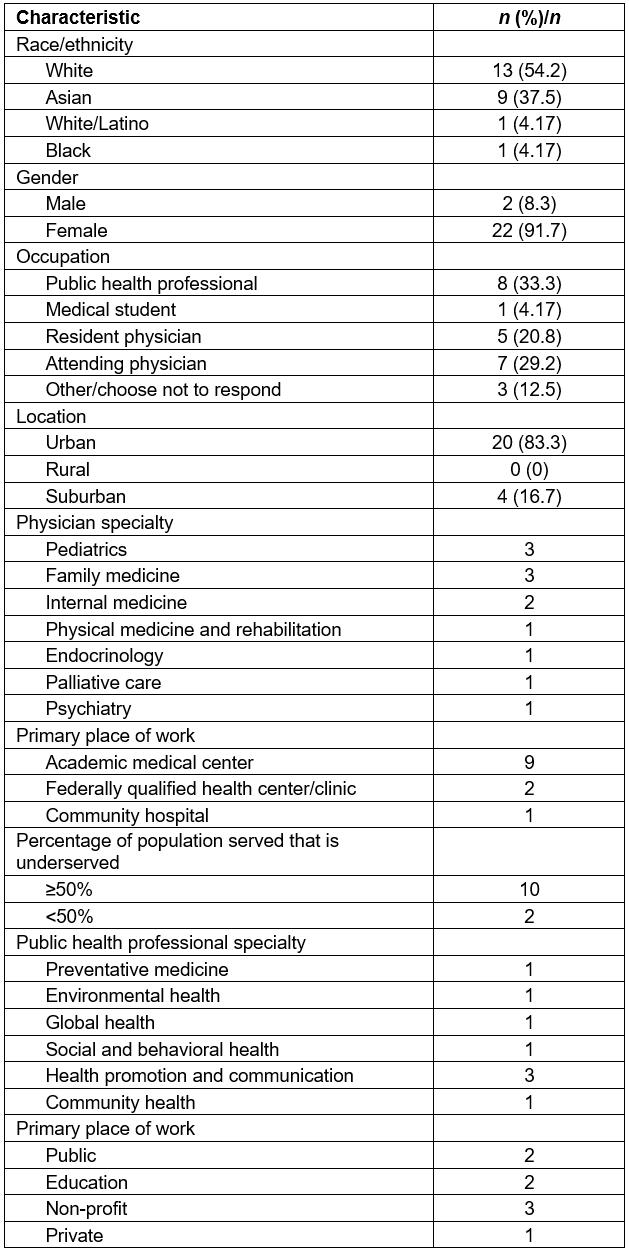
Ethics approval
Local investigational review board (IRB) permission (Spirit Lake Tribal Resolution #A05-12-087) and institutional IRB exemption (Mount Sinai IRB HS#: 16-00894, IDEATE#IRB-16-00457) were received prior to beginning the investigation.
Results
Focus groups with class participants
The majority of focus group participants were not working in the health field at the time of the focus groups. Many were employed by the college in administrative or educational roles. Other participants were retired, not working or working low wage jobs at local businesses. There were several notable exceptions to these trends. Two out of the 15 participants were enrolled in educational programs and on track to pursue health careers and another participant had started working in health care after participating in the course.
Major themes elicited from the focus groups included increased interest in and knowledge of health professions, increased knowledge and understanding of public health, improved health literacy, appreciation for cultural exchange and understanding, and awareness of barriers to entering health professions.
Knowledge about and interest in health and health professions: The majority of participants had not become health professionals, but most indicated that the course increased their interest in pursuing a health professional career. Additionally, participants indicated that the course deepened their understanding of the breadth and variety of career options within health care. One student shared:
I was not thinking about going into the health field at all until after I took this class. And then after I took this class and talking to the people in it, it just made me really interested and now it’s something that I would really like to do. It made a big effect on me.
Participants indicated that the course increased their knowledge and understanding of public health and the way that public health interventions are designed and implemented. Participants spoke about how this new framework motivated them to want to make change within their own communities. One participant stated:
It taught me about public health. Prevention is key … They came here and they taught all about public health and it made you realize how important it is to prevent all these diseases and all this and it makes you want to work towards bettering the people here on this reservation.
The class may also have helped to improve health literacy among participants. They described an increased comfort at the doctor’s office and the pharmacy, feeling more prepared to advocate for themselves or family members in the healthcare setting. One participant said:
After taking the class, being exposed to the different things I learned in class, I asked more questions … What’s the side effects? How long do I have to be on this medication?
Cultural exchange and understanding: Participants acknowledged that the course increased their interest and understanding of health professions, public health and health literacy, but the most often cited benefit was interaction with the student-teachers from New York City. Participants spoke of how they enjoyed learning about the student-teachers’ cultures and sharing their own. They expressed appreciation for the interest and compassion the non-Native student-teachers showed them:
What I got from the people that came down was their compassion for our people. They really were open. They wanted to know how we live, how we get by during the summers and the winters. And I was curious about them. I said, ‘How could you stand there walking around on the concrete 24/7 being where there’s no trees?’ They were curious about us and we were curious about them … We learned a lot about each other.
Connecting with the student-teachers meant more to the Native students than just cultural exchange. Participants spoke about how powerful it was to be seen and heard by non-Native people and to have outsiders take an interest in their lives and struggles:
I think we feel that we’re not important, because we live on the reservation … Outside the reservation, they don’t look up at us like we’re important. ‘All those Indians on the rez, they’re just —’ We’re labeled as drunks. So I mean, you students, teachers, from New York, ‘New York, New York’, coming here, to see us … It’s nice, it’s nice to feel important. It is.
Barriers to health professions: Participants also discussed what they perceived to be barriers to entry into health professions for students from the reservation. Money was frequently cited as a major barrier — whether for tuition, travel to and from school, books or child care. Family obligations were also seen as a barrier. Participants described having to take care of elderly or young family members. Some indicated that they felt a need to focus more on ensuring that their children graduated from high school than on their own education.
Participants spoke about how unprepared they and other people in their community were to pursue higher education. One participant, speaking in reference to a college program to train people to be certified nursing assistants, stated that the students ‘pass the skills, but you still gotta pass the written tests’. When asked what made it difficult for students to pass the written test, she replied, ‘they’re illiterate’. Another participant spoke of how schools on the Spirit Lake Reservation had the ‘worst scores in the entire state of North Dakota’27, which she reported was evidenced by the struggle CCCC faces in supporting local high school graduates who are challenged by college-level courses. Participants also spoke of how young people on the reservation lacked good role models to support and encourage them to finish school and continue through college.
Survey of New York-based participants
Effect of course on career interests and plans: Nearly all of the respondents (91.7%) agreed that their experiences in Spirit Lake made them better healthcare professionals and gave them greater empathy for their patients. Most (77.3%) respondents felt that their experiences in Spirit Lake made them more likely to work with underserved populations during their career and many (50%) reported that their experiences made them more likely to work in a rural area. All of the respondents agreed that their experiences deepened their understanding of Native Americans, people in poverty and ethnic minorities in general. Furthermore, respondents reported an increased understanding of the American healthcare system at large.
Perceptions of impact of course on Native students: Most respondents (87.5%) believed that the course was beneficial to the Native students in that they learned about health careers and public health, improved their health literacy, gained public health skills and learned things that could be used to help their communities. Respondents also believed it was beneficial to the course participants (as well as themselves) to learn about and interact with those from different cultural backgrounds. All of the respondents agreed that the course should continue.
Recommendations for future of course: Two open-ended questions were included in the survey, asking respondents for suggestions to improve the course and reflections on how participating in the program affected their career. Respondents recommended increasing the participation of the Native students in the planning and execution of the class and highlighted the need to maintain relationships between Native students and the student-teachers after course completion. Some respondents suggested that Native students at the college should be included in the design and implementation of the research projects that grow out of the program, as has been the case for CCCC’s faculty.
Reflections on experience in North Dakota: Most of the respondents reported that their experiences were deeply meaningful to their personal and professional lives. Respondents affirmed that their experiences increased their interest in working in rural areas or for the Indian Health Service (IHS) and increased their commitment to working with underserved populations. Other respondents spoke about how meeting and closely interacting with Native students provided real life examples of the social determinants of health:
It taught me how much health is tied up in the things we never address as physicians like work, the economy, family structure, culture and so many other things.
Numerous respondents wrote about how traveling to Spirit Lake increased their understanding of structural racism, how it affects health and how this understanding will make them better, more effective and more empathetic healthcare providers. One respondent wrote:
Honestly, this trip probably influenced me in many more ways than I really realize, but it permanently shifted the way I understand Native American health and the responsibility we have to work towards reversing the damage we’ve both directly and indirectly done to these communities.
Discussion
The study findings suggest that the program successfully increased interest in and knowledge about health professions among Native students and increased health professionals’ commitment to underserved populations.
CCCC students’ participation in the course appeared to increase interest in and knowledge about health and health careers; a small number of participants planned to enter health professions. These findings support previous studies, which showed that targeted educational interventions can increase interest in health careers for Native students28,29. The data collected also provide new insight to the challenges experienced by Native peoples on reservations and the ways that these difficulties impede their ability to pursue careers in the healthcare field.
The student-teachers who responded to the survey indicated that participating in the program increased their commitment to underserved populations and deepened their understanding of the complexities and structural problems leading to poor health outcomes for marginalized communities. Respondents affirmed a newfound interest in Native health. Several expressed interest in working for IHS upon completion of their training, mirroring the impact reported in similar immersive interventions for health professionals in Native communities30,31. Despite their sentiments, all of the respondents were currently working in urban or suburban areas and none were employed by IHS.
The program also had broader effects on both groups. Non-Native survey respondents reported that traveling to Spirit Lake and interacting with Native individuals reshaped their worldview, particularly their historical perspective. CCCC participants spoke about how meaningful it was to talk with empathetic outsiders about growing up on the reservation, the racism they had faced and the problems within their community. While the impact of this human connection is challenging to measure, it may have a more lasting effect than the acquisition of new knowledge and information. Future interventions should investigate the importance of these less tangible outcomes and work to further these beneficial effects.
The impact of this program suggests broad potential future directions, including formal mentoring for Native students by medical trainees and programming that is more tightly tailored to meet community needs. Increasing the number of Native healthcare workers and increasing the interest in Native health for non-Native healthcare workers could potentially have a meaningful impact on the health of Native communities.
The health professions course was not designed to have a significant impact on systemic issues such as disparities in health outcomes and ethnic concordance of health professionals for Native people. While exposure to education about the wide variety of health professions and public health topics is important, lack of such exposure is unlikely to be the primary reason why Native students do not ultimately pursue those careers. As the Native students described in the focus groups, the systemic issues that prevent Native students from being successful in higher education include such intersecting issues as structural racism, lack of access to quality primary education, lack of money and social or family issues related to poverty. A three-week summer course alone will not be able to mitigate the effects of a long history of oppression in the USA, and an understanding of this would be prudent when designing future interventions. Educational interventions will need to be implemented alongside broader social and health policy reforms in order for disparities to be effectively eliminated32.
In addition, the study evaluation technique was limited by the single administration of the survey and the potential bias related to recruitment for the focus groups. The focus group participants were more likely to be employed by the college, remain a student at the college or remain closely connected to the college, which likely occurred because they were easiest to contact to ensure participation. Additionally, some former class participants were unable to participate due to work obligations, some of which were in healthcare professions. This may mean that the focus group participants are not wholly representative of the students who took the class over the 7 years it was available. In fact, the sample may under-represent the number of students who went on to pursue education and careers in the health professions because such students may have been too busy to attend the focus groups.
Conclusion
The results of this study suggest that cross-cultural educational interventions can successfully increase interest in and knowledge about health professions among Native students while increasing non-Native interest in and commitment to Native communities specifically and underserved populations at large. The findings also document the challenges to entering health professions as elaborated by Native individuals and suggest that interest in entering a health profession or working in a rural area does not always translate to achieving those goals. Further interventions to improve the health and wellbeing of indigenous communities should be designed with these limitations in mind.
Acknowledgements
Many thanks to all of the students and student teachers who participated in the class, Ann Wadsworth and the rest of the wonderful staff of Cankdeska Cikana Community College, and the Spirit Lake Tribe.
References
You might also be interested in:
2021 - Problems in implementing interprofessional education in rural areas: an exploratory study
2007 - Clinical skills day: preparing third year medical students for their rural rotation

